Abstract
Choledocholithiasis occurs in up to approximately 20% of patients with cholelithiasis. A majority of stones form in the gallbladder and then pass into the common bile duct, where they generate symptoms, due to biliary obstruction. Confirmatory diagnosis of choledocholithiasis is made with advanced imaging, including magnetic resonance cholangiopancreatography and endoscopic retrograde cholangiopancreatography (ERCP). Treatment varies locally; however, ERCP with sphincterotomy is most commonly employed with a high degree of success. Difficult anatomy and difficult stone burden require advanced surgical, endoscopic, and percutaneous techniques to extract or expel biliary stones. Knowledge of these treatment strategies will optimize outcomes.
Keywords: choledocholithiasis, diagnosis, endoscopy, percutaneous, interventional radiology, treatment
Objectives: Upon completion of this article, the reader will be able to discuss the diagnostic evaluation of choledocholithiasis together with management strategies, including advanced and percutaneous techniques, for difficult biliary anatomy and challenging stone burden.
Accreditation: This activity has been planned and implemented in accordance with the Essential Areas and Policies of the Accreditation Council for Continuing Medical Education (ACCME) through the joint providership of Tufts University School of Medicine (TUSM) and Thieme Medical Publishers, New York. TUSM is accredited by the ACCME to provide continuing medical education for physicians.
Credit: Tufts University School of Medicine designates this journal-based CME activity for a maximum of 1 AMA PRA Category 1 Credit™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
The presence of a stone or stones within the common bile duct (CBD) is known as choledocholithiasis. Choledocholithiasis is reported in 3 to 22% of cholecystectomies.1 2 In distinction to cholelithiasis, the majority of choledocholithiasis is symptomatic—specifically, right upper quadrant pain, caused by distention of the extrahepatic bile duct, along with nausea and vomiting.3 Complications of choledocholithiasis include acute pancreatitis and cholangitis. Acute cholangitis presents with Charcot's triad (fever, right upper quadrant pain, jaundice), along with leukocytosis. Biliary pancreatitis results in marked elevation of serum amylase and lipase levels.4
Biliary stones are classified by chemical composition: cholesterol (>70% cholesterol), mixed (30% < cholesterol < 70%), and pigmented (cholesterol < 30%).5 Cholesterol and mixed gallstones form in the gallbladder after the concentration of cholesterol has exceeded the solubilizing ability of lecithin and bile salts. Cholesterol precipitates out of solution into crystals forming the gallstone nucleus.6 Cholesterol and mixed stones share common risk factors and they make up 80 to 90% of gallstones found upon cholecystectomy in Western societies.6
Pigment stones are classified into black and brown stones. Black stones are formed in the gallbladder from polymerized calcium bilirubinate. Black stones are associated with hemolytic disorders, cystic fibrosis, and Crohn disease.7 8 9 Brown stones are softer and composed of unpolymerized calcium bilirubinate.9 Brown stones are generally found in the extrahepatic and intrahepatic ducts, in the presence of bacterial infection and biliary stasis.10 Bacterial by-products and enzymes, notably β-glucuronidase, cause precipitation of bilirubin out of solution, thus forming a brown stone.9 Brown stones are associated with recurrent pyogenic cholangitis and biliary parasites.9 10 11
