Abstract
In patients with advanced or metastatic lung cancer who present predominantly with dyspnoea and haemoptysis the use of HDR brachytherapy has been proven an effective method of palliation. The application of brachytherapy as a boost to EBRT in curative cases is much more restricted. It can be considered in a selected group of patients with dominating endobronchial disease, who are medically inoperable, or have small or occult carcinomas of the lung.
Keywords: lung cancer, brachytherapy, palliative treatment, radical treatment
Technique of application
In order to evaluate the airway, locate the neoplastic infiltration and define the site of obstruction, an initial bronchoscopy is performed. The catheter (either a 5- or 6-French) used to deliver the brachytherapy should be inserted through the brush channel of the bronchoscope (Fig. 1). If a 6-French catheter is used, a large bronchoscope with brush channel diameter of at least 2.2 mm is required. If the HDR source has to pass tight curves it is not possible with the 5-Fr catheter and the use of a 6-Fr catheter is necessary. If the bronchoscope is connected to a teaching head or a video monitor the physician performing the application can visualize the lesion and the catheter (Figs. 2–9). For the patient’s comfort the bronchoscope should be inserted through the nose. Then the afterloading catheter is inserted through the brush channel of the bronchoscope, passes through the tumour, and is lodged in one of the smaller bronchi. It is recommended to perform a fluoroscopic confirmation of the catheter’s position. Then the distance between the proximal extent of the tumour and fixed structures such as the carina is measured. While the radiation oncologist pushes the catheter in, the assisting physicist (pulmonologist or experienced radiation oncologist) carefully withdraws the bronchoscope. The use of fluoroscopy helps in keeping the catheter in place during this push-pull technique of bronchoscope removal. The catheter should be secured with tape at the nose, and its position is marked in ink to alert the medical staff in case of displacement. The length of the catheter from the tip of the nostril should be noted. In some situations (tumour localized in the carina of the main bronchi or smaller bronchi) multiple catheters are to be used. In such case the procedure is repeated, taking care to clearly mark and describe each catheter. Localization X-rays with radioopaque dummy wires in the catheter are then obtained (Figs. 10–13). To determine the length to be irradiated and the initial dwell position the location of the obstruction and the target length are marked on the X-rays. The length to be irradiated usually covers the endobronchial tumour and ± 2.0-cm proximal and distal margins.
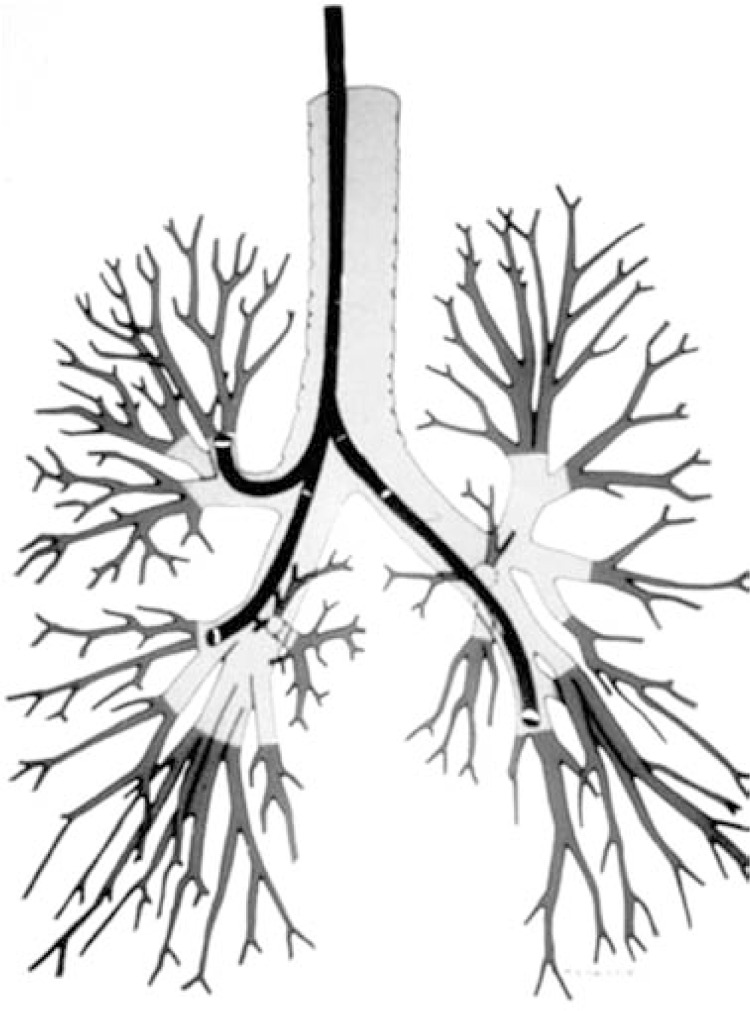
Fig. 1.
