Abstract
Onychomycosis is the most prevalent onychopathy and it requires a correct early diagnosis. Currently, the diagnostic gold standard is the association of direct mycological test with culture; however, it shows variable sensitivity. The histopathological examination of the distal nail plate, called clipping, has shown to be an adjuvant in diagnosing onychomycosis. This is an easy-to-perform, relatively cheap examination that is little dependent of the examiner, rapidly provides results, has high sensitivity, and for patients it is painless and harmless.
Keywords: Diagnosis, Nail diseases, Onychomycosis, Pathology, Periodic acid-Schiff reaction
Onychomycosis accounts for 50% of nail diseases, being considered as the most prevalent one; its clinical presentation is variable and may be mistaken for other nail diseases.1
The correct diagnosis is a must, as it requires long, expensive treatment with possible adverse effects, such as elevation of hepatic enzymes and drug interactions. Furthermore, a late diagnosis may lead to temporary or permanent nail dystrophy.
Currently, the diagnostic gold standard is the association of direct mycological test with culture. This association, however, results in a minimum of 30% false negatives and shows sensitivity varying from 25% and 80%.2
The direct mycological test depends on an adequate sample collection as well as the examiner, and it can be tampered with materials that mimic fungal structures, such as fibers, air bubbles, and fat droplets.3 The culture has high specificity, but it is time-consuming (three to six weeks) and dependent on an appropriate medium, the temperature conditions, and the existence of viable fungus. Contamination by bacteria and other opportunistic fungi may compromise the correct diagnosis.
Histological examination of distal nail plate with periodic acid–Schiff (PAS) has shown to be an option when diagnosing onychomycosis. The result is rapid (24 to 48 hours) and little dependent on the examiner. In addition, there are few factors that could generate false positives, such as starch particles, serum, and parakeratotic cells.4
The histological examination's higher sensitivity to detect fungal infection was demonstrated as early as in the first study of nail clipping––conducted in 1948––that compared it with the direct mycological test and culture.5
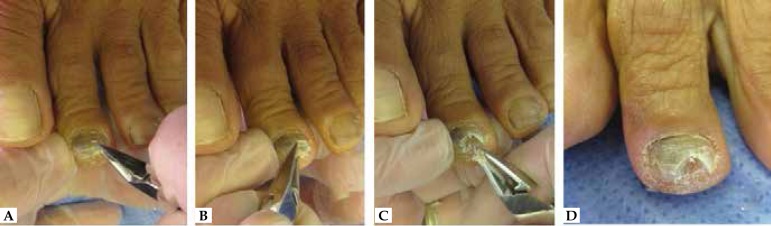
The clipping technique is simple and painless. With the help of a nipper, a fragment of at least 5 mm longitudinally and 2 mm transversely of the affected nail is cut for an adequate fragment fixation in paraffin (Figure 1).6
Figure 1.
A, B, and C. Nail clipping technique with the use of nipper in order to cut distal nail plate of the left second toe. D. “V-like” nail after procedure
The extracted specimen may be placed in a formaldehyde solution or a dry container. When processing this specimen, a chitin-softening or Tween solution may be used.6,7
There seems to be no difference between methods with and without fixation using formaldehyde in terms of difficulty to cut the paraffin and to prepare and stain the microscope blades.4
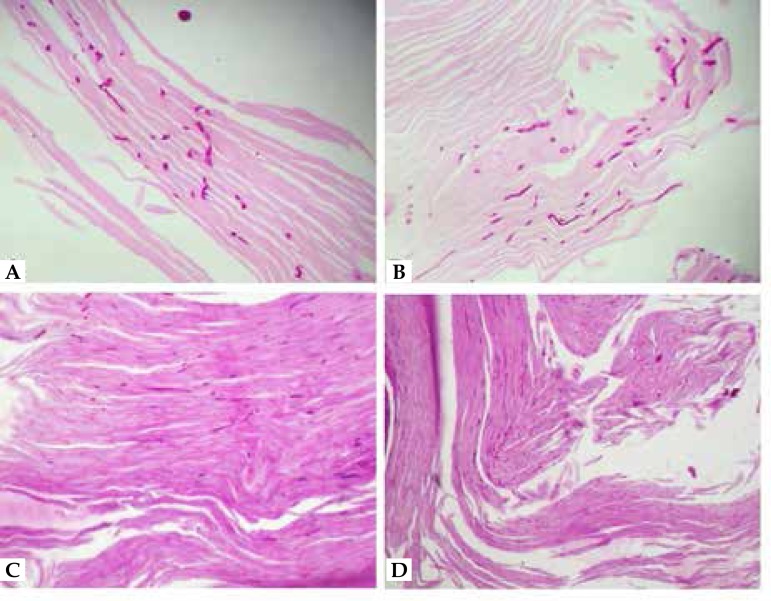
When evaluating onychomycosis with PAS, the hypha is usually spotted in the ventral nail plate or subungual hyperkeratosis (Figure 2). Chang et al. looked at the isolated subungual hyperkeratosis of the plate and found that the diagnosis of onychomycosis was possible in 97% of the cases, suggesting the need of plate processing in 3% of the cases only.8
Figure 2.
