Abstract
Cellular replicative senescence is a major contributing factor to aging and to the development and progression of aging-associated diseases. In this study, we sought to determine viral replication efficiency of influenza virus (IFV) and Varicella Zoster Virus (VZV) infection in senescent cells. Primary human bronchial epithelial cells (HBE) or human dermal fibroblasts (HDF) were allowed to undergo numbers of passages to induce replicative senescence. Induction of replicative senescence in cells was validated by positive senescence-associated β-galactosidase staining. Increased susceptibility to both IFV and VZV infection was observed in senescent HBE and HDF cells, respectively, resulting in higher numbers of plaque formation, along with the upregulation of major viral antigen expression than that in the non-senescent cells. Interestingly, mRNA fold induction level of virus-induced type I interferon (IFN) was attenuated by senescence, whereas IFN-mediated antiviral effect remained robust and potent in virus-infected senescent cells. Additionally, we show that a longevity-promoting gene, sirtuin 1 (SIRT1), has antiviral role against influenza virus infection. In conclusion, our data indicate that enhanced viral replication by cellular senescence could be due to senescence-mediated reduction of virus-induced type I IFN expression.
Keywords: Senescence, Influenza, VZV, SIRT1
INTRODUCTION
Aging is suggested to be promoted by cellular senescence because senescent cells accumulate in tissues and organs with age (1). Replicative senescence refers to a stage which normal cells undergo growth arrest after proliferating for a limited number of population doublings. The main features of replicative senescence are characterized by the following cellular phenotypes, such as large and flat cell morphology, increased SA-β-Gal activity, increased expression levels of p21/p53 and higher cellular production of reactive oxygen species (ROS) (2,3). A better understanding of the molecular mechanisms underlying the multi-step progression of senescence and determining the role of senescence during infection can provide potential therapeutic strategies for age-related infectious diseases.
Influenza virus (IFV) and Varicella Zoster Virus (VZV) are the pathogens that cause the most common infectious diseases worldwide and the elderly populations are most vulnerable to IFV and VZV infections. Influenza is an important contributor to morbidity and mortality worldwide as influenza virus infections result in about 250,000 to 500,000 deaths annually, and over 90% of influenza-related deaths occur in the older adult population. The efficacy and effectiveness of influenza vaccines decrease with age, due to the negative impact of aging on the development of the immune system and its ability to function (4,5). The detailed role and mechanisms of senescence that underlie the increase in the levels of susceptibility to influenza infection have not been well elucidated.
Shingles is caused by the reactivation of VZV that has persisted in latent form within sensory ganglia following an earlier episode of chickenpox, and is characterized by a painful skin rash affecting a significant proportion of the elderly population. The underlying mechanisms involved in VZV reactivation and susceptibility among the elderly or immunocompromised populations are currently unclear, although recent studies suggested that aging may cause an inability to efficiently clear virus-infected cells by immune cells (6). Furthermore, aging is also thought to decrease the efficacy and effectiveness of zoster vaccines, suggesting aging-associated decline in immunogenicity induced by vaccination (7).
Previous work has highlighted the age or senescence-associated decline of innate immune receptor function. For example, decreased toll-like receptor (TLR) function in dendritic cells, dysregulated signaling cascades, and decreased cytokine production have been shown to contribute to impaired innate immune responses (8,9,10,11). Similarly, age-associated defects in retinoic acid inducible gene-I (RIG-I) signaling specifically impairs interferon (IFN) signaling after infection with West Nile virus (WNV) (12). In addition to gene expression changes in receptors, senescence is known to cause inflammaging, characterized by the up-regulation of the inflammatory response that occurs with advancing age. Altered secretion levels of pro-inflammatory cytokines and chemokines, such as interleukin-8 (IL-8) and tumor necrosis factor-α (TNF-α), were observed in elderly mice (13). These aberrant cytokine responses are thought to contribute to the inability of the elderly to mount appropriate immune responses to pathogens, vaccines, and self-antigens.
Human sirtuins are composed of a family of seven nicotinamide adenosine dinucleotide (NAD)-dependent deacetylases that removes acetyl groups from wide ranges of essential proteins. SIRT1 has a broad range of physiological and biological functions, which play an important role in controlling gene expression, metabolism and aging (14). At cellular level, overexpression of SIRT1 was shown to prevent replicative senescence (15). Recent studies by Koyuncu et al identified SIRT1 as an ancient antiviral defense factor (16). They showed that siRNA-mediated inhibition of each of the seven sirtuins could enhance the virus plaque formation for human cytomegalovirus (HCMV) and influenza A virus. The detailed mechanisms of SIRT1-mediated antiviral activities remain to be fully determined.
In the present study, we used a replication-induced senescence in vitro model to illustrate the role and the mechanisms of senescence on viral replication and host response during viral infection. Our results demonstrate that senescent cells have an impaired ability to control viral replication and senescence-associated genes such as sirtuin 1 (SIRT1) exerts antiviral activities against influenza infection. Collectively, our data provides the first evidence for the importance of senescence-associated decline in the viral replication control of primary human epithelial and fibroblast cells.
