Abstract
Background
The potential need for an ostomy is a main concern for patients with inflammatory bowel disease. We performed this study to evaluate the impact of a long term ostomy (≥ 6 months duration) on the functional status and specific patient-reported outcomes (PRO) in a population of patients with Crohn’s disease (CD).
Methods
We performed a cross-sectional analysis within the CCFA Partners cohort Study. Bivariate analyses and logistic regression models were used to investigate associations between ostomy and various demographic, disease factors, and PROs for health related quality of life (HRQOL).
Results
A total of 402 CD patients with ostomy for a minimum duration of 6 months were compared to 4331 CD patients with no ostomy. Patients with ostomy were more likely to be in clinical remission compared to those without ostomy, 48.5% vs. 31.3%, respectively. Having an ostomy did not impact overall HRQOL and was not associated with anxiety, depression, sleep disturbances, or reduced sexual interest and satisfaction. However, the presence of ostomy was associated with reduced social role satisfaction in patients both with controlled and active disease. Additionally, in the subset of patients who did not achieve clinical remission, those with ostomy experienced greater pain interference (OR 1.63, 95% CI 1.12–2.35) and fatigue (OR 1.66 95% CI 1.15–2.39).
Conclusion
Ostomy is well-tolerated in CD patients, particularly when clinical remission is achieved.
Keywords: Quality of Life, Crohn’s disease, Ostomy
Introduction
Despite the recent advances in medical therapies, patients with Crohn’s disease (CD) continue to require surgical interventions at a high rate; with an estimated lifelong likelihood of surgery of up to 80%.1 This frequently entails the creation of either a temporary or a permanent stoma. About 10% of CD patients will need a permanent stoma at a certain stage of their disease course.1 The potential need for an ostomy is among the top concerns for patients with inflammatory bowel disease (IBD).2–7 This concern has been noted to be independent of disease subtype and severity and persisted when patients were assessed longitudinally over a one year period.7 Nevertheless, data about the actual impact of ostomy on IBD patients’ functional status and health related quality of life (HRQOL) are very limited. Furthermore, IBD patients with ostomies are frequently excluded from clinical research as many of the tools used to assess disease activity and HRQOL do not apply to this subpopulation (e.g. questions on bowel movement frequency).
A few studies have linked having a stoma to a number of adverse psychosocial outcomes including; depression and anxiety, increased loneliness, lowered self-esteem, poorer body image, and sexual disturbances.8–11 However, the majority of these studies were qualitative in nature and were not restricted to IBD patients. In fact, two of the above referenced studies were in non-IBD patients who required an ostomy for an underlying malignancy.9,11 IBD patients, who frequently suffer from severe and refractory disease prior to proceeding with surgery, may perceive living with an ostomy differently. For example, in a study by Nordin et al, evaluating HRQOL and psychosocial distresses in 492 IBD patients, of which 67 (14%) reported an ileostomy,12 patients with ileostomy had better social functioning, emotional functioning, and fewer bowel symptoms compared to those with ileoanal anastomosis. Furthermore, when compared to patients without ileostomy but with comparable disease extent, patients with ileostomies had similar levels of HRQOL and comparable anxiety and depression scores to those with no ileostomy.
In this study we aimed to assess the subset of CD patients within the Crohn’s and Colitis Foundation of America (CCFA) Partners cohort study who had an ostomy for a minimum duration of 6 months as compared to those patients with CD and no ostomy and to investigate the impact of ostomy on specific patient-reported outcomes (PROs) including anxiety; depression; fatigue; pain interference; sleep disturbances; social satisfaction; and sexual interest and satisfaction.
Materials and Method
Study Design
We performed a cross-sectional analysis of a subset of CD patients within the CCFA Partners cohort who had an ostomy for a minimum duration of 6 months
Study population
CCFA Partners is a longitudinal internet-based cohort of adult IBD patients, which has been ongoing since 2011. The development of the cohort has been previously described.13 In brief, following a baseline survey, participants are invited to complete follow-up surveys every 6 months. At baseline and at each follow-up interval, data on demographics, disease subtype and characteristics, medications, measures of disease activity, and various PROs are collected. All data are self-reported. Within this cohort, we identified our study population as all CD patients completing two surveys six or more months apart who reported either having or not having an ostomy at both time points (n=4733).
