Abstract
Death certificate inaccuracy is of major concern both in the public health domain and in individual health care, since it may yield untruthful data on the incidence, prevalence, and lethality of medical entities, and may hamper prophylactic measures among those who share, with the deceased, the common genetic, environmental, or behavioral risk factors. An effective way to settle this haziness relies on the increase of autopsy performance, increasing manifold the exactitude as well as facing surprising diagnoses. In this report, the authors present the case of a middle-aged woman who sought medical care because of back pain accompanied by weight loss. She died suddenly and unexpectedly in the Emergency Room. In this case, due to the unusual clinical presentation and the patient’s unexpected death, the causa mortis would not have been elucidated if the autopsy had not been undertaken.
Keywords: Endocarditis, Subacute Bacterial; Streptococcus; Leriche Syndrome
CASE REPORT
A 53-year-old Caucasian woman came to the hospital with a 1 month history of lower back pain radiating to the right lower limb, hampering her normal gait. In the same period, she referred weight loss (10 kg) accompanied by permanent tiredness and weakness. In the week before the admission, petechiae in the lower limbs overspread to the trunk and a reported fever (39°C) ensued. A laboratory work-up was undertaken before her admission, which showed high C-reactive protein and erythrocyte sedimentation rate; and high determinations of serum alkaline phosphatase, bilirubin, and gamma-glutamyl transferase. The platelet count was 37,000 per mm3, and leukocytosis of 14,800 per mm3 without a shift to the left. The lumbar spine magnetic resonance imaging (MRI) showed vertebral disc degeneration with a hernia at L5-S1 space. The Doppler ultrasonography of the lower limbs did not reveal any signs of venous flow disturbance.
The physical examination at admission revealed blood pressure of 90/46 mmHg; a respiratory rate of 17 breaths per minute; a heart rate of 96 beats per minute, blood oxygen saturation of 98%; and an axillary temperature of 35.7°C. Jaundice and palpable purpura at the lower limbs were evident, but pulmonary and heart auscultation were unremarkable. The abdominal examination showed hepatomegaly, with the liver edge palpable up to 2 cm below the rib cage. No signs of edema or ischemia at the extremities were present.
During the observation period, the patient started complaining of pain in the left leg. She was re-examined, and, in the face of an unchanged physical examination, codeine was prescribed. During the following hours, the patient's condition evolved and she began to complain of uneasiness, anxiety, and shortness of breath. Her heart rate rose to 120 beats per minute, and on auscultation a pericardial friction bruit was detected. The electrocardiogram showed right bundle block, supraventricular tachycardia, and deviation of the electrical axis to the right. Serum troponin I was of 2.01 ng/mL (reference value: <0.16 ng/mL). Soon after, she presented cardiac arrest in asystole. Advanced cardiac life support maneuvers were unsuccessful and the patient died. She was then referred to the pathology service for an autopsy.
AUTOPSY FINDINGS
At autopsy, the patient was icteric and had several coalescing elevated petechiae bilaterally at the lower limbs, characterizing a palpable purpura. At the opening of the abdominal cavity, abscesses were found in the left adrenal gland, the liver parenchyma, the spleen, and the cortex of the left kidney, and hepatomegaly was confirmed. In the right internal iliac artery, there was an embolization resulting in subtotal occlusion of the lumen, which was likely to be the cause of the patient’s leg pain. No thrombus or embolus was found at the lower limbs or the iliac veins. On microscopic examination, the abscesses of the adrenal, liver, spleen, and kidney were of septic origin, since bacterial clumps of Gram-positive cocci were found. The same findings were also present at the iliac artery embolus and in the glomerular capillaries—all of which yielded the diagnosis of systemic septic embolism.
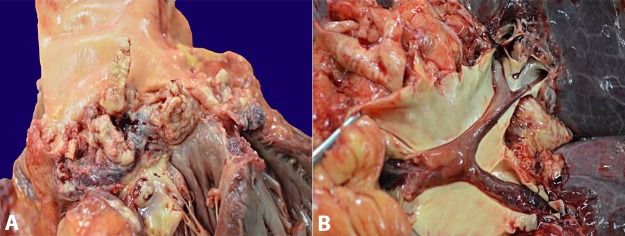
In the thoracic cavity several bilateral pulmonary subpleural hemorrhagic infarctions, a focus of acute bronchopneumonia, and edema were depicted. Mitral and aortic valves had vegetations (Figure 1A), and a thrombus of 6 cm in length extended from the right ventricle until the second-generation bifurcation of the right pulmonary artery (Figure 1B). The pulmonary thromboembolism was considered as the immediate causa mortis. The right atrium had a large-sized thrombus adhered to the free wall.