Flexible bronchofibroscope makes possible insertion of endoluminal applicators through bronchoscope into lobular and segmental bronchus
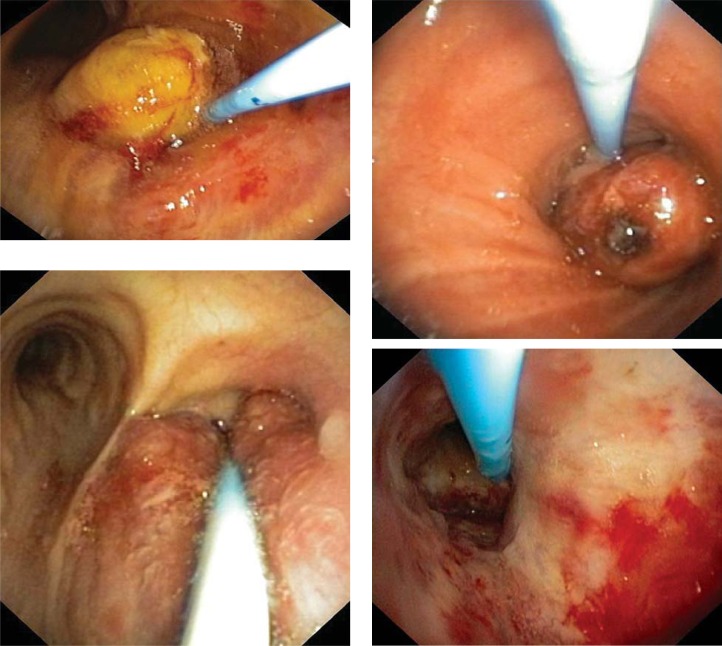
Fig. 2-5.
Examples – tumour in main bronchus visible, French 6 catheter placed in bronchus close by, scale on catheter visible
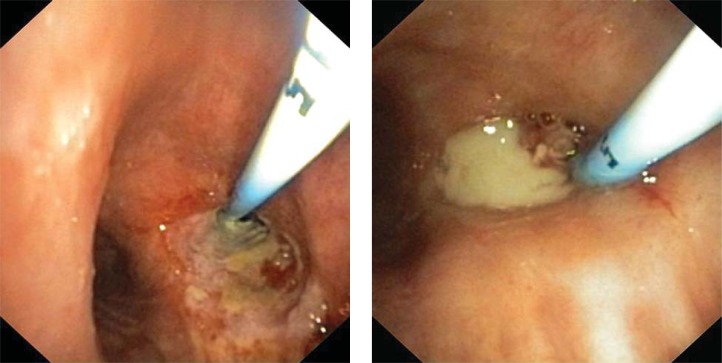
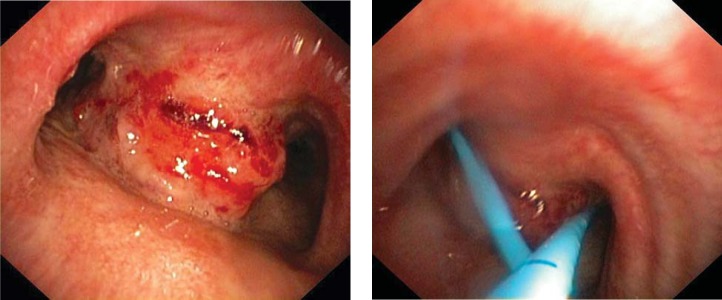
Fig. 8-9.
Examples – tumour in lobular bronchus visible, total obstruction of bronchus. French 6 catheter placed in bronchus through tumour
Fig. 10.