Study Variables
Disease activity was assessed using the Manitoba IBD Index (MIBDI). MIBDI is a validated, single-item, patient-defined disease activity measure.14 Patients are asked to select the statement that best describes their disease activity over the past six months from these categories: (a) constantly active, giving me symptoms every day; (b) often active, giving me symptoms most days; (c) sometimes active, giving me symptoms on some days (for instance 1–2 days/week); (d) occasionally active, giving me symptoms 1–2 days/month; (e) rarely active, giving me symptoms on a few days in the past 6 months; and (f) I was well in the past 6 months, what I consider a remission or absence of symptoms. Patients with any of (a–d) answers are considered to have active disease, while those choosing any of (e–f) are considered to be in clinical remission. The short IBD Questionnaire (SIBDQ)* was used to assess HRQOL. For each participant, levels of anxiety, depression, fatigue, sleep disturbances, pain interference, social satisfaction, and sexual interest and satisfaction were assessed using the Patient-Reported Outcomes Measurement Information System (PROMIS). The PROMIS measures have been previously validated in general and chronically-ill populations and their performance has also been assessed within the CCFA Partners cohort.15–17 In brief, participants completed 2–4 items for each of the PROMIS domains. The items are then calibrated using t-score metric to provide a mean value for the domain assessed, where higher scores indicates higher level of the domain being measured, e.g. more anxiety, or more social satisfaction. In the general healthy populations, the mean t-score for anxiety, depression, fatigue, pain interference, sleep disturbances, and social satisfactions is 50 with standard deviation (SD) of 10. A priori thresholds of ≥ 52 (anxiety, depression, fatigue, pain interference, and sleep disturbances) and ≤ 48 (social satisfaction) were selected to define the presence of an adverse PRO within each domain. We chose these threshold cut points to allow for a clinically meaningful separation from the general population. Minimal important differences (MIDs) in PROMIS measures for IBD patients have not been defined. However, in cancer patients, chronic pain patients and healthy pediatric patients, research has revealed a range of MIDs of 2 to 6 for several of the PROMIS domains.18–20 The mean t-scores within the general population for the domains of sexual interest and satisfaction are gender-specific: 50 (10) in men and 42 (14) in women for sexual interest and 51 (9) in men and 49 (11) in women for sexual satisfaction.21
Statistical Analysis
Descriptive statistics were used to describe the demographic and disease-related characteristics of the studied population stratified by the presence or absence of ostomy. Continuous variables were presented as means and SD while the categorical variables were reported as percentages. We performed statistical tests of group differences using Pearson’s Chi-square test for categorical variables and Student’s t-tests for continuous variables. Within strata defined by disease activity, multivariable logistic regression models were then utilized to investigate independent associations between ostomy status and anxiety, depression, fatigue, pain interference, sleep disturbances, and social satisfaction while controlling for participants’ age, body mass index (BMI), disease duration, gender, smoking status, and IBD therapies. The main outcomes of interest in these logistic models were the presence of adverse PROs defined as means ≥ 52 for anxiety, depression, fatigue, pain interference and sleep disturbances and ≤ 48 for social satisfaction. One-way between-groups analysis of covariance (ANCOVA) was utilized to assess the impact of having an ostomy on sexual interest and satisfaction while controlling for the participant’s age and disease activity. We also used logistic regression modeling to assess predictors of narcotic use. All statistical analyses were performed using SPSS version 22.0 (IBM Corp. Armonk, NY).
Ethical Considerations
The study protocol was approved by the Institutional Review Board at the University of North Carolina
Results
Patients’ characteristics
A total of 4733 CD patients were included in the study. Of these, 402 patients (8.5%) reported an ostomy on both their baseline and first follow up surveys (minimum duration of 6 months). Patients with ostomy were older (mean age 49.3) and had longer disease duration (mean 26.2) compared to those with no ostomy (mean age 43.7 and mean disease duration 15.1). Both groups were comparable in regard to race and gender distributions, BMI, and the proportion of current smokers [Table 1]. As measured by the MIBDI, more patients with ostomy were in clinical remission compared to those without ostomy (48.5% for ostomy versus 31.3% for no ostomy, p <0.001).
Table 1.