Figure 1. Gross findings of: A - Mitral valve with protruding vegetations; B - The opened pulmonary artery with saddle embolus.
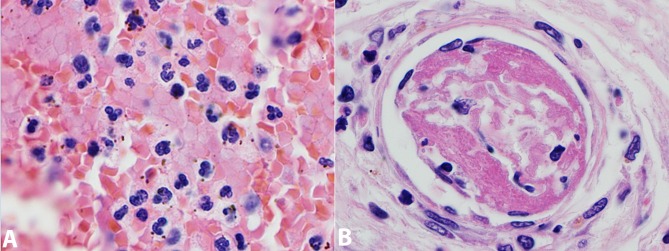
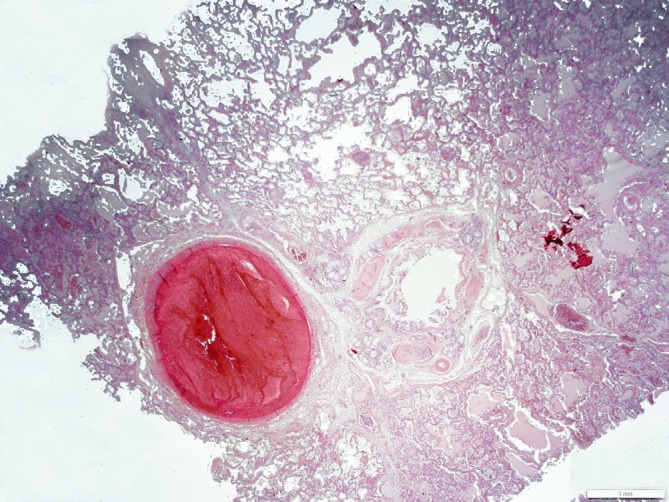
Histology of the pulmonary embolus showed Zahn lines (alternating between erythrocyte and platelet-fibrin aggregates deposition) (Figure 2), confirming the diagnosis of an embolus, and ruling out the suspicion of a postmortem clot.
Figure 2. Photomicrography of an intralobar pulmonary artery with the end of the saddle embolus.
The lung parenchyma showed alveoli filled with plasma and several foci of hemosiderin-laden macrophages, which, along with the sinusoidal dilation and the hepatomegaly, were consistent with the diagnosis of cardiac insufficiency. The heart failure was interpreted to be much more a consequence of the valvular destruction than of the acute pulmonary embolism. There was a focus of bronchopneumonia in the right lung lower lobe, with a mixed inflammatory infiltrate (both mononuclear and polymorphonuclear cells), engorged micro vessels, a low amount of alveolar and interstitial hemorrhage, and eosinophilic transudation material (Figure 3A). Gram stains were made but the results were inconclusive. Several micro emboli were found at the pulmonary microvasculature (Figure 3B), indicating an “embolic shower” and explaining the subpleural infarctions.
Figure 3. Photomicrography of the lung. A - Pulmonary alveoli filled with inflammatory cells and hyaline transudate; B - Peripheral pulmonary micro vessel with embolus.
In the cardiac muscle, we observed stretched, pale pink myocardial fibers with the infiltration of a few polymorphonuclear inflammatory cells, which were consistent with a subacute ischemic myocardial injury. The vegetations of the affected valves were sent for microbiological analysis, which revealed the growth of Streptococcus gallolyticus in both, confirming the septic origin of the emboli (pathogen identification by Vitek-2 compact). A thorough search was undertaken for microscopic signs that could point towards the diagnosis of the chronic rheumatic valvular disease, but there were none. Previous history for rheumatic fever evaluation was unavailable.
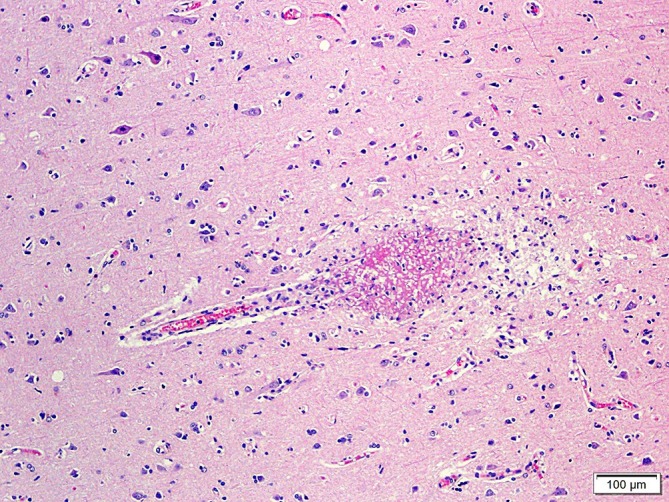
At the cut surface of the brain, several reddish spots scattered on the white matter were found to be microemboli at histology (Figure 4). The pineal gland was enlarged, measuring about 1.2 cm at its longest axis and weighed less than 1 g. Four distinct nodular gray matter heterotopias were spotted in the cerebral white matter of the temporal and parietal lobes.
