Abstract
Adolescents and young adults with type 1 diabetes are at risk for poor health outcomes, including poor glycemic control, acute and chronic complications, and emergency department admissions. During this developmental period, adolescent and young adult patients also experience significant changes in living situation, education, and/or health care delivery, including transferring from pediatric to adult health care. In recent years, professional and advocacy organizations have proposed expert guidelines to improve the process of preparation for and transition to adult-oriented health care. However, challenges remain and evidence-based practices for preparing youth for adult health care are still emerging. Qualitative research suggests that adolescent and young adult patients rely on health care providers to guide them through the transition process and appreciate a gradual approach to preparing for adult-oriented health care, keeping parents in supportive roles into young adulthood. Patients also benefit from specific referrals and contact information for adult care providers. Promising models of transition care include provision of transition navigators, attendance at a young adult bridge clinic, or joint visits with pediatric and adult care providers. However, much of this research is in its early stages, and more rigorous trials need to be conducted to evaluate health outcomes during transition into adult health care. The purpose of this review is to provide an overview of the transition process, patient and health care provider perceptions of transition care, and emerging evidence of successful models of care for engagement in adult-oriented health care. Recommendations and resources for health care providers are also presented.
Keywords: type 1 diabetes, transition to adult care, health care delivery, adolescents, young adults
Introduction
Type 1 diabetes is one of the most common chronic illnesses in childhood, affecting more than one out of every 500 youth.1 As the modal age of diagnosis of type 1 diabetes is in middle childhood,2 a growing number of adolescents and young adults are affected by type 1 diabetes, and they must simultaneously manage diabetes and navigate a complex health care system during a developmental period known for instability and uncertainty in education, employment, living situation, family and intimate relationships, and health care delivery.3 Recent policy statements and related efforts have attempted to increase support for youth during this challenging developmental period, primarily by improving the transition from pediatric to adult-oriented health care.4,5 However, challenges remain, and adolescents and young adults are at risk for poor glycemic control and other adverse health outcomes.6–9 Research suggests that only 20%–30% of late adolescents and young adults meet current recommendations for glycemic control.10,11 In addition, a significant percentage of adolescents and young adults experience acute and chronic complications,12–16 making continuous access to high-quality medical care exceedingly important for this age group.
This review provides a comprehensive, up-to-date overview of research on the transition to adult-oriented health care for youth with type 1 diabetes, highlighting patient and health care provider identification of transition needs, relevant risk factors that may influence outcomes related to transition, and current models of care that may facilitate successful transition to adult diabetes care. Additionally, we offer recommendations and resources for providers working with this age group and potential avenues for future intervention.
Challenges to diabetes management in adolescents and young adults
Management of type 1 diabetes during adolescence and young adulthood requires careful consideration of a number of physiologic, developmental, and health care system issues. This period is characterized by increasing independence and assumption of responsibility for most tasks of daily living, including disease care.3 In addition to potential adherence challenges related to decreased parental involvement in diabetes management, achievement of optimal metabolic control is also complicated by adolescent hormonal changes, leading to temporary increases in insulin resistance and related insulin requirements to maintain euglycemia.17 Longitudinal research suggests that hemoglobin A1c (A1c) levels begin to rise at age 10, concurrent with the onset of puberty and bodily growth. Although A1c values are variable depending on psychosocial, socioeconomic, and individual considerations,18 representative research suggests that youth with type 1 diabetes reach a peak mean A1c level of 8.9% between ages 16 and 18, before A1c gradually declines to 8.2% by age 26.19 As the American Diabetes Association recommends maintenance of A1c levels <7.5% for adolescents and <7.0% for adults with type 1 diabetes, these values are suboptimal.20
Thus, health care providers working with this age group must frequently fine-tune diabetes management. Efforts to improve glycemic control may be stymied by physiologic factors as well as those mentioned earlier, which may be beyond a patient's control. Laboratory assessments recommended for adolescent and young adult patients with type 1 diabetes include quarterly appointments with a pediatric endocrinologist or diabetologist, with evaluation of A1c, downloaded blood glucose data, body mass index, and blood pressure at each visit. In addition, recommended annual laboratory assessments include a lipid panel, level of thyroid-stimulating hormone, celiac panel (total immunoglobulin A [IgA], serum tissue transglutaminase IgA, and endomysial IgA), urine microalbumin-to-creatinine ratio, and creatinine clearance/estimated glomerular filtration rate. Evaluation every 1–2 years by an ophthalmologist 5 years after initial diagnosis of diabetes is also recommended.20
Maintenance of a consistent relationship with a diabetes care provider across adolescence and young adulthood is required to provide the frequent monitoring necessary to minimize diabetes-related complications. The transition from pediatric to adult-oriented health care has the potential to disrupt clinical care and may further contribute to suboptimal glycemic control for adolescents and young adults.
Transition from pediatric to adult-oriented health care
Transition to adult-oriented health care is a key developmental task for adolescents and young adults with type 1 diabetes. Transition refers to the complex, planned process of preparing for and executing the move from pediatric to adult health care.21 Transfer refers to the discrete point in time when a patient initiates care in the adult health care system. Transition is a multiyear process, ideally beginning early in adolescence, designed to develop and enhance effective knowledge, self-management, and advocacy in order to ensure adequate readiness for meeting the demands of adult-oriented health care and to facilitate access to continuous health care into adulthood.5,21 Patients, parents, health care providers, and other supportive persons all contribute to the transition process, and transition activities occur both in pediatric and adult medical care.
There are a number of fundamental differences between pediatric and adult health care systems.22 Pediatric diabetes care is often family based, offering patients and parents access to an integrated team of physicians, nurse educators, dietitians, social workers, and psychologists.23 In contrast, the adult-oriented health care system typically has less availability of multidisciplinary care, particularly social and behavioral health.24 Clinic visits are often shorter, with greater emphasis on objective medical indicators and physical symptoms (eg, weight, blood pressure, and A1c) and less input from parents and other support partners.25–27 Preparing youth for the entrance into the adult care setting can minimize disruption and promote continuous engagement in high-quality diabetes care.