Endobronchial applicator with metal marker inside used for treatment planning, tumour localized in right upper lobe bronchus, X-ray picture
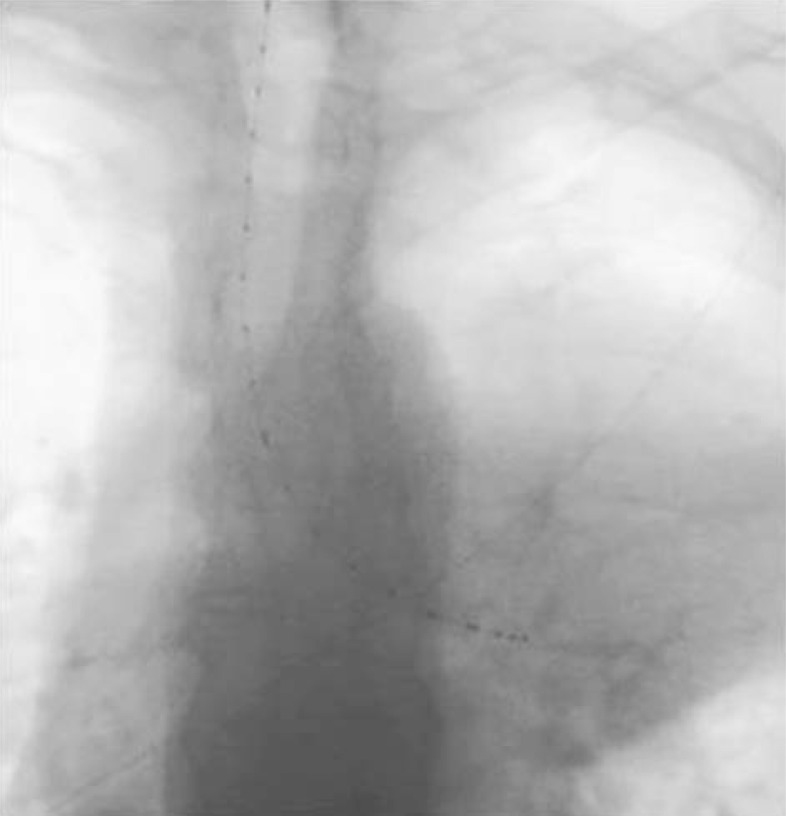
Fig. 13.
Bilateral lung cancer – endobronchial applicators with metal markers inside used for treatment planning, tumour infiltrating carina and both main bronchi, X-ray picture
Fig. 6-7.
Tumour infiltrating carina and both main bronchi before application and after application of two catheters
Fig. 11.
Endobronchial applicator with metal marker inside used for treatment planning, tumour localized in left main bronchus, X-ray picture
Fig. 12.
Endobronchial applicator with metal marker inside used for treatment planning, tumour localized in left main and upper bronchus, X-ray picture
The dose has been commonly prescribed at 1 cm from the source although various points from 0.5 to 2 cm are used [1, 2].
If standard lengths and doses are used the whole time of the brachytherapy procedure can be shortened by starting treatment without any delay. When a single catheter is used and if there is minimal curvature in the area to be irradiated it is possible to minimize the treatment planning time by using pre-calculated treatment plans for 3- to 10-cm lengths to be irradiated to 5 or 7.5 Gy at 1 cm from the source using equal dwell times. However, individualized image-based treatment planning must be performed if multiple catheters are used.
Brachytherapy as a sole palliative treatment or as a planned boost to a palliative course of EBRT
It is clinically proven that the optimum indications for palliative endobronchial brachytherapy include patients with a significant endobronchial tumour component that causes shortness of breath, persistent cough, and other signs of obstructive pneumonitis [1, 3–5]. A typical indication is also haemoptysis. Patients with extrinsic tumours that predominantly compress the bronchus or the trachea are poor candidates for endobronchial brachytherapy. In the general opinion, endobronchial brachytherapy can give quicker palliation of obstruction than EBRT. Furthermore, fractionated brachytherapy as a semi-ambulatory procedure can be more convenient for many patients than 2 to 3 weeks of daily EBRT. A common indication is recurrence after previous high-dose, radical EBRT. Other, individual indications are patients who are unable to tolerate EBRT because of poor lung function.
Palliative endobronchial brachytherapy can be used as a sole modality in non-irradiated patients or as a boost to palliative EBRT of 30 Gy in 10 to 12 fractions. A variety of doses have been successfully applied in various centres. Total doses ranging from 15 Gy to 47 Gy HDR in one to five fractions calculated at 1 cm have been most commonly reported [3, 4]. From the clinical point of view there is no evidence of superiority for one regime over the other. Using the linear quadratic model it has been estimated that commonly reported fractionation regimes have similar radiobiological equivalence [6]. Depending on the clinical situation and risk of potential post-radiological complications, the benefits of fewer bronchoscopic applications should be weighed against the risks of higher dose per fraction. The ABS suggests using three weekly fractions of 7.5 Gy each or two fractions of 10 Gy each or four fractions of 6 Gy each prescribed at 1 cm when HDR is used as the sole treatment for palliation [1]. The interval between fractions is generally 1 to 2 weeks.
