Abstract
Clinical data such as history, physical examination, and laboratory tests are useful in identifying patients with biliary obstruction and biliary sources of infection. However, if intervention is planned, noninvasive imaging is needed to confirm the presence, location, and extent of the disease process. Currently, the most commonly available and used noninvasive modalities are ultrasound (US), computed tomography (CT), magnetic resonance (MR), and nuclear medicine hepatobiliary scintigraphy (HIDA). US is quick, portable, readily available, and is commonly the first imaging modality used when biliary pathology is suspected. It is excellent in the detection of cholelithiasis and acute cholecystitis but is limited in detecting choledocholithiasis. CT is excellent at detecting infected postoperative fluid collections, bilomas, biliary obstruction, and biliary infection but is limited in the detection of cholelithiasis. Therefore, US may be more useful than CT for the initial screening of acute biliary disease. MR has inherent advantages over CT, as it does not use ionizing radiation, can be done without intravenous contrast, and its detection of cholelithiasis is not affected by the internal composition of the stone. Magnetic resonance cholangiopancreatography can be used to determine the cause and location of biliary obstruction but is limited in the detection of small stones and the evaluation of the biliary tract near the ampulla. HIDA is used to evaluate for cholecystitis, biliary obstruction, and bile leaks. The main limitation is its lack of anatomical detail, and it is therefore frequently performed in conjunction with other described modalities.
Keywords: cholelithiasis, cholecystitis, interventional radiology, biliary obstruction, biloma
Objectives: Upon completion of this article, the reader will be able to describe the various modalities available for noninvasive biliary imaging and the benefits and use of each in the diagnosis of various biliary pathologies.
Accreditation: This activity has been planned and implemented in accordance with the Essential Areas and Policies of the Accreditation Council for Continuing Medical Education (ACCME) through the joint providership of Tufts University School of Medicine (TUSM) and Thieme Medical Publishers, New York. TUSM is accredited by the ACCME to provide continuing medical education for physicians.
Credit: Tufts University School of Medicine designates this journal-based CME activity for a maximum of 1 AMA PRA Category 1 Credit™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Biliary imaging in an infected patient aims to find the source of infection such as acute cholecystitis, bilomas in the postoperative setting, or cholangitis in the patient with suspected biliary obstruction. In the setting of biliary obstruction, imaging is focused on detecting the level of obstruction, its severity, and cause. Frequently, biliary imaging requires a multimodality approach starting with ultrasound (US) and continuing with cross-sectional imaging such as computed tomography (CT) or magnetic resonance (MR).
Ultrasonography
US is a readily available, portable, noninvasive, and inexpensive technology. A common indication for US is workup of right upper quadrant pain and suspected gallbladder or biliary pathology.
US is very accurate in detecting calcified and noncalcified gallstones and gallbladder sludge with a reported sensitivity of 97% and specificity of 95%.1 On sonography, gallstones appear as echogenic luminal filling defects with posterior acoustic shadowing.2 Gallbladder sludge is imaged as layering low-level echoes that form a fluid-debris level along the dependent portion of the gallbladder.
US is excellent at detecting acute gallbladder inflammation with a sensitivity and specificity of 94 and 78%, respectively.1 The sonographic features of acute cholecystitis include gallbladder distention, wall thickening, pericholecystic inflammation, gallbladder wall hyperemia, and right upper quadrant pain on exam (Fig. 1).2 Acute cholecystitis may progress to gangrenous cholecystitis, which will be seen as membranes within the gallbladder as a result of fibrinous strands of exudate from the mucosa. Gangrenous cholecystitis may perforate, and if it does, a collection may be seen surrounding the gallbladder.
Fig. 1.
