Abstract
Postoperative biliary leaks have become more common in the past three decades since the development of laparoscopic biliary surgery. The role of the radiologist and interventional radiologist is important in the diagnosis and treatment of such complications, and can play an adjunctive role in the definitive surgical repair. Ultrasound, computed tomography, magnetic resonance cholangiopancreatography, nuclear medicine cholescintigraphy studies, and percutaneous transhepatic cholangiograms (PTC) are the various imaging modalities used for diagnosis. Interventional radiology treatment involves percutaneous drainage of bilomas, characterization of the biliary tree and assessment of the site of ductal injury with PTC, and biliary diversion with external biliary drainage.
Keywords: biliary leak, biloma, percutaneous transhepatic cholangiogram, cholecystectomy, interventional radiology
Objectives: Upon completion of this article, the reader will be able to list the common imaging modalities used to diagnose and the common interventional therapies for management of biliary leaks.
Accreditation: This activity has been planned and implemented in accordance with the Essential Areas and Policies of the Accreditation Council for Continuing Medical Education (ACCME) through the joint providership of Tufts University School of Medicine (TUSM) and Thieme Medical Publishers, New York. TUSM is accredited by the ACCME to provide continuing medical education for physicians.
Credit: Tufts University School of Medicine designates this journal-based CME activity for a maximum of 1 AMA PRA Category 1 Credit™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Cholecystectomy is one of the most common operations performed in the United States, with approximately 500,000 operations performed every year.1 2 With the widespread introduction of laparoscopy in the late 1980s, laparoscopic cholecystectomy has become one of the most common minimally invasive operations for treatment of symptomatic gallbladder disease.2 With the advancements in both open and laparoscopic surgery, there has been an increase in the overall number of operations performed. Shortened recovery time, decreased postoperative pain, decreased size of abdominal wall incision, and shortened hospital stays increased the popularity of the laparoscopic approach for both surgeons and patients.2 3 4 5 Concomitant with the increased use of laparoscopic cholecystectomy came increasing rates of new complications, including biliary ductal injury with resultant biliary leakage. Incidences of biliary duct injury after laparoscopic cholecystectomy have been reported to be higher when compared with open surgery.3 Significant postoperative biliary ductal injury can occur up to 10 times more frequently with laparoscopic surgery than with open surgery.6 Biliary leaks may occur within 1-week postoperatively, but delayed clinical presentation my occur up to 1 month postoperatively.7 8
The clinical presentation of a patient with a postoperative biliary leak may include right upper quadrant pain, nausea, vomiting, anorexia, and fever.4 9 10 Laboratory findings may include leukocytosis and abnormal liver function tests. Leakage of bile can lead to the formation of a biloma, a discrete collection of bile outside the biliary tree.10 An encapsulated biloma can develop from slow biliary leakage with resultant inflammatory reaction and fibrosis in the area of deposition. The rate at which the abdominal peritoneum absorbs bile can determine the size and even location of the biloma.5 7 8 11
Biliary leaks and bilomas can occur from traumatic injury or iatrogenic injury, such as laparoscopic cholecystectomy, endoscopic retrograde cholangiopancreatography (ERCP), percutaneous transhepatic cholangiography (PTC), radiofrequency ablation of hepatic tumors, and liver biopsy. Postcholecystectomy leaks can occur from injury to the common bile duct, cystic duct stump, or small ducts that drain from the gallbladder fossa directly into the biliary system, known as accessory ducts of Luschka.
In this article, we focus on the diagnosis and management of postoperative biliary leaks, most commonly postcholecystectomy biliary leaks. Given the nonspecific clinical signs of biliary leaks, imaging plays a crucial role in diagnosis. The role of the radiologist and interventional radiologist is important in the diagnosis and treatment of such complications.8 9 10 12
Diagnosis
Several imaging modalities can be used in the diagnosis of postoperative biliary leaks and bilomas. These modalities include ultrasound (US), computed tomography (CT), magnetic resonance imaging (MRI), and nuclear medicine hepatobiliary cholescintigraphy.
