Abstract
Background
The Ryan White HIV/AIDS Program (RWHAP) provides persons infected with human immunodeficiency virus (HIV) with services not covered by other healthcare payer types. Limited data exist to inform policy decisions about the most appropriate role for RWHAP under the Patient Protection and Affordable Care Act (ACA).
Methods
We assessed associations between RWHAP assistance and antiretroviral therapy (ART) prescription and viral suppression. We used data from the Medical Monitoring Project, a surveillance system assessing characteristics of HIV-infected adults receiving medical care in the United States. Interview and medical record data were collected in 2009–2013 from 18 095 patients.
Results
Nearly 41% of patients had RWHAP assistance; 15% relied solely on RWHAP assistance for HIV care. Overall, 91% were prescribed ART, and 75% were virally suppressed. Uninsured patients receiving RWHAP assistance were significantly more likely to be prescribed ART (52% vs 94%; P < .01) and virally suppressed (39% vs 77%; P < .01) than uninsured patients without RWHAP assistance. Patients with private insurance and Medicaid were 6% and 7% less likely, respectively, to be prescribed ART than those with RWHAP only (P < .01). Those with private insurance and Medicaid were 5% and 12% less likely, respectively, to be virally suppressed (P ≤ .02) than those with RWHAP only. Patients whose private or Medicaid coverage was supplemented by RWHAP were more likely to be prescribed ART and virally suppressed than those without RWHAP supplementation (P ≤ .01).
Conclusions
Uninsured and underinsured HIV-infected persons receiving RWHAP assistance were more likely to be prescribed ART and virally suppressed than those with other types of healthcare coverage.
Keywords: Ryan White, HIV, health insurance, viral suppression, antiretroviral therapy
Human immunodeficiency virus (HIV) causes a chronic infection, which without treatment leads to AIDS, substantial morbidity, and premature death. Treatment of HIV infection with antiretroviral therapy (ART) to achieve viral suppression reduces morbidity, mortality, and risk of HIV transmission [1, 2]. For 25 years, the Ryan White HIV/AIDS Program (RWHAP) has been the payer of last resort for uninsured and underinsured HIV-infected persons in the United States, providing outpatient medical care, medications, and supportive services that are otherwise inaccessible to these individuals [3].
RWHAP provides assistance with HIV medical care through several mechanisms. RWHAP provides funding for medical services directly to HIV care facilities, and previous research suggests these facilities perform favorably to other facilities providing HIV medical care [4–8]. RWHAP also provides assistance with HIV medical care for persons who are uninsured or have incomplete coverage for HIV-related medications and services [9], but less is known about the impact of this assistance. Grants may be used to pay individuals’ insurance premiums or deductibles for other types of healthcare coverage or to provide nonmedical supportive services (eg, case management, adherence support, transportation assistance, etc.) to HIV-infected persons.
Under the Patient Protection and Affordable Care Act (ACA), many HIV-infected persons are eligible for Medicaid coverage or private insurance through health insurance marketplaces [10]. Questions remain about the most appropriate role for RWHAP given expanded options for healthcare coverage [11, 12]. Thus, a better understanding of HIV treatment outcomes among persons with and without RWHAP assistance is needed. Using data from the Medical Monitoring Project (MMP), a nationally representative sample of HIV-infected adults receiving medical care, we assessed the association between RWHAP assistance, alone and in combination with other sources of healthcare coverage, and prescription of ART and viral suppression.
METHODS
MMP is a surveillance system designed to produce nationally representative, cross-sectional estimates of behavioral and clinical characteristics of HIV-infected adults receiving medical care in the United States [13]. MMP utilizes a 3-stage, complex sampling design in which US states and territories are sampled, followed by facilities providing outpatient HIV medical care in those jurisdictions, then HIV-infected adults (aged 18 years and older) receiving care in those facilities. We used MMP data collected from adults with at least 1 HIV medical care visit to participating facilities during January to April of each of 4 years: 2009, 2010, 2011, and 2012. Data were collected from June 2009 through May 2013 using face-to-face patient interviews and medical record abstractions.
All sampled states and territories participated in MMP. Facility response rates ranged from 76% to 85% from 2009 to 2012. Approximately 50% of persons sampled from these facilities completed an interview and had their medical records abstracted. Data were weighted to account for unequal probabilities of selection and both facility and patient nonresponse. Characteristics of nonresponding facilities and patients were available through program and surveillance data. These data were used to weight MMP data based on predictors of nonresponse.
In accordance with the federal human subjects protection regulations at 45 Code of Federal Regulations 46.101c and 46.102d [14] and with the Guidelines for Defining Public Health Research and Public Health Non-Research [15], MMP was determined to be a nonresearch, public health surveillance activity used for disease control program or policy purposes. As such, MMP is not subject to federal investigational review board review. Participating states or territories and facilities obtained local institutional review board approval to conduct MMP if required locally. Informed consent was obtained from all interviewed participants.
We examined the association between RWHAP assistance and 2 analytic outcomes measured using information from participants’ medical records: prescription of ART, defined as having a documented ART prescription during the 12 months prior to interview, and viral suppression, defined as having a suppressed HIV viral load (undetectable or <200 copies/mL) at last measurement. The independent variable of interest, healthcare payer type, includes RWHAP assistance as well as other sources of healthcare coverage. Payer type was ascertained through interviews, in which participants were asked about type(s) of health insurance or coverage they had and sources of financial assistance for ART. Participants could list multiple types of healthcare coverage and/or sources of financial support for ART, and they could list payer types either by name or generically. For example, patients could name a payer type as either Medicaid or their state’s local Medicaid program (ie, Medi-Cal in California). Responses were recoded accordingly for all payer types, including RWHAP, and then combined into a single indicator that accounts for all major, observed combinations of payer types.
We conducted 3 comparisons with regard to ART and viral suppression: (1) patients with RWHAP only compared to uninsured patients not receiving RWHAP assistance, (2) patients with RWHAP only compared to patients with other source(s) of healthcare coverage, and (3) patients with healthcare coverage supplemented by RWHAP assistance compared to patients with other healthcare coverage alone.
