Abstract
Background
Retention in treatment is a key factor to the success of methadone maintenance treatment (MMT) and considered an important measure in evaluation of treatment effectiveness.
Objectives
This study aimed to investigate the retention rate and predictors of retention in MMT in Rafsanjan.
Patients and Methods
This was a historical cohort study. A total of 1396 patients admitted between March 2011 and March 2012 in 16 MMT clinics (13 private and 3 state clinics) in Rafsanjan, entered the study and their retention rate was examined for one year. The patients’ data abstracted from their medical records using checklists and collected by clinics’ staff. Data analyses were performed using SPSS 15.0 and SAS 9.1. Kaplan-Meier method and Cox proportional hazards model were used to determine the retention rate and identify predictors of retention, respectively.
Results
The mean age of 1396 patients was 37.65 ± 10.77 years and most patients were men (93.8%). The mean and median of retention duration were 193.22 ± 3.83 and 153 ± 9.54 days, respectively. Three-month and one-year retention rates were 66.0% and 34.4%, respectively. Predictor variables of one-year retention in Cox proportional hazards model were high methadone dosage, polysubstance abuse and treatment under state clinics.
Conclusions
In this study, retention rate was lower compared to previous studies from other countries. The results suggested that program related factors are better predictors of retention than individual related ones.
Keywords: Retention; Methadone; Maintenance; Cox Models, Iran
1. Background
Methadone maintenance treatment (MMT) is one of the most effective treatment methods in opioid dependence worldwide (1-3). Retention in treatment is a key factor for a successful MMT and considered critical in evaluation of treatment effectiveness (4-8).
Longer retention in treatment is the most important factor and there have been positive relationships with positive outcomes, such as reducing risk of relapse to drug use and high-risk behaviours (9-12). Drug users who remain in the treatment for a longer time have lower mortality, function better in society and have lower risk of contracting HIV than those who leave the treatment (12-15).
Previous studies have shown that retention rate in MMT is influenced by three factors of individual, program and social related factors. Individual related factors included age (16-18), gender (19, 20), race (21, 22), opiates use history (23, 24), HIV (25, 26), criminal history (18, 27) and mental health status. Program related factors include the methadone dosage (17, 27, 28), treatment service accessibility such as services cost and distance to therapeutic center (20, 29) and social related factors including family (30), society (31) and peers’ support (28).
One primary goal of MMT was to maintain patients on treatment as long as they achieve positive outcomes of treatment (2). Therefore, identification of factors associated with retention is essential.
2. Objectives
The present study was performed to investigate retention rate and predictor variables of retention in MMT among drug users in Rafsanjan.
3. Patients and Methods
This was a historical cohort study. A total of 1396 patients admitted between March 2011 and March 2012 in 16 MMT clinics (13 private and 3 state clinics) in Rafsanjan, entered the study and their retention rate was examined for one year.
The patients’ data abstracted from their medical records using checklists and collected by clinics’ staff. The checklists included demographic information, criminal history, pattern of drug use and the average dosage of daily methadone use during treatment.
Retention duration in MMT was the outcome variable. Retention was defined by the number of days a patient remained in MMT and calculated from the first MMT entry up to the date patients dropped out of treatment.
Predictor variables of retention were examined in two groups of individual and program related factors. Individual related factors included age, gender, marital status, education, employment, physical and mental illness history, addiction treatment history, polysubstance abuse, opiates use duration and prison history. Polysubstance abuse is defined as history of using two or more groups of addictive substances prior to treatment. Program related factors included type of clinic (private or state clinics), average dosage of methadone and experience of clinic providing methadone treatment. Clinic experience was defined as duration that clinic had provided methadone treatment.
3.1. Statistical Analysis
Results presented as mean ± SD (standard deviation) for numeric variables and summarized by absolute frequencies and percentages for categorical variables.
A multivariable Cox proportional hazards model with forward variable selection process for exploring variables associated with retention in methadone treatment was constructed. Variables incorporated into the multivariable model were age, gender, marital status, education, employment, physical and mental illness history, previous drug treatment, polysubstance abuse, duration of opioid dependence, prison history, type of clinic (private or state clinics), average dosage of methadone and experience of clinic providing methadone treatment.