Choledocholithiasis is classified as primary or secondary according to stone origin.3 Primary choledocholithiasis refers to stones formed directly within the biliary tree, while secondary choledocholithiasis refers to stones ejected from the gallbladder. Primary choledocholithiasis is generally composed of brown stones and is rare in Western populations. Secondary choledocholithiasis stone composition parallels that of cholelithiasis, with cholesterol as the most common type.3
Initial Workup
The diagnosis of choledocholithiasis is initially suggested by symptomatology, laboratory tests, and ultrasound (US) findings. Individually, each of these variables has a poor sensitivity and specificity for choledocholithiasis.12 13 The American Society of Gastrointestinal Endoscopy (ASGE) developed a stratification model for the probability of choledocholithiasis—specifically, low (<10%), intermediate (10–50%), and high risk (>50%), based on age, symptoms, liver biochemical tests, and US findings.14 Very strong predicators are the presence of a CBD stone on transabdominal US, acute cholangitis, and serum bilirubin greater than 4 mg/dL. The liver function test pattern of choledocholithiasis is an initial elevation of aspartate aminotransferase and alanine transaminase, with a delayed rise in alkaline phosphatase and total bilirubin with persistent biliary obstruction.3
Transabdominal US is often the initial imaging study in patients with suspected choledocholithiasis, as it is readily available, noninvasive, portable, and low cost. Biliary stones appear echogenic and round with acoustic shadowing. In a meta-analysis, US had a sensitivity of 73% and specificity of 91% for detecting a CBD stone.2 3 The distal CBD is particularly difficult to evaluate, due to overlying bowel gas, as compared with ease of gallbladder evaluation. US can reliably detect a dilated extrahepatic bile duct, typically a CBD > 6 mm, which is an indirect sign of choledocholithiasis. However, a large study of patients undergoing cholecystectomy found that nearly half of the patients with choledocholithiasis had a nondilated CBD.15 Moreover, the diameter of the extrahepatic bile duct increases with age, and as such, older patients may have a normal duct greater than 6 mm. Largely, due to its poor sensitivity, a negative US does not rule out choledocholithiasis.
A computed tomographic (CT) scan is frequently obtained in the evaluation of abdominal pain. The literature regarding CT for diagnosis of choledocholithiasis is heterogeneous and it is usually not considered a definitive test. Many gallstones are similar in density to surrounding bile and lack calcium, which limits CT conspicuity and hence sensitivity. CT diagnosis of choledocholithiasis may be improved by the addition of a hepatobiliary-excreted intravenous contrast agent.16 17 Similar to US, it is able to detect biliary ductal dilation, a secondary sign of choledocholithiasis (Fig. 1).
Fig. 1.
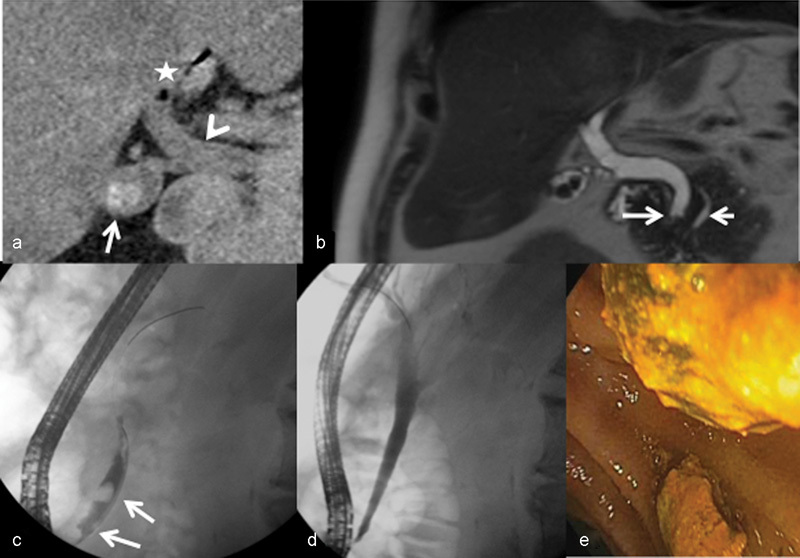
A 71-year-old man with abdominal pain and elevated liver function tests. Patient has a remote history of cholelithiasis, sphincterotomy for choledocholithiasis, and refusal of cholecystectomy. (a) Non–contrast-enhanced CT of the abdomen demonstrating cholelithiasis (arrow) with dilated common bile duct (CBD) (arrowhead) and pneumobilia (asterisk). (b) Magnetic resonance cholangiopancreatography showing cholelithiasis and choledocholithiasis (long arrow) with a dilated CBD and prominent pancreatic duct (short arrow) without evidence of pancreatitis. (c) Endoscopic retrograde cholangiopancreatography with multiple filling defects consistent with choledocholithiasis (arrows). (d) Cholangiogram after balloon extraction of stones with resolution of filling defects. (e) Endoscopic image of biliary stones in the duodenum.