Figure 4. Photomicrography of the brain showing capillary vessel destroyed by micro thrombus. The pineal gland showed numerous full-formed cysts filled with amorphous, acellular, eosinophilic material of unknown origin, which is consistent with the diagnosis of simple pineal cysts. The central nervous system (CNS) microemboli, in contrast with those in the renal glomeruli, were of fibrinous origin and showed no bacteria or inflammatory cells.
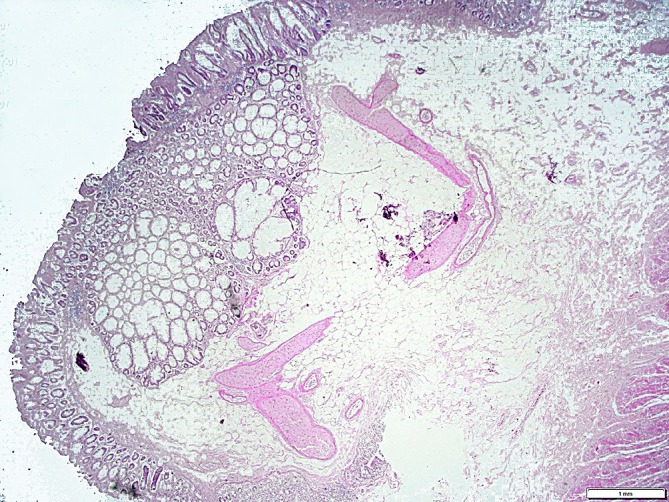
In the colonic lumen, there was a polypoid mass measuring 1.0 × 0.6 cm, which was diagnosed as a hyperplastic polyp at histology (Figure 5).
Figure 5. Photomicrography of the hyperplastic colonic polyp.
DISCUSSION
The microorganism S. gallolyticus, previously known as a subspecies of Streptococcus bovis biotype I,1 is a common cause of infectious endocarditis in individuals with colonic neoplasia. In a recent systematic review and meta-analysis,2 64% of the patients with S. bovis endocarditis simultaneously presented gastrointestinal disease, although only 6% of all infectious endocarditides are caused by this pathogen,3 which is associated with a low mortality rate when compared with other bacteria.4 Although S. gallolyticus endocarditis and septicemia are classically associated with colonic neoplasia or dysplasia, there is no evidence in the literature to support the hypothesis that hyperplastic polyps are also associated with it; therefore, in our case, we regarded the sole hyperplastic polyp to be an incidental finding. Several other findings in this autopsy could be attributed to the septicemia, including jaundice, bronchopneumonia, disseminated intravascular coagulation (especially in the brain and the lung), petechiae, bone marrow hypercellularity, and splanchnic abscesses. The bronchopneumonia was assumed also to be due to S. gallolyticus, but unfortunately we could not substantiate it even with the aid of the Gram stain and the culture.
The lack of fever at the time of the emergency consultation may likely account for the misdiagnosis; however, the patient presented fever in her medical history. The low back pain (her main complaint) was likely attributed to degenerative causes, such as osteoarthritis and osteoporosis, considering the epidemiological data. However, in the setting of the autopsy findings, her back pain could have been due to infectious discitis, vertebral osteomyelitis—both complications of infectious endocarditis—or distention of the renal capsule. At gross postmortem inspection there were no signs of discitis, and at microscopy of the vertebral bone marrow there were no signs of osteomyelitis. The vertebral hernia spotted on the MRI was very small and did not interfere with any adjacent structure. Hence, the distention of the renal capsule of the left kidney by the presence of the renal abscess remains the probable cause of her back pain.