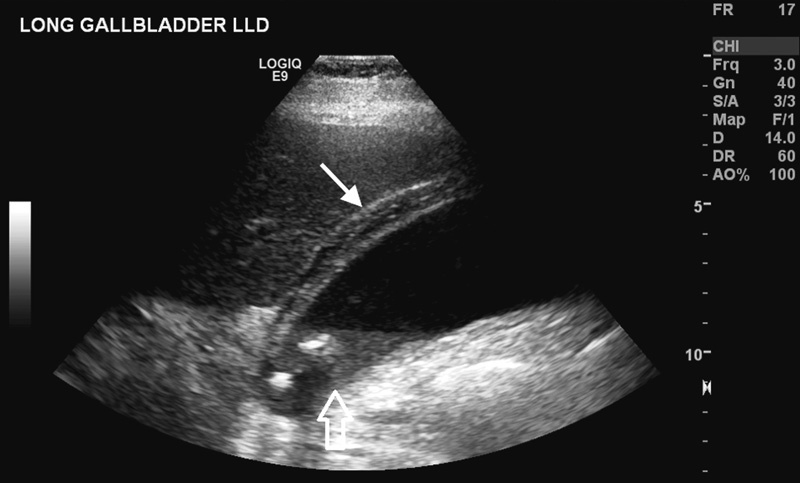
Ultrasound of the gallbladder in a 78-year-old man with right upper quadrant pain. Ultrasound image shows gallbladder wall thickening (solid white arrow) and echogenic stones near the neck with some gallbladder sludge (open white arrow).
US is also commonly used in the workup of biliary obstruction. In cases of suspected biliary obstruction, the presence of dilated intrahepatic ducts and a dilated common bile duct (CBD) is considered indirect evidence of biliary obstruction. However, the presence of normal ducts does not exclude obstruction, as not every case of biliary obstruction is accompanied by ductal dilation. Conversely, CBD dilation does not imply biliary obstruction, as it can be seen in healthy patients after cholecystectomy and as part of the normal process of aging. Despite these pitfalls, US is good in detecting extrahepatic obstruction with an accuracy of 79 to 98% and when used in combination with clinical evaluation, it can accurately differentiate between liver parenchymal disease and extrahepatic obstruction.3 US may not always image the distal CBD due to bowel gas and overlying structures and therefore it may not always detect the level of obstruction or the cause. Because of these limitations, variable sensitivity has been reported in evaluating the level of obstruction (27–95%) and cause (23–88%) of extrahepatic biliary obstruction.3 US is not accurate in differentiating benign from malignant causes of obstruction (47–90%) nor is it sensitive in detecting choledocholithiasis (25–58%) (Fig. 2).3
Fig. 2.
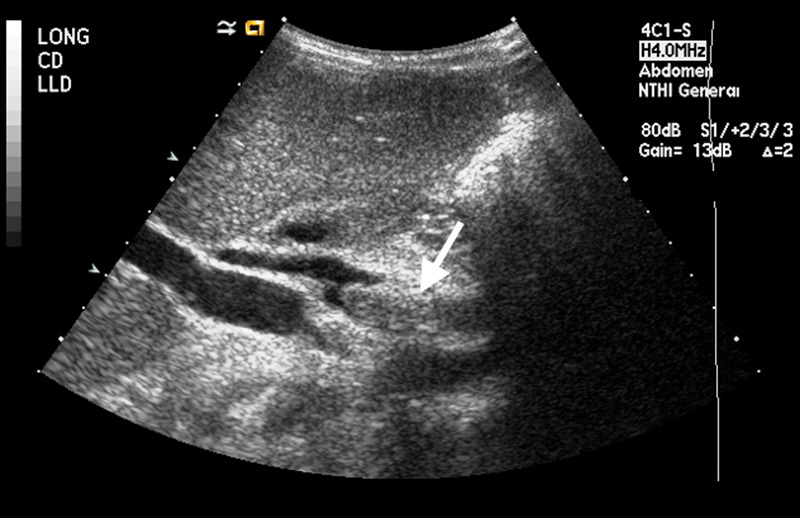
Ultrasound of the common bile duct in a 30-year-old woman with biliary obstruction. Ultrasound image shows an echogenic stone (arrow) located in the common bile duct.
US is often used after cholecystectomy to detect bile leaks and collections and has a sensitivity of 70% in the detection of intra-abdominal bile collections.4 On US, a biloma is a well-circumscribed anechoic collection in the gallbladder fossa or in the perihepatic area. Internal complexity with septations suggests infection of the biloma, but can also be seen in evolving hematomas and abscesses. Percutaneous sampling and drainage may be needed to distinguish these entities.
Computed Tomography
CT is a commonly employed modality in patients with abdominal pain and is frequently used to evaluate biliary-related infection and obstruction. It is useful in evaluating large patients or patients with multisystem disease, which may not be easily evaluated by US.