The associations were presented as hazard ratios (HRs) with 95% confidence intervals (CIs). The overall fit of the final model was checked by Cox-Snell residuals and graphical inspections were also performed to assess any departures from proportionality. To further examine, we checked the proportional hazards assumption by adding a time-dependent covariate adjusted for other covariates (32). No statistically significant violation of the assumption of proportionality was detected in multivariable analysis. Retention rate was also estimated using the Kaplan-Meier method, the standard estimator of the survival function, as univariable analyses.
For statistical analysis, statistical software SPSS version 15.0 for windows (SPSS Inc., Chicago, IL) and statistical package SAS version 9.1 for windows (SAS Institute Inc., Cary, NC, USA) were used. All p-values were 2-tailed, with statistical significance defined by P ≤ 0.05.
4. Results
4.1. Demographic Characteristics
The mean age of 1396 patients was 37.65 ± 10.77 years (ranged from 14 to 80 years). Patients' socio-demographic characteristics are detailed in Table 1.
Table 1. Socio-Demographic Characteristics of Study Sample (n = 1396).
| Variable | No. (%) |
|---|---|
| Gender | |
| Female | 86 (6.2) |
| Male | 1310 (93.8) |
| Marital Status | |
| Single | 182 (13) |
| Married | 1170 (83.8) |
| Divorced | 15 (1.1) |
| Separated | 23 (1.6) |
| Widow | 6 (0.4) |
| Residence | |
| Private | 1120 (80.2) |
| Rental | 276 (19.8) |
| Education | |
| No education | 105 (7.5) |
| Primary school | 278 (19.9) |
| Secondary school | 470 (33.7) |
| High school and Diploma | 448 (32.1) |
| College | 95 (6.8) |
| Employment | |
| Unemployed | 266 (19.1) |
| Part-time | 591 (42.3) |
| Full-time | 539 (38.6) |
| physical illness history | |
| Yes | 169 (12.1) |
| No | 1227 (87.9) |
| Mental illness history | |
| Yes | 102 (7.3) |
| No | 1294 (92.7) |
| Prison history | |
| Yes | 91 (6.5) |
| No | 1305 (93.5) |
| Duration of opioid dependence, y | |
| < 5 | 327 (23.4) |
| 6 - 10 | 394 (28.2) |
| 11 - 15 | 286 (20.5) |
| 16 - 20 | 209 (15.0) |
| > 20 | 280 (12.9) |
| Previous drug treatment | |
| No | 409 (29.3) |
| 1 - 3 times | 782 (56.0) |
| > 3 times | 205 (14.7) |
Most patients (89.6%) were treated in private clinics. The clinics experience was 1 - 5 years with an average of 1.91 ± 1.95 years. The mean daily dose for all patients was 57.06 ± 18.04 mg/day.
4.2. Patterns of Pre-Treatment Drug Abuse
The mean age at start of cigarette and opiate abuse were 21.00 ± 7.23 and 22.95 ± 8.80 years, respectively. The mean duration of opiates use was 12.17 ± 8.06 years in life time.
Opium, “Shireh” (opium juice) and heroin were the common drugs during lifetime and past 30 days prior to treatment, respectively. Oral route was the most common route of administration for using opium and “Shireh” and smoking for using heroin (Table 2).
Table 2. Patterns of Drug Abuse Prior to Treatment Among MMT Patients (n = 1396).