When HDR is used as a planned boost to a palliative course of EBRT of 30 Gy in 10 to 12 fractions, the ABS suggests using two fractions of 7.5 Gy each or three fractions of 5 Gy each or four fractions of 4 Gy each (prescribed at 1 cm) in patients with no previous history of thoracic irradiation [1].
Palliative endobronchial brachytherapy is effective in relief of symptoms and safe. The clinical improvement after typical total and fraction doses, reported in the biggest series, can be obtained in 50-100%. The radiological improvement proved by X-ray examination is lower and varies between 36% and 100%. The bronchoscopy response reported in some series is also high, in the range of 74-100% [7–15]. Comparison of results from the literature is difficult because of the heterogeneity of the patient population and the variability in total and fraction dose employed. The most common complication after endobronchial brachytherapy is radiation bronchitis and stenosis [16]. Thus patients need close follow-up. The most serious complication is fatal haemoptysis, which could result from the high dose delivered to the area of the pulmonary artery. It is very difficult to distinguish this complication from failure of treatment due to progression of the disease [17]. A left upper lobe location, a high previous external beam radiation dose, multiple courses of brachytherapy, or long irradiated segments increase the rate of haemoptysis [18]. Incidence of fatal haemoptysis varies from 0% to 50% with a median value of 8% [4].
Curative endobronchial brachytherapy
According to international recommendations, the standard, definitive therapy for unresectable lung cancer is a combination of neoadjuvant or concomitant chemotherapy and EBRT. Some patients, especially with predominantly endobronchial tumour, may benefit from endobronchial brachytherapy, either alone or as an extremely conformal boost to EBRT. The patients that can benefit the most from curative endobronchial radiation alone are those with occult carcinomas of the lung confined to the bronchus or trachea. However, in this setting an alternative to this option can be extra skull stereotactic radiosurgery. There are a few encouraging data in the literature reporting the preliminary results of small series [19–23].
Endobronchial brachytherapy can be used in combination with EBRT for selected patients with inoperable non-small cell lung carcinoma. However, there are few reports dealing with combined EBRT and endobronchial brachytherapy. The authors obtained median survival in the range of 8 to 13 months with acceptable risk of complications [7, 9, 13, 24–27]. In a non-randomized prospective study on 320 patients with advanced inoperable non-small cell lung cancer, Muto et al. evaluated three endobronchial brachytherapy schemes (10 Gy in one fraction, 14 Gy in two fractions, or 21 Gy in three fractions) given concomitantly with EBRT [27]. Median survival for all patients was 11.1 months with a symptomatic response rate ranging from 82% to 94%.
Endobronchial brachytherapy with curative intent can also be considered in selected, early stage patients who are medically inoperable because of refusal of surgery, decreased pulmonary function, or advanced age. In a study on 34 patients treated with an HDR dose of 30 Gy in six fractions (5 Gy fractions given once a week), Marsiglia et al. reported a survival rate of 78% with a median follow-up of 2 years [28].
Endobronchial brachytherapy can also be used as adjuvant treatment in selected cases with minimal residual disease after surgical resection. Macha et al. [12] reported tumour-free survival up to 4 years in 19 patients with doses of 20 Gy delivered in four fractions at 1 cm from the source axis.
In selected cases of post-obstructive pneumonia or lung collapse, brachytherapy can be used to open the bronchus, aerate the lung and allow some sparing of normal lung from subsequent EBRT.
According to the ABS suggestions an HDR dose of three 5 Gy fractions or two 7.5 Gy fractions as a boost to EBRT (either 60 Gy in 30 fractions or 45 Gy in 15 fractions) should be given [1]. The HDR dose should be prescribed at a distance of 1 cm from the central axis of the catheter and given weekly. If endobronchial brachytherapy is used alone in previously non-irradiated patients, HDR doses of five 5-Gy fractions or three 7.5-Gy fractions prescribed to 1 cm is suggested.