Ultrasound
Sonography is often the initial imaging modality used to evaluate postoperative complications in patients presenting with right upper quadrant pain, or can be used for quick and efficient follow-up of fluid collections. US can be helpful for the assessment of intra-abdominal ascites, perihepatic and intrahepatic discrete fluid collections, and fluid collections in the gallbladder surgical bed, where postcholecystectomy bile leaks are commonly seen. A biloma can present as an anechoic well-circumscribed fluid collection, or a complex loculated collection with internal septations, which can be suggestive of secondary infection.1 3 7 8 11
Computed Tomography
CT can demonstrate discrete fluid collections with or without a surrounding peripheral capsule. The thickness of the rim around the fluid collection can be suggestive of the age of the biloma; longer chronicity of a collection may present with a thicker peripheral rim. The density of a biloma is commonly less than 20 Hounsfield units. High attenuating layering fluid may also be suggestive of hemorrhage. CT is an excellent study to identify a collection and assess the surrounding anatomy (Fig. 1a). However, differential diagnosis can include hematoma, abscess, seroma, hepatic cysts, or lymphoceles. If diagnosis of a biliary leak is still in question, follow-up imaging with CT may be helpful by demonstrating progression of size of a low-attenuating collection in the perihepatic/intrahepatic region. CT also plays a role in the assessment of further complications of biliary leaks, as demonstration of peritoneal thickening and enhancement may be suggestive of biliary peritonitis.7 8
Fig. 1.
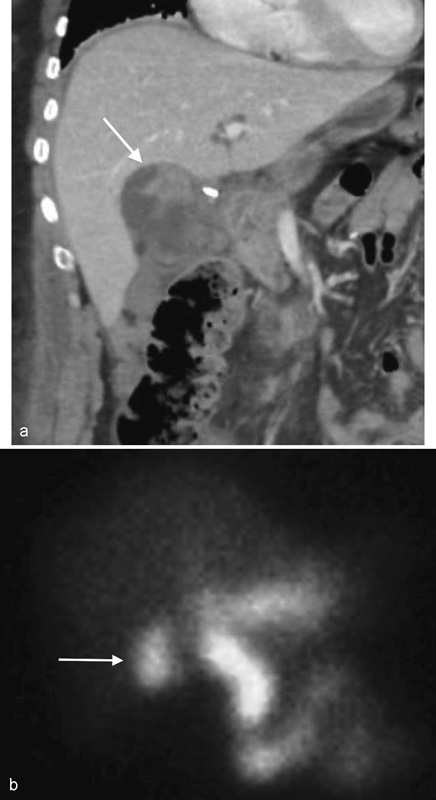
A 50-year-old woman with right upper quadrant abdominal pain 2 days after laparoscopic cholecystectomy. (a) Coronal reconstructed image from contrast-enhanced CT abdomen demonstrates a fluid collection of variable density within the gallbladder fossa (arrow). (b) Hepatobiliary cholescintigraphy reveals activity in the region of the cystic duct stump that diffuses into the abdominal right upper quadrant (arrow), consistent with biliary leak.
Other imaging modalities such as MRI and hepatobiliary cholescintigraphy can be useful for demonstrating the source of biliary leakage, as will be discussed later.
Hepatobiliary Cholescintigraphy
Hepatobiliary cholescintigraphy can demonstrate functional and physiological information, including active leakage and contained fluid collections (Figs. 1b and 2a). Cholescintigraphy uses Tc-99m-iminodiacetic acid chelate complex as a radiotracer, and can detect leaks in lower concentrations than contrast-enhanced CT.7 8 13 14
Fig. 2.
