Abstract
Background: Evidence regarding inflammatory pathways, elevated cardiovascular risk, and negative effects of secondary conditions on disability progression provide a strong rationale for promoting multiple health behaviors in adults with multiple sclerosis (MS). However, many unanswered questions remain about the best ways to design multiple behavior change interventions for adults with MS. We sought to identify facilitators and barriers to engaging in multiple health behaviors (physical activity, nutrition, and sleep) and to gain further insights into how to develop multiple health behavior change interventions based on preferences of adults with MS.
Methods: Focus groups and one-on-one interviews were conducted with 17 participants with MS.
Results: Five qualitative themes were identified as either facilitating or hindering engagement in multiple health behaviors: 1) roles, priorities, and preferences; 2) sense of duty; 3) the fatigue and mobility problem; 4) taking control; and 5) resiliency. Participants identified advantages and disadvantages of delivery formats (eg, face-to-face group vs. telephone), frequency of contacts, and intervention strategies based on their individual circumstances and obligations. Participants felt that discussing the benefits of engaging in multiple health behaviors, developing action plans, accommodating preferences, and addressing health problems would be helpful strategies to include in a multiple behavior change intervention.
Conclusions: These findings indicate that there may be common facilitators and barriers that can be targeted to promote multiple behavior changes. Future research should explore the best ways to tailor multiple behavior change interventions to preferences, symptoms, psychological traits, and social cognitions.
There is now an extensive body of research indicating the need to develop and test multiple health behavior change interventions in people with multiple sclerosis (MS). Research on inflammatory pathways,1 elevated cardiovascular risks,2 and negative effects of secondary conditions on disability progression3 all provide a strong rationale for designing and testing multiple behavior change interventions in adults with MS. Engaging in multiple health behaviors may have cumulative effects on reducing inflammation and secondary conditions.1,4 Furthermore, expert consensus statements on managing common MS symptoms often make recommendations consistent with engaging in multiple health behaviors.5,6 However, few studies of people with MS have addressed pertinent questions on how best to promote multiple health behavior changes.
Although behavior change interventions have been examined in people with MS, the efficacy and theoretical underpinnings of these interventions to support multiple behavior changes are unclear. Behavior change intervention research in MS has typically focused on self-managing symptoms, promoting wellness, and encouraging physical activity.7–9 Each of these types of interventions makes implicit assumptions about promoting engagement in multiple health behaviors. Self-management interventions typically focus on teaching skills, such as problem-solving and decision making, that are relevant to promoting engagement in single or multiple behaviors to manage single or multiple symptoms.10 Wellness interventions typically emphasize holistic approaches and encourage engagement in multiple health behaviors simultaneously.8 Alternatively, physical activity interventions focus on targeting cognitions and skills specific to physical activity or behaviors interfering with engagement in physical activity.9 Because wellness, self-management, and physical activity interventions rarely focus on the linkages between multiple behaviors, there remain many unanswered questions about the best ways to design multiple health behavior change interventions for adults with MS.
Given the complexity and dearth of research on approaches to designing multiple behavior change interventions, a qualitative research approach is warranted. Qualitative methods are often used as a first step in understanding complex human behaviors.11 The two purposes of this study were 1) to identify facilitators and barriers to engaging in multiple health behaviors and 2) to gain further insights into how to develop multiple health behavior change interventions based on preferences of adults with MS. We focused on physical activity, nutrition, and sleep because of their possible synergetic effects in self-managing common symptoms of MS and because of their importance in achieving energy balance to reduce the risks of developing secondary conditions.1,4–6
Methods
Overview
Focus groups and one-on-one telephone interviews were conducted in the same 17 participants with MS. The results of each data collection method were used to corroborate, elaborate on, and explain the results of the other data collection method. Specifically, the focus groups were designed to elicit overall narratives about engaging in physical activity, nutrition, and sleep and their interrelatedness. The one-on-one telephone interviews were designed to elicit further details about facilitators and barriers to engaging in healthy behaviors and to elicit preferences about participating in a multiple behavior change intervention. An institutional review board approved the research protocol.