Demographic and disease-related characteristics of Crohn’s disease patients with and without ostomy
| Characteristics | Patients without ostomy (n=4331) | Patients with ostomy (n= 402) | P-value* |
|---|---|---|---|
| Age, y | 43.7 (15) | 49.3 (14) | < 0.001 |
| Women | 72.9 | 71.8 | 0.64 |
| White race | 95.0 | 95.1 | 0.79 |
| BMI, kg/m2 | 25.6 (6) | 26.2 (6) | 0.06 |
| Current smoker | 6.6 | 8.0 | 0.29 |
| Disease duration, y | 15.1 (13) | 26.2 (14) | <0.001 |
| Remission per MIBDI | 31.3 | 48.5 | <0.001 |
| Systemic steroid | 15.3 | 12.8 | 0.21 |
| 5- Aminosalicylates | 35.9 | 13.6 | <0.001 |
| Immunomodulator therapy | 31.3 | 28.4 | 0.25 |
| Biologic therapy | 42.2 | 33.6 | 0.001 |
| Narcotic | 14.7 | 21.5 | 0.001 |
| Any IBD medication | 64.7 | 49.9 | <0.001 |
Data presented at means (SD) or percentages
Comparisons were made using Pearson’s Chi-square test for categorical variables and Student’s t-test for continuous variables.
The frequencies of medication use by patients with and without ostomies are shown in Table 1. Overall, patients with ostomies were less likely to use medication than patients without ostomies (50% versus 65%, P <0.001). The majority of ostomy patients treated with medications reported use of a biologic agent (40.5%) or an immunomodulator (56.9%). A total of 13.6% of patients with ostomy reported being on 5-aminosalicylate (5-ASA) therapy. The rate of systemic corticosteroid use was similar for patients with and without ostomy (12.8% vs. 15.3%, p-value= 0.21).
Interestingly, narcotic use was higher among patients with an ostomy as compared to patients without ostomy (21.5 % versus 14.7%, p=0.001). Using logistic regression modeling to assess independent predictors for narcotic use among the study population while controlling for disease activity and several demographic and disease-related characteristics, having an ostomy was an independent predictor for narcotic use (OR 1.68, 95% CI. 1.24 – 2.27). Other predictors included in the model are listed in Table 2.
Table 2.
Predictors of narcotic use among the study population, based on a logistic model including all predictors.
| Variable | Odd Ratio | 95% confidence interval |
|---|---|---|
| Remission per MIBDI | 0.64 | 0.49 – 0.83 |
| Current ostomy | 1.68 | 1.24 – 2.27 |
| Current smoker | 1.60 | 1.19 – 2.16 |
| Current age | 1.02 | 1.01 – 1.02 |
| Female gender | 0.97 | 0.78–1.20 |
| Pain interference* | 1.13 | 1.12–1.15 |
Presence of pain interference was defined as PROMIS mean score ≥ 52
Impact of ostomy on quality of life and PROs
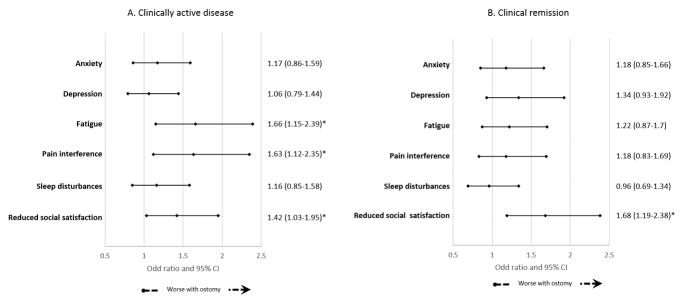
Because disease activity is likely to influence the HRQOL and the various PROs, the impact of ostomy on these outcomes was examined within strata defined by disease activity. On bivariate analysis, the HRQOL as assessed by the SIBDQ was comparable for patients with and without ostomy within each strata of disease activity [Table 3]. Among those in clinical remission, the scores for all six PROMIS domains (anxiety, depression, fatigue, pain interference, sleep disturbances, and social satisfaction) were comparable in patients with and without ostomy. However, for patients whose disease activity is not controlled, those with ostomy had worse PROMIS scores for fatigue, pain interference, and social satisfaction compared to patients with no ostomy [Table 3]. Utilizing logistic regression models to investigate independent (adjusted) associations between ostomy and the 6 PROs within strata defined by disease activity, having an ostomy was noted to be an independent predictor for fatigue (OR 1.66, 95% CI. 1.15–2.39), pain interference (OR 1.63, 95% CI. 1.12–2.35), and reduced social satisfaction (OR 1.42, 95% CI. 1.03–1.95) among patients with active disease. Conversely, among those who were in clinical remission, ostomy was only associated with reduced social satisfaction (OR 1.68, 95% CI. 1.19–2.38) but none of the other assessed outcomes [Figure 1].
