INTRODUCTION
Illicit drug use ranks among the ten leading preventable risk factors for years of healthy life lost to death and disability in the U.S.,1 and is a common concern in civilian workplaces,2,3 and the Armed Forces.4,5 Of interest to the military, drug use among employees is associated with negative job-related consequences including illness, poor attendance, reduced job-performance capability, and increased employee turnover.6 Historically, combat warriors have used drugs to ward off fatigue, reduce pain, and lessen boredom.7 In 1994, the Department of Defense (DoD) implemented a force-wide drug testing program, replacing the unique programs operated by each Service, creating a uniform set of consequences for positive drug tests.8 This force-wide ‘zero tolerance’ policy has been updated periodically but its intent has remained to prevent the use of illicit drugs through a random, and for cause, detection program with sanctions for members who test positive.9,10 A March 2014 DoD Instruction stated that the use of illegal substances, “is incompatible with readiness, the maintenance of high standards of performance, and military discipline.”11
Research suggests the drug testing program has served as a strong deterrent to illicit drug use within the military, and discourages illicit drug users from volunteering or remaining in military service.8 Anonymous surveys of active duty members have found relatively low past year self-reported illicit drug use: 0.9% for marijuana (referred to as pot, THC, or weed and excluding synthetic cannabis such as spice), 0.9% for cocaine/crack, 0.9% for methylenedioxymethamphetamine (MDMA or ecstasy), 0.8% for methamphetamines, and 0.8% for heroin.12 Historically, self-report illicit drug use has been highest among members ages 18 to 25.13 Low use of illicit drugs has been confirmed by recent analysis of drug test results based on urinalysis samples. Platteborze et al. reported that in Army urine specimens submitted for drug testing in FYs 2001–2011, 1.06% were positive for an illicit drug, including 0.79% for the metabolite of marijuana (tetrahydrocannabinol or THC), similar to the self-reported rate above, and 0.26% for cocaine.14 The Platteborze et al. study did not examine positive drug test rates specific to a deployment cohort, or among enlisted members. Another recent study assessed illicit drug use among active duty members from all Services who served on active duty all 12 months of FY 2010 by examining claims data (both medical and pharmacy) and urine drug test results.15 The study reported that 0.4% had a positive drug test. Illicit drug use was significantly higher among those: with an E1–E3 enlisted rank, aged 18 – 24, Army affiliation, receipt of >10 prescriptions for any drug type, receipt of prescriptions for mental health conditions, and having a mental health disorder primary diagnosis. While 44% of the sample had been deployed in FYs 2009 or 2010, the analysis of positive drug tests was not relative to deployment end dates, and not specific to a postdeployment cohort. Analysis of the DoD’s drug testing program does not reveal true prevalence, only the prevalence of those tested during specific random, and for cause, occasions.
To our knowledge, no studies have reported drug test results from the postdeployment reintegration period, a time when members are particularly vulnerable for behavioral health problems, suicide, dishonorable discharge, and alcohol use problems.16–18 Thus, using urinalysis data from the Military Personnel Drug Abuse Testing Program, we report the percent of Army enlisted members testing positive for illicit drug use after deployments in support of Operation Enduring Freedom and Operation Iraqi Freedom (OEF/OIF) ending in FYs 2008–2011. We examine two critical postdeployment periods. The immediate window, covering 0–6 months postdeployment, a period when the military assesses the self-reported health of returning members in order to arrange for medical or psychological services, and a follow-up window of 6 months to 3 years postdeployment. The primary focus of the paper is the follow-up window, which may present an extended opportunity for the DoD to provide intervention to prevent postdeployment problems. We study the associations between demographic and deployment characteristics and testing positive for illicit drug use for the follow-up window.19 The aim of this paper is to provide analyses on the postdeployment health of Army enlisted members that deployed to OEF/OIF to inform the design of effective prevention and treatment programs.20
METHODS
Data
Study data, described below, are from Brandeis University’s Substance Use and Psychological Injury Combat Study (SUPIC), a longitudinal, observational study designed to examine substance use and psychological health outcomes for up to three years postdeployment among Army members returning from OEF/OIF deployments in FYs 2008–2011.19 Urine drug test data were from the Military Personnel Drug Abuse Testing Program, provided by the Defense Manpower Data Center (DMDC). These data included the specimen collection date, collection premise (random, probable cause, safety mishap investigation, medical, rehabilitation, job, other), panels of drugs that were tested, medical record review finding for two drugs that may be legally prescribed (d-amphetamine and d-methamphetamine), and test results for each tested drug. Collection of urine specimens for drug testing is governed by the DoD’s strict requirements including testing at independent laboratories and a precise protocol. The protocol defines the minimum nanograms per milliliter for a positive test, and requires initial immunoassay screening, confirmatory specific gas chromatography/mass spectrometry tests, and other quality safeguards to minimize false positives.14 DoD regulation governs the frequency of random tests, drug classes and tests of the “common test panel” (i.e., minimum across all Services). Commanders may require additional drug tests for other reasons (accident, rehabilitation) and for additional classes of drugs.
Deployment measures were obtained from the DMDC contingency tracking system, and demographic measures were from the Defense Enrollment Eligibility Records System (DEERS).19 The study protocol was approved by the Brandeis University Committee for Protection of Human Subjects and the Human Research Protection Program of the Office of the Assistant Secretary of Defense for Health Affairs/Defense Health Agency (OASD(HA)/DHA). The DHA Privacy and Civil Liberties Office executed an annual Data Sharing Agreement and supplemental approval was received from the DMDC and DHA to analyze the drug test data.