MATERIALS AND METHODS
Cell culture and reagents
Normal human bronchial epithelial cells (HBE) were obtained from Lonza, Basel, Switzerland and grown in bronchial epithelial cell growth medium (BEGM) medium. Normal human dermal fibroblasts (HDF) (Lonza, Walkersville, MD, USA) were grown as adherent cultures in fibroblast basal medium supplemented with FGM SingleQuots (Lonza). Human lung adenocarcinoma cells (A549) and Madin-Darby canine kidney (MDCK) cells were obtained from the American Type Culture Collection (ATCC, Manassas, VA, USA). A549 cells were cultured in Roswell Park Memorial Institute (RPMI)-1640 medium (Invitrogen, Carlsbad, CA, USA) supplemented with 10% fetal bovine serum (FBS), 100 U/mL penicillin, and 100 µg/mL streptomycin and maintained at 37℃ with 5% CO2 in a humidified atmosphere. MDCK cells were grown in Dulbecco's Modified Eagle's Medium (DMEM) (Invitrogen) supplemented with 10% FBS, 100 U/mL penicillin, and 100 µg/mL streptomycin.
Sodium butyrate (NaB), and nicotinamide (NAM) were purchased from Sigma-Aldrich (St. Louis, MO, USA). Recombinant human interferon (IFN)-α, λ1, λ2 was purchased from R&D (Minneapolis, MI, USA) and interferon-β (IFN-β) protein was obtained from PBL Assay Science (Piscataway, NJ, USA).
Viruses and plaque assay
Human influenza virus A/Puerto-Rico/8/34 (H1N1) PR8 and the recombinant PR8 virus expressing green fluorescent protein (GFP) (rPR8-GFP) were kindly provided by Dr. Adolfo Garcia-Sastre (Icahn School of Medicine at Mount Sinai, NY, USA) (17). Virus titers were determined by standard plaque assay in MDCK cells with few modifications. VZV strain YC01 (GenBank Accession No. KJ808816) has been described previously (18) and was cultured in HFFs, as described before (19).
Cellular replicative senescence model
Replicative cellular senescence induction models were used in this study. HBE cells were grown until 7~9 passages and HDF cells were allowed to grow until after 20~25 passages, and senescent cells were verified by their delayed population-doubling times and by using an SA-β-Gal activity assay kit (Cell Signaling Technology, Beverly, MA, USA), as described previously (20). Briefly, cells were washed twice with PBS and incubated in 1 mL of fixing solution at room temperature for 20 min. After removing the fixing solution and washing three times with PBS, the fixed cells were stained with 1 mL of freshly prepared cell staining working solution at 37℃ and protected from light for 24 h. After staining, the cells were counted for SA-β-galactosidase positive staining observed by light microscopy (Olympus, Tokyo, Japan).
Assays for mitochondrial superoxide formation
Cells were stained with mitoSOX Red (Invitrogen) for 20 min and mitochondrial superoxide levels were measured by flow cytometry or confocal microscopy. For FACS analysis, cells were analyzed by a flow cytometer (Beckman Coulter, BC-FC500, Fullerton, CA, USA).
Western blot analysis
Protein lysates (30 µg total protein) were prepared using RIPA buffer (Sigma-Aldrich) and then separated by SDS-PAGE on 10~15% acrylamide gels and transferred to polyvinyldifluoride (PVDF) membranes. The membranes were then incubated in a blocking buffer comprised of 5% (w/v) BSA, 0.2 M Tris base, 1.36 M NaCl, and 0.1% Tween 20 (TBS/T) for 1 h at room temperature and washed three times with 5 mL of TBS/T for 5 min each wash. Membranes were incubated overnight with the primary antibodies against p21, STING, phospho-TBK, total TBK, p-IRF3, IRF3, β-actin (Cell Signaling Technology) at 4℃. For influenza A virus protein expression, anti-NS1 (Santa Cruz Biotechnology), and anti-NP antibodies (Sino Biological Inc., Beijing, China) were used. VZV gE antibody (Abcam, Cambridge, MA, USA) were used to measure the expression of VZV protein. After washing three times with TBS/T, the membranes were incubated with HRP-conjugated anti-rabbit or mouse IgG secondary antibody (Cell Signaling Technology) for 1 h at 25℃. After washing three times with TBS/T, membranes were incubated with Western Lumi Pico solution (ECL solution kit) (DoGen, Seoul, Korea), and exposed to film.
qRT -PCR
Total cellular RNA was prepared using TRIZOL reagent (Invitrogen). First-strand synthesis of cDNA from 1 µg of total RNA was performed using ImProm-II™ (Promega, Madison, WI, USA) according to the manufacturer's instructions. The changes in mRNA expression were calculated using the comparative Ct method as described previously (21). Data were normalized to glyceraldehyde 3-phosphate dehydrogenase (GAPDH) expression. Primer sequences can be given upon request. Quantification of cDNA was performed by qRT-PCR using Power SYBR® Green Master Mix (Invitrogen). Cycling parameters were 95℃ for 10 min, followed by 40 cycles of 95℃ for 30 s and 60℃ for 1 min. The specificity of each reaction was validated by melt curve analysis and agarose gel electrophoresis of PCR products. Expression was normalized using the ΔCt method, in which the amount of target, normalized to an endogenous reference and relative to a calibrator, is given by 2–ΔΔCt, where Ct is the cycle number of the detection threshold.
Immunofluorescence assay for viral replication
Cells were plated in 24-well plates and incubated overnight. Cells were washed twice with PBS and infected with rPR8-GFP virus at an multiplicity of infection (MOI) of 1.0 to allow for viral replication. Cells were infected with influenza in infection media followed by washing with PBS and culturing in RPMI-1640 medium with 2% FBS. After 24 h at 37℃ in 5% CO2, nuclei were stained with 1 µg/ml of the nuclear stain 4,6-diamidino-2-phenylindole (DAPI) (Sigma-Aldrich) for 5 min. Coverslips were mounted on to glass slides and virus-infected cells were examined by confocal microscopy (LSM700; Carl Zeiss, Jena, Germany).
