Abstract
The role of patient-level risk factors such as insufficient vision has been under-studied. Because insufficient vision may interfere with health literacy assessments, the full impact of low health literacy among older patients with impaired vision is unknown. We sought to determine whether senior inpatients’ insufficient vision and low health literacy are associated with adverse outcomes post-discharge, specifically falls and readmissions. We conducted an observational study of adult medicine inpatients at an urban hospital. Visual acuity and health literacy were screened at bedside. Outcomes data were collected by telephone 30 days post-discharge. Among 1,900 participants, 1,244 (65%) were reached post-discharge; 44% had insufficient vision and 43% had low health literacy. Insufficient vision was associated with post-discharge falls among participants ≥65 years (adjusted odds ratio [AOR] 3.38, 95% confidence interval [CI] 1.42-8.05), but not among participants <65 years (AOR 1.44, 95% CI 0.89-2.32. Low health literacy was associated with readmissions among participants ≥65 years (AOR 3.15, 95% CI 1.77-5.61), but not among participants <65 years (AOR 0.78, 95% CI 0.56-1.09). The results suggest the need to implement screening for older inpatients’ vision and health literacy. Developing effective interventions to reduce these risks is critical given national priorities to reduce falls and readmissions.
Keywords: health services for the aged, hospitalization, vision, ocular, health literacy, patient readmission
Introduction
As the population ages, assessing health and safety risks associated with the aging process becomes increasingly critical (U.S. Department of Health and Human Services, 2014). One important health and patient safety factor that changes with age is vision, as older patients are significantly more likely to have poor vision (Klein & Klein, 2013). Among older community-dwelling adults, insufficient vision has been associated with a range of negative outcomes, including lower quality-of-life, lower functional status, falls, fractures, and motor vehicle crashes (Klein, Klein, Lee, & Cruickshanks, 1998; Owsley et al, 1998; Scott et al., 1994; West et al., 1997). Among older hospitalized patients, however, known hazards associated with insufficient vision are much more limited. Delirium (Inouye, 1998) and low health literacy (HL) (Press, Shapiro, Mayo, Meltzer, & Arora, 2013) are two risk factors that have been associated with poor vision in the hospital setting. While low HL is independently associated with adverse health outcomes, including hospitalization and mortality among senior patients (Baker et al., 2007; Baker, Wolf, Feinglass, & Thompson, 2008; Sudore et al., 2006), it is possible that low HL coupled with insufficient vision poses an even greater barrier to self-management (Press et al., 2011). However, much of the HL literature excludes patients with delirium (Kobayashi, Wardle, Wolf, & von Wagner, 2015) and poor vision (Matthiesen, Vela, & Press, 2015).
There is a growing recognition for the need to assess for and intervene on insufficient vision among hospitalized patients. For instance, identifying access to corrective lenses for hospitalized patients is a key national indicator for hospitalized seniors developed by the Assessing Care of Vulnerable Elders (ACOVE) program (Rowe & MacLean, 2007). Providing access to corrective lenses for patients with insufficient vision in the hospital setting is not infeasible. For instance, in our work, among the patients not wearing corrective lenses, we have shown that low-cost “readers” lenses correct the vision for the majority of patients with poor vision, including patients 65 years and older (Press et al., 2015). Despite the growing recognition of poor vision among inpatients, it is still unknown whether poor vision among hospitalized older patients is associated with worse outcomes after hospitalization. Understanding these associations is particularly important for seniors, who often suffer from “post-hospital syndrome,” or a period of acquired vulnerability after hospitalization (Krumholz, 2013). Two post-discharge outcomes that are particularly relevant for both patients and payers are post-discharge falls and readmissions, both of which are associated with significant increases in morbidity and healthcare costs (Jencks, Williams, & Coleman, 2009; Mahoney et al, 2000).