First, we estimated the percentage of patients with each payer type and compared patients by payer type by other characteristics, ART prescription, and viral suppression. We used the following simplified categories for payer type: RWHAP assistance only; other healthcare coverage only; other healthcare coverage + RWHAP assistance; and uninsured, not receiving RWHAP assistance. We also compared patients by the aforementioned, more detailed payer categories (Supplementary Table 1). Patient characteristics included descriptors elicited by interview (gender, age, race/ethnicity, nativity, education level, poverty status, homelessness status, and time since HIV diagnosis) and by medical record abstraction (HIV disease stage). We categorized stage of HIV disease as stage 1 (no AIDS and nadir CD4 + T-lymphocyte cell (CD4) count ≥500 cells/mm3), stage 2 (no AIDS and nadir CD4 count 200–499 cells/mm3), or stage 3 (AIDS or nadir CD4 count <200 cells/mm3) [16]. Nadir CD4 count was defined as the lowest CD4 cell count measured after HIV diagnosis.
Next, we separately estimated the proportion of patients prescribed ART and who were virally suppressed by patient characteristics including payer type. Global F-tests were used to test for statistical significance of the associations between patient characteristics, including payer type, and each outcome.
Using participants with RWHAP only as a reference group, we estimated unadjusted and adjusted prevalence ratios by payer type for the 2 outcomes. To estimate adjusted prevalence ratios, we first constructed a multivariate logistic regression model for each outcome. Potential confounders that were associated with payer type and the outcome in question at P ≤ .10 were added to the model using forward stepwise selection. We used this model to estimate average marginal predictions, or the average of predicted probabilities across a group (eg, 18–29 year-olds), accounting for the distribution of other covariates in that group. Adjusted prevalence ratios were then estimated by calculating the ratio of one predicted probability to another. We combined the ‘other public,’ ‘other public + RWHAP,’ and ‘VA/CHAMPUS/Tricare’ categories with the ‘other’ category, because the sizes of these groups were too small for multivariate analysis.
Finally, for each outcome, we examined associations between having healthcare coverage (private, Medicaid, Medicare, Medicare + Medicaid) supplemented by RWHAP assistance to having the same type of healthcare coverage alone. We used results from the multivariate models to compare the adjusted predicted probability of either being prescribed ART or being virally suppressed with healthcare coverage supplemented by RWHAP assistance vs the same type of healthcare coverage alone.
We accounted for the complex survey design in all analyses, estimating standard errors of the estimates using Taylor linearization. All percentages represent weighted percentages. Stata 12 was used for all analyses (StataCorp. 2011. Stata Statistical Software: Release 12. College Station, Texas).
FINDINGS
Of the 18 095 participants, 46 (0.3%) were missing data for payer type, resulting in an analytic sample of 18 049 (Table 1). In all, 40.7% of HIV-infected adults in medical care received RWHAP assistance, including15.3% who relied solely on RWHAP for HIV care and 25.4% who relied on RWHAP in combination with other healthcare coverage. Nearly 57% of patients had other healthcare coverage only, including private insurance (17.0%), Medicaid (15.9%), Medicare (3.4%), or both (9.4%). Only 2.7% of patients were uninsured, not receiving RWHAP assistance.
Table 1.
Percentagea of Patients by Healthcare Payer Type: By Patient Characteristics, Medical Monitoring Project, 2009–2013 (n = 18 049)
| Total Sample | Healthcare Coverage 56.5% of Total (95% CI, 54.6–58.4) | Healthcare Coverage + RWHAP Assistance 25.4% of Total (95% CI, 23.5–27.3) | RWHAP Assistance Only 15.3% of Total (95% CI, 13.1–17.6) | Uninsured, no RWHAP Assistance 2.7% of Total (95% CI, 2.1–3.3) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | ||||||
| Healthcare payer type | ||||||||||||||||
| RWHAP only | 2581 | 15.3 | 13.1 | 17.6 | 100.0 | … | … | |||||||||
| Private | 2882 | 17.0 | 14.8 | 19.1 | 30.0 | 26.6 | 33.7 | |||||||||
| Medicaid | 2905 | 15.9 | 14.3 | 17.6 | 28.2 | 25.3 | 31.1 | |||||||||
| Medicare | 634 | 3.4 | 2.9 | 3.8 | 5.9 | 5.2 | 6.8 | |||||||||
| Medicaid + Medicare | 1619 | 9.4 | 8.3 | 10.5 | 16.7 | 14.7 | 18.9 | |||||||||
| Other public | 446 | 1.6 | .3 | 2.9 | 2.9 | 1.3 | 6.2 | |||||||||
| Private + RWHAP | 944 | 5.2 | 4.6 | 5.8 | 20.6 | 18.3 | 23.1 | |||||||||
| Medicaid+RWHAP | 1087 | 5.5 | 4.3 | 6.6 | 21.5 | 16.6 | 27.2 | |||||||||
| Medicare+RWHAP | 625 | 3.4 | 2.8 | 4.1 | 13.5 | 11.2 | 16.2 | |||||||||
| Medicaid+Medicare+RWHAP | 764 | 4.2 | 3.5 | 4.9 | 16.5 | 13.5 | 19.9 | |||||||||