While CT is not as accurate as US in detecting gallstones, its sensitivity can be improved by modifying the technique. When imaging is performed at 140 kVp as opposed to a lower kVp, the sensitivity for gallstone detection improves from 67 to 86%. The ability to detect gallstones also increases with increasing calcium content of the stone.5
CT has a reported sensitivity of 92.5% in detecting acute cholecystitis.6 The most specific imaging features of acute cholecystitis on CT are pericholecystic fat stranding, mural stratification, pericholecystic enhancement, gallbladder distention, and wall thickening6 (Fig. 3). Emphysematous cholecystitis is a more severe variant of acute cholecystitis with secondary infection of the gallbladder wall by gas-forming organisms (Fig. 4). It is more frequently seen in patients with diabetes and is associated with a higher rate of gallbladder perforation. CT is a more sensitive and specific modality for the identification of gas in the gallbladder lumen or wall than US, as gallstones or gallbladder wall calcification can impede evaluation by US.7
Fig. 3.

Axial contrast-enhanced CT scan of the gallbladder in a 59-year-old man with abdominal pain. CT image shows gallbladder wall thickening (arrow), hyperenhancement, and pericholecystic fluid in the setting of gallstones.
Fig. 4.

Axial contrast-enhanced CT scan of the gallbladder in an 89-year-old diabetic man with sepsis. CT image shows foci of gas (arrow) within the gallbladder lumen, indicative of emphysematous cholecystitis.
In evaluating biliary obstruction, CT is able to accurately detect dilated intra- and extrahepatic bile ducts when the study is performed with intravenous contrast. Choledocholithiasis is the most common cause of benign biliary obstruction and sensitivities for the detection of CBD stones on conventional CT have ranged from 25 to 90% with most studies reporting sensitivities in the ninth decile.8 The direct imaging findings of choledocholithiasis include the target sign with the stone seen as a central density surrounded by hypoattenuating bile or ampullary soft tissue and the crescent sign (Fig. 5), where the dense calculus is surrounded by a crescent of hypoattenuating bile. Indirect signs include abrupt termination of the duct or ductal dilatation.8
Fig. 5.

Axial contrast-enhanced CT scan of the distal common bile duct in a 30-year-old woman with biliary obstruction. CT image shows a stone (asterisk) in the distal common bile duct with a crescent of bile surrounding the stone.
In cases of malignant strictures, the enhancing soft-tissue mass can be seen either within or encircling the duct. With malignant strictures, the involved segment tends to be longer, has a thicker enhancing wall, and more extensive upstream biliary dilation.9 In cases where biliary stents have been placed, CT is useful in evaluating stent patency. Findings in cases of stent obstruction include new upstream biliary ductal dilation and loss of pneumobilia, which is a result of gas reflux from the bowel (Fig. 6).10 In cases of biliary obstruction due to malignant ingrowth, curved planar reformatted images of the stent show enhancing tissue within the stent lumen, a finding that is specific for tumor ingrowth.11
Fig. 6.

Coronal contrast-enhanced CT of the liver in a 74-year-old woman with jaundice and indwelling plastic common bile duct stent. CT image shows dilated bile ducts (arrow) and gallbladder distention indicating stent dysfunction.
Biliary obstruction can lead to infection and life-threatening acute cholangitis. CT can be used to assess patients with biliary obstruction for acute cholangitis with a reported sensitivity and specificity of 89.7 and 84.6%, respectively.12 CT features of acute cholangitis are nodular, patchy, wedge-shaped, or geographic inhomogeneous enhancement throughout the liver in the arterial phase on dynamic CT (Fig. 7). Infection or inflammation of the ducts can also cause ductal hyperenhancement.13
Fig. 7.