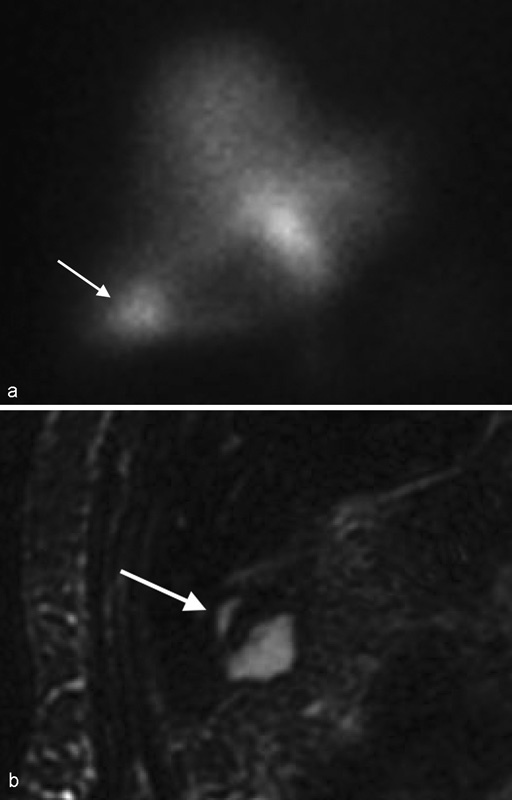
A 77-year-old woman with prior cholecystectomy and concern for bile leak status post right nephrectomy. (a) Hepatobiliary cholescintigraphy demonstrates a bile leak at the inferior right liver lobe (arrow). (b) Coronal MRCP reveals a small laceration at the inferior right liver lobe (arrow), corresponding to the location of bile leak on the HIDA scan.
However, these studies are limited by poor spatial resolution, which can make identification of the precise location of a leak difficult. Studies are also time consuming, as delayed imaging is often required, which can take 4 to 24 hours postinjection. The use of single photon emission computed tomography (SPECT) is helpful in demonstrating more detailed anatomy. With SPECT, identifying the source of a leak in relation to the liver capsule and parenchyma can be helpful in guiding interventional therapy for more effective percutaneous drain placements.7 8 13 14
Magnetic Resonance Imaging
A biloma on MR appears as hypointense signal on T1WI and hyperintense signal on T2WI. High T1 and low T2 signal may suggest concentrated layering biliary fluid. There may be demonstration of rim enhancement. MRCP with hepatobiliary contrast agents can assist in showing a source of biliary leak, as well as distinguishing between fluid collections of biliary and nonbiliary origin. MRCP can also be helpful in demonstrating communications between the biliary ducts and a fluid collection, as well as showing the extent of biliary ductal injury (Fig. 2b). Accessory biliary ducts, such as ducts of Luschka, which can be a source of biliary leak, can also be demonstrated on MRCP.7 8
Invasive diagnostic modalities to assess for biliary leaks include ERCP, in which therapeutic management such as placement of biliary stents can be performed, and PTC (discussed later). Limitations of ERCP include lack of evaluation of the biliary tree proximal to where a leak is demonstrated, and difficulty in passage of the endoscope in postsurgical biliary-enteric anastomosis.7 13
Management
Percutaneous biloma drainage: The interventional radiologist's role in the management of biliary leakage includes biliary diversion away from the site of ductal injury and percutaneous drainage of bilomas.