| Other public + RWHAP | 539 | 2.5 | 1.4 | 3.5 | 9.7 | 6.6 | 13.8 | |||||||||
| VA/Champus/Tricareb | 353 | 1.8 | 1.0 | 2.7 | 3.0 | 1.9 | 4.9 | .5 | .3 | .8 | ||||||
| Other payer typeb | 2181 | 12.1 | 9.9 | 14.2 | 13.3 | 11.6 | 15.2 | 17.8 | 13.5 | 23.1 | ||||||
| Uninsured | 489 | 2.7 | 2.1 | 3.3 | 100.0 | … | … | |||||||||
| Gender | ||||||||||||||||
| Male | 13 025 | 72.4 | 70.0 | 74.8 | 70.3 | 67.5 | 73.1 | 76.0 | 72.6 | 79.4 | 74.8 | 72.5 | 77.1 | 68.2 | 63.4 | 73.0 |
| Female | 4772 | 26.3 | 23.9 | 28.6 | 28.6 | 25.9 | 31.4 | 22.6 | 19.2 | 26.0 | 23.0 | 20.9 | 25.1 | 29.9 | 24.9 | 34.9 |
| Transgender/Intersex | 246 | 1.3 | 1.1 | 1.6 | 1.1 | .8 | 1.3 | 1.4 | 1.0 | 1.7 | 2.2 | 1.6 | 2.7 | 1.9 | .6 | 3.2 |
| Age (years) | ||||||||||||||||
| 18–29 | 1336 | 7.6 | 6.8 | 8.3 | 5.6 | 4.9 | 6.3 | 6.9 | 5.6 | 8.2 | 14.1 | 12.3 | 15.9 | 18.3 | 13.4 | 23.2 |
| 30–39 | 2834 | 16.0 | 15.3 | 16.7 | 13.6 | 12.9 | 14.4 | 15.3 | 13.9 | 16.6 | 23.6 | 21.8 | 25.4 | 28.8 | 23.9 | 33.6 |
| 40–49 | 6380 | 35.1 | 34.3 | 35.9 | 34.7 | 33.5 | 35.8 | 35.1 | 33.4 | 36.8 | 37.1 | 35.1 | 39.2 | 32.4 | 27.4 | 37.4 |
| ≥50 | 7499 | 41.3 | 40.5 | 42.2 | 46.1 | 44.8 | 47.4 | 42.8 | 40.2 | 45.4 | 25.2 | 23.0 | 27.3 | 20.5 | 17.0 | 24.0 |
| Race/Ethnicity | ||||||||||||||||
| non-Hispanic black | 7457 | 41.3 | 34.7 | 48.0 | 41.4 | 34.6 | 48.2 | 36.7 | 27.7 | 45.8 | 46.5 | 41.2 | 51.9 | 53.7 | 47.1 | 60.4 |
| non-Hispanic white | 5887 | 34.5 | 29.3 | 39.7 | 35.7 | 30.1 | 41.3 | 40.9 | 33.4 | 48.4 | 22.5 | 19.9 | 25.1 | 16.4 | 12.6 | 20.1 |
| Hispanic | 3876 | 19.3 | 15.2 | 23.5 | 18.1 | 13.3 | 23.0 | 17.3 | 12.7 | 21.8 | 26.2 | 21.4 | 31.0 | 25.5 | 20.3 | 30.7 |
| Other | 829 | 4.8 | 4.1 | 5.5 | 4.7 | 3.9 | 5.5 | 5.1 | 4.0 | 6.2 | 4.8 | 3.8 | 5.7 | 4.4 | 2.3 | 6.5 |
| Nativity | ||||||||||||||||
| US-born | 15 663 | 86.6 | 85.1 | 88.1 | 90.4 | 88.9 | 91.8 | 88.7 | 86.9 | 90.4 | 71.6 | 66.5 | 76.7 | 73.4 | 66.5 | 80.2 |
| Foreign-born | 2379 | 13.4 | 11.9 | 14.9 | 9.6 | 8.2 | 11.1 | 11.3 | 9.6 | 13.1 | 28.4 | 23.3 | 33.5 | 26.6 | 19.8 | 33.5 |
| Education | ||||||||||||||||
| Less than high school | 3958 | 21.0 | 19.1 | 22.8 | 21.9 | 19.8 | 24.1 | 17.5 | 14.6 | 20.4 | 22.4 | 20.5 | 24.3 | 25.9 | 21.1 | 30.7 |
| High school graduatec | 4924 | 27.0 | 25.4 | 28.6 | 25.8 | 24.3 | 27.2 | 26.7 | 24.1 | 29.3 | 31.1 | 28.7 | 33.5 | 32.3 | 27.9 | 36.7 |
| Some college or more | 9160 | 52.0 | 48.9 | 55.2 | 52.3 | 49.0 | 55.6 | 55.8 | 50.8 | 60.9 | 46.5 | 43.8 | 49.2 | 41.9 | 36.7 | 47.0 |
| Poverty statusd | ||||||||||||||||
| Above poverty level | 9418 | 55.8 | 52.8 | 58.8 | 56.5 | 52.6 | 60.3 | 60.0 | 57.2 | 62.8 | 47.9 | 45.0 | 50.8 | 44.8 | 39.9 | 49.7 |
| At or below poverty level | 8033 | 44.2 | 41.2 | 47.2 | 43.5 | 39.7 | 47.4 | 40.0 | 37.2 | 42.8 | 52.1 | 49.2 | 55.0 | 55.2 | 50.3 | 60.1 |
| Homeless (past 12 mo)e | ||||||||||||||||
| Yes | 1510 | 8.2 | 7.6 | 8.9 | 7.5 | 6.7 | 8.3 | 8.1 | 7.0 | 9.1 | 10.2 | 8.3 | 12.2 | 13.0 | 10.4 | 15.6 |
| No | 16 538 | 91.8 | 91.1 | 92.4 | 92.5 | 91.7 | 93.3 | 91.9 | 90.9 | 93.0 | 89.8 | 87.8 | 91.7 | 87.0 | 84.4 | 89.6 |
| Time since HIV diagnosis | ||||||||||||||||
| <5 y | 3772 | 22.1 | 21.1 | 23.1 | 18.8 | 17.6 | 19.9 | 20.2 | 18.7 | 21.7 | 33.2 | 30.8 | 35.6 | 46.6 | 41.4 | 51.7 |
| 5–9 y | 3851 | 21.3 | 20.6 | 22.0 | 20.2 | 19.3 | 21.1 | 20.3 | 19.1 | 21.4 | 25.8 | 23.7 | 27.8 | 26.3 | 22.6 | 30.1 |
| 10+ years | 10 416 | 56.6 | 55.3 | 58.0 | 61.0 | 59.5 | 62.5 | 59.5 | 57.7 | 61.4 | 41.1 | 38.9 | 43.2 | 27.1 | 23.0 | 31.2 |
| HIV disease stagef | ||||||||||||||||
| Stage 1: No AIDS and nadir CD4 ≥500 (or CD4% ≥29) | 1203 | 7.0 | 6.5 | 7.5 | 7.3 | 6.6 | 7.9 | 5.7 | 4.7 | 6.6 | 6.6 | 5.5 | 7.6 | 15.7 | 11.9 | 19.6 |
| Stage 2: No AIDS and nadir CD4 200–499 (or CD4% 14–<29) | 4310 | 24.4 | 23.5 | 25.3 | 23.7 | 22.4 | 24.9 | 20.3 | 18.4 | 22.2 | 31.0 | 28.9 | 33.0 | 39.5 | 34.2 | 44.8 |
| Stage 3: AIDS or nadir CD4 0–199 (or CD4% <14) | 12 469 | 68.7 | 67.7 | 69.6 | 69.1 | 67.7 | 70.4 | 74.0 | 71.6 | 76.5 | 62.5 | 60.3 | 64.6 | 44.7 | 38.3 | 51.1 |
| Prescribed ARTg (%) | ||||||||||||||||
| Yes | 16 495 | 91.1 | 90.6 | 91.7 | 90.3 | 89.6 | 91.0 | 95.4 | 94.4 | 96.4 | 94.2 | 92.8 | 95.5 | 52.1 | 46.0 | 58.2 |
| No | 1554 | 8.9 | 8.3 | 9.4 | 9.7 | 9.0 | 10.4 | 4.6 | 3.6 | 5.6 | 5.8 | 4.5 | 7.2 | 47.9 | 41.8 | 54.0 |
| HIV viral load undetectable or <200 copies/mL (%) Yes |
13 530 | 74.7 | 73.5 | 76.0 | 74.3 | 72.8 | 75.8 | 78.4 | 76.8 | 80.0 | 76.7 | 74.5 | 78.8 | 38.8 | 33.7 | 43.9 |
| No | 4519 | 25.3 | 24.0 | 26.5 | 25.7 | 24.2 | 27.2 | 21.6 | 20.0 | 23.2 | 23.3 | 21.2 | 25.5 | 61.2 | 56.1 | 66.3 |
| Total | 18 095 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | ||||||||||
Abbreviations: ART, antiretroviral therapy; CI, confidence interval; HIV, human immunodeficiency virus; RWHAP, Ryan White HIV/AIDS Program.