Participants
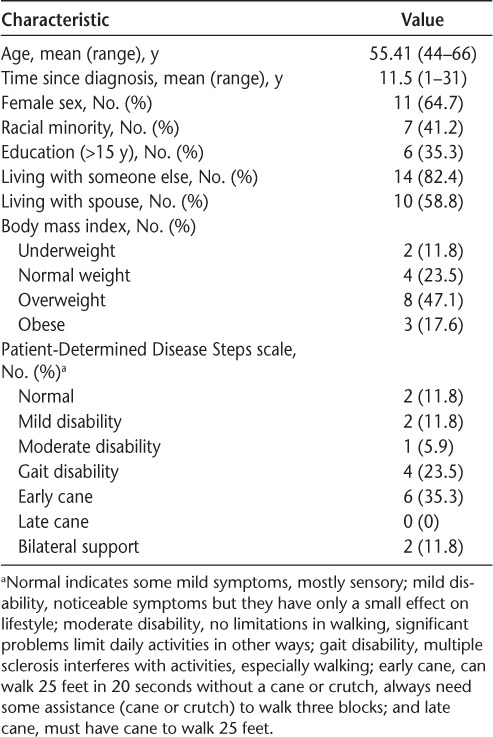
The study inclusion criteria included a self-reported diagnosis of MS, the ability to communicate over the telephone, and age older than 18 years. Participants were recruited via flyers distributed at support groups and National Multiple Sclerosis Society events. The sociodemographic characteristics and self-reported body mass index of the 17 participants are reported in Table 1.
Table 1.
Characteristics of the 17 study participants
Data Collection Methods
Focus Groups
The focus groups helped provide an overall framework for exploring themes in more detail during the one-on-one telephone interviews. Three focus groups of five to six participants each were conducted. The sessions lasted approximately 2 hours and were conducted by the first author (MAP) while a research assistant took notes. The focus groups consisted of two types of open-ended questions to elicit narratives: 1) questions specific to engaging in physical activity, nutrition, and sleep and 2) questions about the interrelatedness of health behaviors.
Questions specific to each behavior addressed the perceptions about engaging in the behavior, whether it was a priority for participants, and the benefits and disadvantages of engaging in that behavior. To help identify facilitators and barriers, we first asked participants to describe their experiences with engaging in the behavior and then probed specifically about how their MS and surrounding environment influenced engagement.
Questions about interrelatedness addressed which behaviors were pertinent to a healthy lifestyle, the relationship between health behaviors and quality of life, and standards and priorities for engaging in different health behaviors. Participants were asked whether they could provide specific examples of how health behaviors were interrelated, and whether they could think of common factors that facilitated or hindered engagement across multiple health behaviors.
When transitioning to a different topic during focus group interviews, the first author would summarize areas of consensus and disagreement and then ask for further input. This input was useful during the interim analysis in helping refine the interview guide and identifying themes. For example, in the third focus group, questions were revised to elaborate on possible themes about the relationship between coping strategies and engaging in health behaviors.
One-on-One Interviews
The one-on-one telephone interviews were primarily conducted to accomplish the second purpose of the study (to gain further insights into how to develop multiple health behavior change interventions based on preferences of adults with MS) and to confirm and elaborate on possible facilitators and barriers identified in the focus groups. A trained research assistant called all 17 participants 3 to 4 weeks after their focus group. The calls lasted approximately 45 minutes. At the beginning of the call, the research assistant read participants a summary of the interim analysis and then asked participants whether they agreed with the summary and whether they wanted to add anything. A definition of a multiple health behavior change intervention was also read to participants: “a health and wellness program designed to support people with MS to engage in a variety of healthy behaviors.” The one-on-one interviews primarily consisted of semi–open-ended questions and closed-ended questions about 1) facilitators and barriers specific to physical activity, nutrition, and sleep and 2) preferences for participating in a multiple behavior change intervention.
Participants were first asked to list facilitators and barriers specific to each behavior. We then asked them about the interrelatedness of facilitators and barriers across multiple health behaviors. Participants' lists and their answers about interrelatedness helped confirm findings from the focus groups. Additional questions were developed during the interim analyses, allowing us to elaborate on possible themes emerging from the focus groups. The additional questions were mainly about whether particular strategies were perceived to be helpful in overcoming barriers and about the perceived relationship between symptom progression/severity and engaging in health behaviors.
Questions about eliciting preferences focused on the educational content, frequency of interactions, delivery format, expectations of benefit, and behavior change strategies. Several of the questions were closed-ended; that is, participants were asked to rate attitudes and preferences on a Likert-type scale. Depending on the question, participants were asked to rate how helpful or how intrusive a particular delivery format or strategy would be on a scale from 0 (not intrusive or not helpful at all) to 10 (very intrusive or extremely helpful).