Confirmatory Diagnosis
Definitive diagnosis of choledocholithiasis is made with advanced imaging, consisting of magnetic resonance cholangiopancreatography (MRCP), endoscopic retrograde cholangiopancreatography (ERCP), endoscopic ultrasound (EUS), intraoperative cholangiography (IOC), intraoperative ultrasound (IUS), and percutaneous transhepatic cholangiography (PTC). The best method for the diagnosis of choledocholithiasis is controversial, as each modality has benefits and shortcomings.
Magnetic Resonance Cholangiopancreatography
MRCP utilizes T2-weighted images to visualize the filling defects (biliary stones) or stenosis in the slow moving fluid within the biliary tree (Fig. 1).18 If extrahepatic cholestasis is present, the configuration of bile, at the point of obstruction, signals the underlying cause (benign vs. malignant). An impacted biliary stone will appear as a rounded filling defect with a crescent of bile.19 In distinction to ERCP, imaging of prestenotic segments is not limited. MRCP is also the preferred imaging modality for the assessment of intrahepatic stone burden.3 Utilizing a contrast agent, with biliary excretion on T1-weighted images, can give additional information about the degree of obstruction, and allows for better visualization of the CBD in patients with ascites. There is no significant difference in diagnostic ability of T1 contrast-enhanced and T2 MRCP for the diagnosis of choledocholithiasis.20 In a study of 34 patients with choledocholithiasis, MRCP identified 91% of biliary stones, yet stones smaller than 5 mm were detected only in 71% of cases.21 MRCP is recommended for patients with intermediate probability of choledocholithiasis by the ASGE.1 14
Endoscopic Ultrasound
EUS utilizes an US probe mounted on the tip of an endoscope. EUS does not require ionizing radiation, is sensitive for stones smaller than 5 mm, and has a much lower complication rate (0.1–0.3%) than ERCP.14 EUS may not be appropriate in patients with postsurgical anatomy, as it requires approximation of the US probe to the CBD. EUS is not limited by bowel gas, as seen with transabdominal US. A systematic review identified a high diagnostic accuracy for both EUS and MRCP for choledocholithiasis—specifically, a sensitivity of 95% and specificity of 97% for EUS, and a sensitivity of 93% and specificity of 96% for MRCP.22 As such, patients with a negative EUS or MRCP do not require invasive evaluation for choledocholithiasis. The choice between EUS and MRCP, for intermediate probability choledocholithiasis, is based on the resource availability, experience, and costs.23
Endoscopic Retrograde Cholangiopancreatography
ERCP is a diagnostic and therapeutic procedure, which entails cannulating the ampulla of Vater and CBD with injection of contrast under fluoroscopy, and observing for filling defects (Fig. 1). ERCP is often used as the reference standard to evaluate choledocholithiasis. ERCP has a complication rate of 8 to 12%, most commonly manifesting as pancreatitis.24 25 26 ERCP is recommended for patients with high probability of choledocholithiasis, due both to its invasiveness and ability to treat, if choledocholithiasis is discovered.14
Intraoperative Cholangiography and Intraoperative Ultrasound
In the operating room, the surgeon may undertake IOC and IUS utilizing a laparoscopic or open surgical approach. IOC is the direct injection of the biliary tree with a water-soluble contrast agent, with radiographic visualization, to detect choledocholithiasis and delineate biliary anatomy. This anatomic delineation reduces the risk of operative CBD injury.27 IOC is highly sensitive (99%) and specific (99%) for the diagnosis of choledocholithiasis, according to a recent systematic review.28 Use of IOC is debated among surgeons, and according to a 2008 survey, it is not routinely performed.27
IUS allows evaluation of the biliary tree during laparoscopic surgery, including detection of choledocholithiasis and delineation of biliary anatomy. Advantages of this technique over IOC include no requirement for cannulation of the biliary tree and no iodinated contrast or ionizing radiation exposure.29 A single-center retrospective study documented a sensitivity of 95% and specificity of 100% for bile duct stones.30 However, the performance of IUS is strongly operator dependent with a slow learning curve and it is not widely available.29
Percutaneous Transhepatic Cholangiography
PTC describes percutaneous cannulation of the intrahepatic biliary system with fluoroscopic-monitored contrast injection (Figs. 2 and 3). It demonstrates biliary anatomy, including the size, number, and position of stones, much like ERCP. With the advent of cross-sectional and endoscopic imaging modalities, PTC is rarely utilized for the diagnosis of choledocholithiasis. Instead, it is the initial component of percutaneous transhepatic therapies for biliary tract disease, including choledocholithiasis, often when ERCP is not feasible.