Preparation for adult-oriented health care often involves frequent, structured assessment of transition readiness – or the skills and behaviors thought to be important in adult-oriented health care – and the creation and implementation of transition plans to address specific deficits in these skills, knowledge, and behaviors prior to transfer.5,28 A number of measures exist to assess transition readiness in youth with special health care needs. Most validated transition questionnaires assess general transition readiness skills (eg, Transition Readiness Assessment Questionnaire [TRAQ]29; Self- Management and Transition to Adulthood with Rx = Treatment [STARx] Questionnaire30). Professional organizations, such as the National Diabetes Education Program and the Endocrine Society, also have created diabetes-specific checklists (http://ndep.nih.gov/transitions/index.aspx) designed to assess key patient skills that may promote successful transition as well as patient concerns and diabetes-specific worries that may affect transition (www.endocrinetransitions.org). A recent systematic review found that measures of general transition readiness are promising but require additional testing and validation, particularly connecting measures of transition readiness with the previous experienced outcomes in adult medical care.31
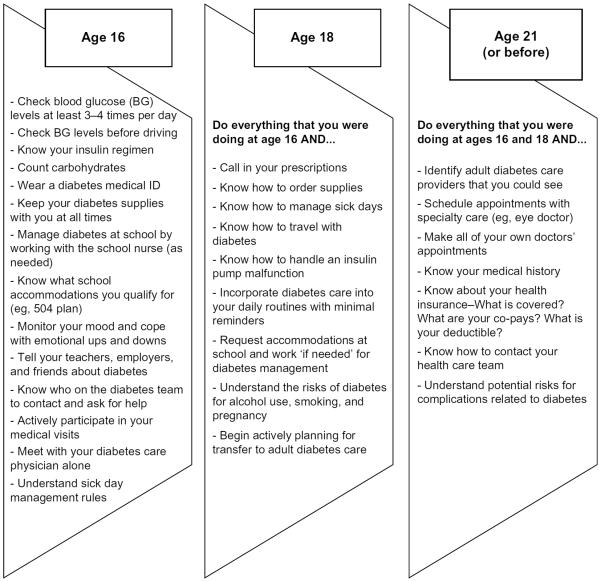
Transition plans target the key tasks and goals that should be completed before entering adult-oriented health care, as well as informing interventions or other strategies for meeting these goals.32 The ongoing processes of assessing transition readiness and providing targeted intervention guided by evolving transition plans help to prepare youth for successful entrance into adult health care.28,33 An example of specific diabetes management skills that should be achieved prior to transition to adult health care is presented in Figure 1.
Figure 1.
Sample diabetes skills and knowledge to be addressed before transfer to adult-oriented health care.
Transition time line for youth with diabetes
Most youth with type 1 diabetes transition to adult medical care during the early young-adult period between the ages of 18 years and 22 years. Research suggests that the median age of transition is 19.5–20 years.9,34 Representative research of transition to adult care for US youth enrolled in the SEARCH for Diabetes in Youth study34 found that 53% of youth aged 18–20 years remained in pediatric care, but only 23% of youth were still in pediatric care at age 21 and older. In international samples, transition may occur closer to age 17 or 18 due to differences in health care systems and procedures.23,35,36 One representative study37 of 36 countries found that 76% of centers reported patient transfer to adult diabetes care occurring at age 18. The age of transition may be important, particularly in clinics with more flexible age limits for transfer, as youth who transition earlier are at risk for worse health outcomes, including poor glycemic control and gaps in medical care.9,34,38
Young adults in adult diabetes care may access health care in a variety of settings, including adult endocrinology clinics, primary care, family medicine, university-based health clinics, or in targeted young adult clinics designed to bridge pediatric and adult care.6,8,39 Most adults with type 1 diabetes see endocrinologists for their care, and research suggests that engagement in specialty care instead of primary care protects youth against negative outcomes in adult care and provides access to more diabetes-specific services (eg, certified diabetes educators, dietitians).8,40
Components of successful transition
In 2011, the American Diabetes Association,4 along with representation from other leading health organizations caring for youth with diabetes, published a position statement on the care needs of late adolescents and young adults with diabetes. This comprehensive statement reviewed key considerations for caring for emerging adults and potential best practices in transitioning youth from pediatric to adult medical care. Considering the limited literature on outcomes of clinical transition programs, many of the recommendations were based on expert consensus. Specifically, this position statement recommended the following: 1) initiating transition preparation at least 1 year prior to the planned transfer date and likely earlier in adolescence if possible; 2) working with patients and parents to facilitate a gradual shift of diabetes management responsibility from shared management by patient and parent to more independent management by the patient; 3) providing practical education on differences between the pediatric and adult health care systems and specific referrals for adult care providers as appropriate; 4) assisting youth in compiling medical record documentation in preparation for adult care; 5) acknowledging developmental and psychosocial challenges that may affect transition; and 6) screening for complications commonly seen in older adolescents and young adults with diabetes, including microvascular and macrovascular complications, disordered eating, depression, and substance abuse concerns.4
Around the same time, the American Academy of Pediatrics, American Academy of Family Physicians, and American College of Physicians5 also published broad guidelines on preparing youth for adult-oriented health care. These recommendations were similar to those put forth by the American Diabetes Association but advocated for transition preparation to begin early in adolescence, potentially by ages 12–13 if possible.5 The combination of these two positions statements has influenced the provision of health care and informed potentially successful models for transition to adult medical care. Unfortunately, it is unclear what recommendations have been put into practice. For example, Hilliard et al41 found that at age 16, most patients had yet to discuss transition with their health care providers. Similarly, Garvey et al42 sent a survey to young adults with type 1 diabetes aged 22–30 years after transition to adult medical care and found that <15% of the sample reported receiving written information related to transition or having a transition-specific visit before leaving pediatric care.