Content Analysis for Focus Groups and One-on-One Interviews
All the focus groups and telephone interviews were audio-recorded and transcribed verbatim. The content analysis was based on recommendations by Elo and Kyngas12 and consisted of an inductive-category and theme-development approach. We searched for overall patterns among the descriptive labels to identify clusters and to organize data into categories for both the focus groups and the one-on-one interviews. Each category was operationally defined to facilitate consistent coding of the data using Atlas.ti software, version 7 (Scientific Software Development GmbH, Berlin, Germany). We (MAP and MG) compared notes for the development of themes and then coded the data independently and discussed any disagreements until consensus was reached. When participants were asked to list preferences, categories were identified and coded and are reported as frequency counts (ie, how many participants said something consistent with that category). Attitudes rated on a Likert-type scale are reported as means.
To help ensure the integrity of the content analyses, we followed guidelines recommended by Shenton,13 which included collecting and analyzing data in an iterative process to identify themes; generating an audit trail (ie, conformability); rereading the focus group and one-on-one interview transcripts as a whole, as well as quotes in categories on multiple occasions (ie, dependability); conducting focus groups followed by one-on-one interviews (ie, member checks); and discussing disagreements until consensus was reached (ie, peer scrutiny).
Results
Qualitative Themes
Using the focus group and one-on-one interview data, we identified five themes that were described by participants as either facilitating or hindering engagement in multiple health behaviors: 1) roles, priorities, and preferences; 2) sense of duty; 3) the fatigue and mobility problem; 4) taking control; and 5) resiliency. We summarize these themes in the following subsections (and in Table 2) using exemplar quotes. Names of participants have been replaced with pseudonyms.
Table 2.
Summary of themes and subthemes
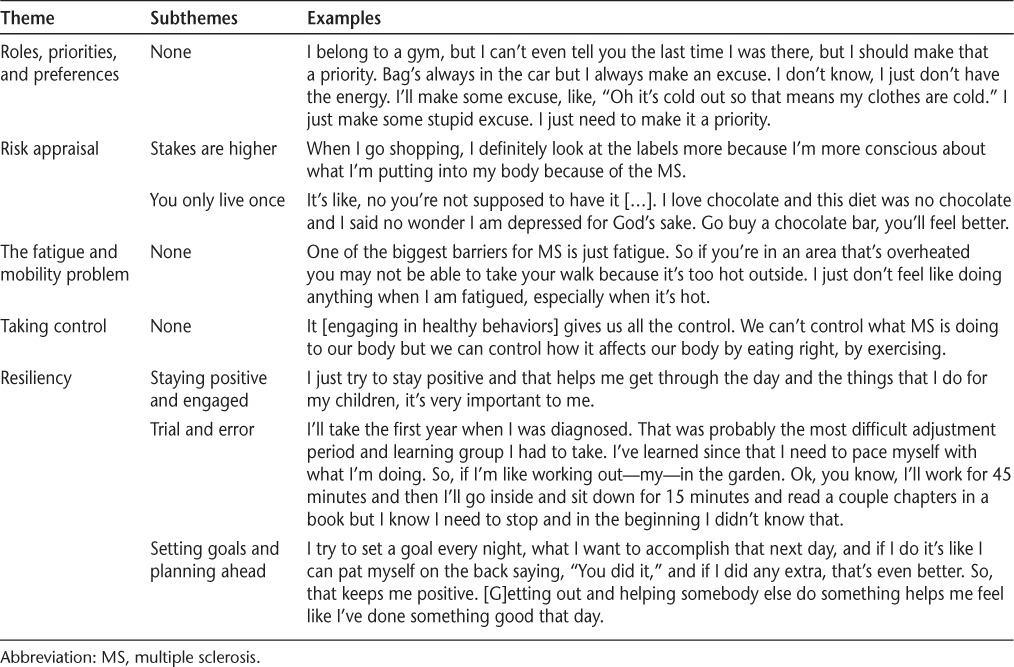
Theme 1: Roles, Priorities, and Preferences
Participants described social roles and preferences that either aligned with engaging in multiple health behaviors or resulted in prioritizing unhealthy behaviors over healthy behaviors. For example, several participants enjoyed attending group exercise classes because it kept them motivated to engage in physical activity and because it was an opportunity to receive health advice from other group members (eg, exchange healthy food recipes). Alternatively, several participants described having to fulfill parental obligations or take care of a loved one, resulting in prioritizing simple and convenient solutions that were often unhealthy. Preferences for unhealthy foods, watching TV, and staying up late were often cited as barriers. For example, George said, “It's so much easier to sit down and turn on the TV instead of going out and doing some work.”