Subjects
SUPIC’s sample consists of 643,205 Army active duty component (AD) and reserve component (RC) members, selected based on contingency data with a deployment ending during FYs 2008–2011 in support of OEF/OIF. The main SUPIC sample is a census of all Army returnees during this time window, excluding a small portion (1.2%) of atypical deployments (i.e., shorter than 30 days or five or more years). For each member, the first deployment record in the window was selected for analysis (index deployment) using rules described in SUPIC’s Rationale and Methods paper.19
Of the main SUPIC sample, analysis for this paper was restricted to enlisted Army returnees who had at least one postdeployment common panel drug test during the postdeployment windows described below. The sample for the immediate postdeployment window for this paper included 265,689 AD and 43,380 RC returnees with urine drug test results. The sample for the follow-up window was comprised of 306,345 AD and 136,433 RC members with urine drug test results. The combined sample represents 92.0% and 80.3% of the SUPIC-PM cohort, respectively. During the period of this study, DoD policy required biennial rather than annual random drug tests for the RC. The unit of analysis is the service member; each member may have had multiple urine specimens collected in either time window, or both.
Time Windows
Drug test results from two time windows, immediate postdeployment (0 to < 6 months) and follow-up (6 months to 3 years postdeployment), were examined separately and combined. Since each Army member’s window is based on the end date of his or her index deployment, the follow-up window varies by member. The follow-up window is the primary focus of most analysis as it corresponds to long-term behaviors and may be influenced by Army programs or interventions for returning service members.
Measures
Positive Drug Test
The outcome for the multivariate analysis was any positive drug test during the follow-up window. During the study period, the Military Personnel Drug Abuse Testing Program had a common test panel comprised of tests for 8 specific drugs: (metabolites of) cocaine, heroin, THC, and 4 drugs in the amphetamine class (separate confirmation of d-Amphetamine, d-Methamphetamine, methylenedioxymethamphetamine (MDMA or ecstasy), methylenedioxyamphetamine (MDA), and methylenedioxyethylamphetamine (MDEA)). Routine testing for the opiate/opioid classes was not introduced until May 2012, and hence not included in this paper.10,14
The test result for each drug was coded as positive, negative, or pending medical review (only relevant for positive d-amphetamine and d-methamphetamine tests). Among 10,146 positive tests for d-amphetamine in the follow-up window, the medical review was pending for 10.9%, while 80.1% of those reviewed were negative. Among the 1,304 positive drug tests for d-methamphetamine, medical review was not complete for 18.4%, yet 98.0% of those reviewed were positive. When medical record review was not available for d-amphetamine and d-methamphetamine, we imputed the test result to be negative for d-amphetamine and positive for d-methamphetamine based the results of those reviewed.
Covariates
Sociodemographic characteristics included age group, gender, race, Hispanic ethnicity, marital status, any child dependents with TRICARE benefits (as a proxy for being a parent), rank, occupation (combat specialist; healthcare; functional support, service, supply; mechanical, electrical, and engineering; and other), education, and TRICARE region of residence. Index deployment characteristics included length in months, assignment to a Warrior Transition Unit after deployment start date, prior deployment, and time between index deployment and last prior deployment.
Control Variables
The fiscal year of the start date of the index deployment was used to control for policy or program changes over time. The number of months between the index deployment end and the last specimen collection date served as an estimate of the months of observation. Since outcomes were based on members, not individual specimens, the number of specimens analyzed per member was determined.
Statistical Analysis
All analyses were stratified by component due to possible differences and hypotheses about postdeployment environment (illicit drug availability; frequency of testing; command leadership influence). The dependent variable was a positive urine drug test for any common panel drug, reported separately by window, and separate variables for each of the tested drugs (follow-up window only). Results were expressed as the percent of the sample with a positive urine drug test, with a 95% Wald asymptotic confidence interval (CI) for the binomial proportion.21 A rate (e.g., the number who tested positive per person months of observation) was not calculated because military separation dates were not available at time of analysis. Chi-square tests of independence were conducted to measure bivariate associations between demographic and deployment characteristics and testing positive in the follow-up window.
We hypothesized that the data may have a clustered structure because Army members within the same military unit may share characteristics related to testing positive: access to illicit drugs, prescription patterns, urine specimen collection schedule if random testing occurs systematically within a unit, troop discipline, and social influences. However, because no suitable clustering variable was available, we used a single-level (i.e., fixed effects) multivariate logistic regression to model the odds of testing positive in the follow-up window. The model was adjusted for demographics, deployment characteristics, and control variables. Regression diagnostics, including multicollinearity diagnostics (variance inflation factors) were performed.
We conducted a sensitivity analysis to compare characteristics of subjects included in and excluded from follow-up window analyses. We also examined whether prevalence of positive drug tests in the immediate postdeployment window was higher among members who only had drug test data in that window compared to those with data in both windows. Additionally, because the analysis was not restricted to random tests, we conducted descriptive analyses to determine the number of drug tests per member by drug test premise.
All calculations were performed using SAS/Base and SAS/STAT software (version 9.2; SAS Institute Inc., Cary, NC).
RESULTS
Prevalence
In the follow-up window, the median number of specimens tested per member was 4 for AD (interquartile range 2 to 7) and 3 for RC (interquartile range 1 to 4) (data not shown). Virtually all members had at least one random test (AD 99.5%; RC 98%) in the follow-up window. The percent of AD and RC enlisted members who had at least one positive test for any common panel drug at any time during the combined window (0 – 3 years postdeployment) was 3.46% for AD and 3.84% for RC (see Table 1). During the immediate window (0<6 months postdeployment) the percent positive was 1.65% for AD and 2.18% for RC. During the follow-up window (6 months to 3 years postdeployment), 2.74% of AD members had at least one positive drug test compared to 3.54% of RC. The magnitude of the difference in AD and RC groups was relatively small (Cohen’s d =0.047; small defined as an ES less than 0.20).22 Figure 1 shows that positive drug tests during the follow-up window were mostly for marijuana (1.89% for AD and 2.83% for RC).