Clinical history and imaging are often times sufficient in the diagnosis of a biloma; however, fluid aspiration may be required for definitive diagnosis. For drainage of bilomas, a percutaneous Seldinger technique can be utilized using an 18- or 22-gauge coaxial needle with the assistance of US, fluoroscopy, or CT guidance. The liver parenchyma can be traversed to reach the collection, at the discretion of the operator. Using US, real-time color sonography can identify any nearby vascular structures to avoid traversing major vessels. Intraprocedural bleeding can be treated via manual sonographic compression with the US probe and/or injection of gelfoam.8 10 13
The use of CT guidance allows more detailed information of surrounding intra-abdominal anatomy. The drawbacks of CT guidance include radiation exposure, lack of real-time imaging, and decreased flexibility compared with a portable US probe. For larger superficial fluid collections, the trocar technique may be used in place of the Seldinger technique with US or CT guidance. Drains may stay in place until the patient's clinical picture improves, drainage output decreases significantly, and/or a follow-up CT or US demonstrates resolution or significant reduction in size of the biloma.8 13 15
Percutaneous Transhepatic Cholangiography with Percutaneous Transhepatic Biliary Drain Placement
PTC is performed for the evaluation of the biliary system prior to percutaneous intervention to demonstrate biliary anatomy proximal to the site of ductal injury, and aid in procedural planning for optimal drain placement and positioning. PTC can also be used to assess for biliary ductal ligation and transection. Coagulopathy is a relative contraindication for percutaneous intra-abdominal drainage procedures, with a desired international normalized ratio of less than 1.5 and a platelet count of 50 × 109 cells/L or higher.1 13 16 17 18 19 Other relative contraindications include allergy to iodinated contrast agents and large volume ascites. In the case of large volume ascites, preprocedural paracentesis may be performed.15
For the PTC procedure, the patient is placed supine and the skin overlying the anticipated approach is sterilely prepared. Depending on the site of ductal leakage, a left sub-xiphoid or right mid-axillary approach can be performed for left or right intrahepatic ductal system injury, respectively. For a right-sided approach, the entry point is chosen along the right mid-axillary line, preferably one to two interspaces below the 10th rib to avoid traversing the lung pleura. Fluoroscopy can also be used to mark the position of maximal lung descent. The overlying skin is anesthetized, and a small 5-mm dermatotomy is made with a no. 11 blade. A 21- or 22-gauge needle-stylet is then inserted through the skin incision, parallel to the table and directed toward the spine (12th vertebral body). Alternatively, a left-sided approach may be performed by inserting the needle between the xiphoid process of the sternum and the medial edges of the costal margins to access the left hepatic lobe. The stylet is then withdrawn and approximately 50% dilute contrast is injected via a syringe (small quick injections) while slowly withdrawing the needle out until the biliary ducts are opacified with contrast medium (Figs. 3a, b and 4a). Contrast that is inadvertently injected into a portal vein or hepatic artery branch will be seen flowing toward the periphery of the liver, whereas bile will flow centrally and clear at a slower rate. Care must be taken to limit biliary manipulation and the amount of contrast injection in the biliary ducts in the setting of suspected cholangitis, to prevent overdistending the biliary ducts, as the patient can be at risk for sepsis.1 6 8 13 15 17
Fig. 3.

PTC, internal/external drain, follow-up. A 55-year-old man status post laparoscopic cholecystectomy complicated by bile leak. (a) Coronal contrast-enhanced CT image demonstrates cholecystectomy clips and a fluid collection adjacent to the common bile duct (arrow). (b) Fluoroscopic image during PTC reveals amorphous extraluminal contrast at the level of the cystic duct stump (arrow) consistent with leak. (c) An 8F internal/external biliary drain was placed for diversion, with distal tip in the duodenum (arrow). (d) Cholangiography performed 4 months later shows no evidence of leak.
Fig. 4.
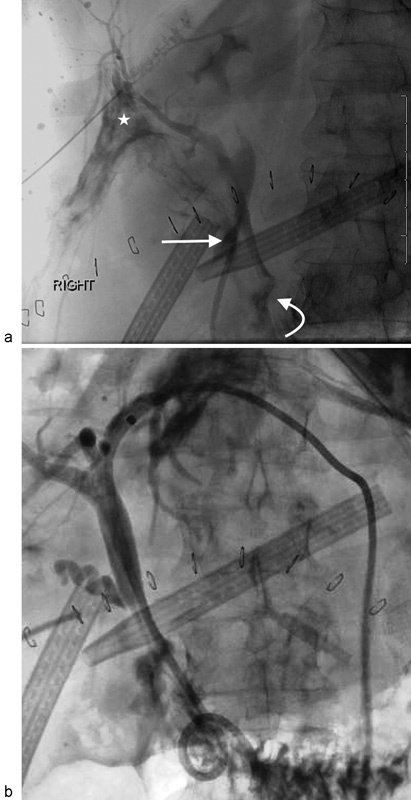
A 74-year-old woman after Whipple procedure for periampullary cancer. (a) Fluoroscopic image during right PTC demonstrates amorphous contrast pooling between two surgical drains (arrow) consistent with a leak arising near the choledochojejunal anastomosis (curved arrow). There is also contrast staining the hepatic parenchyma and opacification of the lymphatic system (asterisk). (b) Placement of an 8F internal/external biliary drain via left-sided approach after a wire was unable to be advanced through the nondilated right ducts.