Theme 2: Sense of Duty
Participants who were motivated to engage in multiple health behaviors often described feeling obligated or having a sense of “ought to” because of their MS. They felt that engaging in multiple health behaviors was a strategy to manage their symptoms and maintain their independence and was consistent with their self-identity. Many felt that it was more important to engage in healthy behaviors compared with people without MS. Michelle said, “When we don't do healthy behavior, eating right, exercising, staying social, things like that, it affects us even harder.” Alternatively, other participants noted that although engaging in healthy behaviors was important, it was equally important to enjoy life, and they felt obligated to “live life to its fullest.” This meant occasionally eating unhealthy foods, staying up late, or participating in sedentary activities. When Melissa was asked about difficulties engaging in healthy behaviors, she said, “So, today the solution for me as far as living with the MS is live this day to the fullest, because it might be my last day of independence because I never know when it's gonna come.”
Theme 3: The Fatigue and Mobility Problem
Fatigue and mobility problems were frequently described as interfering with engagement in multiple health behaviors. Fatigue resulted in unwanted sleeping or a desire to prioritize rest and sedentary behaviors. Fatigue also resulted in decreased motivation to plan and cook healthy meals and go grocery shopping. Mobility impairments and balance problems made participants worry about whether they could cook a meal safely and whether they could walk outside without falling. Tim said, “If it won't go in the microwave, forget it […] the bad thing for me is I pretty much have one hand that works. So everything I do, I have to be able to do it one-handed.” Melissa said, “If you walk around the neighborhood, I'm constantly having to be looking at the ground, making sure I'm not tripping over something. I'm not very good with uneven surfaces.”
Alternatively, some participants noted that fatigue and mobility problems motivated them to be engaged in multiple health behaviors. Some participants described eating less red meat, reducing portion sizes, or consuming fewer sugary foods because they noted that eating unhealthily increased fatigue levels. Chris said, “I know that the fatigue wipes me out. So when I eat right I'm not as fatigued as I used to be, you know, […] when I'm eating better, I don't get fatigued.” Other participants noted the importance of walking to maintain mobility and independence. The desire not to be a burden on family members or to become dependent on others was cited as a motivator to engage in health behaviors.
Theme 4: Taking Control
Engaging in multiple health behaviors was viewed as a strategy to take control over an unpredictable disease course. Ryan said, “I want to be able to walk as long as I can. So that means I have to eat healthy in order to have some control of what's going on. I don't want MS to control me. I just have this disease I have to control and by my eating habits and my other behaviors, you know, exercise, walking, I have control over it.”
Many participants found it challenging to cope with the prospect of not being able to walk and declining cognitive function. Thus, participants who believed they could take actions to control functional declines (ie, locus of control) were often motivated to engage in multiple health behaviors. Participants described prioritizing a particular health behavior over another health behavior because they believed that the first health behavior was more beneficial in preventing functional declines.
Theme 5: Resiliency
Participants motivated to engage in multiple health behaviors often described strategies consistent with being resilient. For example, Robert said, “I have the MS but MS doesn't have me.” Staying positive and engaged, persisting via trial and error, and setting goals and planning ahead helped people cope with the symptoms of MS and facilitated involvement in multiple health behaviors. Several participants noted the importance of staying positive by maintaining engagement in leisure activities, volunteering, and setting and achieving goals regardless of their health problems. Kathryn said, “Staying active with people and not putting yourself in isolation, staying social […] is important in coping.” Accomplishing health-related goals increased confidence to try new things and accomplish more ambitious goals. Many participants described an ongoing trial-and-error process toward achieving their goals and being realistic about what can be accomplished within the constraints of their limitations. Participants recognized that maintaining a healthy lifestyle often involved planning ahead. Joe said, “Focusing on what you need to do next. It's gathering your thoughts. Organizing before you do things. You didn't used to have to do that before you became sick. Every time you leave the house, you have to think about where you're going, what you're going to be doing. And so, just like going to the mall, do I use the scooter, or not? […] You have to organize your life at a level of detail you never had to before. […] That's my coping strategy.”