| Substances | Consumption Duration | No. (%) |
|---|---|---|
| Marijuana | Past 30 days | 10 (0.7) |
| In life time | 61 (4.4) | |
| Alcohol | Past 30 days | 0 |
| In life time | 64 (6.4) | |
| Opium | Past 30 days | 660 (47.3) |
| In life time | 1185 (84.9) | |
| Heroin | Past 30 days | 396 (28.4) |
| In life time | 420 (30.1) | |
| Shireh | Past 30 days | 555 (39.8) |
| (opium juice) | In life time | 718 (51.4) |
| Amphetamine | Past 30 days | 16 (1.1) |
| In life time | 18 (1.3) | |
| Methadone | Past 30 days | 65 (4.7) |
| (illegal) | In life time | 95 (6.8) |
| Hallucinogen | Past 30 days | 0 |
| In life time | 11 (0.8) | |
| Sedative | Past 30 days | 0 |
| In life time | 33 (2.4) |
4.3. Retention Rate in MMT
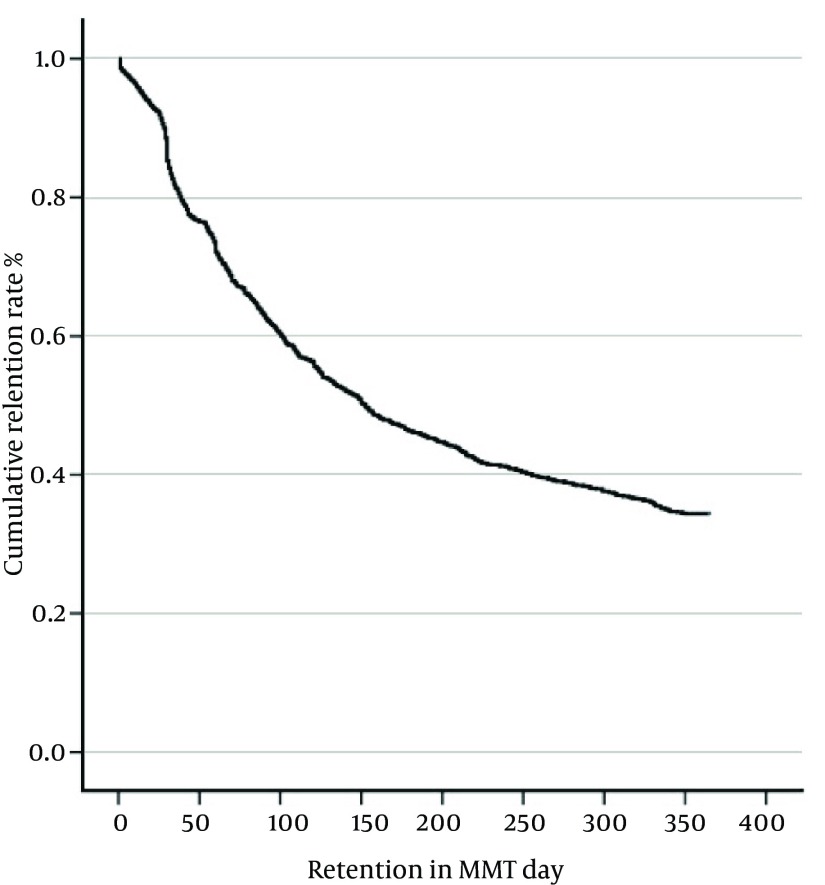
The mean and median of retention duration were 193.22 ± 3.83 and 153 ± 9.54 days, respectively. The cumulative retention rate at 3, 6 and 12 months were 66.0%, 47.3% and 34.4%, respectively. Figure 1 depicts the cumulative retention rates for study sample.
Figure 1. Kaplan- Meier Curve of Cumulative Retention Rate in Study Samples.
Cumulative retention in treatment decreased over time and over 50% of patients dropped out of treatment before 6 months and about one third of patients remained in treatment to complete the 365-day period.
4.4. Predictive Factors of One-Year Retention
In this study, predictive factors of one-year retention were examined in two groups including individual and program factors. The predictors for retention rate in the Cox proportional hazards model were high methadone dosage, polysubstance abuse and treatment under state clinics (Table 3).
Table 3. One-Year Retention Predictors in MMT Using Cox Proportional Hazards Model.
| Variable | Adjusted | ||
|---|---|---|---|
| Hazard Ratio | 95% Confidence Interval | P Value | |
| Polysubstance abuse | 0.0466 | ||
| No | 1 | - | |
| Yes | 1.268 | 1.004-1.603 | |
| Average methadone dosage (mg/day) | 1.006 | 1.001-1.011 | 0.0178 |
| Type of clinic | < 0.0001 | ||
| Private | 1 | - | |
| State | 2.101 | 1.447- 3.049 | |
5. Discussion
The results indicated that one third of the participants (34.4%) had one-year retention. There are a limited number of studies examining retention in MMT in Iran. In a multi-center study (Shiraz, Ardebil, Ilam and Semnan), three and six-month retention rates were 50% and 22.7%, respectively (29).