TABLE 1.
Percent of US Army enlisted personnel with postdeployment positive drug test, by time window and component, Substance Use and Psychological Injury Combat Study
| Postdeployment Time Window and Component | Test Results for Common Panel of Drugsa | |||
|---|---|---|---|---|
| n Positiveb | Total Testedc | % Positive | (95% CI) | |
| Combined (0 to 3 yr) | ||||
| Active Duty | 11,786 | 340,598 | 3.46 | (3.40, 3.52) |
| National Guard/Reserve | 5,522 | 143,859 | 3.84 | (3.74, 3.94) |
| Immediate (0 to <6 mo) | ||||
| Active Duty | 4,382 | 265,689 | 1.65 | (1.60, 1.70) |
| National Guard/Reserve | 947 | 43,380 | 2.18 | (2.05, 2.32) |
| Follow-up (6 mo to 3 yr) | ||||
| Active Duty | 8,399 | 306,345 | 2.74 | (2.68, 2.80) |
| National Guard/Reserve | 4,831 | 136,433 | 3.54 | (3.44, 3.64) |
Common panel: metabolites of cocaine, heroin, marijuana (i.e., THC), and the amphetamine class, with separate confirmation of d-Amphetamine, d-Methamphetamine, and two designer (non-prescribed) amphetamines, MDMA (ecstasy) and MDA
Number of enlisted personnel testing positive for any common panel drug during the time window
Total enlisted personnel who received at least one common panel test during the time window
FIGURE 1.
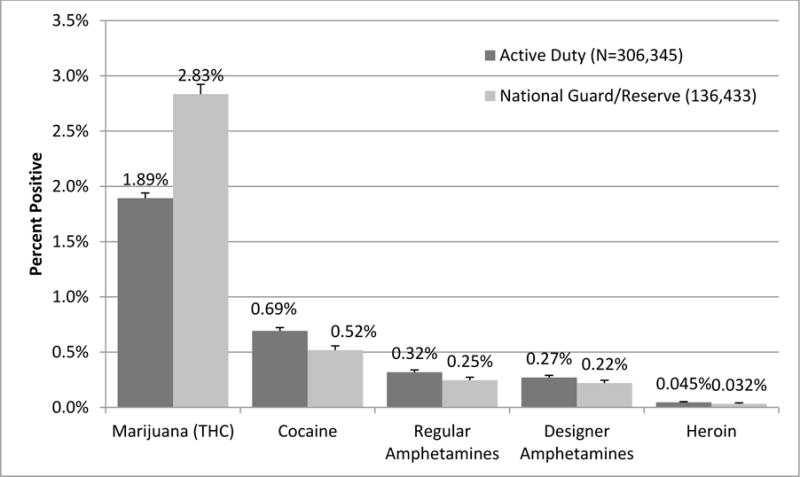
Percent (95% confidence interval) of US Army enlisted personnel with positive drug test, postdeployment follow-up window (6 mo to 3 yr), by type of drug and component, Substance Use and Psychological Injury Combat Study
Unadjusted Association with Demographic and Deployment Characteristics
Table 2 shows the percentage with positive drug tests for each demographic group and deployment characteristic in the follow-up window. Among both AD and RC, the percentage with a positive drug test was higher among males than females. Compared to older members, younger members (age group 17–24 years) were more likely to test positive, as were those with characteristics associated with younger age (never married, no child dependents, junior enlisted members (E1–E4), high school education or less). Black enlisted RC had a higher percent positive than other race groups. Regarding deployment characteristics, AD members with index deployments beginning in FY2008 or earlier had a higher percent positive; for RC members the percent positive was higher in FY2008 and FY2009. In both components, members with no deployments prior to the index deployment were more likely to test positive than those with prior deployments.
TABLE 2.
Percent of US Army enlisted personnel with positive drug test, postdeployment follow-up window (6 mo to 3 yr), by demographic and deployment characteristics and component, Substance Use and Psychological Injury Combat Study
| Characteristica | Test Results for Common Panel of Drugsb, 6 mo to 3 yr postdeployment
|
|||
|---|---|---|---|---|
| Active Duty Enlisted (N=306,345) |
National Guard and Reserve Enlisted (N=136,433) |
|||
|
| ||||
| n Positivec | % Positivec | n Positivec | % Positivec | |
|
| ||||
| All enlisted | 8,399 | 2.74 | 4,831 | 3.54 |
|
| ||||
| Demographic | ||||
|
| ||||
| Gender | ||||
| Male | 7,972 | 2.89 | 4,499 | 3.68 |
| Female | 427 | 1.41 | 332 | 2.32 |
|
| ||||
| Age (yr) | ||||
| 17–24 | 6,280 | 4.12 | 3,131 | 6.16 |
| 25–29 | 1,430 | 1.95 | 870 | 3.10 |
| 30–39 | 613 | 0.91 | 528 | 1.58 |
| 40+ | 76 | 0.55 | 302 | 1.25 |
|
| ||||
| Race | ||||
| White | 5,010 | 2.73 | 3,596 | 3.31 |
| Black | 1,853 | 3.02 | 1,042 | 5.45 |
| Asian/Pacific Islander | 1,363 | 2.97 | 95 | 2.18 |
| Other | 173 | 1.12 | 98 | 2.28 |
|
| ||||
| Hispanic Ethnicity | ||||