Sirt1 siRNA transfection
Cells were seeded in 6-well plates and allowed to grow to a confluency of 70% over 24 hrs. Transient transfections with either control scrambled or Sirt1 siRNA (Bioneer, Daejeon, Korea) were performed with Lipofectamine RNAiMAX reagent® (Invitrogen), according to the manufacturer's protocol as previously described.
Statistical analysis
Paired comparisons were performed using the Student's t-test. Differences were considered statistically significant at p<0.05. All analyses were carried out with the Prism® software program (GraphPad Software, Inc., La Jolla, CA, USA).
RESULTS
Enhanced influenza virus infectivity by replicative senescence
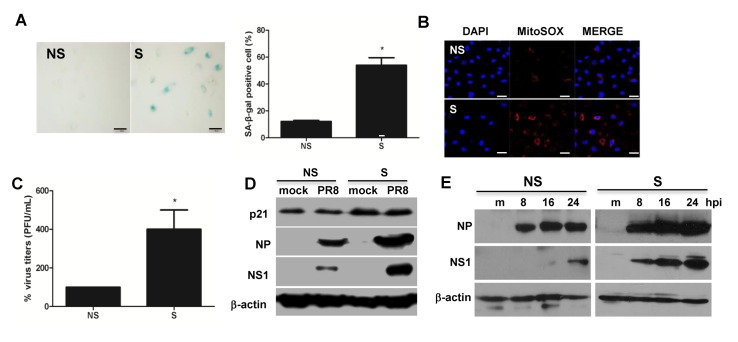
Replicative senescence was first described by Hayflick and Moorhead in human fibroblasts, after they observed cells undergoing extensive replication as a consequence of serial culture passages (22). Given that increased senescence-associated β-galactosidase (SA-β-gal) activity is a well-established biomarker of senescence (20), primary HBE cells were passaged up to 7~9 times until cells display senescent cell-like phenotype and positive SA-βgal staining cells were counted to validate senescence. As seen in Fig. 1A, replication-induced senescence in HBE cells resulted in increased numbers of cells positive for SA-β-gal staining, compared with that of non-senescent cells. We also observed that replicative senescence resulted in increased mitochondrial superoxide formation observed by mitoSOX staining (Fig. 1B).
Figure 1. Replicative senescence of primary human bronchial epithelial cells (HBE) is associated with dysregulated influenza virus replication. Induction of replicative (passage number–associated) senescence was confirmed by SA-β-galactosidase (gal) staining. (A) SA-β-gal staining was increased in senescent (S) HBE cells (right panel) relative to that of non-senescent (NS) cells (left panel). Magnification X200, Relative % SA-β-gal positive cells were counted and represented in the graph. (B) Assessment of mitochondrial superoxide generation was performed by mitoSOX RED staining. (C) NS and S cells were infected with the influenza virus strain PR8 at an MOI of 0.1 for 24 h. Progeny viral titers were calculated and expressed as % viral titers. Data are shown as means±SEM of three different experiments and are presented as the percentage of viral titer normalized to 100% in NS cells. Statistical analysis: *p<0.05 compared with 100% viral titers in NS cells. (D) Western blot analysis was performed in cell lysates of NS and S cells infected with PR8 virus at an MOI of 0.1 for 24 hours to assess the expression of senescence-associated p21 and influenza protein nucleoprotein (NP), nonstructural protein 1 (NS1) and actin. The blot shown is representative of three independent experiments. (E) NS and S cells were mock-infected or infected with PR8 for indicated length of time and western blotting was performed, similar to figure 1D.
We further examined whether the efficacy of influenza virus (IFV) replication differs between non-senescent (NS; passage number 2~4) and senescent (S; passage number 7~9) cell cultures. The reduced virus titers in the supernatants of IFV-infected cultures were confirmed by plaque assay. We detected increased plaque formation when analyzing the supernatants of infected cultures that had undergone replicative senescence (Fig. 1C). The protein levels of major viral proteins, nucleoprotein (NP) and nonstructural protein 1 (NS1), were also measured during senescence. Non-senescent and senescent HBE cells were infected with influenza A virus for 24 hours, and western blotting was performed. The expressions of senescence-associated markers, such as p21, were significantly higher in high passage cells than that in low passage cells. When compared with influenza-infected non-senescent cells, senescent cells had significantly elevated viral protein levels of NP and NS1 at 24 hours post-infection (hpi), suggesting that viral protein synthesis is more efficient in senescent cells than in non-senescent cells (Fig. 1D). Furthermore, Fig. 1E shows that there was delayed synthesis of viral protein NS1 in senescent cells, compared with that of non-senescent cells.