Fig. 2.
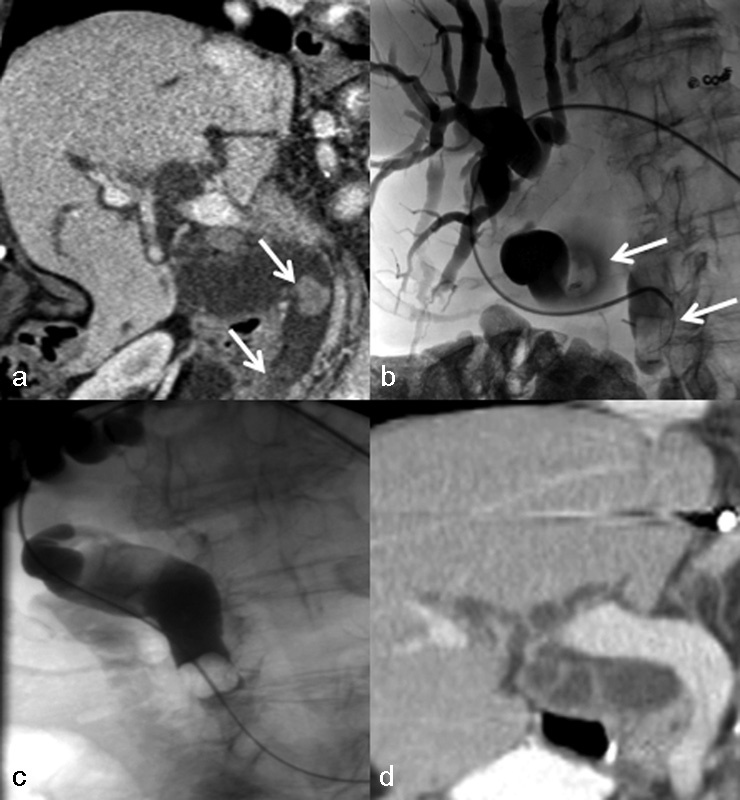
A 91-year-old woman with Roux-en-Y anatomy and choledocholithiasis complicated by acute cholangitis. (a) CT scan with oral and intravenous contrast demonstrates stones in the extrahepatic bile duct (arrows), including subtle distal stone, with marked biliary ductal dilation. (b) Percutaneous placement of curved catheter into the extrahepatic bile duct with limited cholangiogram showing dilated intrahepatic and extrahepatic ducts with filling defects corresponding to CT (arrows). (c) After sphincteroplasty, a Fogarty balloon was used to push stones into the small bowel. (d) Follow-up CT scan with resolution of filling defects and decreased biliary ductal dilation.
Fig. 3.