Because of the relationship between HL and risks associated with care transitions (Mitchell, Sadikova, Jack, & Paasche-Orlow, 2012), it is crucial to consider if and how HL mitigates the risks for those with sufficient and insufficient vision. For instance, the HL literature has made frequent use of written HL assessment instruments and thereby excluded patients with poor vision (Kobayashi et al., 2015; Parker, Baker, Williams, & Nurss, 1995; Press et al., 2011; Press et al., 2012; Press et al., 2013; Press et al., in press). Therefore, the full extent of the risk of low HL among vulnerable seniors after discharge may not be fully realized.
Understanding whether insufficient vision and low HL are associated with post-discharge outcomes for hospitalized seniors is critical to be able to identify interventions to improve post-discharge care. The aim of this study was to assess the associations between insufficient vision and low HL among hospitalized seniors with adverse post-hospital outcomes, specifically post-discharge falls and readmissions for seniors.
Methods
Participants were enrolled as part of an ongoing study of care quality for hospitalized patients at the University of Chicago Medicine (Meltzer et al., 2002). Eligible patients were English-speaking, non-blind, adult (age ≥ 18), hospitalized patients on the general medicine service. The University of Chicago Medicine institutional review board approved the protocol (IRB #9967).
Visual acuity was tested using the handheld Snellen Eye Chart held 14 inches away from the patient, and participants wore lenses if available. Room conditions were optimized prior to vision screening, including ensuring that the room was well lit. Sufficient vision was defined as having at least 20/40 vision in one eye, a cutoff chosen based on its association with decreased functional status in senior patients (West et al., 1997). HL was screened using the Brief Health Literacy Screen, an oral tool that does not rely on vision to assess HL (Chew, Bradley, & Boyko, 2004). This validated instrument consists of three questions, including “How confident are you filling out medical forms by yourself?,” “How often do you have someone help you read hospital materials?,” and “How often do you have problems learning about your medical condition because of difficulty understanding written information?” Each of these items is scored on a Likert scale from 0 to 4 (low to high). Participants were deemed to have low HL if they scored 2 or less on any question. Participants were surveyed for gender, race, and education, and were asked to self-rate their health one month prior to the interview. Participants were contacted by telephone 30 days after discharge and asked to complete a comprehensive assessment through phone interviews. Included within this assessment, participants were asked if they had fallen or been hospitalized since discharge (Bell et al., 2008; Hasan et al., 2009).
Chi-square tests were used to compare categorical variables. Multivariable logistic regression analyses controlling for gender, race, education, and general health were conducted to assess the association between insufficient vision and the two outcomes of interest (falls and rehospitalization). Similar models were created to test the association between low HL and these outcomes. In the models examining insufficient vision, low HL was tested as an effect modifier. In those examining low HL, insufficient vision was tested as an effect modifier. Likelihood ratio tests were performed to compare models with and without the effect modifier. Separate models were created for seniors and non-seniors, based on age 65 years and older. Statistical significance was defined as a p value less than 0.05, and analyses were performed using Stata version 14 (College Station, TX).
Results
Of the 1,900 participants who completed vision screening, the average age was 54 years with a standard deviation of 19 years. The majority of participants were female, African-American, and had graduated high school (Table 1). About half of the participants reported their overall health as less than good.
Table 1.
Characteristics of the Study Population by Age
| Overall | Age ≥ 65 | Age < 65 | P | |
|---|---|---|---|---|
|
|
||||
| Insufficient Vision, % (n) | 44.3 (841) | 65.9 (384) | 34.7 (457) | < 0.001 |
| Low HL, % (n)* | 42.7 (801) | 52.6 (303) | 38.3 (498) | < 0.001 |
| Female, % (n) | 55.3 (1,050) | 58.3 (340) | 53.9 (710) | 0.08 |
| AA race, % (n)† | 77.9 (1,438) | 76.5 (433) | 78.5 (1,005) | 0.3 |
| Health < good, % (n)‡ | 53.4 (1,007) | 50.5 (291) | 54.6 (716) | 0.1 |
| HS graduate, % (n)§ | 81.5 (1,510) | 76.2 (426) | 83.8 (1,084) | < 0.001 |
22 patients (1.2%) had missing data for health literacy.
333 patients (18.0%) were white, and 75 patients (4.1%) were classified as other; 54 patients (2.8%) had missing data for race.