Patient perspectives on health care transition
The experiences of young adults with successful or unsuccessful transitions can inform best practices in transition to adult-oriented health care. Some adolescents and young adults report feeling prepared for the transition to and expectations related to adult diabetes care,8 whereas other patients may struggle to initiate or engage in adult-oriented health care. Pyatak et al43 interviewed 20 young adults who had had a lapse in medical care for >1 year and identified factors that contributed to their disrupted transition, including lack of preparation in the pediatric care setting, difficulties with insurance, difficulty identifying appropriate adult care providers, and psychosocial challenges such as life stressors or competing priorities to diabetes care. These barriers have been identified in other samples as well. Garvey et al7 found that lack of a specific adult provider referral or contact information was the most frequently endorsed barrier to establishing adult care. Balfe et al44,45 interviewed 35 young adults with diabetes aged 23–30 years about their experiences with diabetes management, including dealing with the health care system. Common complaints about the adult-oriented health care system included a lack of multidisciplinary diabetes care services, time constraints for routine appointments, difficulties with communication and continuity of care, and difficulty scheduling appointments.
Qualitative data suggest that families rely on health care providers to initiate conversations about adult diabetes care and how to manage expectations related to transfer. While patients and families often feel comfortable managing the shift in responsibility for daily diabetes-related tasks, they are not as familiar with aspects of the health care system that require navigation and attention in adulthood.41 Patients and parents generally report that talking with health care providers at regular clinic visits and receiving family-based supports are particularly helpful in the transition process.46 Additionally, young adult patients have identified services that may improve the transition process, including provision of targeted referrals to adult diabetes care providers, discussion of transition services earlier in pediatric care, assistance with logistics of transfer to adult care, increasing attention to differences between pediatric and adult care, and increased opportunities to connect with other young adults with type 1 diabetes.41,47,48 Services for transitioning patients to adult-oriented health care should continue to include parents as key aspects of the patient's support team rather than excluding them from the process.41,48 It is important to note that once young adults are firmly established in adult diabetes care, they often report a positive experience, including feeling more involved in their own medical care and enjoying the independence encouraged by adult providers.48 However, some young adults in adult medical care report dissatisfaction with adult providers' knowledge of type 1 diabetes and insufficient time with providers during medical appointments.49
Patients and parents have also requested more written resources related to transition8; however, the utilization of these resources varies. For example, one study offering transition classes and a comprehensive binder of materials found that only 50% of eligible parent/adolescent dyads attended the transition class or used the education materials. Furthermore, only 25% of adolescents found the written materials to be very helpful.46 It is likely that transition services are best received when they are integrated into routine clinical care and are built upon interactions and relationships with health care providers.
Transition outcomes and related risk factors
Systematic reviews have examined the impact of transition on diabetes-related outcomes, and evidence suggests that there is a decrease in annual diabetes care visits after transferring to adult care.6,38 In addition to a lower number of yearly clinic visits, ≥25% of young adults report a significant gap in medical care (>6 months) when transferring out of pediatric care.8,50 There is also some evidence to indicate that the timing of transition influences outcomes in adult care. Transition to adult-oriented health care at younger ages has been associated with poorer glycemic control9 and late adolescents who remain in pediatric care into early young adulthood demonstrate better glycemic control and fewer hospitalizations as compared to those who transfer to adult care.34,51 However, evidence on the impact of transition on glycemic control is inconsistent, and one recent review38 found that young adults generally maintained stable or even improved glycemic control after the transfer to adult medical care. This is similar to large cohort studies that report a general improvement in glycemic control in the mid-20s.19 As discussed earlier, this improvement may be due to a number of factors, including physiology.
Risk factors that may contribute to poor outcomes in adult health care have been identified through prospective and retrospective studies. Gaps in medical care in young adulthood may be related to 1) health care system issues, such as lapses in insurance or difficulties in finding an adult care provider, or 2) issues unique to the young adult, such as competing life priorities or an unstable living situation.7 Mistry et al52 evaluated clinic attendance in adult care in a prospective group of young adults referred to a Diabetes Transition Clinic. Overall, nearly one third of participants had a gap in care of at least 1 year after their last transition clinic appointment. Risk factors associated with failure to successfully transition included longer duration of diabetes, use of a conventional two-to-three-injection insulin regimen, worse glycemic control prior to transfer (A1c >9.0%), poor attendance in pediatric care, and low communication with care providers in the transition clinic.52 Young adults with lower family income or who live in areas with poorer access to adult care physicians are also at risk for poor health outcomes posttransfer to adult medical care.9,53 Addressing barriers to successful transition prior to the transfer to adult care may decrease gaps in care and increase engagement in adult-oriented health care, as identification of even one significant barrier to transition has been related to a >4-fold increase in risk for poor attendance.7
Evidence-based models of transition care delivery
Much of the expert opinion on components of a successful transition has focused on preparation on the pediatric side, including the skills, attitudes, and knowledge that contribute to overall transition readiness. Less research has explored what outcomes constitute a successful transition in adult medical care. Pierce and Wysocki54 recently modified a validated theoretical model of transition to identify key outcomes of transition, including biomedical (eg, A1c, acute complications, emergency room visits, and inpatient hospitalizations); behavioral (adherence, engagement in care, reduced gaps in care); and emotional (quality of life, depression, and care satisfaction) outcomes. Others have argued that attendance in adult care should be the primary outcome variable for adult care.6,38,55
Models of care delivery for transition-aged youth vary by program. In addition to the standard model of a discrete move from pediatric to adult-oriented health care, some programs include an interim level of care by young adult providers as a bridge between pediatric and adult care, a joint pediatric–adult clinic where young adults meet with both care providers in the same setting, or additional supports through patient navigators or educational groups.35,36,49,56,57 Some youth temporarily transfer diabetes care to student health centers while attending college; however, research suggests that only 50% of universities report adequate resources to manage type 1 diabetes.58 Comprehensive programs promoting successful transition to adult-oriented care often utilize detailed transition protocols with checklists for transition steps, formal transition-related materials for youth, and targeted interventions to improve self-management.59 Regardless of the method, most agree that a structured, planned transition to adult-oriented health care with adequate communication among providers is necessary to promote engagement in adult medical care.60 Best practices for providers working with transition-aged youth are included in Table 1, and select programs with outcome data are reviewed below.