Percentages and 95% CIs are weighted to account for unequal selection probabilities and non-response.
Some patients with this payer type also received RWHAP assistance.
Includes general education development (GED) credential.
US Department of Health and Human Services. HHS Poverty Guidelines. Available at: http://aspe.hhs.gov/poverty/09poverty.shtml.
McKinney-Vento definition of homelessness: living on the street, living in a shelter, living in a single-room-occupancy hotel, temporarily staying with friends or family, or living in a car. A person is categorized as homeless if that person lacks a fixed, regular, adequate night-time residence or has a steady night-time residence that is 1) a supervised publicly or privately operated shelter designed to provide temporary living accommodation, 2) an institution that provides a temporary residence for persons intended to be institutionalized, or 3) a public or private place not designed for or ordinarily used as a regular sleeping accommodation for human beings (eg, in an automobile or under a bridge) (Stewart B. McKinney Homeless Assistance Act, 42 U.S.C. §11301, et seq; 1987).
Schneider E, Whitmore S, Glynn KM, et al Revised surveillance case definitions for HIV infection among adults, adolescents, and children aged <18 months and for HIV infection and AIDS among children aged 18 months to <13 years—United States, 2008. MMWR. Recommendations and reports : Morbidity and mortality weekly report. Recommendations and reports/Centers for Disease Control. Dec 5 2008; 57(RR-10):1–12.
Documented ART prescription in the medical record during the 12 months prior to interview.
Among HIV-infected adults in medical care, 72.4% were male, 76.4% were at least 40 years old, 41.3% were non-Hispanic black, 34.5% were non-Hispanic white, and 19.3% were Hispanic. Nearly 52.0% had more than a high school education, 44.2% lived at or below the federal poverty level [17, 18], and 8.2% had been homeless (McKinney-Vento definition of homelessness: living on the street, living in a shelter, living in a single-room-occupancy hotel, temporarily staying with friends or family, or living in a car. A person is categorized as homeless if that person lacks a fixed, regular, adequate night-time residence or has a steady night-time residence that is 1) a supervised publicly or privately operated shelter designed to provide temporary living accommodation, 2) an institution that provides a temporary residence for persons intended to be institutionalized, or 3) a public or private place not designed for or ordinarily used as a regular sleeping accommodation for human beings [eg, in an automobile or under a bridge] [Stewart B. McKinney Homeless Assistance Act, 42 U.S.C. §11 301, et seq; 1987]) in the past 12 months. Over half (56.6%) had been diagnosed with HIV for at least 10 years, and 68.7% had ever had stage 3 disease. Overall, 91.1% of patients were prescribed ART, and 74.7% were virally suppressed.
All patient characteristics varied significantly by payer type (P ≤ .01 for all characteristics). Uninsured patients with or without RWHAP assistance were younger and more likely to have household incomes at or below the federal poverty level, have been homeless during the past 12 months, and have been diagnosed with HIV for 5 years or fewer than patients with other types of coverage.
Patients with RWHAP Only Compared to Uninsured Patients not receiving RWHAP Assistance
Among patients with RWHAP only, 94.2% were prescribed ART, compared to 52.1% of those who were uninsured, not receiving RWHAP assistance (P < .01) (Table 1). Similarly, 76.7% of patients with RWHAP only were virally suppressed, compared to 38.8% of those uninsured, not receiving RWHAP assistance (P < .01).
Patients with RWHAP Only Compared to Patients with Other Healthcare Coverage
To assess how payer type was associated with ART prescription and viral suppression, we excluded uninsured patients not receiving RWHAP assistance, resulting in an analytic sample of 17 560.
Among patients with some payer type for HIV medical care, payer type was associated with having been prescribed ART and viral suppression (Table 2). Of patients with RWHAP only, 94.2% were prescribed ART, and 76.7% were virally suppressed. Patients with Medicare + RWHAP (96.3%) or Medicaid + Medicare + RWHAP (96.4%) were most likely to be prescribed ART, whereas those with private (88.5%), Medicaid (88.8%) or other public coverage (88.7%) were least likely. Patients with private + RWHAP (82.4%) or Medicare + RWHAP (82.2%) were most likely to be virally suppressed, and those with Medicaid (65.7%) or Medicaid + RWHAP (70.4%) were least likely. Prescription of ART and viral suppression were also associated with other patient characteristics.
Table 2.