13 patients (0.7%) had data missing for self-reported health.
47 patients (2.5%) had missing data for education.
Abbreviations: HL, health literacy; AA, African-American; HS, high school
Nearly half of the participants had insufficient vision. Among participants with insufficient vision, just under half (45%; 373/832) were wearing lenses during vision screening, about a third (34%; 286/832) did not have their lenses available, and a fifth (21%; 173/832) did not own lenses. Forty-three percent of participants had low HL. Participants aged 65 and over were significantly more likely to have insufficient vision, low HL, and to not have graduated high school (Table 1). Those with insufficient vision were significantly more likely to have low HL than their sufficient vision counterparts (Table 2). Participants with insufficient vision and with low HL were more likely to be African-American and to not have graduated high school (Table 2).
Table 2.
Characteristics of the Study Population by Vision Status and Health Literacy
| Sufficient Vision |
Insufficient Vision |
P | Adequate HL |
Low HL | P | |
|---|---|---|---|---|---|---|
|
|
||||||
| Low HL, % (n) | 34.0 (355) | 53.5 (446) | < 0.001 | -- | -- | -- |
| Age ≥ 65, % (n) | 18.8 (199) | 45.7 (384) | < 0.001 | 25.4 (273) | 37.8 (303) | < 0.001 |
| Female, % (n) | 55.8 (591) | 54.6 (459) | 0.59 | 57.6 (620) | 52.2 (418) | 0.02 |
| AA race, % (n) | 75.2 (771) | 81.3 (667) | 0.001 | 75.7 (793) | 80.9 (632) | 0.007 |
| Health < good, % (n) | 52.2 (550) | 54.8 (457) | 0.27 | 50.1 (538) | 57.5 (457) | 0.001 |
| HS graduate, % (n) | 85.5 (881) | 76.5 (629) | < 0.001 | 89.3 (941) | 70.7 (553) | < 0.001 |
Abbreviations: HL, health literacy; AA, African-American; HS, high school
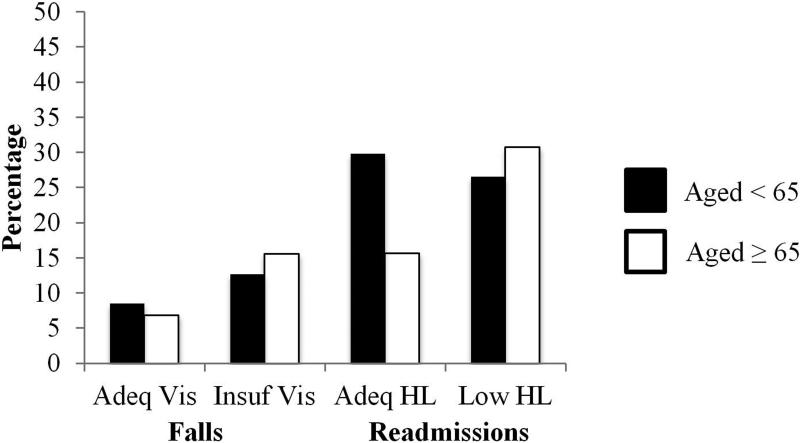
Nearly two-thirds (65%, 1,244/1,900) of the participants were reached by telephone for post-discharge assessment. Of those reached, a small proportion did not complete the falls assessment (2%, 31/1,244) or the readmissions assessment (1%, 12/1,244). During the follow-up assessment, 10% of participants younger than 65 years (85/845) versus 13% of participants aged 65 years or older (46/368) reported having sustained a fall in the month since discharge (p = 0.2). Among participants 65 years or older, those with insufficient vision (vs. sufficient vision) were significantly more likely to report a post-discharge fall (16% [37/237] vs. 7% [9/131], p = 0.02; Figure 1). This relationship approached, but did not meet, statistical significance among participants younger than 65 years (13% [39/306] vs. 9% [46/539], p = 0.05; Figure 1).
Figure 1. Readmissions and Falls at 30 Days Post-Discharge.