After anatomic detail of the biliary tree is demonstrated, a percutaneous transhepatic biliary drain can be placed to divert bile from the site of injury to allow acute inflammatory effects to settle and allow healing (Figs. 3c and 4b). If the initial accessed biliary duct is not sufficiently peripheral, or does not allow for an optimal angle of entry for drain placement, then a second needle may be inserted with fluoroscopic guidance. An external drain can be placed with the tip immediately proximal to the site of biliary ductal injury. This may definitively treat the biliary leak (Fig. 3d) or serve as a temporizing effort prior to definitive surgical repair.2 13
Operative management for external biliary ductal injury can include placement of a T-tube stent, which allows bridging of the site of leakage as well as external biliary drainage. An intraoperative cholangiography can help confirm and locate the site of leakage. Immediate operative management may also include primary end-to-end anastomotic repair of the injured bile duct. The definitive surgical treatment for biliary duct injuries is best achieved by means of a Roux-en-Y hepaticojejunostomy procedure, performed by an experienced hepatobiliary surgeon.18 20
Conclusion
Postoperative biliary ductal injuries can present with a myriad of problems resulting in significant morbidity, including biliary peritonitis, cholangitis, and sepsis.1 Postoperative bilomas can become colonized by bacteria and become infected if left undrained.3 Multiple imaging modalities are utilized for swift diagnosis and treatment planning. Interventional radiological treatment in the case of postoperative bile duct injury involves percutaneous drainage of fluid collections, characterization of the biliary tract anatomy and assessment of the site and extent of bile duct injury with PTC, and biliary diversion from the site of bile leakage with external biliary drainage. Percutaneous interventional procedures can result in definitive treatment or temporization prior to definitive surgical repair.6 13
References
- 1.vanSonnenberg E, Casola G, Wittich G R. et al. The role of interventional radiology for complications of cholecystectomy. Surgery. 1990;107(6):632–638. [PubMed] [Google Scholar]
- 2.Bezzi M, Silecchia G, Orsi F. et al. Complications after laparoscopic cholecystectomy. Coordinated radiologic, endoscopic, and surgical treatment. Surg Endosc. 1995;9(1):29–36. doi: 10.1007/BF00187881. [DOI] [PubMed] [Google Scholar]
- 3.Nuñez D Jr, Becerra J L, Martin L C. Subhepatic collections complicating laparoscopic cholecystectomy: percutaneous management. Abdom Imaging. 1994;19(3):248–250. doi: 10.1007/BF00203518. [DOI] [PubMed] [Google Scholar]
- 4.vanSonnenberg E, D'Agostino H B, Easter D W. et al. Complications of laparoscopic cholecystectomy: coordinated radiologic and surgical management in 21 patients. Radiology. 1993;188(2):399–404. doi: 10.1148/radiology.188.2.8327685. [DOI] [PubMed] [Google Scholar]
- 5.Stathopoulos V, Georganas M, Stratakis K, Delaporta E, Karallas E, Koutsopoulos K. Hepatic subcapsular biloma: a rare complication of laparoscopic cholecystectomy. Case Rep Surg. 2014;2014:186819. doi: 10.1155/2014/186819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kaufman J A, Lee M J. Philadelphia, PA: Elsevier Health Sciences; 2013. Vascular and Interventional Radiology. [Google Scholar]