Table 1.
Best practices for health care providers working with transition-aged youth
| For pediatric health care providers | Provide personalized referral to specific adult health care provider based on individualized knowledge of the patient or assist with identifying providers participating within a patient's insurance network47,48 |
| Initiate discussion about transition early, lead expectation-setting for transition and the adult medical setting, and time the transition based on individual readiness41,56,57 | |
| Communicate with intended adult health care provider before transition and with patient afterward for follow-up48 | |
| Transition process | Employ a transition coordinator to remind, facilitate, and rebook appointments when necessary; follow-up on any missed appointments; ensure transfer of information from pediatric to adult providers56,57,63,64,68 |
| Multidisciplinary ”joint” (involving members of both the pediatric and adult health care teams) appointments ranging from one visit to up to 2 years before seeing solely adult providers, especially for those with history of infrequent clinic attendance57,63 | |
| For adult health care providers | Consider setting up an introductory meeting with new adult patients before transition41 |
| Provide orientation to clinic practices and take time to develop personal rapport and relationship with patients47 | |
| For any providers serving adolescents and young adults with type 1 diabetes | Encourage collaboration in doctor–patient relationship and promote the patient's autonomy and gradual assumption of personal responsibility as developmentally appropriate48 |
| As appropriate, involve parents as an important source of support and continually needed resource41,46,48 | |
| Adequately address concerns specific to this age group (ie, risky behaviors, dietary patterns, changes in living situation, insurance status, and health effects of stress)43,56 |
Young adults have requested participation in a structured young adult transition clinic or joint visits with a pediatric and adult care provider to increase engagement in adult care.61 Simply meeting an adult care provider prior to transfer has been associated with increased satisfaction.62 Egan et al57 piloted a program for 29 young adults with type 1 diabetes transitioning to adult-oriented health care. Participating young adult patients had one to two joint appointments with a pediatric and an adult health care provider prior to transfer to adult care and access to a transition coordinator to assist with appointment scheduling. All participants were seen at least twice in the first year of adult care and diabetes distress decreased over the same period, suggesting that joint appointments were successful in maintaining engagement in medical care across the transition period.57 Another program offered young adults (n=53; mean age =22 years) care in a structured transition clinic staffed by pediatric and adult endocrinologists and a transition coordinator. The joint clinic was highly attended, with 68% of participants attending three visits per year. Notably, of the participants with a previous lapse of >6 months between visits, nearly half met the recommended number of visits (three visits per year) during their first year in the joint clinic. A1c also decreased for attendees, suggesting that this targeted model of care was successful in improving glycemic control.63 If possible, it may be helpful to minimize the amount of change experienced during transition, including referring young adults for adult care in the same health care system/location as their pediatric care.62 Provision of continuity with the health care team or provider across the transition from pediatric to adult care also has been associated with decreased risk for diabetes-related hospitalization.53
Some transition programs have aimed to provide targeted education and resources for young adults moving to adult care. One comprehensive program, Let's Empower and Prepare (LEAP),56 provided a structured transition program to young adults to facilitate the transition to adult medical care. Intervention participants (n=51) received structured individual and group education targeted to young adult issues, access to transition coordinators and a dedicated young adult clinic, and membership in a private online community to discuss transition issues. A convenience sample control group received standard care. Results indicated that 78% of young adults in the intervention group successfully attended at least one adult care visit in the specialized young adult clinic created for this study. Intervention group participants also experienced an improvement in A1c (0.4%) as compared to a worsening in A1c for the control group (0.4%), suggesting that the resources provided in the intervention were successful in improving diabetes care.56 Another program49 offered a monthly support group designed to increase peer-to-peer social support for young adults aged 18–30 years with type 1 diabetes. Ten of the 15 group participants demonstrated an improvement in A1c from pre- to postgroup participation. Transition to adult care was a topic of discussion in the group, along with strategies for managing daily diabetes care and related emotional burden.49
Few randomized controlled trials have rigorously evaluated outcomes of transition programs. Steinbeck et al64 recruited 26 young adults during the transition to adult-oriented health care and randomly assigned them to receive either telephone support after leaving pediatric care or standard care. Results indicated that the provision of support posttransfer did not contribute to transition outcomes, including attendance in adult care and glycemic control; however, at 1 year, 88% of all participants were established in adult care.64 Another randomized controlled trial65 utilized technology to improve disease self-management in youth with chronic illness, including type 1 diabetes. Participants randomized to the intervention group received a 2-month Web- and text-message-based program designed to improve disease management skills prior to transition to adult care. The intervention group showed improved disease management and communication with health care providers as compared to the control group; however, this study did not examine outcomes over the transition to adult care.65
Resources for working with transition-aged youth with diabetes
There are a number of high-quality, freely available resources designed to promote successful transition to adult-oriented health care for patients and their families, as well as health care providers. Although the majority of these resources have not been rigorously evaluated, these are based on expert consensus, and research is beginning to evaluate specific components of transition programs that may be efficacious. Health care providers are encouraged to utilize these resources when working with transition-aged youth and to connect patients with targeted resources as necessary, based on patient needs and goals.
Got Transition, one of the largest sources of information about transition, represents a cooperative agreement between the Maternal and Child Health Bureau and the National Alliance to Advance Adolescent Health. While not specific to type 1 diabetes, Got Transition offers resources and tools for health care providers, patients, and families preparing for entrance into adult-oriented health care. The cornerstone of Got Transition's work concerns the Six Core Elements of Health Care Transition, reflecting best practices for the transition process. The Six Core Elements of Health Care Transition include the following: Transition Policy, Transition Tracking and Monitoring, Transition Readiness, Transition Planning, Transfer of Care, and Transfer Completion (www.gottransition.org). These elements have been implemented in clinical practice, resulting in individual- and practice-level improvements in key areas that promote successful transition to adult-oriented health care.33,66 A number of diabetes-specific resources for transition have also been developed for use by providers in routine clinical care, including resources from the Pediatric Endocrine Society, Endocrine Society, and National Diabetes Education Program (NDEP). Furthermore, patient advocacy organizations such as JDRF, formerly known as the Juvenile Diabetes Research Foundation, and the College Diabetes Network also have extensive resources geared toward young adult patients and their families. Table 2 highlights select online resources.