Table 3.
Patient-reported outcomes by ostomy status, stratified by MIBDI-defined disease activity. All values are means (SD) of the relevant PRO
| Patient-reported outcome | MIBD-defined active disease | MIBDI-defined remission | ||
|---|---|---|---|---|
| No ostomy (n=2948) | Ostomy (n=205) | No ostomy (n=1344) | Ostomy (n=193) | |
| HRQOL (SIBDQ) | 4.5 (1.1) | 4.7 (1.1) | 5.8 (0.8) | 5.8 (0.8) |
| Anxiety (PROMIS) | 54.2 (9.5) | 54.7 (9.9) | 49.2 (8.8) | 49.4 (9.1) |
| Depression (PROMIS) | 52.6 (9.5) | 53.5 (10.0) | 47.4 (8.0) | 48.5 (8.9) |
| Fatigue (PROMIS) | 58.3 (10.4) | 59.8 (10.8)* | 49.8 (9.8) | 49.8 (10.4) |
| Pain interference (PROMIS) | 55.2 (9.5) | 57.8 (9.5)* | 46.3 (7.6) | 46.7 (8.3) |
| Sleep disturbances (PROMIS) | 52.0 (3.5) | 52.1 (3.5) | 52.0 (3.3) | 52.3 (3.6) |
| Social satisfaction (PROMIS) | 46.3 (9.2) | 44.3 (9.2)* | 53.0 (9.3) | 51.7 (9.9) |
P-value of ≤ 0.05 for Student’s t-test.
Figure 1.
The impact of having an ostomy on patients reported outcomes among patients with clinically active disease (A) and patients in clinical remission (B). A separate logistic regression model was applied for each outcome. The models controlled for gender, age, disease duration, smoking status, current corticosteroid, biologic, and immunomodulator therapies.
For patients who completed the sexual function domains (n= 1326 for sexual interest domain and n= 991 for sexual satisfaction domain), means scores for sexual interest and satisfaction were similar in patients both with and without ostomy, which remained true after adjusting for age and disease activity [Table 4].
Table 4.
Age- and disease activity-adjusted means of PROMIS scores for sexual interest and satisfaction among patients with and without ostomy stratified by gender.*
| Gender | Sexual function domain | Patients without ostomy | Patients with ostomy | P-value (One-way ANCOVA) |
|---|---|---|---|---|
| Adjusted means (SE) | Adjusted means (SE) | |||
| Men | Sexual interest (n=270) | 48.7 (0.6) | 48.5 (1.7) | 0.91 |
| Sexual Satisfaction (n=280) | 48.2 (0.4) | 46.1(1.5) | 0.17 | |
| Women | Sexual interest (n=956) | 40.4 (0.4) | 40.8 (1.3) | 0.77 |
| Sexual Satisfaction (n=711) | 46.7 (0.3) | 47.5 (1.1) | 0.5 |
The general population means (SD) for sexual interest are 50 (10) in men and 42 (14) in women and sexual satisfaction are 51 (9) in men and 49 (11) in women
Discussion
The potential need for an ostomy is a major concern for patients with IBD, particularly CD patients who may be at higher risk of needing a permanent ostomy. Nevertheless, up until now, the data on the actual impact of having an ostomy in this population were very limited. In this large sample of CD patients, we analyzed the demographic and disease-related characteristics of patients with ostomy for a minimum duration of 6 months compared to those without ostomy. Furthermore, we investigated the impact of having an ostomy on several patient-reported outcomes pertaining to different functional and psychosocial domains. We observed several important findings. First, as expected, patients with ostomy were older and had longer disease duration compared to those without an ostomy. This is likely a reflection of the general notion that surgery is reserved as a last resort for patients with CD after failing several medical therapies.
Second, patients with an ostomy were more likely to be in clinical remission compared to those without an ostomy (48.5% vs. 31.3%, respectively). This is mirrored by the observation that only half of the patients with ostomy reported being on any IBD therapy. For CD patients, in whom the disease can involve any part of the GI tract, surgery is not considered or advocated as a cure. However, those with primarily colonic disease have higher chances of maintaining long term clinical remission after colectomy with a suggested advantage of ileostomy over anastomosis.22,23 In a study by Bernell et al, the cumulative 10-year risk of a symptomatic recurrence after colectomy with ileorectal anastomosis was 58% compared to 24% after colectomy with ileostomy.22 The outcome is likely different for patients requiring ostomy for other indications, particularly those with refractory perianal disease. Our sample likely includes patients who received their ostomy for multiple indications.