In the current study, one-year retention rate was lower than those from studies in Cambodia 70.7% (33), Guizhou 57.4% (34), Israel 74.4% (35), Colombia 52% (36) and Ireland 61% (37). The lower retention rate in the current study may be explained by possible differences in socio-economic and political context, clinic policy, organization of service and drug use conditions.
Results of Cox proportional hazards model indicated that one-year retention was predicted by high methadone dosage, polysubstance abuse and treatment under state clinics. Higher doses of methadone were associated with longer retention in treatment, which is consistent with prior investigations (27, 28, 38). A review of 44 methadone programs found that the dose level was the single most important factor affecting retention in treatment (39). Methadone dose is a critical factor in retaining patients in treatment (40). Higher doses were consistently shown to encourage treatment retention and reductions in illicit drug use in MMT (41).
Methadone dosage should be based on patient’s individual needs and there is no single best dose for all patients. Researchers suggest that responsive and flexible individualized dosing is associated with better retention in MMT (38, 42).
The strongest retention predictor was treatment under state clinics (Marginal clinics). The likelihood of remaining in treatment within one-year duration was higher for patients in state clinic compared to those of private clinic. There are possible explanations for this finding. One explanation may be related to costs of delivering treatment. Monthly treatment cost in private clinics is nearly three-fold as much as state clinics. Some studies found that treatment fee is associated with retention in MMT and fee-for-service methadone has poorer retention rates than free treatment (28, 43). Another explanation is that the state clinics’ clients are patients with low economical status who cannot afford opiates costs and these patients are forced to remain more in treatment and have more retention, not because of medical motivation but due to financial inability in affording opiates.
Retention rates were further predicted by polysubstance abuse. This study revealed that patients who abused polysubstances are more likely to remain in treatment at one year compared to those who abused a single substance before entering MMT. This finding is inconsistent with some other studies (18, 44). Another study showed that patients who abuse a single substance (only opium) were less motivated for treatment and as early leaving treatment (45). A prior study indicated that an important predictor of early dropout was lower motivation for treatment (46).
Finally, although the study sample was large, it may not be representative of all MMT retention in different regions of Iran. Therefore, more studies are needed from different parts of the country.
5.1. Conclusion
In summary, the present study showed that retention rate is lower compared to studies in other countries. The results showed that program related factors are better predictors of retention than individual related factors.
Given the importance of program related factors on retention, policies and practices that influence retention such as reducing treatment costs and prescribing appropriate methadone dosage, may yield better outcomes.
Acknowledgments
This research was supported by Rafsanjan University of Medical Sciences (RUMS). The authors wish to thank the staff of MMT clinics of Rafsanjan.
Footnotes
Authors’ Contribution:Study concept and design: Rezaeian, Sheikh Fathollahi, Torkashvand and Najmeddin; analysis and interpretation of data: Rezaeian, Torkashvand and Sheikh Fathollahi; drafting of the manuscript: Torkashvand; critical revision of the manuscript for important intellectual content: Sheikh Fathollahi, Rezaeian and Najmeddin; statistical analysis: Sheikh Fathollahi and Torkashvand.