Attitudes and Preferences About Multiple Behavior Change Interventions
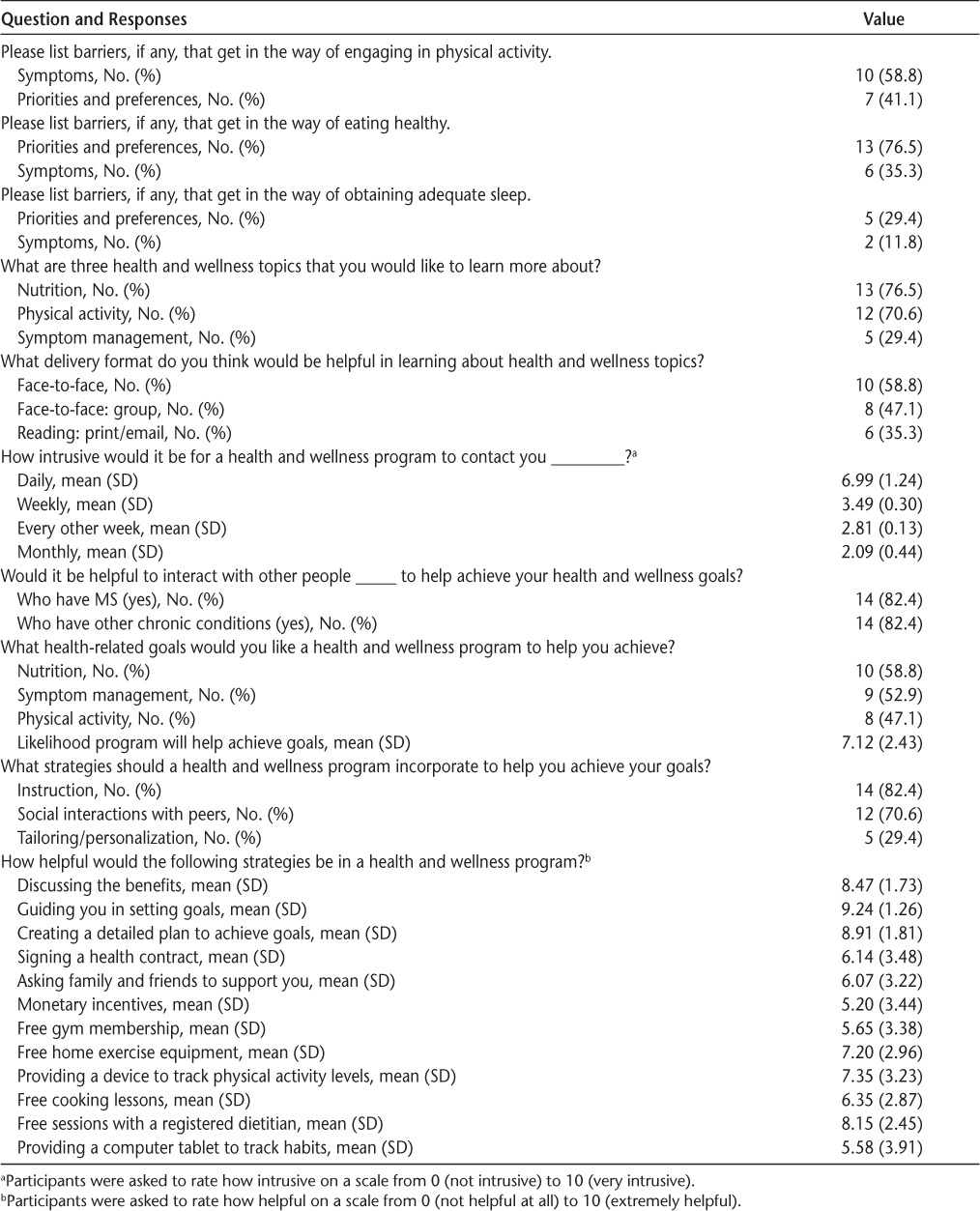
Responses to closed-ended questions are presented in Table 3. We found a variety of topics that participants wanted to learn about and a variety of goals that they wanted to achieve based on their unique circumstances. For example, when we probed participants about whether weight management strategies should be included in a health and wellness program, responses depended on whether the participant perceived that they were overweight and on whether they had a desire to lose weight. Participants also preferred a variety of different delivery formats, but most agreed that weekly or every-other-week intervention contacts would not be too intrusive. Participants thought it would be useful to interact and learn from people with and without MS. Several participants felt that education about the benefits of engaging in health behaviors, guidance in setting and achieving goals, sessions with a dietitian, and free home exercise equipment and devices to track physical activity levels would be helpful to include in a health and wellness program. Participants thought it would be less helpful to include monetary incentives, gym memberships, and health contract signings.
Table 3.