Despite the higher prevalence of clinical remission, patients with ostomy were more likely to report narcotic use compared to those without ostomy (21.5% versus 14.7%, respectively). The higher rate of narcotic use in patients with ostomy persisted even amongst patients reporting remission based on the MIBDI (9.7% in patients with ostomy versus 5.5% in patients without ostomy). Furthermore, in the logistic regression modeling, having an ostomy was an independent predictor for narcotic use after controlling for age, gender, disease activity, smoking status, and pain interference. Within the CCFA Partners cohort, patients are not asked to specify which narcotic agents they are using. Hence, it is possible that that the higher rate of narcotic use among patients with ostomy in our study is related to using this class of therapy to reduce ostomy output (e.g. Tincture of opium) rather than managing pain. However, ostomy patients with active disease had a much higher prevalence of narcotic use compared to those with ostomy but in remission (32.5% versus 9.7%, respectively), and also compared to non-ostomy patients with active disease (19%), suggesting that narcotic may be used to control disease symptoms in a significant proportion of patients with ostomy. This is further supported by the noted association between narcotic use and pain interference scores [Table 2]. Narcotic use in IBD patients has been linked to a number of adverse effects, including higher rate of infectious complications, surgical complications and even mortality.24–26 Thus, further research is needed to understand the nature of pain in CD patients with ostomy and provide appropriate alternatives to narcotic-based analgesia in this population.
In our study, having an ostomy did not impact HRQOL as measured by SIBDQ. Although, SIBDQ is an IBD-specific QOL measure, it is important to note that this questionnaire has not been separately validated in patients with ostomy. Hence, our results should be interpreted in the context of this limitation. Nevertheless, our findings are comparable to results from two previous studies that used a generic QOL tool, the Short Form 36 (SF-36) questionnaire, to assess the impact of ostomy on HRQOL among IBD patients.12,27 In both studies, ostomy did not have a significant impact on HRQOL.
In regards to the six assessed PROMIS domains, having an ostomy appears to primarily impact social satisfaction given our observed association between ostomy and reduced social satisfaction irrespective of active/remission disease status. This impact of ostomy on social satisfaction may be related to an altered body image and the technical issues related to daily ostomy care. In a study by Carlsson et al, the Rating Form of IBD Patients Concerns (RFIPC) questionnaire was used to assess the concerns of patients with ileostomy.27 Producing unpleasant odor and being a burden on others were among the top 5 concerns, both of which can impact social functioning and satisfaction. We also observed significant associations between ostomy status and both fatigue and pain interference among patients with clinically active disease but not for those in clinical remission. It is unclear whether these associations represent a causal effect of ostomy in this population or, alternatively, ostomy serves as a surrogate marker for more severe and complicated disease with resultant pain and fatigue in patients who continue to have active disease despite prior surgical intervention. At a more reassuring note, having an ostomy did not impact anxiety, depression, or sleep disturbances scores even in patients with active disease, and ostomy was not associated with pain interference or fatigue among those in remission.
Lastly, in our study population, having an ostomy did not impact sexual interest or satisfaction in both men and women, even after adjusting for age and disease activity. This is contrary to what has previously been reported in the literature as having an ostomy was linked to a number of adverse physiological and psychological effects that can impact sexual function in both men and women. Among those effects are: erectile dysfunction; retrograde ejaculation; orgasmic dysfunction; dyspareunia; and reduced sexual desire.28,29 The discrepancy between our results and the prior literature is likely related to the indication for the ostomy, IBD, rather than malignancy. This is particularly true for the physiological effects resulting from nerve damage caused by more extensive surgical resection and manipulation needed for cancer resections but not typically for IBD-related surgeries. It is also important to note that a smaller proportion of patients completed the sexual function modules in our study, which may have an impact on the power of our results.
There are several strengths to this study. It is, to our knowledge, the largest to date to assess the characteristics of CD patients with ostomy and investigate its impact on several patient-reported outcomes. Furthermore, the studied population was part of a well maintained and geographically diverse cohort of IBD patients. In a validation study from a subset of participants in the parent cohort, there was a 97% accuracy rate of self-reported IBD status and disease subtypes when compared to medical records. 30 The use of validated scales to assess a wide variety of clinically relevant PROs is also a strength for this study. Finally, using the MIBDI, we were able to conduct analyses stratified by disease activity in patients both with and without ostomy.