Funding/Support:This study was supported by a grant from Rafsanjan University of Medical Sciences (RUMS)
References
- 1.Dole VP, Nyswander ME. Rehabilitation of heroin addicts after blockade with methadone. N Y State J Med. 1966;66(15):2011–7. [PubMed] [Google Scholar]
- 2.Ball JC, Ross A. The effectiveness of methadone maintenance treatment: Patients, programs, services, and outcome. USA: Springer-Verlag Publishing; 1991. [Google Scholar]
- 3.Clausen T, Anchersen K, Waal H. Mortality prior to, during and after opioid maintenance treatment (OMT): a national prospective cross-registry study. Drug Alcohol Depend. 2008;94(1-3):151–7. doi: 10.1016/j.drugalcdep.2007.11.003. [DOI] [PubMed] [Google Scholar]
- 4.Strike CJ, Gnam W, Urbanoski K, Fischer B, Marsh DC, Millson M. Factors predicting 2-year retention in methadone maintenance treatment for opioid dependence. Addict Behav. 2005;30(5):1025–8. doi: 10.1016/j.addbeh.2004.09.004. [DOI] [PubMed] [Google Scholar]
- 5.Des Jarlais DC, Joseph H, Dole VP. Long-term outcomes after termination from methadone maintenance treatment. Ann N Y Acad Sci. 1981;362:231–8. doi: 10.1111/j.1749-6632.1981.tb12812.x. [DOI] [PubMed] [Google Scholar]
- 6.Simpson DD. The relation of time spent in drug abuse treatment to posttreatment outcome. Am J Psychiatry. 1979;136(11):1449–53. doi: 10.1176/ajp.136.11.1449. [DOI] [PubMed] [Google Scholar]
- 7.Caplehorn JR, Dalton MS, Cluff MC, Petrenas AM. Retention in methadone maintenance and heroin addicts' risk of death. Addiction. 1994;89(2):203–9. doi: 10.1111/j.1360-0443.1994.tb00879.x. [DOI] [PubMed] [Google Scholar]
- 8.Peles E, Schreiber S, Adelson M. Variables associated with perceived sleep disorders in methadone maintenance treatment (MMT) patients. Drug Alcohol Depend. 2006;82(2):103–10. doi: 10.1016/j.drugalcdep.2005.08.011. [DOI] [PubMed] [Google Scholar]
- 9.Zhang Z, Friedmann PD, Gerstein DR. Does retention matter? Treatment duration and improvement in drug use. Addiction. 2003;98(5):673–84. doi: 10.1046/j.1360-0443.2003.00354.x. [DOI] [PubMed] [Google Scholar]
- 10.Hubbard RL, Craddock SG, Anderson J. Overview of 5-year followup outcomes in the drug abuse treatment outcome studies (DATOS). J Subst Abuse Treat. 2003;25(3):125–34. doi: 10.1016/s0740-5472(03)00130-2. [DOI] [PubMed] [Google Scholar]
- 11.Darke S, Ross J, Teesson M, Ali R, Cooke R, Ritter A, et al. Factors associated with 12 months continuous heroin abstinence: findings from the Australian Treatment Outcome Study (ATOS). J Subst Abuse Treat. 2005;28(3):255–63. doi: 10.1016/j.jsat.2005.01.006. [DOI] [PubMed] [Google Scholar]
- 12.Fareed A, Casarella J, Amar R, Vayalapalli S, Drexler K. Benefits of retention in methadone maintenance and chronic medical conditions as risk factors for premature death among older heroin addicts. J Psychiatr Pract. 2009;15(3):227–34. doi: 10.1097/01.pra.0000351884.83377.e2. [DOI] [PubMed] [Google Scholar]
- 13.Simpson DD, Joe GW, Rowan-Szal GA. Drug abuse treatment retention and process effects on follow-up outcomes. Drug Alcohol Depend. 1997;47(3):227–35. doi: 10.1016/s0376-8716(97)00099-9. [DOI] [PubMed] [Google Scholar]
- 14.Simpson D, Sells S. Effectiveness of treatment for drug abuse: an overview of the DARP research program. Adv Alcohol Subst Abuse. 1982;2(1):7–29. [Google Scholar]
- 15.Simpson DD, Joe GW, Bracy SA. Six-year follow-up of opioid addicts after admission to treatment. Arch Gen Psychiatry. 1982;39(11):1318–23. doi: 10.1001/archpsyc.1982.04290110070012. [DOI] [PubMed] [Google Scholar]