Percentagea of Patients Prescribed Antiretroviral Therapy and Virally Suppressed: By Patient Characteristics Among Those With Healthcare Coverage or Assistance, Medical Monitoring Project, 2009–2013 (n = 17 560)
| Prescribed ART (%)b | HIV Viral Load Undetectable or <200 copies/mL (%) | |||||||
|---|---|---|---|---|---|---|---|---|
| Characteristic | % | 95% CI | P Valuec | % | 95 % CI | P Valuec | ||
| Health care payer type | <.01 | <.01 | ||||||
| RWHAP only | 94.2 | 92.8 | 95.5 | 76.7 | 74.5 | 78.8 | ||
| Private | 88.5 | 87.3 | 89.8 | 79.4 | 77.5 | 81.2 | ||
| Medicaid | 88.8 | 87.3 | 90.3 | 65.7 | 63.2 | 68.2 | ||
| Medicare | 92.6 | 90.3 | 94.9 | 78.0 | 75.0 | 81.0 | ||
| Medicaid +Medicare | 93.9 | 92.7 | 95.1 | 76.0 | 73.8 | 78.3 | ||
| Other public | 88.7 | 83.3 | 94.2 | 73.6 | 67.7 | 79.5 | ||
| Private+RWHAP | 95.2 | 93.3 | 97.1 | 82.4 | 79.3 | 85.5 | ||
| Medicaid+RWHAP | 94.9 | 93.6 | 96.3 | 70.4 | 67.3 | 73.4 | ||
| Medicare+RWHAP | 96.3 | 95.0 | 97.7 | 82.2 | 79.1 | 85.3 | ||
| Medicaid+Medicare+RWHAP | 96.4 | 94.7 | 98.2 | 80.0 | 76.0 | 84.0 | ||
| Other public + RWHAP | 95.4 | 92.8 | 97.9 | 78.8 | 74.4 | 83.2 | ||
| VA/Champus/Tricare | 95.2 | 92.7 | 97.8 | 79.4 | 74.9 | 83.9 | ||
| Other payer type | 92.4 | 90.7 | 94.0 | 77.3 | 74.7 | 80.0 | ||
| Gender | .02 | <.01 | ||||||
| Male | 92.6 | 91.9 | 93.3 | 77.6 | 76.4 | 78.8 | ||
| Female | 91.2 | 90.3 | 92.1 | 71.1 | 69.2 | 73.0 | ||
| Transgender/Intersex | 93.6 | 90.0 | 97.2 | 67.5 | 60.4 | 74.6 | ||
| Age (years) | <.01 | <.01 | ||||||
| 18–29 | 82.5 | 79.7 | 85.3 | 62.2 | 59.3 | 65.2 | ||
| 30–39 | 90.7 | 89.3 | 92.1 | 70.9 | 68.9 | 72.9 | ||
| 40–49 | 92.7 | 91.8 | 93.6 | 74.8 | 73.2 | 76.3 | ||
| ≥50 | 94.1 | 93.3 | 94.9 | 80.7 | 79.5 | 82.0 | ||
| Race/Ethnicity | <.01 | <.01 | ||||||
| non-Hispanic black | 91.2 | 90.3 | 92.1 | 70.1 | 68.4 | 71.8 | ||
| non-Hispanic white | 93.5 | 92.4 | 94.6 | 81.9 | 80.8 | 82.9 | ||
| Hispanic | 92.3 | 91.1 | 93.4 | 76.4 | 74.1 | 78.8 | ||
| Other | 91.8 | 90.0 | 93.7 | 76.5 | 73.2 | 79.7 | ||
| Nativity | .31 | .03 | ||||||
| US-born | 92.2 | 91.6 | 92.7 | 75.4 | 74.2 | 76.6 | ||
| Foreign-born | 92.8 | 91.5 | 94.1 | 78.1 | 75.7 | 80.5 | ||
| Education | .33 | <.01 | ||||||
| Less than high school | 92.8 | 92.0 | 93.6 | 70.3 | 68.4 | 72.2 | ||
| High school graduated | 92.0 | 91.1 | 92.9 | 74.0 | 72.6 | 75.4 | ||
| Some college or more | 92.1 | 91.4 | 92.9 | 78.8 | 77.6 | 80.1 | ||
| Poverty statuse | .07 | <.01 | ||||||
| Above poverty level | 92.7 | 91.9 | 93.4 | 80.2 | 79.1 | 81.3 | ||
| At or below poverty level | 91.9 | 91.2 | 92.6 | 70.4 | 68.7 | 72.1 | ||
| Homeless (past 12 mo)f | <.01 | <.01 | ||||||
| Yes | 89.4 | 87.5 | 91.3 | 62.0 | 58.8 | 65.1 | ||
| No | 92.5 | 91.9 | 93.1 | 77.0 | 75.8 | 78.1 | ||
| Time since HIV diagnosis (years) | <.01 | <.01 | ||||||
| <5 | 86.8 | 85.4 | 88.2 | 72.4 | 70.3 | 74.6 | ||
| 5–9 | 92.9 | 91.9 | 93.9 | 76.1 | 74.5 | 77.8 | ||
| 10+ | 94.0 | 93.3 | 94.8 | 76.9 | 75.5 | 78.2 | ||
| HIV disease stageg | <.01 | .22 | ||||||
| Stage 1: No AIDS and nadir CD4 ≥500 (or CD4% ≥29) | 79.5 | 76.9 | 82.0 | 77.9 | 75.1 | 80.6 | ||
| Stage 2: No AIDS and nadir CD4 200–499 (or CD4% 14–<29) | 87.0 | 85.7 | 88.2 | 75.0 | 73.2 | 76.7 | ||
| Stage 3: AIDS or nadir CD4 0–199 (or CD4% <14) | 95.6 | 94.9 | 96.2 | 76.2 | 74.9 | 77.6 | ||
| Total | 92.2 | 91.6 | 92.8 | 75.8 | 74.6 | 76.9 | ||
Abbreviations: ART, antiretroviral therapy; CI, confidence interval; HIV, human immunodeficiency virus; RWHAP, Ryan White HIV/AIDS Program.
Percentages and 95 CIs are weighted to account for unequal selection probabilities and nonresponse.
Documented ART prescription in the medical record during the 12 months prior to interview.
P-value corresponding to global F-test.
Includes general education development (GED) credential.
US Department of Health and Human Services. Available at: http://aspe.hhs.gov/poverty/09poverty.shtml.