Table 2.
Sample resources to assist with the transition from pediatric to adult-oriented health care
| Organization | Web site | Target audience | Resources |
|---|---|---|---|
| Got Transition | www.gottransition.org | Health care providers, patients, families |
Information on best practices for general transition to adult-oriented health care; answers to frequently asked questions about transition |
| Pediatric Endocrine Society |
https://www.pedsendo.org/patients_families/transition_toolkit/index.cfm | Health care providers | Toolkit to assist pediatric providers with planning for, structuring, and facilitating patient transition to adult-oriented endocrinology care |
| Endocrine Society |
https://www.endocrine.org/education-and-practice-management/quality-improvement-resources/clinical-practice-resources/transition-of-care | Health care providers | Tools to implement in clinical practice with young adult patients preparing for and receiving care in the adult health care system |
| National Diabetes Education Program |
http://ndep.nih.gov/transitions | Health care providers, patients, families |
Transition planning checklist and clinical summary template for providers, links to information on health care and daily diabetes management for patients and families; includes in-person and online support groups |
| JDRF | http://typeonenation.org/resources/newly-diagnosed/t1d-toolkits/ | Adult patients | Toolkits for adults with type 1 diabetes, with information about diabetes management |
| College Diabetes Network |
https://collegediabetesnetwork.org/ | Young adult patients | Resources for diabetes management during young adulthood, including diabetes at college, navigating health insurance, and addressing diabetes in personal relationships |
Abbreviation: JDRF, Juvenile Diabetes Research Foundation.
Future directions
The transition from pediatric to adult-oriented health care has been an important topic of research and clinical care in recent years and many suggestions exist for improving this process. It is recommended that pediatric and adult endocrinology practices take an inventory of their current resources and approaches for transition and identify ways to incorporate additional supports for adolescents and young adults with type 1 diabetes. Resources such as Got Transition offer practice-level assessments that can be a starting point to identify areas for growth and improvement. Transition is not a discrete event that can be parceled out of comprehensive care for youth with diabetes. Much of the research supports transition as a gradual, integrated process built upon ongoing interactions with trusted health care providers, starting in early to mid-adolescence. Pediatric health care providers are in a unique position to encourage key diabetes management skills and behaviors that can contribute to improved health well into adulthood.
Future research should more rigorously evaluate promising models of transition education and care for youth with diabetes in order to develop a robust collection of evidence-based practices in this area. Sophisticated trial designs, such as randomized controlled trials, and long-term follow-up into adult medical care are needed. Furthermore, it is necessary to define and evaluate specific outcomes in adult-oriented health care to determine how “successful” transition can be measured and to identify key risk factors that may predispose youth to transition-related challenges, such as income, insurance status, and availability of specialty adult-oriented health care providers. Changes to the health care landscape ushered in by the Affordable Care Act,67 such as the ability to remain on a parent's insurance until age 26, may influence transition timing and procedures and promote more successful diabetes management during this period.
Conclusion
Late adolescence and young adulthood represent risky developmental periods characterized by poor glycemic control and related acute and chronic complications. The transition from pediatric to adult-oriented health care can present many challenges for patients, families, and health care providers, as well as exacerbating health concerns during this developmental period. Consistent engagement in high-quality diabetes care throughout young adulthood promotes health and well-being for youth and potentially prevents some of the complications experienced. However, identification of best practices to support successful transition to adult-oriented health care is in its early stage, and more research is needed to identify universal components of effective transition programs. Furthermore, models of adult care delivery may need to be modified to best meet the needs of young adult patients with type 1 diabetes. Health care providers can support the transition process by ongoing, integrated attention to developmental and health care system-related issues during preparation for adult-oriented health care and upon entrance into the adult-oriented health care system.
Acknowledgments
Dr Maureen Monaghan's work is currently funded by the National Institutes of Health (K23DK099250).
Footnotes
Disclosure The authors report no other conflicts of interest in this work.