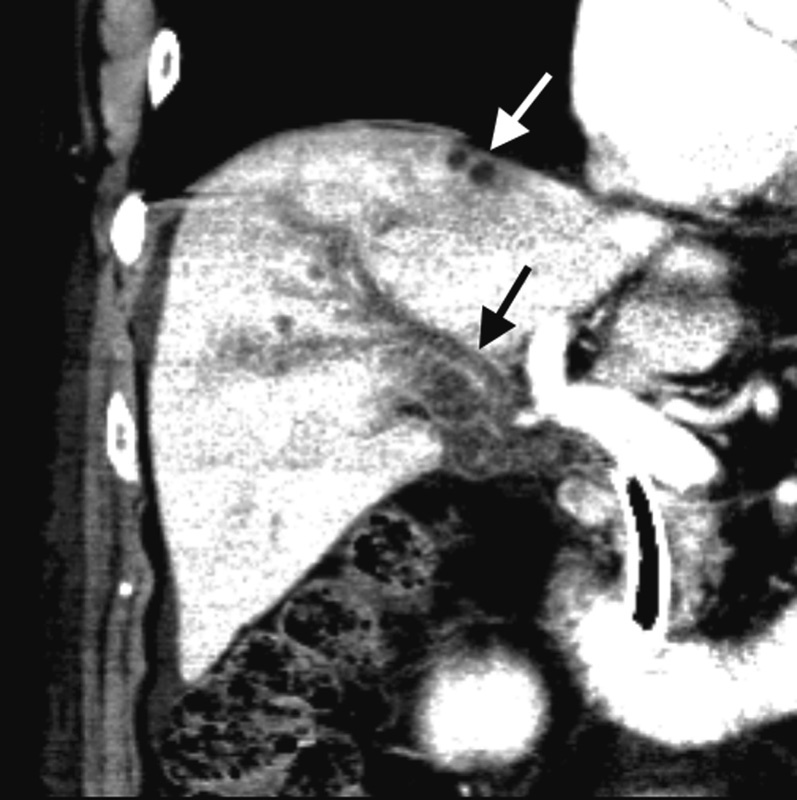
Coronal contrast-enhanced CT of the liver in an 89-year-old man with sepsis and indwelling metal common bile duct stent. CT image shows perfusional changes near the dome of the liver with a small developing liver abscess (white arrow). Note the hyperenhancing obstructed ducts (black arrow) indicating inflammation or infection.
CT is an excellent modality for evaluating the infected postoperative patient with a reported sensitivity of 95% for detection of intra-abdominal bile collections.4 Infected fluid collections have an enhancing wall, local mass effect, and may contain locules of gas (Fig. 8). The benefit of CT in imaging-infected collections is that it can be used as a modality to guide catheter drainage and can image deeper abdominal collections.
Fig. 8.

Axial contrast-enhanced CT scan of the gallbladder fossa in an 85-year-old woman with infection after cholecystectomy. CT image shows fluid collection (asterisk) in the gallbladder fossa consistent with a postoperative abscess.
Magnetic Resonance
Magnetic resonance cholangiopancreatography (MRCP) is performed with heavily T2-weighted sequences that produce bright signal in stationary fluids. The benefit of MR is that biliary imaging can be performed without intravenous contrast or ionizing radiation. Functional MRCP can be performed by using intravenous contrast agents that have biliary excretion.
MR, unlike CT, is able to reliably image stones in the biliary tree and is not limited by stone composition. Gallstones are imaged as filling defects in the gallbladder or biliary tree (Fig. 9). Pigmented gallstones are hyperintense on three-dimensional, fast spoiled gradient echo and are hypointense on T2-weighted imaging.14 In a meta-analysis of 67 published controlled trials, MRCP had an overall sensitivity of 95% and specificity of 97% in determining the level and presence of biliary obstruction.15 Sensitivity of MRCP to detect stones is 91% and decreases with stone size as follows: 67 to 100% for stones greater than 10 mm, 89 to 94% for stones 6 to 10 mm, and 33 to 71% for stones smaller than 6 mm.3
Fig. 9.
Magnetic resonance cholangiopancreatography (MRCP) in a 38-year-old woman with biliary obstruction. MRCP image shows multiple luminal filling defects (arrow) in a dilated common bile duct consistent with choledocholithiasis.