- 16.Mancino M, Curran G, Han X, Allee E, Humphreys K, Booth BM. Predictors of attrition from a national sample of methadone maintenance patients. Am J Drug Alcohol Abuse. 2010;36(3):155–60. doi: 10.3109/00952991003736389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sarasvita R, Tonkin A, Utomo B, Ali R. Predictive factors for treatment retention in methadone programs in Indonesia. J Subst Abuse Treat. 2012;42(3):239–46. doi: 10.1016/j.jsat.2011.07.009. [DOI] [PubMed] [Google Scholar]
- 18.Magura S, Nwakeze PC, Demsky SY. Pre- and in-treatment predictors of retention in methadone treatment using survival analysis. Addiction. 1998;93(1):51–60. doi: 10.1046/j.1360-0443.1998.931516.x. [DOI] [PubMed] [Google Scholar]
- 19.Deck D, Carlson MJ. Retention in publicly funded methadone maintenance treatment in two Western States. J Behav Health Serv Res. 2005;32(1):43–60. doi: 10.1007/BF02287327. [DOI] [PubMed] [Google Scholar]
- 20.Hser YI, Evans E, Huang D, Anglin DM. Relationship between drug treatment services, retention, and outcomes. Psychiatr Serv. 2004;55(7):767–74. doi: 10.1176/appi.ps.55.7.767. [DOI] [PubMed] [Google Scholar]
- 21.Saxon AJ, Wells EA, Fleming C, Jackson TR, Calsyn DA. Pre-treatment characteristics, program philosophy and level of ancillary services as predictors of methadone maintenance treatment outcome. Addiction. 1996;91(8):1197–209. doi: 10.1046/j.1360-0443.1996.918119711.x. [DOI] [PubMed] [Google Scholar]
- 22.Friedmann PD, Lemon SC, Stein MD. Transportation and retention in outpatient drug abuse treatment programs. J Subst Abuse Treat. 2001;21(2):97–103. doi: 10.1016/s0740-5472(01)00185-4. [DOI] [PubMed] [Google Scholar]
- 23.Hiltunen AJ, Eklund C. Withdrawal from methadone maintenance treatment. Reasons for not trying to quit methadone. Eur Addict Res. 2002;8(1):38–44. doi: 10.1159/000049486. [DOI] [PubMed] [Google Scholar]
- 24.Sorensen JL, Gibson D, Bernal G, Deitch D. Methadone applicant dropouts: impact of requiring involvement of friends or family in treatment. Int J Addict. 1985;20(8):1273–80. doi: 10.3109/10826088509056363. [DOI] [PubMed] [Google Scholar]
- 25.Grella CE, Wugalter SE, Anglin MD. Predictors of treatment retention in enhanced and standard methadone maintenance treatment for HIV risk reduction. J Drug Issues. 1997;27:203–24. [Google Scholar]
- 26.Wimbush J, Amicarelli A, Stein MD. Does HIV test result influence methadone maintenance treatment retention? J Subst Abuse. 1996;8(2):263–9. doi: 10.1016/s0899-3289(96)90304-1. [DOI] [PubMed] [Google Scholar]
- 27.Kelly SM, O'Grady KE, Mitchell SG, Brown BS, Schwartz RP. Predictors of methadone treatment retention from a multi-site study: a survival analysis. Drug Alcohol Depend. 2011;117(2-3):170–5. doi: 10.1016/j.drugalcdep.2011.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Booth RE, Corsi KF, Mikulich-Gilbertson SK. Factors associated with methadone maintenance treatment retention among street-recruited injection drug users. Drug Alcohol Depend. 2004;74(2):177–85. doi: 10.1016/j.drugalcdep.2003.12.009. [DOI] [PubMed] [Google Scholar]
- 29.Shirinbayan P, Rafiey H, VejdaniRoshan A, Narenjiha H, Farhoudian A. Predictors of retention in methadone maintenance therapy: A prospective multi-center study. Sci Res Essay . 2010;5(21):3231–6. [Google Scholar]
- 30.Dobkin PL, De CM, Paraherakis A, Gill K. The role of functional social support in treatment retention and outcomes among outpatient adult substance abusers. Addiction. 2002;97(3):347–56. doi: 10.1046/j.1360-0443.2002.00083.x. [DOI] [PubMed] [Google Scholar]