We also recognize a number of limitations to our study. We were unable to determine the indication for having an ostomy in each patient, the exact time since surgery, and whether the ostomy is permanent or temporary. In addition, the disease location and behavior could not be specified for each patient. These characteristics may influence how patients perceive the impact of having an ostomy on their quality of life. To mitigate this limitation and minimize the variability, we only analyzed patients who reported the same ostomy status in two subsequent surveys and we used the responses in the second survey to assess the impact on the various PROs. A second limitation is the use of SIBDQ to assess HROQL. As we pointed out earlier, the SIBDQ is not validated in ostomy patients. Furthermore, one item in the questionare is not applicable to patients with ostomy (pertaining to tenesmus). Several stoma-specific QOL questionares were proposed in the past. 31–33 Those questionares are relatively long (20–34 items) and none of them is specific for IBD patients, hence we elected to use the SIBDQ. The relatively smaller proportion of patients completing the sexual function modules is another limitation, as we were unable to utilize regression modeling to control for multiple variables in a manner similar to our analyses of the other PROs. Nevertheless, we were able to control for age and disease activity in our calculations, both are expected to have greater impact on sexual function.
In conclusion, in this cross-sectional study of CD patients, having an ostomy did not impact patients’ quality of life or sexual function. Moreover, ostomy was not associated with anxiety, depression or sleep disturbances. The majority of ostomy-adverse PROs associations, with the exclusion of social satisfaction, were only observed in patients with active disease. Therefore, it is reassuring that the presence of an ostomy concomitant with controlled disease does not impact important PROs. These data will aid in counseling individuals facing a surgical need for temporary or permanent stoma creation.
Acknowledgments
Study Funding: This work was supported by the Crohn’s and Colitis Foundation of America, Patient Centered Outcomes Research Institute, and the National Institutes of Health (Grants numbers: NIH P30 DK34987 and NIH 1K08DK088957-01).
Footnotes
Short Inflammatory Bowel Disease Questionnaire (SIBDQ) was authored by Dr. J. Irvine, et al, was made under license from McMaster University, Hamilton, Canada
Conference presentation: the study was presented as an abstract at Digestive Disease Week, San Diego CA 2016
Authors’ contributions: M.I.A: participated in formulating the study conception and design, acquisition of data, statistical analysis, analysis and interpretation of data; drafting the article or revising it critically for important intellectual content; and final approval of the version to be submitted. R.S.S: participated in the conception and design of the study; critical revision of the manuscript for important intellectual content final and approval of the version to be submitted. M.D.K.: participated in the conception and design of the study, critical revision of the manuscript for important intellectual content, and approval of the version to be submitted. C.F.M.: participated in the conception and design of the study, acquisition of data, analysis and final approval of the version to be submitted. W.C.: participated in acquisition of data and final approval of the version to be submitted. K.A.: participated in acquisition of data, and final approval of the version to be submitted. M.D.L.: participated in conception and design of the study, analysis and interpretation of data, critical revision of the manuscript for important intellectual content, and approval of the version to be submitted
Disclosures: Dr. Long has consulted for Abbvie, Salix, Pfizer and Theravance pharmaceuticals. No relevant conflict of interest is present. Dr. Kappelman has consulted for Abbvie, Janssen, Celgene, and GlaxoSmithKline and has received support from Abbvie, Janssen, and GlaxoSmithKline. No relevant conflict of interest is present. The remaining authors declare no conflict of interest.