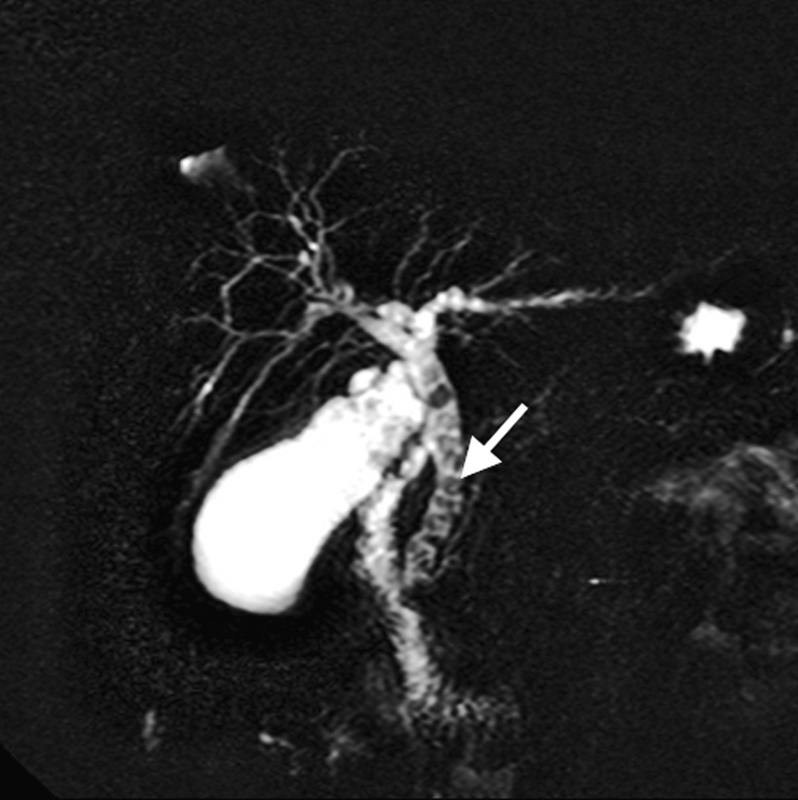
MRCP has an accuracy of 88% in differentiating benign from malignant strictures.15 It is useful in the diagnosis of malignant biliary obstruction due to cholangiocarcinoma and is able to identify the location, extent, and severity of obstruction (Fig. 10).3 Given its good performance, MRCP can evaluate surgical candidates and help guide biliary drainage via a percutaneous or endoscopic retrograde cholangiopancreatography (ERCP) route depending on the location of the blockage.
Fig. 10.
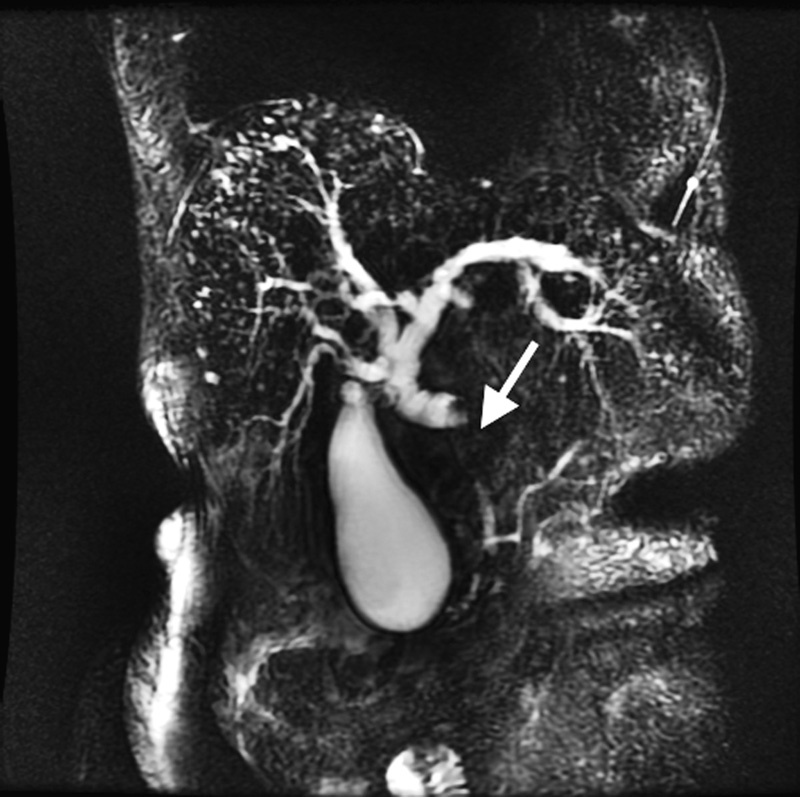
Magnetic resonance cholangiopancreatography (MRCP) in a 63-year-old woman with jaundice. MRCP image shows intrahepatic and proximal biliary ductal dilation. There is a long segment stricture in the mid common bile duct (arrow) due to an underlying cholangiocarcinoma.