Abbreviations: Adeq, adequate; vis, vision; insuf, insufficient; HL, health literacy
Insufficient vision was independently associated with post-discharge falls among participants 65 years or older, but not among participants younger than 65 years, when controlling for gender, race, education, and general health (Table 3). Low HL did not significantly modify the association between vision and fall risk (p = 0.6) among participants 65 years or older. There was no significant association between low HL and falls, either among those 65 years or older (AOR 1.86, 95% CI 0.92-3.77) or younger than 65 years (AOR 1.33, 95% CI 0.81-2.17).
Table 3.
Associations with Post-discharge Falls: Multivariable Logistic Regression
| Age < 65 | Age ≥ 65 | |||
|---|---|---|---|---|
|
|
|
|||
| OR (95% CI) | P | OR (95% CI) | P | |
|
|
|
|||
| Insufficient vision | 1.44 (0.89-2.32) | 0.13 | 3.38 (1.42-8.05) | 0.006 |
| Female | 1.57 (0.95-2.58) | 0.08 | 0.91 (0.46-1.78) | 0.77 |
| AA | 0.76 (0.45-1.31) | 0.33 | 0.48 (0.23-1.02) | 0.06 |
| Health < good | 3.19 (1.84-5.53) | < 0.001 | 0.83 (0.43-1.62) | 0.59 |
| HS graduate | 1.13 (0.57-2.26) | 0.72 | 1.15 (0.49-2.71) | 0.75 |
| N | 809 | 343 | ||
Abbreviations: AA, African-American; HS, high school
Overall, similar proportions of participants reported readmissions in both age-groups: 24% (88/373) of participants 65 years or older and 29% (245/859) of participants younger than 65 years (p = 0.07). Within the 65 years or older group, those with low HL were significantly more likely to report a readmission (31% [61/198] vs. 16% [27/172], p = 0.001; Figure 1); this finding was not seen in the younger than 65 years cohort (27% [85/320] vs. 30% [158/530], p = 0.3; Figure 1). Low HL was independently associated with readmissions among participants 65 years or older, but not among participants younger than 65 years, when controlling for gender, race, education, and general health (Table 4).
Table 4.
Associations with Readmissions: Multivariable Logistic Regression
| Age < 65 | Age ≥ 65 | |||
|---|---|---|---|---|
|
|
|
|||
| OR (95% CI) | P | OR (95% CI) | P | |
|
|
|
|||
| Low HL | 0.78 (0.56-1.09) | 0.15 | 3.15 (1.77-5.61) | < 0.001 |
| Female | 0.86 (0.63-1.17) | 0.33 | 0.95 (0.56-1.61) | 0.84 |
| AA | 0.82 (0.58-1.18) | 0.29 | 0.40 (0.22-0.74) | 0.004 |
| Health < good | 1.41 (1.04-1.93) | 0.03 | 0.90 (0.53-1.52) | 0.69 |
| HS graduate | 0.66 (0.42-1.02) | 0.06 | 0.96 (0.51-1.83) | 0.91 |
| N | 815 | 345 | ||
Abbreviations: HL, health literacy; AA, African -American;, high school
Among the participants 65 years or older, insufficient vision did not significantly modify the association between low HL and readmissions (p = 0.6). There was no significant association between insufficient vision and readmission in either age group (≥ 65 years: AOR 1.51, 95% CI 0.87-2.64; < 65 years: AOR 1.01, 95% CI 0.74-1.40).
Discussion
Hospitalized seniors with insufficient vision are at higher risk of falls in the post-discharge period. This finding is not surprising, as it complements work conducted in the outpatient setting that shows that insufficient vision is a risk factor for falls among community dwelling seniors (de Boer et al., 2004; Lord & Dayhew, 2001). However, these findings do represent a missed opportunity to assess for, and intervene on, poor vision among vulnerable hospitalized seniors. Furthermore, this work advances our understanding of the risk of low HL among seniors with regards to hospitalization. We found that senior inpatients are at higher risk for readmission within one month post-discharge. This finding again complements previous work on risks for index hospital admissions that are known to be associated with community dwelling seniors with low HL (Baker et al., 2002; Baker, Parker, Williams, & Clark, 1998; Berkman et al., 2011; Cho, Lee, Arozullah, & Crittenden, 2008).