McKinney-Vento definition of homelessness: living on the street, living in a shelter, living in a single-room-occupancy hotel, temporarily staying with friends or family, or living in a car. A person is categorized as homeless if that person lacks a fixed, regular, adequate night-time residence or has a steady night-time residence that is 1) a supervised publicly or privately operated shelter designed to provide temporary living accommodation, 2) an institution that provides a temporary residence for persons intended to be institutionalized, or 3) a public or private place not designed for or ordinarily used as a regular sleeping accommodation for human beings (eg, in an automobile or under a bridge) (Stewart B. McKinney Homeless Assistance Act, 42 U.S.C. §11301, et seq; 1987).
Schneider E, Whitmore S, Glynn KM, et al Revised surveillance case definitions for HIV infection among adults, adolescents, and children aged <18 months and for HIV infection and AIDS among children aged 18 months to <13 years—United States, 2008. MMWR. Recommendations and reports : Morbidity and mortality weekly report. Recommendations and reports/Centers for Disease Control. Dec 5 2008; 57(RR-10):1–12.
After adjustment for patient characteristics, patients with private insurance, Medicaid, Medicare, or Medicaid + Medicare were 4%–7% less likely to be prescribed ART than those with RWHAP only (Table 3). Patients with Medicaid were 12% less likely to be virally suppressed than those with RWHAP only, whereas those with private insurance, Medicaid + Medicare, and Medicaid + RWHAP were 4%–5% less likely to be virally suppressed (Table 4).
Table 3.
Unadjusted and Adjusted Prevalence Ratios for Being Prescribed Antiretroviral Therapy by Healthcare Payer Type Among Human Immunodeficiency Virus (HIV)-infected Adults Receiving Medical Care With Healthcare Coverage or Assistance: Medical Monitoring Project, 2009–2013 (n = 17 560)
| Unadjusted Prevalence Ratio | 95% CI | P Value | Adjusteda Prevalence Ratio | 95% CI | P Value | |||
|---|---|---|---|---|---|---|---|---|
| RWHAP only | 1.00 | 1.00 | ||||||
| Private | 0.94 | .92 | .96 | <.01 | 0.94 | .92 | .96 | <.01 |
| Medicaid | 0.94 | .92 | .96 | <.01 | 0.93 | .92 | .95 | <.01 |
| Medicare | 0.98 | .95 | 1.01 | .26 | 0.96 | .92 | .99 | <.01 |
| Medicaid +Medicare | 1.00 | .98 | 1.02 | .79 | 0.96 | .95 | .98 | <.01 |
| Private+RWHAP | 1.01 | .99 | 1.03 | .33 | 1.00 | .98 | 1.02 | .79 |
| Medicaid+RWHAP | 1.01 | .99 | 1.02 | .32 | 1.00 | .98 | 1.01 | .66 |
| Medicare+RWHAP | 1.02 | 1.00 | 1.04 | .02 | 0.99 | .96 | 1.01 | .25 |
| Medicaid+Medicare+RWHAP | 1.02 | 1.00 | 1.04 | .01 | 0.99 | .97 | 1.02 | .59 |
| Other payer type | 0.98 | .97 | 1.00 | .13 | 0.97 | .95 | .99 | <.01 |
Abbreviations: CI, confidence interval; HIV, human immunodeficiency virus; RWHAP, Ryan White HIV/AIDS Program.
Results from logistic regression model adjusted for age, race, time since HIV diagnosis, HIV disease stage.
Table 4.
Unadjusted and Adjusted Prevalence Ratios for Having Human Immunodeficiency Virus (HIV) Viral Load < 200 copies/mL by Healthcare Payer Type Among HIV-infected Adults Receiving Medical Care With Healthcare Coverage or Assistance: Medical Monitoring Project, 2009–2013 (n = 17 560)
| Unadjusted Prevalence Ratio | 95% CI | P Value | Adjusteda Prevalence Ratio | 95% CI | P Value | |||
|---|---|---|---|---|---|---|---|---|
| RWHAP only | 1.00 | 1.00 | ||||||
| Private | 1.03 | .99 | 1.08 | .11 | 0.95 | .91 | .99 | .02 |
| Medicaid | 0.86 | .82 | .89 | <.01 | 0.88 | .85 | .92 | <.01 |
| Medicare | 1.02 | .97 | 1.06 | .48 | 0.96 | .91 | 1.00 | .06 |
| Medicaid +Medicare | 0.99 | .95 | 1.03 | .67 | 0.96 | .92 | .99 | .02 |
| Private+RWHAP | 1.07 | 1.03 | 1.12 | <.01 | 1.01 | .97 | 1.06 | .51 |
| Medicaid+RWHAP | 0.92 | .88 | .96 | <.01 | 0.95 | .91 | .98 | <.01 |
| Medicare+RWHAP | 1.07 | 1.03 | 1.12 | <.01 | 0.98 | .93 | 1.03 | .39 |
| Medicaid+Medicare+RWHAP | 1.04 | .98 | 1.11 | .17 | 0.99 | .93 | 1.05 | .73 |
| Other payer type | 1.01 | .97 | 1.05 | .65 | 0.95 | .91 | .99 | .01 |
Abbreviations: CI, confidence interval; HIV, human immunodeficiency virus; RWHAP, Ryan White HIV/AIDS Program.
Results from logistic regression model adjusted for age, race, nativity, poverty, education, homelessness, HIV disease stage.
Patients with Healthcare coverage Supplemented by RWHAP Assistance Compared to Patients with Other Healthcare coverage only
Patients whose private insurance or Medicaid coverage was supplemented by RWHAP assistance had better treatment outcomes than those without RWHAP supplementation. Those with private insurance + RWHAP were significantly more likely to be prescribed ART than those with private insurance only (96.0% vs 90.0%) (Figure 1). Those with Medicaid + RWHAP were more likely to be prescribed ART than those with Medicaid only (95.0% vs 89.0%). Patients with private insurance + RWHAP were significantly more likely to be virally suppressed than those with private insurance only (81.0% vs 76.0%), as were patients with Medicaid + RWHAP compared to those with Medicaid only (76.0% vs 71.0%).
Figure 1.