| Yes | 836 | 2.24 | 346 | 2.63 |
| No | 7,563 | 2.81 | 4,485 | 3.64 |
|
| ||||
| Marital Status | ||||
| Never Married | 4,633 | 3.99 | 3,223 | 5.57 |
| Married | 3,551 | 2.03 | 1,388 | 2.04 |
| Divorced | 187 | 1.27 | 211 | 2.10 |
|
| ||||
| Any child dependent receiving TRICARE benefits | ||||
| Yes | 2,522 | 1.82 | 1,439 | 2.25 |
| No | 5,877 | 3.50 | 3,392 | 4.68 |
|
| ||||
| Rank, pay grade | ||||
| Junior Enlisted (E1–E4) | 7,702 | 4.02 | 4,328 | 5.85 |
| Senior Enlisted (E5–E9) | 697 | 0.61 | 503 | 0.81 |
|
| ||||
| Education | ||||
| Less than high school | 2,846 | 5.89 | 1,451 | 7.12 |
| High school | 5,154 | 2.32 | 3,074 | 3.54 |
| Some college | 284 | 1.36 | 236 | 1.16 |
| College degree | 62 | 0.57 | 38 | 0.46 |
|
| ||||
| Occupation Type | ||||
| Combat Specialist | 3,136 | 3.48 | 1,627 | 4.70 |
| Healthcare | 311 | 1.73 | 177 | 2.45 |
| Functional Support, Service, Supply | 2,034 | 2.46 | 1,472 | 2.94 |
| Mechanical, Electrical, & Engineering | 1,557 | 2.53 | 744 | 3.20 |
| Other | 1,361 | 2.51 | 811 | 3.83 |
|
| ||||
| Region of residence | ||||
| North | 2,188 | 2.59 | 2,088 | 3.83 |
| South | 2,745 | 2.92 | 1,683 | 3.98 |
| West (including Alaska) | 2,690 | 2.85 | 958 | 2.77 |
| Outside US | 755 | 2.34 | 92 | 1.88 |
|
| ||||
| Deployment | ||||
|
| ||||
| Fiscal year of beginning of index deployment | ||||
| FY2007 or earlier | 2,363 | 3.37 | 713 | 3.39 |
| FY2008 | 2,270 | 2.92 | 1,234 | 4.09 |
| FY2009 | 2,407 | 2.70 | 1,876 | 3.83 |
| FY2010 | 1,293 | 2.04 | 847 | 2.86 |
| FY2011 | 66 | 1.13 | 161 | 2.38 |
|
| ||||
| Length of index deployment (months), | ||||
| 1–11 | 2,945 | 2.65 | 4,432 | 3.60 |
| 12 | 2,296 | 2.58 | 231 | 3.32 |
| >12 | 3,158 | 2.97 | 168 | 2.66 |
|
| ||||
| Any deployment prior to index | ||||
| Yes | 1,796 | 1.35 | 719 | 1.54 |
| No | 6,603 | 3.81 | 4,112 | 4.59 |
|
| ||||
| Dwell timed under 12 months (among those with prior deployment) | ||||
| Yes | 244 | 1.65 | 79 | 2.55 |
| No | 1,552 | 1.31 | 640 | 1.46 |
|
| ||||
| Assigned to Warrior Transition Unit since start of index deployment | ||||
| Yes | 442 | 4.77 | 206 | 3.22 |
| No | 7,957 | 2.68 | 4,625 | 3.56 |
Characteristic measured at beginning of FY2008–2011 deployment (index), unless indicated.
Common panel: metabolites of cocaine, heroin, marijuana (THC), amphetamine class, with confirmation of d-Amphetamine, d-Methamphetamine, and 2 designer (non-prescribed) amphetamines, MDMA (ecstasy) and MDA.
Number and percent testing positive for any common panel drug among those with the characteristic shown. Cells do not always sum to total due to suppression of categories < 30 cases or item non-response. All bivariate associations between each characteristic and testing positive were statistically significant (p<0.001; Chi-Square test for independence) except for assigned to Warrior Transition Unit among National Guard and Reserve.
Dwell time is the time between the end of the deployment immediately prior to the index deployment and the start of the index deployment.
Multivariate Models
Table 3 shows the demographic and deployment characteristics associated with a positive drug test in the follow-up window. In the multivariate model, being male, black or Asian/Pacific Islander relative to white (AD only), never married, no college degree, and combat specialist (relative to all other occupations), were each associated with higher odds of a positive drug test. By contrast, each older age group (relative to 17–24), and being Asian/Pacific Islander relative to white (RC only), were associated with lower odds of a positive drug test.
TABLE 3.