It is noteworthy that the effect of low HL on readmissions in this study was isolated to the senior population. Previous work examining the implications of HL on hospital admissions among a mixed population of seniors and non-seniors has either not found this interaction or not examined for it (Baker et al., 1998; Mitchell et al., 2012; Murray, Tu, Wu, Morrow, Smith, & Brater, 2009). It is likely that the detrimental effects of low HL have special relevance for the elderly, as aging has been associated with increased risk of declining health literacy (Kobayashi et al., 2015). Such effects could be due in part to an increased relevance of HL among the elderly due to the higher burden of chronic disease requiring self-management efficacy to mitigate an increased vulnerability to functional decline (Parker, Ratzan, & Lurie, 2003).
Because recently hospitalized patients are, in general, a higher risk population than outpatients (Krumholz, 2013), these findings highlight opportunities to enhance hospital-based efforts to reduce adverse events. For instance, screening hospitalized patients for insufficient vision could be a valuable way to identify seniors with post-discharge health risks in order to target important hospital-to-home transition interventions. The findings also suggest that wearing lenses cannot be taken itself as a proxy for sufficient vision, as just under half of patients with insufficient vision were wearing lenses at the time of screening. This finding could stem from inadequate vision care in the community or from hospital-specific vision hazards including decreased level of arousal.
Further, our finding that hospitalized seniors who had low HL were nearly twice as likely to report a readmission within 30 days of discharge has important policy implications given the focus on reducing costly readmissions for Medicare patients. For example, hospitals could use identifying low HL to target novel readmission reduction interventions. Such programs could ultimately improve care and prevent costly readmissions for common conditions among hospitalized vulnerable seniors.
Finally, our data that show that inpatients with insufficient vision are more likely to have low HL; these risks may not be mutually exclusive. For instance, low HL may lead to decreased awareness of, and/or access to, vision care to improve vision level; vision screening may aid in overcoming HL barriers and improve awareness of and access to vision care post-hospital discharge. In addition, correcting vision may contribute to improved self-efficacy that could lead to improved HL; given that a significant percentage of hospitalized patients with insufficient vision can have their vision corrected by cost-effective interventions such as “readers” lenses, this is a promising finding (Press et al., 2015). Future work could explore the extent to which vision and low health literacy interact.
However, despite likely overlap between poor vision and low health literary, it is important to understand the independent risks associated with poor vision and low health literacy, as the two are not complete proxies for each other. For instance, even if vision is adequate, low HL likely interferes with a patient’s ability to understand post-discharge instructions and contributes to an increased readmission risk. Similarly, regardless of one’s health literacy level, insufficient vision predisposes patients to negative health outcomes including falls.
Although our findings advance our understanding of important inpatient risk factors for hospitalized seniors, there are limitations to our study. First, since the majority of this population was African American and at a single urban site, our findings may not be generalizable. Second, we used self-report to identify our fall and readmission outcomes, therefore response bias could limit our findings. Additionally, we used a self-report tool to identify low-health literacy, a complex construct without a gold standard; several studies have shown this verbal self-response assessment has fair concordance with more objective vision-based HL assessments (Chew et al., 2004; Press et al., 2013; Wallston et al., 2014). Finally, there was a significant loss to follow-up in this study, though participants lost to follow up were not significantly different with respect to the primary study variables, vision and HL. Future work can address some of these limitations by including different study populations and administrative data.
Despite these limitations, this study demonstrates that in-hospital insufficient vision and low HL are each associated with important adverse post-hospitalization outcomes for seniors. These findings suggest that future efforts should test whether screening and addressing both insufficient vision and low HL among hospitalized seniors could improve the health and safety of this vulnerable and growing population after hospital discharge.