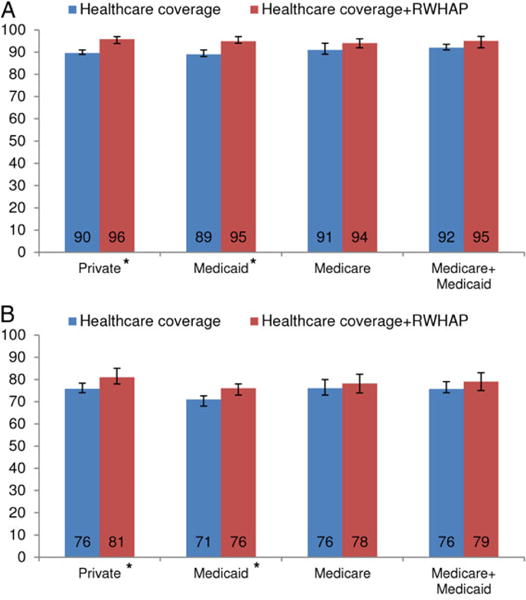
Adjusteda prevalence of (A) being prescribed antiretroviral therapy (ART) and (B) having human immunodeficiency virus (HIV) viral load <200 copies/mL, by private, Medicaid, or Medicare healthcare coverage and receipt of Ryan White HIV/AIDS Program (RWHAP) assistance among HIV-infected adults receiving medical care: Medical Monitoring Project, 2009–2013. Prevalence estimates are predicted probabilities from logistic regression model adjusted for (a) age, race, time since HIV diagnosis, and HIV disease stage and (b) age, race, nativity, poverty, education level, homelessness, and HIV disease stage. *P ≤ .01 for χ2 test comparing healthcare coverage with and without RWHAP.
DISCUSSION
RWHAP provides essential support for HIV care to uninsured and underinsured HIV-infected persons. More than 40% of HIV-infected patients in medical care during 2009–2012 relied on RWHAP, including 15% who relied solely on RWHAP for HIV medical care. Compared to the 3% of uninsured patients not receiving RWHAP assistance, uninsured persons whose HIV medical care was supported by RWHAP were nearly twice as likely to be prescribed ART and virally suppressed.
As a payer of last resort, RWHAP serves a sociodemographically disadvantaged population. As expected, we found that uninsured patients receiving RWHAP assistance were more likely to have incomes at or below the federal poverty level and to have been homeless during the past year than those with other types of coverage, and that these characteristics were negatively associated with viral suppression. Less expected was the finding that when sociodemographically disadvantaged patients received RWHAP assistance, they were more likely to be prescribed ART and virally suppressed than those with other types of coverage, including private insurance.
The largest observed differences in treatment outcomes were between patients receiving RWHAP assistance and those with Medicaid. Even patients with Medicaid + Medicare and Medicaid + RWHAP were less likely to be virally suppressed than those with RWHAP only. It should be noted that patients with Medicaid were more likely to have incomes at or below the federal poverty level than those with all other payer types, including the uninsured. We controlled for sociodemographic factors in our analysis but cannot rule out the possibility of residual confounding. Whereas the magnitude of this difference should be interpreted with caution, the significantly better treatment outcomes among patients with RWHAP only compared to those with Medicaid is an important finding.
Under the ACA, many HIV-infected persons are eligible for Medicaid coverage, and others are eligible to purchase private insurance through the marketplaces. However, increased eligibility for traditional sources of healthcare coverage is not a complete solution for uninsured and underinsured HIV-infected persons. First, some HIV-infected persons will remain uninsured if they reside in a state that is not expanding Medicaid [19], are not eligible for Medicaid due to residence in the United States <5 years, or are unable to afford private insurance. Second, these findings suggest that replacing HIV-infected persons’ RWHAP assistance with private insurance or Medicaid alone may not be optimal in terms of treatment outcomes. Last, transitions from RWHAP assistance to other coverage types are likely to be complicated by variable drug formularies, levels of provider expertise, and cost-sharing requirements, all of which could affect patient adherence and, ultimately, viral suppression [12]. RWHAP supplementation to private insurance or Medicaid may be one solution. Our analysis suggests that patients whose Medicaid or private insurance was supplemented by RWHAP were more likely to be prescribed ART and virally suppressed compared to those with Medicaid or private insurance only.
RWHAP’s impact on treatment outcomes is likely attributable to a number of pathways. These pathways include provision of medications, core medical and nonmedical case management, and supportive services such as substance abuse counseling, which are needed to promote ART treatment adherence, viral suppression, and overall health [9, 20, 21]. Importantly, RWHAP facilitates provision of these medical and supportive services using a coordinated approach similar to that of the medical home model, and many health providers in RWHAP facilities see HIV-infected patients exclusively [8, 12]. Patients with RWHAP only may have been more likely than those with other payer types, including those receiving supplemental RWHAP assistance, to receive coordinated care from RWHAP facilities serving as medical homes.
This study has limitations. First, we do not have information on which types of RWHAP support patients received; thus, we cannot attribute our findings to a particular service, or combinations of services, provided by RWHAP. RWHAP assistance was self-reported, and patients unaware of receiving RWHAP support may have underreported assistance. To alleviate this limitation, we asked patients to list all sources of health insurance or coverage either by name or generically, and we recoded state and local programs that received RWHAP funding as RWHAP assistance. Our data are cross-sectional, so we cannot establish temporality between RWHAP assistance and our outcomes. However, we know that RWHAP assistance was received during the same year that a participant was prescribed ART and virally suppressed based on medical record data. Last, RWHAP program data indicate that approximately 60% of HIV-diagnosed persons receive RWHAP assistance [22], which is higher than the 40% we observed. MMP represents HIV-diagnosed persons in HIV medical care during an index year and not all persons diagnosed with HIV, so these data sources cannot be directly compared.
Despite these limitations, we were able to examine the impact of RWHAP on HIV treatment outcomes through ascertainment of RWHAP and other healthcare coverage types and other patient characteristics. This is critical because payer type is highly associated with both sociodemographic characteristics and health status. For example, 73% of patients with Medicaid had ever had stage 3 HIV disease, compared to 56% of those with private insurance. By ascertaining key health status variables and associated sociodemographic variables, we were able to control for them in the multivariate analysis. The value of this analysis is perhaps best highlighted by the more extreme differences in viral suppression that we observed between RWHAP and other types of coverage after adjusting for other patient characteristics compared to those observed before adjustment.