- 7.Melamud K, LeBedis C A, Anderson S W, Soto J A. Biliary imaging: multimodality approach to imaging of biliary injuries and their complications. Radiographics. 2014;34(3):613–623. doi: 10.1148/rg.343130011. [DOI] [PubMed] [Google Scholar]
- 8.Copelan A, Bahoura L, Tardy F, Kirsch M, Sokhandon F, Kapoor B. Etiology, diagnosis, and management of bilomas: a current update. Tech Vasc Interv Radiol. 2015;18(4):236–243. doi: 10.1053/j.tvir.2015.07.007. [DOI] [PubMed] [Google Scholar]
- 9.Oliva V L, Nicolet V, Soulez G. et al. Bilomas developing after laparoscopic biliary surgery: percutaneous management with embolization of biliary leaks. J Vasc Interv Radiol. 1997;8(3):469–473. doi: 10.1016/s1051-0443(97)70591-8. [DOI] [PubMed] [Google Scholar]
- 10.Vazquez J L, Thorsen M K, Dodds W J. et al. Evaluation and treatment of intraabdominal bilomas. AJR Am J Roentgenol. 1985;144(5):933–938. doi: 10.2214/ajr.144.5.933. [DOI] [PubMed] [Google Scholar]
- 11.Gould L, Patel A. Ultrasound detection of extrahepatic encapsulated bile: “biloma”. AJR Am J Roentgenol. 1979;132(6):1014–1015. doi: 10.2214/ajr.132.6.1014. [DOI] [PubMed] [Google Scholar]
- 12.Peters J H, Ellison E C, Innes J T. et al. Safety and efficacy of laparoscopic cholecystectomy. A prospective analysis of 100 initial patients. Ann Surg. 1991;213(1):3–12. doi: 10.1097/00000658-199101000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thompson C M, Saad N E, Quazi R R, Darcy M D, Picus D D, Menias C O. Management of iatrogenic bile duct injuries: role of the interventional radiologist. Radiographics. 2013;33(1):117–134. doi: 10.1148/rg.331125044. [DOI] [PubMed] [Google Scholar]
- 14.Rosenberg D J, Brugge W R, Alavi A. Bile leak following an elective laparoscopic cholecystectomy: the role of hepatobiliary imaging in the diagnosis and management of bile leaks. J Nucl Med. 1991;32(9):1777–1781. [PubMed] [Google Scholar]
- 15.Pomerantz B J. Biliary tract interventions. Tech Vasc Interv Radiol. 2009;12(2):162–170. doi: 10.1053/j.tvir.2009.08.009. [DOI] [PubMed] [Google Scholar]
- 16.Dewhurst C, Kane R A, Mhuircheartaigh J N, Brook O, Sun M, Siewert B. Complication rate of ultrasound-guided percutaneous cholecystostomy in patients with coagulopathy. AJR Am J Roentgenol. 2012;199(6):W753–W760. doi: 10.2214/AJR.11.8445. [DOI] [PubMed] [Google Scholar]
- 17.Kandarpa K, Machan L. Philadelphia, PA: Lippincott Williams & Wilkins; 2011. Handbook of Interventional Radiologic Procedures. [Google Scholar]
- 18.Lau W Y, Lai E C, Lau S H. Management of bile duct injury after laparoscopic cholecystectomy: a review. ANZ J Surg. 2010;80(1–2):75–81. doi: 10.1111/j.1445-2197.2009.05205.x. [DOI] [PubMed] [Google Scholar]
- 19.Patel I J, Davidson J C, Nikolic B. et al. Consensus guidelines for periprocedural management of coagulation status and hemostasis risk in percutaneous image-guided interventions. J Vasc Interv Radiol. 2012;23(6):727–736. doi: 10.1016/j.jvir.2012.02.012. [DOI] [PubMed] [Google Scholar]
- 20.Lepsien G, Lüdtke F E, Neufang T, Schafmayer A, Peiper H J. Treatment of iatrogenic common bile duct injury during laparoscopic cholecystectomy through the laparoscopic insertion of a T-tube stent. Surg Endosc. 1991;5(3):119–122. doi: 10.1007/BF02653216. [DOI] [PubMed] [Google Scholar]