References
- 1.Cosnes J, Gower–Rousseau C, Seksik P, Cortot A. Epidemiology and natural history of inflammatory bowel diseases. Gastroenterology. 2011;140(6):1785–1794. e4. doi: 10.1053/j.gastro.2011.01.055. [DOI] [PubMed] [Google Scholar]
- 2.Drossman DA, Leserman J, Li ZM, Mitchell CM, Zagami EA, Patrick DL. The rating form of IBD patient concerns: A new measure of health status. Psychosom Med. 1991;53(6):701–712. doi: 10.1097/00006842-199111000-00010. [DOI] [PubMed] [Google Scholar]
- 3.Blondel-Kucharski F, Chircop C, Marquis P, et al. Health-related quality of life in crohn’s disease: A prospective longitudinal study in 231 patients. Am J Gastroenterol. 2001;96(10):2915–2920. doi: 10.1111/j.1572-0241.2001.4681_b.x. [DOI] [PubMed] [Google Scholar]
- 4.de Rooy EC, Toner BB, Maunder RG, et al. Concerns of patients with inflammatory bowel disease: Results from a clinical population. Am J Gastroenterol. 2001;96(6):1816–1821. doi: 10.1111/j.1572-0241.2001.03877.x. [DOI] [PubMed] [Google Scholar]
- 5.Stjernman H, Tysk C, Almer S, Strom M, Hjortswang H. Worries and concerns in a large unselected cohort of patients with crohn’s disease. Scand J Gastroenterol. 2010;45(6):696–706. doi: 10.3109/00365521003734141. [DOI] [PubMed] [Google Scholar]
- 6.Lesage AC, Hagege H, Tucat G, Gendre JP. Results of a national survey on quality of life in inflammatory bowel diseases. Clin Res Hepatol Gastroenterol. 2011;35(2):117–124. doi: 10.1016/j.gcb.2009.08.015. [DOI] [PubMed] [Google Scholar]
- 7.Jelsness-Jorgensen LP, Moum B, Bernklev T. Worries and concerns among inflammatory bowel disease patients followed prospectively over one year. Gastroenterol Res Pract. 2011;2011:492034. doi: 10.1155/2011/492034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Follick MJ, Smith TW, Turk DC. Psychosocial adjustment following ostomy. Health Psychol. 1984;3(6):505–517. doi: 10.1037//0278-6133.3.6.505. [DOI] [PubMed] [Google Scholar]
- 9.Ramer L. Self-image changes with time in the cancer patient with a colostomy after operation. J ET Nurs. 1992;19(6):195–203. doi: 10.1097/00152192-199211000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Brown H, Randle J. Living with a stoma: A review of the literature. J Clin Nurs. 2005;14(1):74–81. doi: 10.1111/j.1365-2702.2004.00945.x. [DOI] [PubMed] [Google Scholar]
- 11.Cotrim H, Pereira G. Impact of colorectal cancer on patient and family: Implications for care. Eur J Oncol Nurs. 2008;12(3):217–226. doi: 10.1016/j.ejon.2007.11.005. [DOI] [PubMed] [Google Scholar]
- 12.Nordin K, Pahlman L, Larsson K, Sundberg-Hjelm M, Loof L. Health-related quality of life and psychological distress in a population-based sample of swedish patients with inflammatory bowel disease. Scand J Gastroenterol. 2002;37(4):450–457. doi: 10.1080/003655202317316097. [DOI] [PubMed] [Google Scholar]
- 13.Long MD, Kappelman MD, Martin CF, et al. Development of an internet-based cohort of patients with inflammatory bowel diseases (CCFA partners): Methodology and initial results. Inflamm Bowel Dis. 2012;18(11):2099–2106. doi: 10.1002/ibd.22895. [DOI] [PubMed] [Google Scholar]
- 14.Clara I, Lix LM, Walker JR, et al. The manitoba IBD index: Evidence for a new and simple indicator of IBD activity. Am J Gastroenterol. 2009;104(7):1754–1763. doi: 10.1038/ajg.2009.197. [DOI] [PubMed] [Google Scholar]
- 15.Kappelman MD, Long MD, Martin C, et al. Evaluation of the patient-reported outcomes measurement information system in a large cohort of patients with inflammatory bowel diseases. Clin Gastroenterol Hepatol. 2014;12(8):1315–23. e2. doi: 10.1016/j.cgh.2013.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rothrock NE, Hays RD, Spritzer K, Yount SE, Riley W, Cella D. Relative to the general US population, chronic diseases are associated with poorer health-related quality of life as measured by the patient-reported outcomes measurement information system (PROMIS) J Clin Epidemiol. 2010;63(11):1195–1204. doi: 10.1016/j.jclinepi.2010.