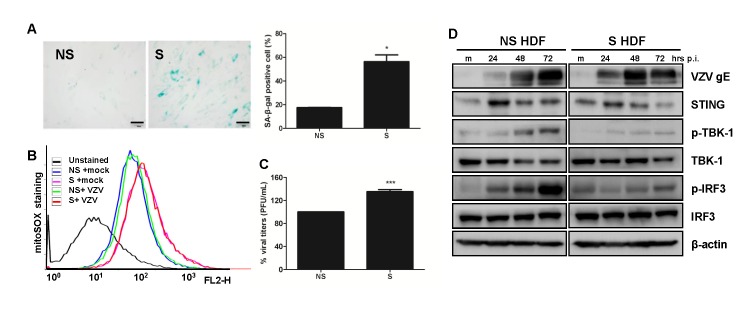
The effect of replicative senescence on VZV replication efficiency
To investigate if replicative senescence has a modulating effect on other viral replication, we used human dermal fibroblasts (HDF) in culture which underwent extensive replication as a consequence of serial passaging. To confirm the senescence phenotype during replicative senescence, we compared non-senescent HDF at low passage with senescent HDF that had higher than 20 passages, following infection with VZV. Induction of senescence in highly passaged HDF was confirmed, with increased numbers of SA-β-gal-positive cells observed (Fig. 2A). Then, we also confirmed that replicative senescence of HDF cells led to increased numbers of cells with positive mitoSOX staining, regardless of VZV infection (Fig. 2B). Next, plaque assay was performed to determine whether the efficacy of VZV replication differed between non-senescent and senescent cells. Senescent HDF exhibited approximately 1.5-fold higher VZV infectivity titers than non-senescent HDF (Fig. 2C).
Figure 2. Varicella Zoster Virus (VZV) replication efficiency in replication-induced senescent human dermal fibroblasts (HDF) cells. (A) SA-β-gal staining was increased in senescent (S) HDF cells (right panel) relative to that of non-senescent (NS) cells (left panel). Magnification X200, Relative % SA-β-gal positive cells were counted and represented in the graph. (B) Assessment of mitochondrial superoxide formation was performed by flow cytometry. MitoSOX Red stain revealed increased numbers of cells with superoxide in senescent HDF. (C) VZV progeny viral titers were calculated and expressed as plaque forming units (PFU)/mL. Virus titers in NS cells were normalized to 100% and relative virus titers were determined in S cells. Statistical analysis: ***p<0.001 compared with virus-infected NS cells. (D) HDF cells were mock-infected (m) or infected with the VZV for 24, 48 and 72 h. Protein levels of STING, pTBK-1, TBK-1 and p-IRF3 and IRF3 were analyzed by western blotting. Anti-actin monoclonal antibody was used as a loading control. VZV gE expression was also measured. The blot shown is representative of three independent experiments.
Given that VZV glycoprotein E (gE), encoded by ORF68, is the most abundant VZV glycoprotein and is required for viral replication in skin and T cells (23), we measured the protein synthesis of gE in VZV-infected HDF cells. At 24 hpi, gE levels were more increased in senescent HDF cells as compared to non-senescent HDF cells. Expressions of gE in VZV-infected senescent HDF cells continued to be more enhanced at 48 hpi, but were found to have decreased slightly at 72 hpi, whereas expression of gE in VZV-infected non-senescent HDF cells was the highest at 72 hpi, suggesting the delayed protein synthesis (Fig. 2D).
Our previous data suggested that Stimulator of Interferon Genes (STING) is important for host defense against VZV infection. Thus, expression levels of STING and its downstream signaling pathways, TANK-binding kinase 1 (TBK1) and interferon regulatory factor 3 (IRF3), were measured after VZV infection in HDF cells. Although mock-infected senescent cells showed higher basal expression levels of STING and p-IRF3 than mock-infected non-senescent cells, the induction levels of these proteins following VZV infection differed. Expression level of STING and phosphorylation of TBK-1 and IRF3 in non-senescent HDF cells appeared to be highly up-regulated after VZV infection at indicated times, compared with that in senescent HDF cells. These data suggest that viral infection-mediated host antiviral signaling pathways can be affected by replicative senescence (Fig. 2D).
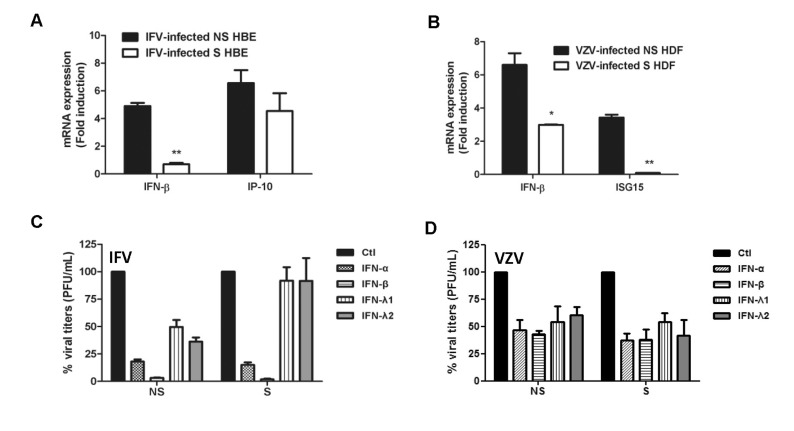
Replicative senescence-induced IFN expression and IFN responsiveness in response to viral infection
To further characterize whether replicative senescence would have any effect on host antiviral gene expression patterns, we compared mRNA fold induction levels of IFN-β and interferon-associated genes, such as IFN-γ-Inducible Protein 10 (IP-10) during IFV infection and interferon-stimulated gene 15 (ISG15) in response to VZV infection, in non-senescent and senescent cells. There were approximately ~5 and ~7 fold increases in IFN-β and IP-10 mRNA levels, respectively, at early timepoints (8 hpi) in non-senescent HBE cells, whereas its fold induction level was lower in senescent HBE cells (Fig. 3A). Similar to IFV infection, we also measured transcriptional levels of IFN-β and ISG15 in VZV-infected cells. In comparison with VZV-infected non-senescent cells, we observed significantly elevated mRNA levels of VZV ORF14 in VZV-infected senescent cells at 24 hpi. (data not shown). Replicative senescence in HDF cells drove a significant down-regulation of IFN-β and ISG15 gene induction, compared with that of VZV-infected non-senescent cells (Fig. 3B). These findings suggest that the induction patterns of antiviral genes following viral infection differ between non-senescent and senescent primary human cells.