Preferences for engaging in a multiple health behavior change intervention
Discussion
Despite the growing body of research examining linkages between health behaviors in healthy adults,14 such studies in adults with disabling conditions are scarce.15 Important findings from this study include the identification of possible factors to target when designing multiple behavior change interventions and the heterogeneity in preferences for participating in such an intervention. The present findings indicate that there may be common facilitators and barriers that can be targeted to promote multiple behavior changes. Given the heterogeneity in preferences for participating in a multiple behavior change intervention, future research should examine how best to tailor such interventions.
Addressing Purpose 1
Even in research with healthy adults, theories about how to promote multiple health behaviors are still in their formative stages. Noar et al.16 suggest that one way to conceptualize and understand engagement in multiple behaviors is to identify global perceptions that influence multiple behaviors. Consistent with this suggestion, we found that perceptions toward fatigue and mobility problems, sense of duty, beliefs about being able to control MS, and resiliency might help facilitate engagement in multiple health behaviors. The present findings are consistent with studies of single health behaviors in adults with disabling conditions, which also helps support the notion that there may be global perceptions that can be targeted to promote multiple behavior changes.
Not surprisingly,17,18 fatigue and mobility problems were often cited as a barrier to engaging in physical activity and healthy eating. However, perceptions that fatigue was linked with particular eating habits resulted in motivation to problem-solve and find solutions that would facilitate eating healthier. Perceptions that physical activity could prevent further declines in mobility and loss of independence helped motivate participants to engage in physical activity. Putnam et al.19 found in a qualitative study of adults with disabilities that perceptions of personal development also motivated engagement in health behaviors. Thus, a possible intervention strategy is cultivating perceptions that engagement in multiple health behaviors is synergistic in achieving outcomes that are valued by the individual.
Those who prioritized engagement in multiple health behaviors often felt obligated (ie, sense of duty) because of their MS, felt that it was a way to take control of their MS, and perceived it as being a part of their self-identity. Previous research in individuals with MS has indicated that an internal locus of control (ie, believing that one can influence events and their outcomes) may be associated with treatment adherence, disability, and symptoms.20 We found in a previous study of people with MS that self-identity was a strong independent correlate (β = 0.44) of physical activity behavior and was influenced by participating in a group wellness intervention.21 Future research should examine whether promoting an internal locus of control, a sense of duty, and a self-identity consistent with the notion of wellness can promote multiple behavior changes in adults with MS.
We also found that participants motivated to engage in multiple health behaviors often noted the importance of staying positive and engaged, persisting via trial and error, and setting goals and planning ahead. Ploughman et al.18 found in a study of older adults with MS that persistence was a significant predictor of exercise participation even when controlling for fatigue and mobility impairments. The present findings are also consistent with those of studies on coping, resiliency, and optimism22 as well as meta-analyses on the effectiveness of setting goals.23 Resilience and optimism are considered to be positive psychological constructs and may be interrelated traits that facilitate coping with chronic disabling conditions.22 Research is warranted on whether interventions developed via a positive psychology paradigm have utility in promoting multiple health behavior changes.
Addressing Purpose 2
Consistent with other studies that have examined preferences for participating in behavior change interventions among adults with disabling conditions,24,25 we found that participants identified advantages and disadvantages in topics, delivery format, dosing, and intervention strategies based on their individual circumstances and obligations resulting from different social roles. Unfortunately, the optimal delivery formats, frequency of contacts, and intervention strategies to use based on a participant's unique circumstances and preferences are unknown. Comparative effectiveness research on optimal delivery formats, frequency of contacts, and intervention strategies remains inconclusive, and few studies have examined how best to accommodate preferences to improve outcomes.26,27 Although there are several examples of formative research to develop behavior change interventions in adults with disabling conditions, most interventions are developed using consensus agreement derived from focus groups or means derived from a survey. A drawback to this approach is that it may ignore variability in preferences and, therefore, may decrease enthusiasm to participate in the intervention.
Accommodating participants' preferences in a multiple behavior change intervention may improve outcomes, particularly in people with MS. In a comparative study across different chronic conditions, Hamann et al.28 found that people with MS were significantly more likely to prefer making active, shared decisions with health-care professionals. Accommodating preferences may help foster autonomy and a sense of volition, which, in turn, can promote intrinsic motivation to engage in multiple health behaviors.29 However, the challenge is deciding which preferences should be accommodated. Glasgow et al.30 suggested that providing participants with opportunities to set priorities in choosing which health behaviors to focus on would result in better outcomes. Providing participants with opportunities to choose which health behaviors to prioritize could help avoid the scenario where participants view topics as irrelevant.31 Furthermore, it may help address one of the potential disadvantages of a multiple behavior change intervention, that is, overwhelming participants, because it would focus efforts on only the behaviors that the participant is ready and willing to change.