Acknowledgements
Funders: Mr. Jaffee is supported by a Calvin Fentress Research Fellowship. Dr. Press is supported by a career development award (NHLBI K23HL118151). This work was also supported by a pilot award from The Center on the Demography and Economics of Aging (CoA, National Institute of Aging P30 AG012857) and a Seed Grant from the Center for Health Administration Studies.
Footnotes
Contributors: None
Prior presentations: Preliminary versions of this work have been presented in abstract form on September 5, 2014 (oral) and August 25, 2015 (poster) at the Midwest Society of General Internal Medicine Annual Meeting in Chicago, IL and Cleveland, OH, respectively.
Conflicts of Interest: Dr. Hariprasad reports being a consultant or participating on a speaker’s bureau for Alcon, Allergan, Regeneron, Genentech, Optos, OD-OS, Bayer, Clearside Biomedical, and Ocular Therapeutix. All other authors have no conflicts of interest to report.
References
- Baker DW, Gazmararian JA, Williams MV, Scott T, Parker RM, Green D, Peel J. Functional health literacy and the risk of hospital admission among Medicare managed care enrollees. American Journal of Public Health. 2002;92(8):1278–1283. doi: 10.2105/ajph.92.8.1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker DW, Parker RM, Williams MV, Clark WS. Health literacy and the risk of hospital admission. Journal of General Internal Medicine. 1998;13(12):791–798. doi: 10.1046/j.1525-1497.1998.00242.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker DW, Wolf MS, Feinglass J, Thompson JA, Gazmararian JA, Huang J. Health literacy and mortality among elderly persons. Archives of Internal Medicine. 2007;167(14):1503–1509. doi: 10.1001/archinte.167.14.1503. http://doi.org/10.1001/archinte.167.14.1503. [DOI] [PubMed] [Google Scholar]
- Baker DW, Wolf MS, Feinglass J, Thompson JA. Health Literacy, Cognitive Abilities, and Mortality among Elderly Persons. Journal of General Internal Medicine. 2008;23(6):723–726. doi: 10.1007/s11606-008-0566-4. doi:10.1007/s11606-008-0566-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell CM, Schnipper JL, Auerbach AD, Kaboli PJ, Wetterneck TB, Gonzales DV, Meltzer DO. Association of Communication Between Hospital-based Physicians and Primary Care Providers with Patient Outcomes. Journal of General Internal Medicine. 2008;24(3):381–386. doi: 10.1007/s11606-008-0882-8. http://doi.org/10.1007/s11606-008-0882-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Family Medicine. 2004;36(8):588–594. [PubMed] [Google Scholar]
- Cho YI, Lee S-YD, Arozullah AM, Crittenden KS. Effects of health literacy on health status and health service utilization amongst the elderly. Social Science & Medicine (1982) 2008;66(8):1809–1816. doi: 10.1016/j.socscimed.2008.01.003. http://doi.org/10.1016/j.socscimed.2008.01.003. [DOI] [PubMed] [Google Scholar]
- de Boer MR, Pluijm SM, Lips P, Moll AC, Völker-Dieben HJ, Deeg DJ, van Rens GH. Different Aspects of Visual Impairment as Risk Factors for Falls and Fractures in Older Men and Women. Journal of Bone and Mineral Research. 2004;19(9):1539–1547. doi: 10.1359/JBMR.040504. http://doi.org/10.1359/JBMR.040504. [DOI] [PubMed] [Google Scholar]
- Hasan O, Meltzer DO, Shaykevich SA, Bell CM, Kaboli PJ, Auerbach AD, Schnipper JL. Hospital Readmission in General Medicine Patients: A Prediction Model. Journal of General Internal Medicine. 2009;25(3):211–219. doi: 10.1007/s11606-009-1196-1. http://doi.org/10.1007/s11606-009-1196-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inouye SK. Delirium in hospitalized older patients: recognition and risk factors. Journal of Geriatric Psychiatry and Neurology. 1998;11(3):118–125. doi: 10.1177/089198879801100302. discussion 157–158. [DOI] [PubMed] [Google Scholar]