Figure 3. The effect of senescence on viral infection-induced IFN expression and IFN-mediated antiviral activities. Host antiviral gene expression was assessed by qRT-PCR. The expression of IFN-β and IFN-γ-Inducible Protein 10 (IP-10) in response to IFV infection (A) and IFN-β and interferon-stimulated gene 15 (ISG15) in response to VZV infection (B) was normalized to GAPDH and shown as fold induction level relative to mock (m) control. The results are representative of three independent experiments. Statistical analysis: *p<0.05, **p<0.01 compared with virus-infected NS cells. (C, D) Recombinant human IFN-α (10 ng/mL), IFN-β (10 ng/mL), IFN-λ1 (10 ng/mL) and IFN-λ2 (10 ng/mL) were added to cells. Next day, cells were infected with IFV or VZV and plaque assays were performed. Progeny viral titers were calculated and expressed as plaque forming units (PFU)/mL. Control-treated cells were normalized to 100% viral titers and data are presented as the percentage of control treated samples. Data are shown as means±SEM of two independent experiments.
Following viral infection, cells begin to synthesize and secrete a range of antiviral molecules, including type I and III interferons, that are important for the recruitment of immune effector cells, activation of adaptive immunity, and attenuation of localized spread of virus infection by producing interferon stimulated genes (ISGs) (24). Most viruses are highly sensitive to interferon signaling and thus, the pre-treatment of cells with recombinant IFN proteins can result in the suppression of plaque formation. Recombinant human interferons α and β were used to represent type I IFNs, whereas interferons λ1 (IL-29) and λ2 (IL-28A) represented type III IFNs. Antiviral activities of these IFNs were measured by plaque assays, shown in Fig. 3C and D. Both type I and III IFN pre-treatments in non-senescent cells led to a significant reduction in plaque formation for IFV and VZV, compared with control-treated cells. Interestingly, antiviral effect of IFN-α and –β treatment resulted in greater reduction in plaque formation that that of IFN-λ1 or λ2 treatment in IFV-infected non-senescent cells. Moreover, type III IFN-mediated antiviral effect against IFV became attenuated in senescent cells, contributing to higher numbers of cells with plaque formation. For VZV infection, both type I and III IFN treatment led to 40~60% decrease in viral plaque formation, regardless of senescence levels of HDF cells. These data suggest that type I IFN-mediated antiviral responsiveness in senescent cells is not significantly affected by replicative senescence.
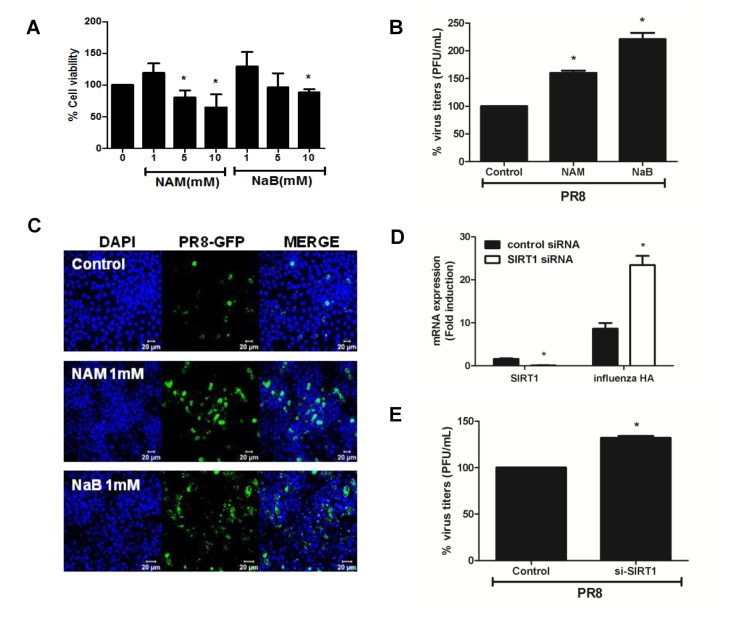
Role of anti-senescence gene SIRT 1 during influenza virus infection
SIRT1 can be considered as the most well-known anti-aging gene known so far but the effect of SIRT1 during viral infection has not been fully investigated. Thus, we investigated whether modulation of SIRT1 activity would have an impact on influenza viral replication. Nicotinamide (NAM) was used as a SIRT1-specific inhibitor and sodium butyrate (NaB) was used as an inhibitor of histone deacetylation in cultured cells. Among SIRT family members 1~7, SIRT1 expression was specifically induced upon influenza virus infection at 24 hpi (Data not shown). Influenza-infected cells were exposed to the SIRT1 inhibitor NAM and class I HDAC inhibitor NaB and cell viability was measured. At 1mM concentration of NAM and NaB, no cellular toxicity was found in A549 cells (Fig. 4A). Exposure of cells to NaB and NAM following influenza infection resulted in increased numbers of viral plaques as well as viral replication measured by rPR8-GFP-expressing virus infection model (Fig. 4B and C). Furthermore, we examined the effect of SIRT1 knockdown on influenza hemagluttinin (HA) gene expression by qRT-PCR. SIRT1 expression was efficiently inhibited by siRNA treatment, and there was a significant increase in the mRNA expression of influenza HA upon SIRT1 knockdown (Fig. 4D). Consistent with these findings, the knockdown of SIRT1 also led to a significant increase in viral plaque formation (Fig. 4E). Thus, these results suggest that SIRT1 can contribute to antiviral effect against influenza virus infection.