Characteristics associated with the odds of a positive drug test, postdeployment follow-up window (6 mo to 3 yr), US Army enlisted personnel by component, Substance Use and Psychological Injury Combat Study
| Characteristica | Multivariate Logistic Model Adjusted Odds Ratiob (95% CI) |
|
|---|---|---|
| Active Duty Enlisted N=306,345 |
National Guard/Reserve Enlisted N=136,433 |
|
|
| ||
| Demographic | ||
|
| ||
| Gender | ||
| Female (ref.) | 1.0 | 1.0 |
| Male | 2.27 (2.05–2.51)* | 1.98 (1.76–2.23)* |
|
| ||
| Age | ||
| 17–24 (ref.) | 1.0 | 1.0 |
| 25–29 | 0.69 (0.65–0.73)* | 0.74 (0.68–0.81)* |
| 30–39 | 0.36 (0.32–0.39)* | 0.41 (0.37–0.45)* |
| 40+ | 0.21 (0.16–0.26)* | 0.31 (0.27–0.36)* |
|
| ||
| Race | ||
| White (ref.) | 1.0 | 1.0 |
| Black | 1.71 (1.61–1.81)* | 2.01 (1.86–2.17)* |
| Asian/Pacific Islander | 1.14 (1.07–1.22)* | 0.75 (0.60–0.92)* |
| Other/unknown | 0.82 (0.70–0.96)* | 0.98 (0.79–1.21) |
|
| ||
| Hispanic ethnicity | ||
| No (ref.) | 1.0 | 1.0 |
| Yes | 0.93 (0.87–1.01) | 0.94 (0.83–1.06) |
|
| ||
| Marital status | ||
| Married/divorced/other (ref.) | 1.0 | 1.0 |
| Never married | 1.15 (1.09–1.22)* | 1.66 (1.53–1.81)* |
|
| ||
| Any child dependent receiving TRICARE benefits | ||
| No (ref.) | 1.0 | 1.0 |
| Yes | 1.08 (1.02–1.16)* | 1.13 (1.04–1.23)* |
|
| ||
| Education level | ||
| College degree (ref.) | 1.0 | 1.0 |
| Less than college degree | 2.96 (2.29–3.81)* | 4.23 (3.06–5.84)* |
|
| ||
| DoD occupation | ||
| Other occupation (ref.) | 1.0 | 1.0 |
| Combat specialist | 1.17 (1.11–1.23)* | 1.43 (1.34–1.52)* |
|
| ||
| Deployment | ||
|
| ||
| Fiscal year of begin date of index deployment | ||
| FY2007 or earlier | 10.44 (8.09–13.48)* | 4.04 (3.34–4.87)* |
| FY2008 | 8.54 (6.64–10.99)* | 4.16 (3.48–4.96)* |
| FY2009 | 5.47 (4.26–7.03)* | 3.39 (2.86–4.02)* |
| FY2010 | 2.27 (1.76–2.92)* | 1.56 (1.30–1.86)* |
| FY2011 (ref.) | 1.0 | 1.0 |
|
| ||
| Length of index deployment (months) | ||
| 1–11 (ref.) | 1.0 | 1.0 |
| 12 | 0.87 (0.82–0.92)* | 0.93 (0.80–1.08) |
| >12 | 0.80 (0.75–0.86)* | 0.67 (0.57–0.80)* |
|
| ||
| Dwell time under 12 months | ||
| No (ref.) | 1.0 | 1.0 |
| Yes | 1.12 (0.97–1.29) | 1.55 (1.22–1.97)* |
| No prior deployment | 1.97 (1.85–2.09)* | 2.28 (2.09–2.50)* |
|
| ||
| Assigned to Warrior Transition Unit since start of index deployment | ||
| No (ref.) | 1.0 | 1.0 |
| Yes | 1.63 (1.47–1.80)* | 1.10 (0.95–1.28) |
Characteristic measured at beginning of FY2008–2011 index deployment, unless indicated.
Models also control for number of specimens tested, number of months between the ending of the index deployment and the last collection date, and region of residence.
CI = 95% confidence interval
Wald Chi-Square Test, p<0.05
Regarding deployment characteristics, a long deployment (relative to 11 months or less) was associated with decreased odds of a positive drug test. Members with no prior deployment had approximately twice the odds of a positive drug test compared to those with a previous deployment. A short dwell time after the previous deployment increased the odds of a positive test (RC only) as did assignment to a Warrior Transition Unit after the index deployment start (AD only). Finally, there was a time trend in the percent positive associated with start date of deployment; this was strongest in the AD model.
Sensitivity Analyses
To determine if members included versus excluded from the follow-up window analyses were systematically different, we compared their demographic and deployment characteristics. Dropped subjects were more likely to be white (AD only) and have an index deployment beginning in FY2007 or earlier (AD only) or in FY2011, and less likely to be on first deployment or have child dependents than those with data in the follow-up window. A small group of subjects dropped from follow-up analyses (9.2% of enlisted AD and 4.1% of enlisted RC) had drug test data in the immediate postdeployment window. Compared to those with data in both postdeployment analysis windows, the percent positive in the dropped group was nearly five times higher (AD) and nearly four times higher (RC in the immediate postdeployment window: 5.37% vs. 1.10%, 5.48% vs. 1.50%, respectively, data not shown).
We further assessed the occurrence of non-random testing, a phenomenon where the commander may order a test for a group or individual because of suspected drug use or an accident. Only a small proportion (0.46% of AD; 1.98% of RC) had only a non-random drug test in the follow-up window and 7.08% (AD) and 16.54% (RC) had at least one non-random test. While the percent positive in these members was high (16.94% of AD, 9.67% of RC, data not shown), we consider this a mediating variable and the primary interest is the underlying demographic and deployment characteristics of members with positive drug tests.