- Jencks SF, Williams MV, Coleman EA. Rehospitalizations among Patients in the Medicare Fee-for-Service Program. New England Journal of Medicine. 2009;360(14):1418–1428. doi: 10.1056/NEJMsa0803563. http://doi.org/10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- Klein BE, Klein R, Lee KE, Cruickshanks KJ. Performance-based and self-assessed measures of visual function as related to history of falls, hip fractures, and measured gait time. The Beaver Dam Eye Study. Ophthalmology. 1998;105(1):160–164. doi: 10.1016/s0161-6420(98)91911-x. [DOI] [PubMed] [Google Scholar]
- Klein R, Klein BE. The Prevalence of Age-Related Eye Diseases and Visual Impairment in Aging: Current Estimates. Investigative Opthalmology & Visual Science. 2013;54(14):ORSF5–ORSF13. doi: 10.1167/iovs.13-12789. doi: 10.1167/iovs.13-12789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kobayashi LC, Wardle J, Wolf MS, von Wagner C. Cognitive Function and Health Literacy Decline in a Cohort of Aging English Adults. Journal of General Internal Medicine. 2015;30(7):958–964. doi: 10.1007/s11606-015-3206-9. http://doi.org/10.1007/s11606-015-3206-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krumholz HM. Post-Hospital Syndrome — An Acquired, Transient Condition of Generalized Risk. New England Journal of Medicine. 2013;368(2):100–102. doi: 10.1056/NEJMp1212324. http://doi.org/10.1056/NEJMp1212324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lord SR, Dayhew J. Visual risk factors for falls in older people. Journal of the American Geriatrics Society. 2001;49(5):508–515. doi: 10.1046/j.1532-5415.2001.49107.x. [DOI] [PubMed] [Google Scholar]
- Mahoney JE, Palta M, Johnson J, Jalaluddin M, Gray S, Park S, et al. Temporal association between hospitalization and rate of falls after discharge. Archives of Internal Medicine. 2000;160(18):2788–2795. doi: 10.1001/archinte.160.18.2788. http://doi.org/10.1001/archinte.160.18.2788. [DOI] [PubMed] [Google Scholar]
- Matthiesen MI, Vela MB, Press VG. Health Literacy During Aging. Journal of General Internal Medicine. 2015;30(12):1731. doi: 10.1007/s11606-015-3487-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meltzer D, Manning WG, Morrison J, Shah MN, Jin L, Guth T, Levinson W. Effects of physician experience on costs and outcomes on an academic general medicine service: results of a trial of hospitalists. Annals of Internal Medicine. 2002;137(11):866–874. doi: 10.7326/0003-4819-137-11-200212030-00007. [DOI] [PubMed] [Google Scholar]
- Mitchell SE, Sadikova E, Jack BW, Paasche-Orlow MK. Health Literacy and 30-Day Postdischarge Hospital Utilization. Journal of Health Communication. 2012;17(3):325–338. doi: 10.1080/10810730.2012.715233. doi:10.1080/10810730.2012.715233. [DOI] [PubMed] [Google Scholar]
- Murray MD, Tu W, Wu J, Morrow D, Smith F, Brater DC. Factors Associated With Exacerbation of Heart Failure Include Treatment Adherence and Health Literacy Skills. Clinical Pharmacology & Therapeutics. 2009;85(6):651–658. doi: 10.1038/clpt.2009.7. doi:10.1038/clpt.2009.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owsley C, Ball K, McGwin G, Jr, Sloane ME, Roenker DL, White MF, Overley ET. Visual processing impairment and risk of motor vehicle crash among older adults. JAMA. 1998;279(14):1083–1088. doi: 10.1001/jama.279.14.1083. [DOI] [PubMed] [Google Scholar]
- Parker RM, Baker DW, Williams MV, Nurss JR. The Test of Functional Health Literacy in Adults. Journal of General Internal Medicine. 1995;10(10):537–541. doi: 10.1007/BF02640361. doi:10.1007/BF02640361. [DOI] [PubMed] [Google Scholar]