Embolic events occur in nearly 27% of patients with infectious endocarditis; however, this rate is smaller in S. bovis endocarditis.4 The main site of embolism involves the CNS, followed by the spleen, the kidney, the lungs, the peripheral arteries, the mesentery, and the eye.5 Our patient had several septic emboli to the kidneys’ microvasculature and one semi-occlusive septic embolus into the iliac artery, besides the less obvious septic microemboli in the pulmonary and cerebral microvasculature. Pulmonary embolism is a potentially lethal condition characterized by the impaction of an embolus in some part of the pulmonary arterial tree, which is called “saddle embolism” or Leriche’s syndrome when the it impacts at the pulmonary artery bifurcation. Sometimes, the diagnosis of a pulmonary embolism is not straightforward, and estimates are that between 100,000 and 120,000 deaths occur each year in the United States because of this missed diagnosis.6
It is remarkable, in this case, that the clinical features and the final event were not enough to furnish a precise diagnosis. If the autopsy had not been performed, the case would have remained unclarified and certainly an inaccurate death certificate would have been reported. Death certificate information is a useful tool for epidemiologic and public health studies. The reliability of such certificates may be put under suspicion when they are not endorsed by postmortem examination, especially in the case of unexpected death.7 The S. gallolyticus infection and the pulmonary thromboembolism would not have been diagnosed without the autopsy. This information is important both to the family regarding the eventual colon cancer screening procedures,8 and to the public health statistics, allowing more precise data of mortality by this infectious agent.
CONCLUSION
Although infectious endocarditis is a relatively common disorder, this case was atypical because no colonic neoplasia or dysplasia was associated with the infection by S. bovis/gallolyticus. Moreover, the massive pulmonary thromboembolism is also not classically associated with S. gallolyticus endocarditis and sepsis. Also remarkable is the fact that the patient presented to the Emergency Room with vague complaints, which highlights the importance of being aware of signs of more severe, acute conditions in patients who seem otherwise stable in every scenario.
Footnotes
Starosta RT, Rivero R, Oliveira FH, Lopes E, Cerski MR. Misdiagnosis of Streptococcus gallolyticus endocarditis. Autopsy Case Rep [Internet]. 2016;6(3):29-33. http://dx.doi.org/10.4322/acr.2016.042
REFERENCES
- 1.Gómez-Garcés JL, Gil Y, Burillo A, Wilhelmi I, Palomo M. Cuadros clínicos asociados a bacteriemia causada por las nuevas especies incluidas en el antiguo grupo Streptococcus bovis. Enferm Infecc Microbiol Clin. 2012;30(4):175-9. http://dx.doi.org/10.1016/j.eimc.2011.09.015. PMid: [DOI] [PubMed] [Google Scholar]
- 2.Boleij A, van Gelder MM, Swinkels DW, Tjalsma H. Clinical Importance of Streptococcus gallolyticus infection among colorectal cancer patients: systematic review and meta-analysis. Clin Infect Dis. 2011;53(9):870-8. http://dx.doi.org/10.1093/cid/cir609. PMid: [DOI] [PubMed] [Google Scholar]
- 3.Alozie A, Köller K, Pose L, et al. Streptococcus bovis infectious endocarditis and occult gastrointestinal neoplasia: experience with 25 consecutive patients treated surgically. Gut Pathol. 2015;7(1):27-31. http://dx.doi.org/10.1186/s13099-015-0074-0. PMid: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kupferwasser I, Darius H, Müller AM, et al. Clinical and morphological characteristics in Streptococcus bovis endocarditis: a comparison with other causative microorganisms in 177 cases. Heart. 1998;80(3):276-80. http://dx.doi.org/10.1136/hrt.80.3.276. PMid: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thuny F, Di Salvo G, Belliard O, et al. Risk of embolism and death in infective endocarditis: prognostic value of echocardiography: a prospective multicenter study. Circulation. 2005;112(1):69-75. http://dx.doi.org/10.1161/CIRCULATIONAHA.104.493155. PMid: [DOI] [PubMed] [Google Scholar]
- 6.Calder KK, Herbert M, Henderson SO. The mortality of untreated pulmonary embolism in emergency department patients. Ann Emerg Med. 2005;45(3):302-10. http://dx.doi.org/10.1016/j.annemergmed.2004.10.001. PMid: [DOI] [PubMed] [Google Scholar]
- 7.Mieno MN, Tanaka N, Arai T, et al. Accuracy of death certificates and assesment of factors for misclassification for underlying cause of death. J Epidemiol. 2016;26(4):191-8. http://dx.doi.org/10.2188/jea.JE20150010. PMid: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Boleij A, Muytjens CM, Bukhari SI, et al. Novel clues on the specific association of Streptococcus gallolyticus subsp gallolyticus with colorectal cancer. J Infect Dis. 2011;203(8):1101-9. http://dx.doi.org/10.1093/infdis/jiq169. PMid: [DOI] [PubMed] [Google Scholar]