MRCP is 84% as sensitive as ERCP in detecting pancreatic cancer with ductal dilation; however, the detection of pancreatic cancer by MRCP in cases without significant ductal dilation is difficult, as focal ductal interruption is an important indirect sign of an underlying mass. Imaging of ampullary lesions is particularly difficult due to gas artifact from the duodenum.16
Functional MR cholangiography is performed using lipophilic paramagnetic contrast agents that have hepatobiliary excretion. Contrast-enhanced cholangiography is superior in (1) demonstrating communications between cystic liver lesions and draining bile ducts in the diagnosis of congenital biliary disorders; (2) demonstrating biliary excretion in cases with dilated ducts to differentiate between true and pseudoobstruction; (3) demonstrating extravasation of biliary contrast in suspected bile leaks.17
In suspected infected fluid collections, diffusion-weighted imaging has been shown to differentiate between infected and noninfected fluid collections, as abscesses tend to restrict movement of water molecules compared with bland fluid collections. This feature can be exploited to guide appropriate drainage when multiple collections are present.18
Nuclear Medicine Hepatobiliary Imaging
HIDA scanning has excellent accuracy in detecting acute cholecystitis. It has been shown to be superior to US in accuracy with an overall sensitivity and specificity of 97 and 94%, respectively.19 On HIDA, the absence of gallbladder visualization after radiotracer injection is indicative of cystic duct obstruction. Nonvisualization of the gallbladder 1 hour after radiotracer injection is abnormal but not specific for acute cholecystitis. The diagnosis is made with higher specificity if delayed imaging at 3 to 4 hours shows no gallbladder visualization.20 HIDA is more accurate for diagnosing acalculous cholecystitis than US or CT. An assessment of cystic duct patency with cholescintigraphy is probably the best strategy for imaging suspected acalculous cholecystitis.21
HIDA scanning is used in the postoperative detection of bile leaks and collections (biloma). Bile leaks and bilomas are detected as an extravasation of radiotracer into the gallbladder fossa or abdomen. HIDA is more specific than US or CT for bile leaks, as radiotracer should not be present outside the biliary system or bowel.22 Frequently, HIDA scanning is used in conjunction with a modality such as CT or US for better delineation of anatomy.
Conclusion
Noninvasive biliary imaging is accurate in the infected patient, in patients with gallbladder disease and with benign or malignant biliary obstruction. US, CT, and MRI play complementary roles in the imaging of biliary tract disease. US is frequently the initial test in the assessment of patients with suspected biliary obstruction, as it is widely available and relatively inexpensive. CT and MR have added value in determining the cause of obstruction, particularly if it is located distally in the biliary tree, and can also provide added information on the extent of disease.
References
- 1.Shea J A, Berlin J A, Escarce J J. et al. Revised estimates of diagnostic test sensitivity and specificity in suspected biliary tract disease. Arch Intern Med. 1994;154(22):2573–2581. [PubMed] [Google Scholar]
- 2.Bortoff G A, Chen M Y, Ott D J, Wolfman N T, Routh W D. Gallbladder stones: imaging and intervention. Radiographics. 2000;20(3):751–766. doi: 10.1148/radiographics.20.3.g00ma16751. [DOI] [PubMed] [Google Scholar]
- 3.Tse F, Barkun J S, Romagnuolo J, Friedman G, Bornstein J D, Barkun A N. Nonoperative imaging techniques in suspected biliary tract obstruction. HPB (Oxford) 2006;8(6):409–425. doi: 10.1080/13651820600746867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee C M Stewart L Way L W Postcholecystectomy abdominal bile collections Arch Surg 20001355538–542., discussion 542–544 [DOI] [PubMed] [Google Scholar]