RWHAP is likely to remain an important source of support for HIV medical care, even as some HIV-infected persons’ coverage options increase under the ACA. HIV-infected persons have complex needs for both medical care and supportive services; transitioning this population to traditional sources of healthcare coverage may not be straightforward or optimal. Flexible and creative strategies may become more essential as RWHAP strives to maintain and further improve HIV care and treatment outcomes in an evolving healthcare environment.
Supplementary Material
Acknowledgments
We thank the participating Medical Monitoring Project (MMP) patients, facilities, project areas, and Provider and Community Advisory Board members. We also acknowledge the contributions of the Clinical Outcomes Team and Behavioral and Clinical Surveillance Branch at the Centers for Disease Control and Prevention (CDC) and the MMP Study Group Members: (http://www.cdc.gov/hiv/statistics/systems/mmp/resources.html#StudyGroupMembers).
Financial support. This work, and the Medical Monitoring Project, is supported by cooperative agreement (PS09-937) from the CDC.
Footnotes
Supplementary Data
Supplementary materials are available at http://cid.oxfordjournals.org. Consisting of data provided by the author to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the author, so questions or comments should be addressed to the author.
Disclaimer. The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the CDC.
Potential conflicts of interest. All authors: No potential conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1.Cohen MS, Chen YQ, McCauley M, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365:493–505. doi: 10.1056/NEJMoa1105243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents. Washinton, DC: Department of Health and Human Services; [Google Scholar]
- 3.US Department of Health and Human Services HRSA, HIV/AIDS Bureau. The Ryan White HIV/AIDS Program Progress Report 2012: Ahead of the Curve. 2012 [Google Scholar]
- 4.Hirschhorn LR, Landers S, McInnes DK, et al. Reported care quality in federal Ryan White HIV/AIDS Program supported networks of HIV/AIDS care. AIDS Care. 2009;21:799–807. doi: 10.1080/09540120802511992. [DOI] [PubMed] [Google Scholar]
- 5.Sullivan PS, Denniston M, Mokotoff E, Buskin S, Broyles S, McNaghten AD. Quality of care for HIV infection provided by Ryan White Program-supported versus non-Ryan White Program-supported facilities. PLoS One. 2008;3:e3250. doi: 10.1371/journal.pone.0003250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Valverde E, Del Rio C, Metsch L, et al. Characteristics of Ryan White and non-Ryan White funded HIV medical care facilities across four metropolitan areas: results from the Antiretroviral Treatment and Access Studies site survey. AIDS Care. 2004;16:841–50. doi: 10.1080/09546120412331290130. [DOI] [PubMed] [Google Scholar]
- 7.Weiser J, Beer L, Frazier EL, et al. Service delivery and patient outcomes in Ryan White Human Immunodeficiency Virus/AIDS program-funded and nonfunded health care facilities in the United States. JAMA Intern Med. 2015 doi: 10.1001/jamainternmed.2015.4095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Beane SN, Culyba RJ, Demayo M, Armstrong W. Exploring the medical home in Ryan White HIV care settings: a pilot study. J Assoc Nurses AIDS Care. 2014;25:191–202. doi: 10.1016/j.jana.2013.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Health Resources and Services Administration HAB. Going the Distance: The Ryan White HIV/AIDS Program, 20 Years of Leadership, a Legacy of Care. 2010 [Google Scholar]
- 10.Kates J, Garfield R, Young K, Quinn K, Frazier E, Skarbinski J. Assessing the Impact of the Affordable Care Act on Health Insurance Coverage of People with HIV. Washington, DC: Kaiser Family Foundation; 2012. [Google Scholar]
- 11.Kates J. Implications of the Affordable Care Act for people with HIV infection and the Ryan White HIV/AIDS program: what does the future hold? Top Antiviral Med. 2013;21:138–42. [PMC free article] [PubMed] [Google Scholar]
- 12.Sood N, Juday T, Vanderpuye-Orgle J, et al. HIV care providers emphasize the importance of the Ryan White Program for access to and quality of care. Health Aff. 2014;33:394–400. doi: 10.1377/hlthaff.2013.1297. [DOI] [PubMed] [Google Scholar]
- 13.Frankel MR, McNaghten A, Shapiro MF, et al. A probability sample for monitoring the HIV-infected population in care in the U.S. and in selected states. Open AIDS J. 2012;6:67–76. doi: 10.2174/1874613601206010067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.US Department of Health and Human Services. Protection of Human Subjects, US Federal Code Title 45 Part 46. 2009 [Google Scholar]
- 15.Centers for Disease Control and Prevention. Distinguishing Public Health Research and Public Health Nonresearch. 2010 [Google Scholar]
- 16.Schneider E, Whitmore S, Glynn KM, et al. Revised surveillance case definitions for HIV infection among adults, adolescents, and children aged <18 months and for HIV infection and AIDS among children aged 18 months to <13 years—United States, 2008. MMWR Recomm Rep. 2008;57(RR-10):1–12. [PubMed] [Google Scholar]
- 17.US Department of Health and Human Services. The 2009 HHS Poverty Guidelines. 2009 [Google Scholar]
- 18.US Department of Health and Human Services. The 2010 HHS Poverty Guidelines. 2010 [Google Scholar]
- 19.Snider JT, Juday T, Romley JA, et al. Nearly 60,000 uninsured and low-income people with HIV/AIDS live in states that are not expanding Medicaid. Health Aff. 2014;33:386–93. doi: 10.1377/hlthaff.2013.1453. [DOI] [PubMed] [Google Scholar]
- 20.Katz MH, Cunningham WE, Fleishman JA, et al. Effect of case management on unmet needs and utilization of medical care and medications among HIV-infected persons. Ann Intern Med. 2001;135:557–65. doi: 10.7326/0003-4819-135-8_part_1-200110160-00006. [DOI] [PubMed] [Google Scholar]
- 21.Craw JA, Gardner LI, Marks G, et al. Brief strengths-based case management promotes entry into HIV medical care: results of the antiretroviral treatment access study-II. J Acquir Immune Defic Syndr. 2008;47:597–606. doi: 10.1097/QAI.0b013e3181684c51. [DOI] [PubMed] [Google Scholar]
- 22.Health Resources and Services Administration HAB. The Intersection of the Ryan White HIV/AIDS Program with the Essential Health Benefits in Private Health Insurance and Medicaid. 2013 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