References
- 1.Pettitt D, Talton J, Dabelea D, et al. SEARCH for Diabetes in Youth Study Group. Prevalence of diabetes in U.S. youth in 2009: the SEARCH for Diabetes in Youth Study. Diabetes Care. 2014;37(2):402–408. doi: 10.2337/dc13-1838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Patterson CC, Dahlquist GG, Gyurus E, et al. EURODIAB Study Group. Incidence trends for childhood type 1 diabetes in Europe during 1989–2003 and predicted new cases 2005–20: a multicentre prospective registration study. Lancet. 2009;373(9680):2027–2033. doi: 10.1016/S0140-6736(09)60568-7. [DOI] [PubMed] [Google Scholar]
- 3.Arnett J. Emerging adulthood: a theory of development from late teens through the twenties. Am Psychol. 2000;55(5):469–480. [PubMed] [Google Scholar]
- 4.Peters A, Laffel L. American Diabetes Association Transitions Working Group. Diabetes care for emerging adults: recommendations for transition from pediatric to adult diabetes care systems. Diabetes Care. 2011;34(11):2477–2485. doi: 10.2337/dc11-1723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.American Academy of Pediatrics. American Academy of Family Physicians. American College of Physicians Transitions Clinical Report Authoring Group Clinical report – supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics. 2011;128(1):182–200. doi: 10.1542/peds.2011-0969. [DOI] [PubMed] [Google Scholar]
- 6.Hynes L, Byrne M, Dinneen SF, McGuire BE, O'Donnell M, Mc Sharry J. Barriers and facilitators associated with attendance at hospital diabetes clinics among young adults (15–30 years) with type 1 diabetes mellitus: a systematic review. Pediatr Diabetes. doi: 10.1111/pedi.12198. Epub 2014 Aug 1. [DOI] [PubMed] [Google Scholar]
- 7.Garvey KC, Wolpert HA, Laffel LM, Rhodes ET, Wolfsdorf JI, Finkelstein JA. Health care transition in young adults with type 1 diabetes: barriers to timely establishment of adult diabetes care. Endocr Pract. 2013;19(6):946–952. doi: 10.4158/EP13109.OR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Garvey KC, Finkelstein JA, Laffel LM, Ochoa V, Wolfsdorf JI, Rhodes ET. Transition experiences and health care utilization among young adults with type 1 diabetes. Patient Prefer Adherence. 2013;7:761–769. doi: 10.2147/PPA.S45823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Helgeson VS, Reynolds KA, Snyder PR, et al. Characterizing the transition from paediatric to adult care among emerging adults with type 1 diabetes. Diabet Med. 2013;30(5):610–615. doi: 10.1111/dme.12067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Miller K, Foster N, Beck R, et al. T1D Exchange Clinic Network. Current state of type 1 diabetes treatment in the U.S.: updated data from the T1D exchange clinic registry. Diabetes Care. 2015;38(6):971–978. doi: 10.2337/dc15-0078. [DOI] [PubMed] [Google Scholar]
- 11.Petitti DB, Klingensmith GJ, Bell RA, et al. SEARCH for Diabetes in Youth Study Group. Glycemic control in youth with diabetes: the SEARCH for diabetes in Youth Study. J Pediatr. 2009;155(5):668–672. doi: 10.1016/j.jpeds.2009.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bryden K, Dunger D, Mayou R, Peveler RC, Neil HA. Poor prognosis of young adults with type 1 diabetes: a longitudinal study. Diabetes Care. 2003;26(4):1052–1057. doi: 10.2337/diacare.26.4.1052. [DOI] [PubMed] [Google Scholar]
- 13.Rewers A, Chase H, Mackenzie T, et al. Predictors of acute complications in children with type 1 diabetes. JAMA. 2002;287(19):2511–2518. doi: 10.1001/jama.287.19.2511. [DOI] [PubMed] [Google Scholar]
- 14.Cengiz E, Xing D, Wong J, et al. T1D Exchange Clinic Network. Severe hypoglycemia and diabetic ketoacidosis among youth with type 1 diabetes in the T1D exchange clinic registry. Pediatr Diabetes. 2013;14(6):447–454. doi: 10.1111/pedi.12030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ly T, Anderson M, McNamara K, Davis EA, Jones TW. Neurocognitive outcomes in young adults with early-onset type 1 diabetes: a prospective follow-up study. Diabetes Care. 2011;34(10):2192–2197. doi: 10.2337/dc11-0697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rollo A, Salardi S, Ciavarella A, et al. Transition from pediatric to adult care. Eight years after the transition from pediatric to adult diabetes care: metabolic control, complications and associated diseases. J Endocrinol Invest. 2014;37(7):653–659. doi: 10.1007/s40618-014-0090-9. [DOI] [PubMed] [Google Scholar]
- 17.Silverstein J, Klingensmith G, Copeland K. American Diabetes Association. Care of children and adolescents with type 1 diabetes: a statement of the American Diabetes Association. Diabetes Care. 2005;28(1):186–212. doi: 10.2337/diacare.28.1.186. [DOI] [PubMed] [Google Scholar]
- 18.Rohan J, Rausch J, Pendley J, et al. Identification and prediction of group-based glycemic control trajectories during the transition to adolescence. Health Psychol. 2014;33(10):1143–1152. doi: 10.1037/hea0000025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Clements M, Foster N, Maahs D, et al. T1D Exchange Clinic Network. Hemoglobin A1c (HbA1c) changes over time among adolescent and young adult participants in the T1D exchange clinic registry. Pediatr Diabetes. doi: 10.1111/pedi.12295. Epub 2015 Jul 8. [DOI] [PubMed] [Google Scholar]
- 20.Chiang JL, Kirkman MS, Laffel LM, Peters AL. Type 1 Diabetes Sourcebook Authors. Type 1 diabetes through the life span: a position statement of the American Diabetes Association. Diabetes Care. 2014;37(7):2034–2054. doi: 10.2337/dc14-1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rosen DS, Blum RW, Britto M, Sawyer SM, Siegel DM. Society for Adolescent Medicine. Transition to adult health care for adolescents and young adults with chronic conditions: position paper of the society for adolescent medicine. J Adolesc Health. 2003;33(4):309–311. doi: 10.1016/s1054-139x(03)00208-8. [DOI] [PubMed] [Google Scholar]
- 22.Dovey-Pearce G, Hurrell R, May C, Walker C, Doherty Y. Young adults' (16–25 years) suggestions for providing developmentally appropriate diabetes services: a qualitative study. Health Soc Care Community. 2005;13(5):409–419. doi: 10.1111/j.1365-2524.2005.00577.x. [DOI] [PubMed] [Google Scholar]