- 5.Chan W C, Joe B N, Coakley F V. et al. Gallstone detection at CT in vitro: effect of peak voltage setting. Radiology. 2006;241(2):546–553. doi: 10.1148/radiol.2412050947. [DOI] [PubMed] [Google Scholar]
- 6.Soyer P, Hoeffel C, Dohan A. et al. Acute cholecystitis: quantitative and qualitative evaluation with 64-section helical CT. Acta Radiol. 2013;54(5):477–486. doi: 10.1177/0284185113475798. [DOI] [PubMed] [Google Scholar]
- 7.Grayson D E, Abbott R M, Levy A D, Sherman P M. Emphysematous infections of the abdomen and pelvis: a pictorial review. Radiographics. 2002;22(3):543–561. doi: 10.1148/radiographics.22.3.g02ma06543. [DOI] [PubMed] [Google Scholar]
- 8.Miller F H, Hwang C M, Gabriel H, Goodhartz L A, Omar A J, Parsons W G III. Contrast-enhanced helical CT of choledocholithiasis. AJR Am J Roentgenol. 2003;181(1):125–130. doi: 10.2214/ajr.181.1.1810125. [DOI] [PubMed] [Google Scholar]
- 9.Choi S H, Han J K, Lee J M. et al. Differentiating malignant from benign common bile duct stricture with multiphasic helical CT. Radiology. 2005;236(1):178–183. doi: 10.1148/radiol.2361040792. [DOI] [PubMed] [Google Scholar]
- 10.Thomas S, Patel R P, Oto A. Resolution of pneumobilia as a predictor of biliary stent occlusion. Clin Imaging. 2015;39(4):650–653. doi: 10.1016/j.clinimag.2015.03.010. [DOI] [PubMed] [Google Scholar]
- 11.Bang B W, Jeong S, Lee D H, Kim C H, Cho S G, Jeon Y S. Curved planar reformatted images of MDCT for differentiation of biliary stent occlusion in patients with malignant biliary obstruction. AJR Am J Roentgenol. 2010;194(6):1509–1514. doi: 10.2214/AJR.09.3060. [DOI] [PubMed] [Google Scholar]
- 12.Kim S W, Shin H C, Kim H C, Hong M J, Kim I Y. Diagnostic performance of multidetector CT for acute cholangitis: evaluation of a CT scoring method. Br J Radiol. 2012;85(1014):770–777. doi: 10.1259/bjr/72001875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Arai K, Kawai K, Kohda W, Tatsu H, Matsui O, Nakahama T. Dynamic CT of acute cholangitis: early inhomogeneous enhancement of the liver. AJR Am J Roentgenol. 2003;181(1):115–118. doi: 10.2214/ajr.181.1.1810115. [DOI] [PubMed] [Google Scholar]
- 14.Tsai H M, Lin X Z, Chen C Y, Lin P W, Lin J C. MRI of gallstones with different compositions. AJR Am J Roentgenol. 2004;182(6):1513–1519. doi: 10.2214/ajr.182.6.1821513. [DOI] [PubMed] [Google Scholar]
- 15.Romagnuolo J, Bardou M, Rahme E, Joseph L, Reinhold C, Barkun A N. Magnetic resonance cholangiopancreatography: a meta-analysis of test performance in suspected biliary disease. Ann Intern Med. 2003;139(7):547–557. doi: 10.7326/0003-4819-139-7-200310070-00006. [DOI] [PubMed] [Google Scholar]
- 16.David V, Reinhold C, Hochman M. et al. Pitfalls in the interpretation of MR cholangiopancreatography. AJR Am J Roentgenol. 1998;170(4):1055–1059. doi: 10.2214/ajr.170.4.9530058. [DOI] [PubMed] [Google Scholar]
- 17.Griffin N, Charles-Edwards G, Grant L A. Magnetic resonance cholangiopancreatography: the ABC of MRCP. Insights Imaging. 2012;3(1):11–21. doi: 10.1007/s13244-011-0129-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sinha R Rajiah P Ramachandran I Sanders S Murphy P D Diffusion-weighted MR imaging of the gastrointestinal tract: technique, indications, and imaging findings Radiographics 2013333655–676., discussion 676–680 [DOI] [PubMed] [Google Scholar]
- 19.Ziessman H A. Nuclear medicine hepatobiliary imaging. Clin Gastroenterol Hepatol. 2010;8(2):111–116. doi: 10.1016/j.cgh.2009.10.017. [DOI] [PubMed] [Google Scholar]
- 20.Weissmann H S, Frank M S, Bernstein L H, Freeman L M. Rapid and accurate diagnosis of acute cholecystitis with 99mTc-HIDA cholescintigraphy. AJR Am J Roentgenol. 1979;132(4):523–528. doi: 10.2214/ajr.132.4.523. [DOI] [PubMed] [Google Scholar]
- 21.O'Connor O J, Maher M M. Imaging of cholecystitis. AJR Am J Roentgenol. 2011;196(4):W367–74. doi: 10.2214/AJR.10.4340. [DOI] [PubMed] [Google Scholar]
- 22.Rayter Z, Tonge C, Bennett C, Thomas M, Robinson P. Ultrasound and HIDA: scanning in evaluating bile leaks after cholecystectomy. Nucl Med Commun. 1991;12(3):197–202. [PubMed] [Google Scholar]