Figure 4. Antiviral effect of anti-senescence gene SIRT1. (A) A549 cells were treated with 3 concentrations (1, 5, and 10 mM) of SIRT1 inhibitor nicotinamide (NAM) and class I HDAC inhibitor sodium butyrate (NaB) for 24 h, after which cell viability was measured using the MTT assay. Data are shown as a percentage (%) of the cell viability of the control cells. The average of 3 independent experiments is shown. Statistical analysis: *p< 0.05 vs. DMSO control-treated group. (B) Cells were treated with 1 mM NAM and 1mM NaB, infected with influenza A PR8 virus, and plaque assay was performed. (C) A549 cells were infected with rPR8-GFP virus (MOI of 1) for 1 h, after which drugs were added in the media for 24 h and GFP expression was monitored by confocal microscopy. Scale bar=20 µM(D) Control or SIRT1-specific siRNA was transfected in A549 cells and the knockdown efficiency was measured by realtime qRT-PCR. SIRT1 mRNA level was greatly reduced upon the mRNA silencing, whereas knockdown of SIRT1 led to upregulation of influenza A hemagluttinin (HA) mRNA expression. Transcript expression levels were calculated in relation to the expression level of GAPDH. Statistical analysis: *p<0.05 compared with virus-infected control siRNA-transfected cells. (E) Plaque assays were performed following SIRT1-specific siRNA transfection in A549 cells. The average of two independent experiments is shown. Statistical analysis: *p <0.05 vs. the control siRNA-transfected cell.
DISCUSSION
In our study, we used two different virus infection models to examine the impact of replication-induced senescence and anti-senescence gene, SIRT1, on viral replication efficiency and host innate immune signaling pathways. A significant increase in viral replication efficiency was detected by replicative senescence during IFV and VZV infection. Furthermore, we confirmed that SIRT1 is an important antiviral factor, and SIRT inhibitor treatment or knockdown of SIRT1 resulted in the enhancement of virus plaque formation.
The two most highly studied forms of senescence include replicative senescence through cellular aging, and loss of telomeres and premature senescence induced by a wide range of stressors, including oncogenes and chemotherapeutics (25). Both forms of senescence can lead to permanent cellular growth arrest. In our study, we confirmed that replication-induced senescence caused distinct cellular phenotype in HBE and HDF cells, by confirming the followings; First, senescent cells revealed enlarged and flattened cell morphology with increased granularity. Second, increased numbers of senescent cells were stained with SA-associated β-gal staining and mitochondrial superoxide production increased with replicative age in human primary epithelial cells and fibroblasts, as well as increased protein levels of p21 (Fig. 1 and 2). Moreover, we also noticed telomere shortening and dysfunctional mitochondria in senescent cells (data not shown).
As one of possible mechanisms for the increase in viral replication in senescent cells, a reduction in interferon (IFN) response after viral infection may account for it. Although DNA damage response caused by senescence-induced cell growth arrest can lead to increased basal expression levels of IFN and IFN-associated genes, our data suggests that virus-mediated induction of IFN and IFN-associated genes are down-regulated in senescent cells. Weiland et al suggest that since senescence leads to a profound reprogramming of cellular phenotype, it is questionable whether senescent cells could function as efficient host cells, supporting viral gene expression and replication (26). Our previous studies with replicative senescence induced fibroblasts and progeria cells show that cellular senescence could impact the replication efficiency of VZV (27). Furthermore, a recent report suggests that there was an accelerated lysis of senescent cancer cells, supporting an enhanced viral replication with an increase in cell-associated and released infectious measles vaccine virus (MeV) particles (26). Another possibility for the enhanced viral replication associated with senescence may largely attributed to the disruption of mitochondrial dynamics in that a defect in mitochondrial dynamics in senescent cells may contribute to down-regulation of early interferon response by inactivating the fission factor dynamin-related protein 1 (DRP1) in favor of viral replication. Further studies are required to test this hypothesis.
It is generally accepted that the seasonal influenza vaccine has lower efficacy and effectiveness in the elderly than that in the younger population (28). Aging is known to cause many alterations to both innate and acquired immunity. In the elderly, these alterations generally result in the deterioration of immunity. Indeed, many immunological parameters vary significantly between the elderly and the young (11). In particular, Qian et al reported that dendritic cells from older donors have lower expression of type I IFN genes and diminished induction of interferon signaling proteins such as STAT1, IRF7, and IRF1, suggesting defective regulation of type I IFN (12). Given that retinoic acid-inducible gene (RIG-I) is known to recognize 5'triphosphorylated blunt ends of influenza virus genomic dsRNA, it is highly plausible that senescent cells may have impaired RIG-I dependent signaling and thus suppressed type I IFN signaling at the level of JAK/STAT activation following influenza A virus infection. Similarly, our previous studies with VZV showed that STING may be a novel VZV receptor and its expression following VZV infection is affected by replicative senescence (27). Additionally, STING-mediated IFN responses can be inhibited by age-enhanced endoplasmic reticulum (ER) stress during Streptococcus pneumoniae infection in an in vivo model (29). These data suggest that cellular senescence can contribute to dysregulated viral sensing of host cells and thus affect viral replication efficiency in these cells.