Acknowledgements
The author thanks Dr Janusz Skowronek from the Greater Poland Cancer Centre for bronchoscopy and X-ray pictures.
References
- 1.Nag S, Kelly JF, Horton JL, et al. The American Brachytherapy Society recommendations for HDR brachytherapy for carcinoma of the lung. Oncology. 2001;15:371–381. [PubMed] [Google Scholar]
- 2.Speiser BL. High dose-rate endobronchial brachytherapy: Whither goest thou? Int J Radiat Oncol Biol Phys. 1992;23:250. doi: 10.1016/0360-3016(92)90571-x. [DOI] [PubMed] [Google Scholar]
- 3.Gaspar LE. Brachytherapy in lung cancer. J Surg Oncol. 1998;67:60–70. doi: 10.1002/(sici)1096-9098(199801)67:1<60::aid-jso13>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 4.Mehta MP, Speiser BL, Macha HN. High dose rate brachytherapy for lung cancer. In: Nag S, editor. High dose rate brachytherapy: A textbook. Armonk: Futura Publishing Co.; 1994. pp. 295–319. [Google Scholar]
- 5.Speiser BL. Brachytherapy in the treatment of thoracic tumors: Lung and esophageal. Hematol Oncol Clin North Am. 1999;13:609–634. doi: 10.1016/s0889-8588(05)70079-4. [DOI] [PubMed] [Google Scholar]
- 6.Nag S, Gupta N. A simple method of obtaining equivalent doses for use in HDR brachytherapy. Int J Radiat Oncol Biol Phys. 2000;46:507–513. doi: 10.1016/s0360-3016(99)00330-2. [DOI] [PubMed] [Google Scholar]
- 7.Aygun C, Weiner S, Scariato A, et al. Treatment of non-small cell lung cancer with external beam radiotherapy and high dose rate brachytherapy. Int J Radiat Oncol Biol Phys. 1992;23:127–132. doi: 10.1016/0360-3016(92)90551-r. [DOI] [PubMed] [Google Scholar]
- 8.Celebioglu B, Gurkan OU, Erdogan S, et al. High dose rate endobronchial brachytherapy effectively palliates symptoms due to inoperable lung cancer. Jpn J Clin Oncol. 2002;32:443–448. doi: 10.1093/jjco/hyf102. [DOI] [PubMed] [Google Scholar]
- 9.Chang LFL, Horvath J, Peyton W. High dose rate afterloading intraluminal brachytherapy in malignant airway obstruction of lung cancer. Int J Radiat Oncol Biol Phys. 1994;28:589–596. doi: 10.1016/0360-3016(94)90183-x. [DOI] [PubMed] [Google Scholar]
- 10.Escobar-Sacristan JA, Granda-Orive JI, Gutierrez JT, et al. Endobronchial brachytherapy in the treatment of malignant lung tumors. Eur Respir J. 2004;24:348–352. doi: 10.1183/09031936.04.00114902. [DOI] [PubMed] [Google Scholar]
- 11.Kelly JF, Delclos ME, Morice C, et al. High-dose-rate endobronchial brachytherapy effectively palliates symptoms due to airway tumors: The 10-year M.D. Anderson Cancer Center experience. Int J Radiat Oncol Biol Phys. 2000;48:697–702. doi: 10.1016/s0360-3016(00)00693-3. [DOI] [PubMed] [Google Scholar]
- 12.Macha HN, Wahlers B, Reichle C, et al. Endobronchial radiation therapy for obstructing malignancies: Ten years' experience with iridium-192 high-dose radiation brachytherapy afterloading technique in 365 patients. Lung. 1995;173:271–280. doi: 10.1007/BF00176890. [DOI] [PubMed] [Google Scholar]
- 13.Mehta MP, Petereit DG, Chosy L, et al. Sequential comparison of low dose rate and hyperfractionated high dose rate endobronchial radiation for malignant airway occlusion. Int J Radiat Oncol Biol Phys. 1992;23:133–139. doi: 10.1016/0360-3016(92)90552-s. [DOI] [PubMed] [Google Scholar]
- 14.Sutedja G, Baris G, Schaake-Koning C, et al. High dose rate brachytherapy in patients with local recurrence after radiotherapy of non-small cell lung cancer. Int J Radiat Oncol Biol Phys. 1992;24:551–553. doi: 10.1016/0360-3016(92)91072-u. [DOI] [PubMed] [Google Scholar]