Limitations
This study has limitations that are inherent in qualitative research methods. It is unknown whether these findings are generalizable to others in similar circumstances, that is, community-dwelling adults with mild-to-moderate symptoms of MS. Furthermore, participants may have had a particular interest in learning about health and wellness topics that may not reflect the population with MS. Purposefully selecting participants who were unmotivated to engage in healthy behaviors could have helped reduce selection bias. Last, conducting one-on-one in-person interviews rather than one-on-one telephone interviews could have helped establish a better rapport with the participants, which may have facilitated obtaining a richer and more detailed narrative.
Conclusion
There are many challenges inherent in determining the optimal approach to changing multiple health behaviors in adults with MS. Disciplinary silos have been created in MS research that have resulted in a growing focus on developing and testing behavior change interventions that target a particular symptom or signal behavior. Furthermore, several methodological problems arise when evaluating a multiple behavior change intervention with several primary behavioral outcomes, for example, heterogeneity in adherence across multiple behaviors, familywise error, and measurement burden. The diversity in symptoms, uncertainty in disease progression, and differences in psychological characteristics all present challenges that may need to be addressed when designing a multiple behavior change intervention for adults with MS.
PracticePoints
There is now an extensive body of research indicating the need to encourage multiple health behaviors in adults with MS.
Participants felt that discussing the benefits of engaging in multiple health behaviors, developing action plans, accommodating preferences, addressing fatigue and mobility problems, and talking to health experts about their specific needs would be helpful strategies to include in a multiple behavior change intervention.
Participants motivated to engage in multiple health behaviors described it as a strategy to take control of their MS and noted the importance of staying positive and engaged, persisting via trial and error, and setting goals and planning ahead.
Footnotes
Financial Disclosures: The authors have no conflicts of interest to disclose.
Funding/Support: This work was supported by the National Institute of Nursing Research of the National Institutes of Health (grant K01NR012975).
Disclaimer: The information presented in this article does not necessarily reflect the position, ideas, or opinions of the National Institutes of Health.
References
- 1. Riccio P, Rossano R. Nutrition facts in multiple sclerosis. ASN Neuro. 2015; 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wens I, Dalgas U, Stenager E, Eijnde BO. Risk factors related to cardiovascular diseases and the metabolic syndrome in multiple sclerosis: a systematic review. Mult Scler. 2013; 19: 1556– 1564. [DOI] [PubMed] [Google Scholar]
- 3. Marrie RA, Horwitz RI. Emerging effects of comorbidities on multiple sclerosis. Lancet Neurol. 2010; 9: 820– 828. [DOI] [PubMed] [Google Scholar]
- 4. Sabia S, Singh-Manoux A, Hagger-Johnson G, Cambois E, Brunner EJ, Kivimaki M. Influence of individual and combined healthy behaviours on successful aging. CMAJ. 2012; 184: 1985– 1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Expert opinion paper: Management of MS-related fatigue. National Multiple Sclerosis Society website. http://www.nationalmssociety.org/NationalMSSociety/media/MSNationalFiles/Brochures/Clinical_Bulletin_MS-Related-Fatigue.pdf. Published 2006. Accessed October 1, 2015.