- Parker RM, Ratzan SC, Lurie N. Health Literacy: A Policy Challenge For Advancing High-Quality Health Care. Health Affairs. 2003;22(4):147–53. doi: 10.1377/hlthaff.22.4.147. doi:10.1377/hlthaff.22.4.147. [DOI] [PubMed] [Google Scholar]
- Press VG, Arora VM, Shah LM, Lewis SL, Ivy K, Charbeneau J, et al. Misuse of respiratory inhalers in hospitalized patients with asthma or COPD. Journal of General Internal Medicine. 2011;26(6):635–642. doi: 10.1007/s11606-010-1624-2. http://doi.org/10.1007/s11606-010-1624-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Press VG, Matthiesen MI, Ranadive A, Hariprasad SM, Meltzer DO, Arora VM. Insights into inpatients with poor vision: A high value proposition. Journal of Hospital Medicine. 2015;10(5):311–313. doi: 10.1002/jhm.2342. http://doi.org/10.1002/jhm.2342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Press VG, Arora VM, Lewis SL, Charbeneau J, Starkey J, Naureckas ET, et al. Teaching the Use of Respiratory Inhalers to Hospitalized Patients with Asthma or COPD: A Randomized Trial (TURI) J Gen Intern Med. 2012;27(10):1317–1325. doi: 10.1007/s11606-012-2090-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Press VG, Shapiro MI, Mayo AM, Meltzer DO, Arora VM. More than meets the eye: relationship between low health literacy and poor vision in hospitalized patients. Journal of Health Communication. 2013;18(Suppl 1):197–204. doi: 10.1080/10810730.2013.830346. http://doi.org/10.1080/10810730.2013.830346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Press VG, Arora VM, Trela KC, Adhikari R, Zadravecz FJ, Liao C, Naureckas T, White SR, Meltzer DM, Krishnan JA. Effectiveness of Teaching Respiratory Inhaler Technique (ETRAIN): A Randomized Trial. AnnalsATS. doi: 10.1513/AnnalsATS.201509-603OC. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Public health and aging: Trends in aging—united states and worldwide JAMA. 2003;289(11):1371–1373. http://doi.org/10.1001/jama.289.11.1371. [PubMed] [Google Scholar]
- Rowe S, MacLean CH. Quality Indicators for the Care of Vision Impairment in Vulnerable Elders. Journal of the American Geriatrics Society. 2007;55:S450–S456. doi: 10.1111/j.1532-5415.2007.01355.x. http://doi.org/10.1111/j.1532-5415.2007.01355.x. [DOI] [PubMed] [Google Scholar]
- Scott IU, Schein OD, West S, Bandeen-Roche K, Enger C, Folstein MF. Functional status and quality of life measurement among ophthalmic patients. Archives of Ophthalmology (Chicago, Ill.: 1960) 1994;112(3):329–335. doi: 10.1001/archopht.1994.01090150059023. [DOI] [PubMed] [Google Scholar]
- Sudore RL, Yaffe K, Satterfield S, Harris TB, Mehta KM, Simonsick EM, Newman AB, et al. Limited Literacy and Mortality in the Elderly: The Health, Aging, and Body Composition Study. Journal of General Internal Medicine. 2006;21(8):806–812. doi: 10.1111/j.1525-1497.2006.00539.x. doi:10.1111/j.1525-1497.2006.00539.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services . A Profile of Older Americans: 2014. Administration on Aging, Administration for Community Living; 2014. [Google Scholar]
- Wallston KA, Cawthon C, McNaughton CD, Rothman RL, Osborn CY, Kripalani S. Psychometric Properties of the Brief Health Literacy Screen in Clinical Practice. Journal of General Internal Medicine. 2014;29(1):119–126. doi: 10.1007/s11606-013-2568-0. doi:10.1007/s11606-013-2568-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- West SK, Munoz B, Rubin GS, Schein OD, Bandeen-Roche K, Zeger S, Fried LP. Function and visual impairment in a population-based study of older adults. The SEE project. Salisbury Eye Evaluation. Investigative Ophthalmology & Visual Science. 1997;38(1):72–82. [PubMed] [Google Scholar]