Among senescence-associated genes, SIRT1 is the best studied and currently considered to be the most important controlling factor involved in senescence and aging (30). Nicotinamide (NAM) is a well-known SIRT1 inhibitor (31,32) and we wanted to assess whether NAM-mediated inhibition of deacetylase activity of SIRT1 was able to modulate viral replication. As expected, SIRT1 inhibition led to increased viral plaque formation. Recent studies also indicate that human SIRT1 shows a broad range antiviral function against DNA and RNA viruses, suggesting that sirtuin-modulating drugs can be used to treat viral diseases (16,33,34). Thus, sirtuin-modulating drugs can have a significant impact on the potential therapeutic approach for influenza infection. Considering that SIRT1 can be induced by viral infection and potentially affect the host immune response, further studies on the in vivo role of SIRT1 in determining susceptibility to viral infection may shed light on the function of SIRT1 in the amelioration of viral infection-associated symptoms.
In conclusion, our data demonstrate that cellular replicative senescence can contribute to increased viral replication. Furthermore, we provide the evidence that replicative senescence-associated changes could affect IFN expression, but not IFN-mediated antiviral response, which could result in an increased susceptibility of senescent cells to viral infection. A better understanding of immunosenescence during viral infection will greatly improve our knowledge of the pathogenesis of the IFV and VZV and provide insight for therapeutic improvements in the response to IFV and VZV infection treatment in the elderly.
ACKNOWLEDGEMENTS
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT & Future Planning (NRF-2016R1C1B2006493).
Abbreviations
- IFV
Influenza virus
- VZV
Varicella-zoster virus
- NS
Non-senescent
- S
Senescent
- SIRT1
Sirtuin 1
- HBE
Human bronchial epithelial cells
- HDF
Human dermal fibroblasts
References
- 1.van Deursen JM. The role of senescent cells in ageing. Nature. 2014;509:439–446. doi: 10.1038/nature13193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hwang ES. Replicative senescence and senescence-like state induced in cancer-derived cells. Mech Ageing Dev. 2002;123:1681–1694. doi: 10.1016/s0047-6374(02)00102-1. [DOI] [PubMed] [Google Scholar]
- 3.Campisi J. The biology of replicative senescence. Eur J Cancer. 1997;33:703–709. doi: 10.1016/S0959-8049(96)00058-5. [DOI] [PubMed] [Google Scholar]
- 4.Dorrington MG, Bowdish DM. Immunosenescence and novel vaccination strategies for the elderly. Front Immunol. 2013;4:171. doi: 10.3389/fimmu.2013.00171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reber AJ, Chirkova T, Kim JH, Cao W, Biber R, Shay DK, Sambhara S. Immunosenescence and challenges of vaccination against influenza in the aging population. Aging Dis. 2012;3:68–90. [PMC free article] [PubMed] [Google Scholar]
- 6.Arvin A. Aging, immunity, and the varicella-zoster virus. N Engl J Med. 2005;352:2266–2267. doi: 10.1056/NEJMp058091. [DOI] [PubMed] [Google Scholar]
- 7.Levin MJ, Oxman MN, Zhang JH, Johnson GR, Stanley H, Hayward AR, Caulfield MJ, Irwin MR, Smith JG, Clair J, Chan IS, Williams H, Harbecke R, Marchese R, Straus SE, Gershon A, Weinberg A. Varicella-zoster virus-specific immune responses in elderly recipients of a herpes zoster vaccine. J Infect Dis. 2008;197:825–835. doi: 10.1086/528696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Panda A, Qian F, Mohanty S, van Duin D, Newman FK, Zhang L, Chen S, Towle V, Belshe RB, Fikrig E, Allore HG, Montgomery RR, Shaw AC. Age-associated decrease in TLR function in primary human dendritic cells predicts influenza vaccine response. J Immunol. 2010;184:2518–2527. doi: 10.4049/jimmunol.0901022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wong CP, Magnusson KR, Ho E. Aging is associated with altered dendritic cells subset distribution and impaired proinflammatory cytokine production. Exp Gerontol. 2010;45:163–169. doi: 10.1016/j.exger.2009.11.005. [DOI] [PubMed] [Google Scholar]
- 10.Shaw AC, Goldstein DR, Montgomery RR. Age-dependent dysregulation of innate immunity. Nat Rev Immunol. 2013;13:875–887. doi: 10.1038/nri3547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shaw AC, Joshi S, Greenwood H, Panda A, Lord JM. Aging of the innate immune system. Curr Opin Immunol. 2010;22:507–513. doi: 10.1016/j.coi.2010.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Qian F, Wang X, Zhang L, Lin A, Zhao H, Fikrig E, Montgomery RR. Impaired interferon signaling in dendritic cells from older donors infected in vitro with West Nile virus. J Infect Dis. 2011;203:1415–1424. doi: 10.1093/infdis/jir048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Baylis D, Bartlett DB, Patel HP, Roberts HC. Understanding how we age:insights into inflammaging. Longev. Healthspan. 2013;2:8. doi: 10.1186/2046-2395-2-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Haigis MC, Sinclair DA. Mammalian sirtuins:biological insights and disease relevance. Annu Rev Pathol. 2010;5:253–295. doi: 10.1146/annurev.pathol.4.110807.092250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen H, Wan Y, Zhou S, Lu Y, Zhang Z, Zhang R, Chen F, Hao D, Zhao X, Guo Z, Liu D, Liang C. Endothelium-specific SIRT1 overexpression inhibits hyperglycemia-induced upregulation of vascular cell senescence. Sci China Life Sci. 2012;55:467–473. doi: 10.1007/s11427-012-4329-4. [DOI] [PubMed] [Google Scholar]