DISCUSSION
This study presents the first postdeployment drug test findings in representative Army samples of AD and RC members returning from OEF/OIF deployments. On balance, despite a decade of war, Army members deployed during the study period had low positive drug tests during a postdeployment follow-up window (6 months to 3 years). Among those with at least one common panel drug test, the percent with a positive test was 2.74 (CI 2.68, 2.80) and 3.54 (CI 3.44, 3.64) for AD and RC, respectively. The follow-up window comprises a longitudinal period that could be influenced by early intervention for members returning from deployment. Examining all postdeployment drug test data starting with the date of deployment return, inclusive of a small number of members with no data in the follow-up window, yields a higher percent positive for AD and RC of 3.46 (CI 3.40, 3.53) and 3.84 (CI 3.73, 3.94), respectively. Positive drug tests were predominantly for THC, and the difference in percentages between RC and AD was explained by THC prevalence. This finding lends support to prevention theories based on the social-ecological model, that societal and community environments influence drug use behavior.20,23 Thus, RC members who return to their civilian communities postdeployment may have more opportunity and cultural influences to use illicit drugs. It also may reflect an artifact of the drug testing program; AD members had more frequent drug tests than RC in this study and the threat of more frequent tests may be a deterrent to use. Future research could examine the effect on drug testing results after implementation of the 2012 DoD policy change that requires annual random drug testing for the RC. African Americans/blacks in the RC had twice the odds of a positive test relative to whites, but this association was attenuated among AD. Conversely, those identified as Asian/Pacific Islander in AD had increased odds relative to whites, but RC Asian/Pacific Islanders had reduced odds. It is unknown how geographic location or connection to military bases influence these findings, and future research could explore the relationship of locations of home communities or military bases with regulations regarding marijuana access and legal consequences in those communities.24
Differences in analysis methods and different definitions of drug use make it difficult to compare this study’s results to prior research. Most drug use measures are based on self-report12 and few studies are specific to the reintegration phase after a deployment.14,15 Only one other person-level analysis was found in the literature, which predominantly reports population trends over time rather than prevalence among cohorts of individuals.11 This study’s finding that THC is the most prevalent positive drug test is consistent with prior research.14 One study found that 33.7% of OEF/OIF veterans in low-income, predominantly minority neighborhoods within New York City reported using marijuana in the past 30 days.24 Our inclusion of variables that control for time trends (FY of deployment), the number of specimens tested and observation months is a particular strength of this study. Drug testing frequency varies among members and follow-up windows were not uniform in length (e.g., members returning from deployments in FYs 2010 and 20111 had shorter follow-up windows and fewer chances to get tested), thus controlling for these variables strengthens the validity of our conclusions.
A policy-relevant finding is the increased odds of a positive drug test among first-time deployers, a finding consistent with prior research on selection of healthy individuals for deployment and repeat deployment.25–27 This finding is consistent with a prior study of incident drug use disorders and deployment based on claims data; the adjusted rate ratio for members with no or one deployment was much higher than members deployed 4 or more times.28 One interpretation is that deployment stress may be greatest among first deployers and illicit drugs may be part of a coping strategy.4,29 Consistent with the theory of increased stress, combat specialists had increased odds (RC model) of a positive drug test, as did members assigned to Warrior Transition Units who are coping with combat-related injuries. If additional studies associate postdeployment drug use with stress levels, the military could explore evidence-based early intervention strategies targeted at these risk groups.
There are plausible, alternative reasons for the observed time trend regarding year deployed including possible confounding of time with combat theater (OEF vs OIF), improvements over time in the handling of theater psychological injury, and military recruitment changes (e.g., issue of waivers) around 2007. We control for observable drug test program features; however, there may be other uncontrolled changes in the operation of the program. It is plausible that the findings reflect true declines in illicit drug use among returning members that may be the result of more attention to postdeployment problems, reductions in combat trauma not captured by our measures, or other unmeasured factors.
Several limitations are associated with this study. These estimates do not include results for drugs that were not on the common panel before the 2012 DoD Instruction.9 While there has been an explosion in prescribing drugs for pain with high abuse potential (e.g., oxycodone),30 the military’s drug testing program did not require 100% testing of urine samples for prescribed opioids until 2012, so force-wide estimates of abuse are generally incomplete.4,5,31–35 Now, or in the near future, 100% of specimens from random tests (formerly only a sample) will be tested for opioids (Codeine, Morphine, Oxycodone, Oxymorphone, Hydrocodone, Hydromorphone) and benzodiazepines (α-OH-Alprazolam, Lorazepam, Nordiazepam, Oxazepam, Temazepam).36 In late 2013, the DoD expanded its zero tolerance policy to include synthetic marijuana (also known as spice), and planned to include it in the drug testing panel.36 One estimate of synthetic marijuana use before it was banned was 2.5% of members,36 while another study found that synthetic marijuana was the most prevalently abused illicit substance among a subsample of substance-using Army members.37 Thus, this analysis restricted to four drug classes provides the lower bound of positive drug tests. Additionally, periodic drug tests underestimate the true prevalence of drug use in a population. While drug testing is intended to be random, we do not know if there is speculation about when testing will happen which would impact positive drug tests results. Anecdotal findings from a non-random sample of 50 active duty members found reports of how to avoid detection of drug use (e.g., using immediately after a prior drug test was completed).38 The metabolites of drugs other than marijuana are detectable in urine for only 2 to 4 days; marijuana metabolites can be detectable 1 to 3 weeks and longer. Assuming only one random drug test per year, and that the drug is detectable, we calculate that a person using cocaine or amphetamine two consecutive days a month would have a probability of detection of 0.13 (24 days of use × 2 day detection window/365 days). Borack39 demonstrated that when use of illicit drugs is infrequent, the expected time until detection can range from one year to as long as 10 years depending on the frequency of urine testing. We cannot draw any conclusions about the severity of drug use, consequences of use, or whether Army members met criteria for a drug use disorder, all information which would be important for planning appropriate clinical services.15 We suspect there may be differences based on drug exposure and availability during deployment, but analysis did not examine deployment location (Afghanistan versus Iraq). This study cannot draw any conclusions about the causes of postdeployment drug use. Finally, we lacked historical data to examine whether drug use differs pre- and postdeployment among those deployed.