- 6. Bennett S, Bethoux F, Brown T, et al. Comprehensive management of mobility impairment and complex symptoms in multiple sclerosis: a focus on walking. Int J MS Care. 2014; 16( suppl 1): 1– 11. 24688349 [Google Scholar]
- 7. Plow M, Finlayson M, Rezac M. A scoping review of self-management interventions for adults with multiple sclerosis. PM R. 2011; 3: 251– 262. [DOI] [PubMed] [Google Scholar]
- 8. Stuifbergen AK. Building health promotion interventions for persons with chronic disabling conditions. Fam Community Health. 2006; 29( suppl): 28S– 34S. [DOI] [PubMed] [Google Scholar]
- 9. Motl RW. Lifestyle physical activity in persons with multiple sclerosis: the new kid on the MS block. Mult Scler. 2014; 20: 1025– 1029. [DOI] [PubMed] [Google Scholar]
- 10. Lorig KR, Holman H. Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med. 2003; 26: 1– 7. [DOI] [PubMed] [Google Scholar]
- 11. Patton MQ. Qualitative Research. Hoboken, NJ: Wiley Online Library; 2005. [Google Scholar]
- 12. Elo S, Kyngas H. The qualitative content analysis process. J Adv Nurs. 2008; 62: 107– 115. [DOI] [PubMed] [Google Scholar]
- 13. Shenton AK. Strategies for ensuring trustworthiness in qualitative research projects. Educ Inform. 2004; 22: 63– 75. [Google Scholar]
- 14. Prochaska JO. Multiple health behavior research represents the future of preventive medicine. Prev Med. 2008; 46: 281– 285. [DOI] [PubMed] [Google Scholar]
- 15. Plow MA, Moore S, Husni ME, Kirwan JP. A systematic review of behavioural techniques used in nutrition and weight loss interventions among adults with mobility-impairing neurological and musculoskeletal conditions. Obes Rev. 2014; 15: 945– 956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Noar SM, Chabot M, Zimmerman RS. Applying health behavior theory to multiple behavior change: considerations and approaches. Prev Med. 2008; 46: 275– 280. [DOI] [PubMed] [Google Scholar]
- 17. Plow M, Resnik L, Allen SM. Exploring physical activity behaviour of persons with multiple sclerosis: a qualitative pilot study. Disabil Rehabil. 2009; 31: 1652– 1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ploughman M, Harris C, Wallack E, Drodge O, Beaulieu S, Mayo N. Predictors of exercise participation in ambulatory and non-ambulatory older people with multiple sclerosis. PeerJ. 2015; 3: e1158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Putnam M, Geenen S, Powers L, Saxton M, Finney S, Dautel P. Health and wellness: people with disabilities discuss barriers and facilitators to well being. J Rehabil. 2003; 69: 37– 45. [Google Scholar]
- 20. Bragazzi NL. The gap in the current research on the link between health locus of control and multiple sclerosis: lessons and insights from a systematic review. Mult Scler Int. 2013; 2013: 972471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Plow M, Mathiowetz V, Resnik L. Multiple sclerosis: impact of physical activity on psychosocial constructs. Am J Health Behav. 2008; 32: 614– 626. [DOI] [PubMed] [Google Scholar]
- 22. Martz E, Livneh H. Psychosocial adaptation to disability within the context of positive psychology: findings from the literature. J Occup Rehabil. 2016; 26: 4– 12. [DOI] [PubMed] [Google Scholar]
- 23. Conn VS, Hafdahl AR, Brown SA, Brown LM. Meta-analysis of patient education interventions to increase physical activity among chronically ill adults. Patient Educ Couns. 2008; 70: 157– 172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Rabin C, Simpson N, Morrow K, Pinto B. Intervention format and delivery preferences among young adult cancer survivors. Int J Behav Med. 2013; 20: 304– 310. [DOI] [PubMed] [Google Scholar]
- 25. Eames S, Hoffmann T, Worrall L, Read S. Delivery styles and formats for different stroke information topics: patient and carer preferences. Patient Educ Couns. 2011; 84: e18– e23. [DOI] [PubMed] [Google Scholar]
- 26. Hartmann-Boyce J, Johns DJ, Jebb SA, Aveyard P. Effect of behavioural techniques and delivery mode on effectiveness of weight management: systematic review, meta-analysis and meta-regression. Obes Rev. 2014; 15: 598– 609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kiesler DJ, Auerbach SM. Optimal matches of patient preferences for information, decision-making and interpersonal behavior: evidence, models and interventions. Patient Educ Couns. 2006; 61: 319– 341. [DOI] [PubMed] [Google Scholar]
- 28. Hamann J, Neuner B, Kasper J, et al. Participation preferences of patients with acute and chronic conditions. Health Expect. 2007; 10: 358– 363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ryan RM, Deci EL. Self-regulation and the problem of human autonomy: does psychology need choice, self-determination, and will? J Pers. 2006; 74: 1557– 1585. [DOI] [PubMed] [Google Scholar]
- 30. Glasgow RE, Goldstein MG, Ockene JK, Pronk NP. Translating what we have learned into practice: principles and hypotheses for interventions addressing multiple behaviors in primary care. Am J Prev Med. 2004; 27( suppl): 88– 101. [DOI] [PubMed] [Google Scholar]
- 31. Kreuter M. Tailoring Health Messages: Customizing Communication with Computer Technology. Mahwah, NJ: Lawrence Erlbaum Associates; 2013. [Google Scholar]