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cella D, Yount S, Rothrock N, et al. The patient-reported outcomes measurement information system (PROMIS): Progress of an NIH roadmap cooperative group during its first two years. Med Care. 2007;45(5 Suppl 1):S3–S11. doi: 10.1097/01.mlr.0000258615.42478.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yost KJ, Eton DT, Garcia SF, Cella D. Minimally important differences were estimated for six patient-reported outcomes measurement information system-cancer scales in advanced-stage cancer patients. J Clin Epidemiol. 2011;64(5):507–516. doi: 10.1016/j.jclinepi.2010.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Swanholm E, McDonald W, Makris U, Noe C, Gatchel R. Estimates of minimally important differences (MIDs) for two patient-reported outcomes measurement information system (PROMIS) computer-adaptive tests in chronic pain patients. Journal of Applied Biobehavioral Research. 2014;19(4):217–232. [Google Scholar]
- 20.Thissen D, Liu Y, Magnus B, et al. Estimating minimally important difference (MID) in PROMIS pediatric measures using the scale-judgment method. Qual Life Res. 2016;25(1):13–23. doi: 10.1007/s11136-015-1058-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Weinfurt KP, Lin L, Bruner DW, et al. Development and initial validation of the PROMIS((R)) sexual function and satisfaction measures version 2.0. J Sex Med. 2015;12(9):1961–1974. doi: 10.1111/jsm.12966. [DOI] [PubMed] [Google Scholar]
- 22.Bernell O, Lapidus A, Hellers G. Recurrence after colectomy in crohn’s colitis. Dis Colon Rectum. 2001;44(5):647–54. doi: 10.1007/BF02234559. discussion 654. [DOI] [PubMed] [Google Scholar]
- 23.Lopez J, Konijeti GG, Nguyen DD, Sauk J, Yajnik V, Ananthakrishnan AN. Natural history of crohn’s disease following total colectomy and end ileostomy. Inflamm Bowel Dis. 2014;20(7):1236–1241. doi: 10.1097/MIB.0000000000000072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hirsch A, Yarur AJ, Dezheng H, et al. Penetrating disease, narcotic use, and loop ostomy are associated with ostomy and IBD-related complications after ostomy surgery in crohn’s disease patients. J Gastrointest Surg. 2015;19(10):1852–1861. doi: 10.1007/s11605-015-2908-y. [DOI] [PubMed] [Google Scholar]
- 25.Lichtenstein GR, Feagan BG, Cohen RD, et al. Serious infections and mortality in association with therapies for crohn’s disease: TREAT registry. Clin Gastroenterol Hepatol. 2006;4(5):621–630. doi: 10.1016/j.cgh.2006.03.002. [DOI] [PubMed] [Google Scholar]
- 26.Targownik LE, Nugent Z, Singh H, Bugden S, Bernstein CN. The prevalence and predictors of opioid use in inflammatory bowel disease: A population-based analysis. Am J Gastroenterol. 2014;109(10):1613–1620. doi: 10.1038/ajg.2014.230. [DOI] [PubMed] [Google Scholar]
- 27.Carlsson E, Bosaeus I, Nordgren S. What concerns subjects with inflammatory bowel disease and an ileostomy? Scand J Gastroenterol. 2003;38(9):978–984. doi: 10.1080/00365520310004687. [DOI] [PubMed] [Google Scholar]
- 28.Black PK. Psychological, sexual and cultural issues for patients with a stoma. Br J Nurs. 2004;13(12):692–697. doi: 10.12968/bjon.2004.13.12.13254. [DOI] [PubMed] [Google Scholar]
- 29.Sprunk E, Alteneder RR. The impact of an ostomy on sexuality. Clin J Oncol Nurs. 2000;4(2):85–88. [PubMed] [Google Scholar]
- 30.Randell RL, Long MD, Cook SF, et al. Validation of an internet-based cohort of inflammatory bowel disease (CCFA partners) Inflamm Bowel Dis. 2014;20(3):541–544. doi: 10.1097/01.MIB.0000441348.32570.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Baxter NN, Novotny PJ, Jacobson T, Maidl LJ, Sloan J, Young-Fadok TM. A stoma quality of life scale. Dis Colon Rectum. 2006;49:205–12. doi: 10.1007/s10350-005-0275-6. [DOI] [PubMed] [Google Scholar]
- 32.Olbrisch ME. Development and validation of the ostomyadjustment scale. Rehabil Psychol. 1983;28:3–12. [Google Scholar]
- 33.Canova C, Giorato E, Roveron G, Turrini P, Zanotti R. Validation of a stoma-specific quality of life questionnaire in a sample of patients with colostomy or ileostomy. Colorectal Dis. 2013 Nov;15:e692–8. doi: 10.1111/codi.12324. [DOI] [PubMed] [Google Scholar]