Military policy gives commanders authority to process for separation those members with detected drug use, but the military services are not precluded from taking disciplinary action in appropriate cases (Personal communication, Defense Office of Prepublication and Security Review). An Institute of Medicine Committee argued that voluntary treatment-seeking for substance use should not lead to automatic separation especially among postdeployment members and among those who are still performing their duties adequately.4 Expanded access to treatment of postdeployment stress and depression may be effective at reducing drug use and lead to greater retention of military members who have undergone costly training and demonstrated they have effectively performed deployment duties. One study of active duty members within a treatment population found that the odds of having a prior diagnosis of posttraumatic stress disorder was 20 times greater among those with a diagnosis of opiate abuse/dependency.40 We are currently analyzing the association of postdeployment positive drug tests with self-report mental health screening results and combat exposure on postdeployment health assessments. If these self-assessments are associated with increased risk of follow-up positive drug tests, this will strengthen the rationale to explore expanded evidence-based postdeployment interventions as part of a comprehensive preventive strategy for military drug use.
Footnotes
Guarantor: Mary Jo Larson
References
- 1.U.S. Preventative Services Task Force. Screening for Illicit Drug Use: U.S. Preventive Services Task Force Recommendation Statement. 2008 http://www.uspreventiveservicestaskforce.org/uspstf08/druguse/drugrs.htm. Accessed October 1, 2014.
- 2.Carpenter C. Workplace drug testing and worker drug use. Health Services Research. 2007;42(2):795–810. doi: 10.1111/j.1475-6773.2006.00632.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.French M, Roebuck MC, KÃbreau-Alexandre P. To test or not to test: do workplace drug testing programs discourage employee drug use? Social science research. 2004;33(1):45–63. doi: 10.1016/s0049-089x(03)00038-3. [DOI] [PubMed] [Google Scholar]
- 4.IOM (Institute of Medicine) Substance Use Disorders in the U.S Armed Forces. 2013 http://www.nap.edu/catalog.php?record_id=13441. Accessed November 15, 2014.
- 5.Army Suicide Prevention Task Force. Army Health Promotion Risk Reduction Suicide Prevention Report. 2010 csf2.army.mil/downloads/HP-RR-SPReport2010.pdf. Accessed November 1, 2014.
- 6.Larson SL, Eyerman J, Foster MS, Gfroerer JC. (DHHS Publication No. SMA 07-4273, Analytic Series A-29).Worker Substance Use and Workplace Policies and Programs. 2007 http://www.oas.samhsa.gov/work2k7/work.htm#6.1. Accessed September 29, 2014.
- 7.Robins LN. Vietnam Veterans’ Rapid Recovery from Heroin Addiction: A Fluke or Normal Expectation? Addiction. 1993;88:1041–1054. doi: 10.1111/j.1360-0443.1993.tb02123.x. [DOI] [PubMed] [Google Scholar]
- 8.Mehay SL, Pacula RL. The Effectiveness of Workplace Drug Prevention Policies: Does Zero Tolerance’ Work? 1999 http://www.nber.org/papers/w7383. Accessed Access August 11, 2014.
- 9.Department of Defense. Instruction Number 1010.01 Military Personnel Drug Abuse Testing Program (MPDATP) 2012 www.dtic.mil/whs/directives/corres/pdf/101001p.pdf. Accessed December 1, 2014.
- 10.Department of Defense. Instruction Number 1010.16 Technical Procedures for the Military Personnel Drug Abuse Testing Program (MPDATP) 2012 www.dtic.mil/whs/directives/corres/pdf/101016p.pdf. Accessed December 1, 2014.
- 11.Department of Defense. Instruction Number 1010.04 Problematic Substance Use by DoD Personnel. 2014 www.dtic.mil/whs/directives/corres/pdf/101004p.pdf. Accessed December 1, 2014.
- 12.Barlas FM, Higgins WB, Pflieger JC, Diecker K. 2011 Department of Defense Health Related Behaviors Survey of Active Duty Military Personnel. Fairfax, Virginia: ICF International; 2013. [Google Scholar]
- 13.Bray RM, Pemberton MR, Hourani LL, et al. 2008 Department of Defense Survey of Health Related Behaviors Among Active Duty Military Personnel. 2009 http://www.tricare.mil/tma/2008HealthBehaviors.pdf. Accessed January 3, 2015.
- 14.Platteborze PL, Kippenberger DJ, Martin TM. Drug Positive Rates for the Army, Army Reserve, and Army National Guard From Fiscal Year 2001 through 2011. Military medicine. 2013;178(10):1078–1084. doi: 10.7205/MILMED-D-13-00193. [DOI] [PubMed] [Google Scholar]
- 15.Jeffery DD, May L, Luckey B, Balison BM, Klette KL. Use and abuse of prescribed opioids, central nervous system depressants, and stimulants among U.S. active duty military personnel in FY 2010. Military medicine. 2014;179(10):1141–1148. doi: 10.7205/MILMED-D-14-00002. [DOI] [PubMed] [Google Scholar]
- 16.Larson MJ, Wooten NR, Adams RS, Merrick EL. Military Combat Deployments and Substance Use: Review and Future Directions. Journal of Social Work Practice in the Addictions. 2012;12(1):6–27. doi: 10.1080/1533256X.2012.647586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Adams RS, Larson MJ, Corrigan JD, Horgan CM, Williams TV. Frequent binge drinking after combat-acquired traumatic brain injury among active duty military personnel with a past year combat deployment. The Journal of head trauma rehabilitation. 2012;27(5):349–360. doi: 10.1097/HTR.0b013e318268db94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.IOM (Institute of Medicine) Returning home from Iraq and Afghanistan: Assessment of readjustment needs of veterans, service members, and their families. 2013 http://www.iom.edu/Reports/2013/Returning-Home-from-Iraq-and-Afghanistan.aspx. Accessed October 17, 2014. [PubMed]