- 16.Koyuncu E, Budayeva HG, Miteva YV, Ricci DP, Silhavy TJ, Shenk T, Cristea IM. Sirtuins are evolutionarily conserved viral restriction factors. MBio. 2014:5. doi: 10.1128/mBio.02249-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Manicassamy S, Belicha-Villanueva A, Pisanelli G, Pulendran B, Garcia-Sastre A. Analysis of in vivo dynamics of influenza virus infection in mice using a GFP reporter virus. Proc Natl Acad Sci U S A. 2010;107:11531–11536. doi: 10.1073/pnas.0914994107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jeon JS, Won YH, Kim IK, Ahn JH, Shin OS, Kim JH, Lee CH. Analysis of single nucleotide polymorphism among varicella-zoster virus and identification of vaccine-specific sites. Virology. 2016;496:277–286. doi: 10.1016/j.virol.2016.06.017. [DOI] [PubMed] [Google Scholar]
- 19.Choi EJ, Lee CH, Kim YC, Shin OS. Wogonin inhibits Varicella-Zoster (shingles) virus replication via modulation of type I interferon signaling and adenosine monophosphate-activated protein kinase activity. J Funct Foods. 2015;17:399–409. [Google Scholar]
- 20.Kurz DJ, Decary S, Hong Y, Erusalimsky JD. Senescence-associated (beta)-galactosidase reflects an increase in lysosomal mass during replicative ageing of human endothelial cells. J Cell Sci. 2000;113(Pt 20):3613–3622. doi: 10.1242/jcs.113.20.3613. [DOI] [PubMed] [Google Scholar]
- 21.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 22.Hayflick L, Moorhead PS. The serial cultivation of human diploid cell strains. Exp Cell Res. 1961;25:585–621. doi: 10.1016/0014-4827(61)90192-6. [DOI] [PubMed] [Google Scholar]
- 23.Moffat J, Ito H, Sommer M, Taylor S, Arvin AM. Glycoprotein I of varicella-zoster virus is required for viral replication in skin and T cells. J Virol. 2002;76:8468–8471. doi: 10.1128/JVI.76.16.8468-8471.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schneider WM, Chevillotte MD, Rice CM. Interferon-stimulated genes:a complex web of host defenses. Annu Rev Immunol. 2014;32:513–545. doi: 10.1146/annurev-immunol-032713-120231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ben-Porath I, Weinberg RA. The signals and pathways activating cellular senescence. Int J Biochem Cell Biol. 2005;37:961–976. doi: 10.1016/j.biocel.2004.10.013. [DOI] [PubMed] [Google Scholar]
- 26.Weiland T, Lampe J, Essmann F, Venturelli S, Berger A, Bossow S, Berchtold S, Schulze-Osthoff K, Lauer UM, Bitzer M. Enhanced killing of therapy-induced senescent tumor cells by oncolytic measles vaccine viruses. Int J Cancer. 2014;134:235–243. doi: 10.1002/ijc.28350. [DOI] [PubMed] [Google Scholar]
- 27.Kim JA, Park SK, Kumar M, Lee CH, Shin OS. Insights into the role of immunosenescence during varicella zoster virus infection (shingles) in the aging cell model. Oncotarget. 2015;6:35324–35343. doi: 10.18632/oncotarget.6117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Targonski PV, Jacobson RM, Poland GA. Immunosenescence:role and measurement in influenza vaccine response among the elderly. Vaccine. 2007;25:3066–3069. doi: 10.1016/j.vaccine.2007.01.025. [DOI] [PubMed] [Google Scholar]
- 29.Mitzel DN, Jacobson RM, Poland GA. Age-enhanced endoplasmic reticulum stress contributes to increased Atg9A inhibition of STING-mediated IFN-beta production during Streptococcus pneumoniae infection. J Immunol. 2014;192:4273–4283. doi: 10.4049/jimmunol.1303090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kida Y, Goligorsky MS. Sirtuins, cell senescence, and vascular aging. Can J Cardiol. 2016;32:634–641. doi: 10.1016/j.cjca.2015.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang T, Cui H, Ma N, Jiang Y. Nicotinamide-mediated inhibition of SIRT1 deacetylase is associated with the viability of cancer cells exposed to antitumor agents and apoptosis. Oncol Lett. 2013;6:600–604. doi: 10.3892/ol.2013.1400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sauve AA, Schramm VL. Sir2 regulation by nicotinamide results from switching between base exchange and deacetylation chemistry. Biochemistry. 2003;42:9249–9256. doi: 10.1021/bi034959l. [DOI] [PubMed] [Google Scholar]
- 33.He M, Gao SJ. A novel role of SIRT1 in gammaherpesvirus latency and replication. Cell Cycle. 2014;13:3328–3330. doi: 10.4161/15384101.2014.968431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pagans SA. SIRT1 regulates HIV transcription via Tat deacetylation. PLoS Biol. 2005;3:e41. doi: 10.1371/journal.pbio.0030041. [DOI] [PMC free article] [PubMed] [Google Scholar]