A and B. View of chambered, regular and eosinophilic hyphae, through lateral (linear) and frontal (punctate) sections in subungual hyperkeratosis (PAS, 400x). C and D. Parakeratosis and regular eosinophilic hyphae, distributed in the plate and subungual material (PAS, 200x) are observed
The presence of chambered, uniform hyphae invading the nail plate suggests infection by dermatophytes (Figure 2). Hyphae with thicker, irregular walls represent non-dermatophytes fungi. Conidia in the ventral face of the plate––especially when accompanied by sprouts and pseudo-hyphae––point out to infection by candida. Hyphae with degenerated appearance and isolated arthroconidia may occur as a result of previously used antifungal drugs. In this case, in addition to PAS, methenamine silver (Grocott's) staining may be necessary.6
Several studies reported that clipping with PAS has higher sensitivity in detecting onychomycosis when compared to the gold standard as well as in differentiating colonization from the infection per se by virtue of the finding of fungi invading the nail plate.5,7,9,10
Wilsmann-Theis et al. found that PAS is the method with the highest sensitivity to detect fungal elements in nail specimens, especially in cases with pre-diagnosis antifungal treatment.7
A diagnostic algorithm was then proposed. Upon clinical suspicion of onychomycosis, a direct mycological test is performed because it is quicker and cheaper. In case of a positive result, a culture is carried out in order to identify the agent; if negative, the test is repeated. If the negative result is confirmed, a histopathological examination of the nail using PAS staining and fungi culture are indicated.10
Nail clipping must be considered because it is an easy-to-perform, relatively cheap examination, that is little dependent of the examiner, rapidly provides results, has high sensitivity, and for patients it is painless and harmless. It has a role in the differential diagnosis between fungal colonization and infection and it also points out characteristics of other potentially associated nail dystrophies. It is useful when following up and diagnosing patients that are on antifungal treatment as well as in cases for which several direct examinations and cultures have been negative despite the persistent clinical suspicion.
Inadequate collection, insufficient specimens, and the impossibility of etiological identification of the fungus are limiting factors of the method; however, its association with other methods broadens its diagnostic sensitivity.
Footnotes
Conflict of Interest: None
Financial Support: None
Work performed at Hospital do Servidor Público Municipal de São Paulo (HSPM-SP) – São Paulo (SP), Brazil.
REFERENCES
- 1.Effendy I, Lecha M, Feuilhade de Chauvin M, Di Chiacchio N, Baran R, European Onychomycosis Observatory Epidemiology and clinical classification of onychomycosis. J Eur Acad Dermatol Venereol. 2005;19:8–12. doi: 10.1111/j.1468-3083.2005.01281.x. [DOI] [PubMed] [Google Scholar]
- 2.Gupta AK, Simpson FC. Diagnosing onychomycosis. Clin Dermatol. 2013;31:540–543. doi: 10.1016/j.clindermatol.2013.06.009. [DOI] [PubMed] [Google Scholar]
- 3.Achten G, Wanet-Rouard J. Onychomycoses in the laboratory. Mykosen. 1978;23:125–127. [PubMed] [Google Scholar]
- 4.Werner B, Antunes A. Microscopic examination of normal nail clippings. Dermatol Pract Concept. 2013;3:9–14. doi: 10.5826/dpc.0303a04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sagher F. Histologic examinations of fungous infections of the nails. J Invest Dermatol. 1948;11:337–357. [PubMed] [Google Scholar]
- 6.Fillus J, Neto, Tchornobay AM. How the nail clipping helps the dermatologist. An Bras Dermatol. 2009;84:173–176. doi: 10.1590/s0365-05962009000200010. [DOI] [PubMed] [Google Scholar]
- 7.Wilsmann-Theis D, Sareika F, Bieber T, Schmid-Wendtner MH, Wenzel J. New reasons for histopathological nail-clipping examination in the diagnosis of onychomycosis. J Eur Acad Dermatol Venereol. 2011;25:235–237. doi: 10.1111/j.1468-3083.2010.03704.x. [DOI] [PubMed] [Google Scholar]
- 8.Chang A, Wharton J, Tam S, Kovich OI, Kamino H. A modified approach to the histologic diagnosis of onychomycosis. J Am Acad Dermatol. 2007;57:849–853. doi: 10.1016/j.jaad.2007.05.015. [DOI] [PubMed] [Google Scholar]
- 9.Jeelani S, Ahmed QM, Lanker AM, Hassan I, Jeelani N, Fazili T. Histopathological examination of nail clippings using PAS staining (HPE-PAS) gold standard in diagnosis of Onychomycosis. Mycoses. 2015;58:27–32. doi: 10.1111/myc.12251. [DOI] [PubMed] [Google Scholar]
- 10.Jung MY, Shim JH, Lee JH, Lee JH, Yang JM, Lee DY, et al. Comparison of diagnostic methods for onychomycosis, and proposal of a diagnostic algorithm. Clin Exp Dermatol. 2015;40:479–484. doi: 10.1111/ced.12593. [DOI] [PubMed] [Google Scholar]