- 23.Pacaud D, Yale J, Stephure D, Trussell R, Davies H. Problems in transition from pediatric care to adult diabetes care for individuals with diabetes. Can J Diabetes. 2005;29(1):13–18. [Google Scholar]
- 24.Garvey K, Telo G, Needleman J, Forbes P, Finkelstein J, Laffel L. Health care transition in young adults with type 1 diabetes: perspectives of adult endocrinologists in the U.S. Diabetes Care. 2016;39(2):190–197. doi: 10.2337/dc15-1775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Geddes J, McGeough E, Frier B. Young adults with type 1 diabetes in tertiary education: do students receive adequate specialist care? Diabet Med. 2005;23:1155–1157. doi: 10.1111/j.1464-5491.2006.01933.x. [DOI] [PubMed] [Google Scholar]
- 26.Findley MK, Cha E, Wong E, Faulkner MS. A systematic review of transitional care for emerging adult with diabetes. J Pediatr Nurs. 2015;30(5):e47–e62. doi: 10.1016/j.pedn.2015.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Visentin K, Koch T, Kralik D. Adolescents with type 1 diabetes: transition between diabetes services. J Clin Nurs. 2006;15(6):761–769. doi: 10.1111/j.1365-2702.2006.01347.x. [DOI] [PubMed] [Google Scholar]
- 28.Schwartz LA, Tuchman LK, Hobbie WL, Ginsberg JP. A social-ecological model of readiness for transition to adult-oriented care for adolescents and young adults with chronic health conditions. Child Care Health Dev. 2011;37(6):883–895. doi: 10.1111/j.1365-2214.2011.01282.x. [DOI] [PubMed] [Google Scholar]
- 29.Sawicki GS, Lukens-Bull K, Yin X, et al. Measuring the transition readiness of youth with special healthcare needs: validation of the TRAQ – Transition Readiness Assessment Questionnaire. J Pediatr Psychol. 2011;36(2):160–171. doi: 10.1093/jpepsy/jsp128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ferris M, Cohen S, Haberman C, et al. Self-management and transition readiness assessment: development, reliability, and factor structure of the STARx questionnaire. J Pediatr Nurs. 2015;30(5):691–699. doi: 10.1016/j.pedn.2015.05.009. [DOI] [PubMed] [Google Scholar]
- 31.Schwartz LA, Daniel LC, Brumley LD, Barakat LP, Wesley KM, Tuchman LK. Measures of readiness to transition to adult health care for youth with chronic physical health conditions: a systematic review and recommendations for measurement testing and development. J Pediatr Psychol. 2014;39(6):588–601. doi: 10.1093/jpepsy/jsu028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.van Staa A, Sattoe J, Strating M. Experiences with and outcomes of two interventions to maximize engagement of chronically ill adolescents during hospital consultations: a mixed methods study. J Pediatr Nurs. 2015;30(5):757–775. doi: 10.1016/j.pedn.2015.05.028. [DOI] [PubMed] [Google Scholar]
- 33.McManus M, White P, Pirtle R, Hancock C, Ablan M, Corona-Parra R. Incorporating the six core elements of health care transition into a medicaid managed care plan: lessons learned from a pilot project. J Pediatr Nurs. 2015;30(5):700–713. doi: 10.1016/j.pedn.2015.05.029. [DOI] [PubMed] [Google Scholar]
- 34.Lotstein DS, Seid M, Klingensmith G, et al. SEARCH for Diabetes in Youth Study. Transition from pediatric to adult care for youth diagnosed with type 1 diabetes in adolescence. Pediatrics. 2013;131(4):e1062–e1070. doi: 10.1542/peds.2012-1450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Van Walleghem N, MacDonald CA, Dean HJ. Evaluation of a systems navigator model for transition from pediatric to adult care for young adults with type 1 diabetes. Diabetes Care. 2008;31(8):1529–1530. doi: 10.2337/dc07-2247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Holmes-Walker DJ, Llewellyn AC, Farrell K. A transition care programme which improves diabetes control and reduces hospital admission rates in young adults with Type 1 diabetes aged 15–25 years. Diabet Med. 2007;24(7):764–769. doi: 10.1111/j.1464-5491.2007.02152.x. [DOI] [PubMed] [Google Scholar]
- 37.de Beaufort C, Jarosz-Chobot P, Frank M, de Bart J, Deja G. Transition from pediatric to adult diabetes care: smooth or slippery? Pediatr Diabetes. 2010;11(1):24–27. doi: 10.1111/j.1399-5448.2009.00524.x. [DOI] [PubMed] [Google Scholar]
- 38.Lyons SK, Becker DJ, Helgeson VS. Transfer from pediatric to adult health care: effects on diabetes outcomes. Pediatr Diabetes. 2014;15(1):10–17. doi: 10.1111/pedi.12106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sharma N, O'Hare K, Antonelli RC, Sawicki GS. Transition care: future directions in education, health policy, and outcomes rsearch. Acad Pediatr. 2014;14(2):120–127. doi: 10.1016/j.acap.2013.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lyons S, Helgeson V, Witchel S, Becker DJ, Korytkowski MT. Physicians' self-perceptions of care for emerging adults with type 1 diabetes. Endocr Pract. 2015;21(8):903–909. doi: 10.4158/EP14553.OR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hilliard ME, Perlus JG, Clark LM, et al. Perspectives from before and after the pediatric to adult care transition: a mixed-methods study in type 1 diabetes. Diabetes Care. 2014;37(2):346–354. doi: 10.2337/dc13-1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Garvey KC, Wolpert HA, Rhodes ET, et al. Health care transition in patients with type 1 diabetes: young adult experiences and relationship to glycemic control. Diabetes Care. 2012;35(8):1716–1722. doi: 10.2337/dc11-2434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pyatak EA, Sequeira PA, Whittemore R, Vigen CP, Peters AL, Weigensberg MJ. Challenges contributing to disrupted transition from paediatric to adult diabetes care in young adults with type 1 diabetes. Diabet Med. 2014;31(12):1615–1624. doi: 10.1111/dme.12485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Balfe M, Doyle F, Smith D, et al. What's distressing about having type 1 diabetes? A qualitative study of young adults' perspectives. BMC Endocr Disord. 2013;13(1):25. doi: 10.1186/1472-6823-13-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Balfe M, Brugha R, Smith D, Sreenan S, Doyle F, Conroy R. Considering quality of care for young adults with diabetes in Ireland. BMC Health Serv Res. 2013;13:448. doi: 10.1186/1472-6963-13-448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Polfuss M, Babler E, Bush L, Sawin K. Family perspectives of components of a diabetes transition program. J Pediatr Nurs. 2015;30(5):748–756. doi: 10.1016/j.pedn.2015.05.010. [DOI] [PubMed] [Google Scholar]