- 31.Brown BS, O'Grady KE, Battjes RJ, Katz EC. The Community Assessment Inventory--client views of supports to drug abuse treatment. J Subst Abuse Treat. 2004;27(3):241–51. doi: 10.1016/j.jsat.2004.08.002. [DOI] [PubMed] [Google Scholar]
- 32.Klein J, Moeschberger M. Survival analysis: statistical methods for censored and truncated data. New York: Springer-Verlag; 2003. [Google Scholar]
- 33.Phallyka C. Prospective cohort study of factors associated with retention of methadone maintenance therapy among patients at the center for mental health and drug dependence in Cambodia. Japan: Ritsumeikan Asia Pacific university; 2012. [Google Scholar]
- 34.Liu E, Liang T, Shen L, Zhong H, Wang B, Wu Z, et al. Correlates of methadone client retention: a prospective cohort study in Guizhou province, China. Int J Drug Policy. 2009;20(4):304–8. doi: 10.1016/j.drugpo.2008.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Peles E, Schreiber S, Adelson M. 15-Year survival and retention of patients in a general hospital-affiliated methadone maintenance treatment (MMT) center in Israel. Drug Alcohol Depend. 2010;107(2-3):141–8. doi: 10.1016/j.drugalcdep.2009.09.013. [DOI] [PubMed] [Google Scholar]
- 36.Anderson JF, Warren LD. Client retention in the British Columbia Methadone Program, 1996-1999. Can J Public Health. 2004;95(2):104–9. doi: 10.1007/BF03405776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mullen L, Barry J, Long J, Keenan E, Mulholland D, Grogan L, et al. A national study of the retention of Irish opiate users in methadone substitution treatment. Am J Drug Alcohol Abuse. 2012;38(6):551–8. doi: 10.3109/00952990.2012.694516. [DOI] [PubMed] [Google Scholar]
- 38.Bao YP, Liu ZM, Epstein DH, Du C, Shi J, Lu L. A meta-analysis of retention in methadone maintenance by dose and dosing strategy. Am J Drug Alcohol Abuse. 2009;35(1):28–33. doi: 10.1080/00952990802342899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Joseph H, Stancliff S, Langrod J. Methadone maintenance treatment (MMT): a review of historical and clinical issues. Mt Sinai J Med. 2000;67(5-6):347–64. [PubMed] [Google Scholar]
- 40.D'Ippoliti D, Davoli M, Perucci CA, Pasqualini F, Bargagli AM. Retention in treatment of heroin users in Italy: the role of treatment type and of methadone maintenance dosage. Drug Alcohol Depend. 1998;52(2):167–71. doi: 10.1016/s0376-8716(98)00091-x. [DOI] [PubMed] [Google Scholar]
- 41.Ward J, Mattick RP, Hall W. Methadone Maintenance Treatment and Other Opioid Replacement Therapies. United Kingdom: Harwood Academic Publishers; 1997. [Google Scholar]
- 42.Leavitt SB, Shinderman M, Maxwell S, Eap CB, Paris P. When "enough" is not enough: new perspectives on optimal methadone maintenance dose. Mt Sinai J Med. 2000;67(5-6):404–11. [PubMed] [Google Scholar]
- 43.Maddux JF, Prihoda TJ, Desmond DP. Treatment fees and retention on methadone maintenance. J Drug Issues. 1994;24(3):429–43. [Google Scholar]
- 44.Magruder KM, Bichun O, Miller S, Tilley BC. Retention of under-represented minorities in drug abuse treatment studies. Clin Trials. 2009;6(3):252–60. doi: 10.1177/1740774509105224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Karimi Talabari Z, Noori Khajavi M, Rafiei H. Reasons of Methadone Maintenance Therapy Drop out in Clients of Iranian National Center for Addiction Studies (INCAS): A Qualitative Study. Iranian J Psychiatr Clin Psychol. 2013;18(4):299–309. [Google Scholar]
- 46.McKellar J, Kelly J, Harris A, Moos R. Pretreatment and during treatment risk factors for dropout among patients with substance use disorders. Addict Behav. 2006;31(3):450–60. doi: 10.1016/j.addbeh.2005.05.024. [DOI] [PubMed] [Google Scholar]