- 15.Zajac AJ, Kohn ML, Heiser D, et al. High dose rate intraluminal brachytherapy in the treatment of endobronchial malignancy. Radiology. 1993;187:571–575. doi: 10.1148/radiology.187.2.7682723. [DOI] [PubMed] [Google Scholar]
- 16.Speiser BL, Spratling L. Radiation bronchitis and stenosis secondary to high dose rate endobronchial irradiation. Int J Radiat Oncol Biol Phys. 1993;25:589–597. doi: 10.1016/0360-3016(93)90003-e. [DOI] [PubMed] [Google Scholar]
- 17.Speiser B, Spratling L. Fatal hemoptysis: Complication or failure of treatment. Int J Radiat Oncol Biol Phys. 1993;25:925. doi: 10.1016/0360-3016(93)90325-p. [DOI] [PubMed] [Google Scholar]
- 18.Khanavkar B, Stern P, Alberti W, et al. Complications associated with brachytherapy alone or with laser in lung cancer. Chest. 1991;99:1062–1065. doi: 10.1378/chest.99.5.1062. [DOI] [PubMed] [Google Scholar]
- 19.Furuta M, Tsukiyama I, Ohno T, et al. Radiation therapy for roentogenographically occult lung cancer by external beam irradiation and endobronchial high dose rate brachytherapy. Lung Cancer. 1999;25:183–189. doi: 10.1016/s0169-5002(99)00059-8. [DOI] [PubMed] [Google Scholar]
- 20.Perol M, Caliandro R, Pommier P, et al. Curative irradiation of limited endobronchial carcinomas with high-dose-rate brachytherapy. Results of a pilot study. Chest. 1997;111:1417–1423. doi: 10.1378/chest.111.5.1417. [DOI] [PubMed] [Google Scholar]
- 21.Saito M, Yokoyama A, Kurita Y, et al. Treatment of roent-genographically occult endobronchial with external beam radiotherapy and intraluminal low dose rate brachytherapy: Second report. Int J Radiat Oncol Biol Phys. 2000;47:673–680. doi: 10.1016/s0360-3016(00)00489-2. [DOI] [PubMed] [Google Scholar]
- 22.Sutedja G, Baris G, van Zandwijk N. High dose rate brachytherapy has a curative potential in patients with intraluminal squamous cell lung cancer. Respiration. 1994;61:167–168. doi: 10.1159/000196330. [DOI] [PubMed] [Google Scholar]
- 23.Tredaniel J, Hennequin C, Zalcman G, et al. Prolonged survival after high dose rate endobronchial radiation for malignant airway obstruction. Chest. 1994;105:767–772. doi: 10.1378/chest.105.3.767. [DOI] [PubMed] [Google Scholar]
- 24.Anacak Y, Mogulkoc N, Ozkok S, et al. High dose rate endobronchial brachytherapy in combination with external beam radiotherapy for stage III non-small cell lung cancer. Lung Cancer. 2001;34:253–259. doi: 10.1016/s0169-5002(01)00249-5. [DOI] [PubMed] [Google Scholar]
- 25.Cotter GW, Craig L, Ellingwood KE, et al. Inoperable endobronchial obstructing lung cancer treated with combined endobronchial and external beam irradiation: A dosimetric analysis. Int J Radiat Oncol Biol Phys. 1993;27:531–535. doi: 10.1016/0360-3016(93)90376-7. [DOI] [PubMed] [Google Scholar]
- 26.Huber RM, Fischer R, Haútmann H, et al. Does additional brachytherapy improve the effect of external irradiation? A prospective, randomized study in central lung tumors. Int J Radiat Oncol Biol Phys. 1997;38:533–540. doi: 10.1016/s0360-3016(97)00008-4. [DOI] [PubMed] [Google Scholar]
- 27.Muto P, Ravo V, Panelli G, et al. High-dose rate brachytherapy of bronchial cancer: Treatment optimization using three schemes of therapy. Oncologist. 2000;5:209–214. doi: 10.1634/theoncologist.5-3-209. [DOI] [PubMed] [Google Scholar]
- 28.Marsiglia H, Baldeyrou P, Lartigau E, et al. High-dose-rate brachytherapy as a sole modality for early-stage endobronchial carcinoma. Int J Radiat Oncol Biol Phys. 2000;47:665–672. doi: 10.1016/s0360-3016(00)00486-7. [DOI] [PubMed] [Google Scholar]