- 19.Larson MJ, Adams RS, Mohr BA, et al. Rationale and methods of the substance use and psychological injury combat study (SUPIC): A longitudinal study of Army service members returning from deployment in FY2008–2011. Substance Use & Misuse. 2013;48(10):863–879. doi: 10.3109/10826084.2013.794840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.IOM (Institute of Medicine) Preventing Psychological Disorders in Service Members and Their Families: An Assessment of Programs. 2014 doi: 10.7205/MILMED-D-14-00360. http://www.iom.edu/Reports/2014/Preventing-Psychological-Disorders-in-Service-Members-and-Their-Families.aspx. Accessed January 4, 2015. [DOI] [PubMed]
- 21.Agresti A. Categorical Data Analysis. 2nd. New York, NY: John Wiley & Sons; 2002. [Google Scholar]
- 22.Cohen J. Analysis for the Behavioral Sciences. 2nd. Hillsdale, NJ: Lawrence Erlbaum Associates Publishers; 1988. [Google Scholar]
- 23.Bronfenbrenner U. The Ecology of Human Development: Experiments by Nature and Design. Cambridge, MA: Harvard University Press; 1979. [Google Scholar]
- 24.Golub A, Bennett AS. Substance use over the military–veteran life course: An analysis of a sample of OEF/OIF veterans returning to low-income predominately minority communities. Addictive Behaviors. 2014;39(2):449–454. doi: 10.1016/j.addbeh.2013.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wilson J, Jones M, Fear NT, et al. Is Previous Psychological Health Associated With the Likelihood of Iraq War Deployment? An Investigation of the “Healthy Warrior Effect”. American Journal of Epidemiology. 2009;169(11):1362–1369. doi: 10.1093/aje/kwp044. [DOI] [PubMed] [Google Scholar]
- 26.Larson GE, Highfill-McRoy RM, Booth-Kewley S. Psychiatric Diagnoses in Historic and Contemporary Military Cohorts: Combat Deployment and the Healthy Warrior Effect. American Journal of Epidemiology. 2008;167(11):1269–1276. doi: 10.1093/aje/kwn084. [DOI] [PubMed] [Google Scholar]
- 27.Larson M, Ritter GA, Adams R. Suicides among military personnel. JAMA. 2013;310(23):2565–2565. doi: 10.1001/jama.2013.282695. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4132876/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shen Y-C, Arkes J, Williams TV. Effects of Iraq/Afghanistan Deployments on Major Depression and Substance Use Disorder: Analysis of Active Duty Personnel in the US Military. American Journal of Public Health. 2012;102(S1):S80–S87. doi: 10.2105/AJPH.2011.300425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bliese PD, Wright KM, Hoge CW. Preventive Mental Health Screening in the Military. In: Adler AB, Bliese PD, Castro CA, editors. Deployment Psychology: Evidence-Based Strategies to Promote Mental Health in the Military. Washington, DC: American Psychological Association; 2011. pp. 175–193. [Google Scholar]
- 30.Centers for Disease Control and Prevention. Policy Impact: Prescription Painkiller Overdoses. 2011. [Google Scholar]
- 31.Seal KH, Cohen G, Waldrop A, Cohen BE, Maguen S, Ren L. Substance use disorders in Iraq and Afghanistan veterans in VA healthcare, 2001–2010: Implications for screening, diagnosis and treatment. Drug and Alcohol Dependence. 2011;116(1–3):93–101. doi: 10.1016/j.drugalcdep.2010.11.027. [DOI] [PubMed] [Google Scholar]
- 32.Macey TA, Morasco BJ, Duckart JP, Dobscha SK. Patterns and correlates of prescription opioid use in OEF/OIF veterans with chronic noncancer pain. Pain Medicine. 2011;12(10):1502–1509. doi: 10.1111/j.1526-4637.2011.01226.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Seal KH, Shi Y, Cohen G, et al. Association of mental health disorders with prescription opioids and high-risk opioid use in US veterans of Iraq and Afghanistan. JAMA. 2012;307(9):940–947. doi: 10.1001/jama.2012.234. [DOI] [PubMed] [Google Scholar]
- 34.Wu PC, Lang C, Hasson NK, Linder SH, Clark DJ. Opioid use in young veterans. J Opioid Manag. 2010;6(2):133–139. doi: 10.5055/jom.2010.0013. [DOI] [PubMed] [Google Scholar]
- 35.Dao J, Frosch D. Feeling Warehoused in Army Trauma Care Units. The New York Times. 2010 http://www.nytimes.com/2010/04/25/health/25warrior.html. Accessed December 2, 2014.
- 36.Marshall TC., Jr DoD Adds Synthetic Marijuana to Random Drug Testing. 2013 http://www.navy.mil/submit/display.asp?story_id=78325. Accessed June 4, 2014.
- 37.Walker D, Neighbors C, Walton T, et al. Spicing up the military: Use and effects of synthetic cannabis in substance abusing army personnel. Addictive behaviors. 2014;39(7):1139–1144. doi: 10.1016/j.addbeh.2014.02.018. [DOI] [PubMed] [Google Scholar]
- 38.Bucher J. Soldiering with substance: substance and steroid use among military personnel. Journal of drug education. 2012;42(3):267–292. doi: 10.2190/DE.42.3.b. [DOI] [PubMed] [Google Scholar]
- 39.Borack JL. A Technique for Estimating the Impact of Improvements in Drug Testing Sensitivity on Detection and Deterrence of Illicit Drug Use by Navy Personnel. NPRDC TR-97-2. 1997 https://libsearch.nps.edu/vufind/Record/189880. Accessed December 8, 2014.
- 40.Dabbs C, Watkins EY, Fink DS, Eick-Cost A, Millikan AM. Opiate-related dependence/abuse and PTSD exposure among the active-component U.S. military, 2001 to 2008. Military medicine. 2014;179(8):885–890. doi: 10.7205/MILMED-D-14-00012. [DOI] [PubMed] [Google Scholar]