- 47.Garvey K, Beste M, Luff D, Atakov-Castillo A, Wolpert HA, Ritholz MD. Experiences of health care transition voiced by young adults with type 1 diabetes: a qualitative study. Adolesc Health Med Ther. 2014;5:191–198. doi: 10.2147/AHMT.S67943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ritholz MD, Wolpert H, Beste M, Atakov-Castillo A, Luff D, Garvey KC. Patient-provider relationships across the transition from pediatric to adult diabetes care: a qualitative study. Diabetes Educ. 2014;40(1):40–47. doi: 10.1177/0145721713513177. [DOI] [PubMed] [Google Scholar]
- 49.Markowitz JT, Laffel LM. Transitions in care: support group for young adults with type 1 diabetes. Diabet Med. 2012;29(4):522–525. doi: 10.1111/j.1464-5491.2011.03537.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Duke D, Raymond J, Shimomaeda L, Harris MA. on behalf of the Harold Schnitzer Diabetes Health Center Transition Committee. Recommendations for transition from pediatric to adult diabetes care: patients' perspectives. Diabetes Manage. 2013;3(4):297–304. doi: 10.2217/dmt.13.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sheehan A, While A, Coyne I. The experiences and impact of transition from child to adult healthcare services for young people with type 1 diabetes: a systematic review. Diabet Med. 2015;32(4):440–458. doi: 10.1111/dme.12639. [DOI] [PubMed] [Google Scholar]
- 52.Mistry B, Van Blyderveen S, Punthakee Z, Grant C. Condition-related predictors of successful transition from paediatric to adult care among adolescents with type 1 diabetes. Diabet Med. 2015;32(7):881–885. doi: 10.1111/dme.12746. [DOI] [PubMed] [Google Scholar]
- 53.Nakhla M, Daneman D, To T, Paradis G, Guttmann A. Transition to adult care for youths with diabetes mellitus: findings from a universal health care system. Pediatrics. 2009;124(6):e1134–e1141. doi: 10.1542/peds.2009-0041. [DOI] [PubMed] [Google Scholar]
- 54.Pierce J, Wysocki T. Topical review: advancing research on the transition to adult care for type 1 diabetes. J Pediatr Psychol. 2015;40(10):1041–1047. doi: 10.1093/jpepsy/jsv064. [DOI] [PubMed] [Google Scholar]
- 55.Monaghan M, Helgeson V, Wiebe D. Type 1 diabetes in young adulthood. Curr Diabetes Rev. 2015;11(4):239–250. doi: 10.2174/1573399811666150421114957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sequeira P, Pyatak E, Weigensberg M, et al. Let's empower and prepare (LEAP): evaluation of a structured transition program for young adults with type 1 diabetes. Diabetes Care. 2015;38(8):1412–1419. doi: 10.2337/dc14-2577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Egan E, Corrigan J, Shurpin K. Building the bridge from pediatric to adult diabetes care: making the connection. Diabetes Educ. 2015;41(4):432–443. doi: 10.1177/0145721715581666. [DOI] [PubMed] [Google Scholar]
- 58.Lemly DC, Lawlor K, Scherer EA, Kelemen S, Weitzman ER. College health service capacity to support youth with chronic medical conditions. Pediatrics. 2014;134(5):885–891. doi: 10.1542/peds.2014-1304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Nieboer A, Cramm J, Sonneveld H, Roebroeck ME, van Staa A, Strating MM. Reducing bottlenecks: professionals' and adolescents' experiences with transitional care delivery. BMC Health Serv Res. 2014;14:47. doi: 10.1186/1472-6963-14-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Cadario F, Prodam F, Bellone S, et al. Transition process of patients with type 1 diabetes (T1DM) from paediatric to the adult health care service: a hospital-based approach. Clin Endocrinol. 2009;71(3):346–350. doi: 10.1111/j.1365-2265.2008.03467.x. [DOI] [PubMed] [Google Scholar]
- 61.Busse F, Hiermann P, Galler A, et al. Evaluation of patients' opinion and metabolic control after tranfer of young adults with type 1 diabetes from a pediatric diabetes clinic to adult care. Horm Res. 2007;67:132–138. doi: 10.1159/000096583. [DOI] [PubMed] [Google Scholar]
- 62.Kipps S, Bahu T, Ong K, et al. Current methods of transfer of young people with type 1 diabetes to adult services. Diabet Med. 2002;19:649–654. doi: 10.1046/j.1464-5491.2002.00757.x. [DOI] [PubMed] [Google Scholar]
- 63.Levy-Shraga Y, Elisha N, Ben-Ami M, et al. Glycemic control and clinic attendance of emerging adults with type 1 diabetes at a transition care clinic. Acta Diabetol. 2016;53:27–33. doi: 10.1007/s00592-015-0734-z. [DOI] [PubMed] [Google Scholar]
- 64.Steinbeck K, Shrewsbury V, Harvey V, et al. A pilot randomized controlled trial of a post-discharge program to support emerging adults with type 1 diabetes mellitus transition from pediatric to adult care. Pediatr Diabetes. 2014;16(8):634–639. doi: 10.1111/pedi.12229. [DOI] [PubMed] [Google Scholar]
- 65.Huang JS, Terrones L, Tompane T, et al. Preparing adolescents with chronic disease for transition to adult care: a technology program. Pediatrics. 2014;133(6):e1639–e1646. doi: 10.1542/peds.2013-2830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.McManus M, White P, Barbour A, et al. Pediatric to adult transition: a quality improvement model for primary care. J Adolesc Health. 2015;56:73–78. doi: 10.1016/j.jadohealth.2014.08.006. [DOI] [PubMed] [Google Scholar]
- 67.Monaghan M. The Affordable Care Act and implications for young adult health. Transl Behav Med. 2014;4(2):170–174. doi: 10.1007/s13142-013-0245-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Bridgett M, Abrahamson G, Ho J. Transition, it's more than just an event: supporting young people with type 1 diabetes. J Pediatr Nurs. 2015;30(5):e11–e14. doi: 10.1016/j.pedn.2015.05.008. [DOI] [PubMed] [Google Scholar]