A 44-year-old woman with Roux-en-Y anatomy, due to bariatric surgery, with symptomatic choledocholithiasis and failed endoscopic retrograde cholangiopancreatography utilizing double-balloon technique. (a) Percutaneous cholangiogram, with sheath tip in the extrahepatic bile duct, shows postoperative changes of cholecystectomy, with mild biliary ductal dilation and stone in the distal common bile duct (arrow). (b) Balloon sphincteroplasty. (c) Fogarty balloon was used to push stone into duodenum. (d) Delayed sheath cholangiogram showing resolution of biliary ductal dilation and choledocholithiasis with an intact percutaneous tract.
Management
The treatment of choledocholithiasis varies locally, according to the skills of the practitioner and availability of equipment. The cornerstone of therapy is removal of the biliary stone together with early recognition and treatment of complications (jaundice, acute pancreatitis, and acute cholangitis). This section will briefly review the surgical and endoscopic means of treatment.
Surgery
Surgical techniques include open, laparoscopic common bile duct exploration (LCBDE) and laparoscopic-assisted transgastric endoscopic retrograde cholangiopancreatography (LA-ERCP). Before the current era of laparoscopic surgery and endoscopic intervention, open CBD exploration, at the time of cholecystectomy, was standard practice. Owing to increased hospital stay and recuperation time, open cholecystectomy is largely replaced by laparoscopic cholecystectomy, with a commensurate decrease in open CBD exploration. LCBDE is safe with a complication rate similar to ERCP.31 32 Single-stage laparoscopic cholecystectomy and LCBDE decrease length of hospital stay, compared with two-stage ERCP and laparoscopic cholecystectomy.33 34 LCBDE is limited by the need for specialized instruments and training. LA-ERCP is a hybrid procedure used to access the biliary tree in patients with Roux-en-Y anatomy. In LA-ERCP, a gastrostomy is preformed in the excluded gastric remnant by placing a laparoscopic trochar. Subsequently, an endoscope is inserted through the trochar into the gastric remnant and an ERCP is performed with standard technique. A 2012 review of LA-ERCP found a papillary cannulation rate of 99%, and a complication rate of 7.2%.35
Endoscopy
Endoscopy is capable of treating 90% of choledocholithiasis.36 37 38 39 40 Endoscopic sphincterotomy (ES) and endoscopic papillary balloon dilation (EPBD), in conjunction with stone extraction, are the primary treatment methods for choledocholithiasis.
ES utilizes electrocautery to sever the deep muscles of the sphincter of Oddi, and the term is often used interchangeably with papillotomy, which refers to severing the superficial sphincter of the duodenal papilla. ES eliminates the primary anatomic barrier to stone passage and aids stone extraction techniques. Cholecystectomy usually follows ES to eliminate the most common source of biliary stones. The short-term complication rate is approximately 5 to 10%, with the most common complications being pancreatitis and bleeding.41 Long-term complications include papillary stenosis, cholangitis, and recurrent choledocholithiasis.42 43 Chronic reflux of bowel contents into the biliary system after ES results in bacterial contamination and low-grade inflammation, which may underpin the aforementioned long-term complications.44
EPBD is an alternative procedure for the removal of biliary stones in which the papilla is dilated without a sphincterotomy. This technique attempts to preserve sphincter function and mitigate complications compared with ES. In a randomized trial, the success rate of EPBD (89%) was similar to ES (91%); however, mechanical lithotripsy (ML) was used in a greater proportion of EPBD procedures.25 EPBD decreases risk of bleeding in the short term, and more importantly, especially for younger patients, decreases long-term complications of ES.25 45 A disputed drawback of EPBD is a higher rate of postprocedure pancreatitis compared with ES.
Stone extraction following ES or EPBD is commonly achieved with balloons and baskets (Fig. 1). These devices are available in a variety of configurations to suit varying stone burden and biliary tree anatomy.
Advanced Endoscopy
Endoscopy treatment may fail, due to difficult anatomy or a difficult stone. Difficult anatomy is divided into difficulty in cannulating the papilla and difficulty in reaching the papilla. As the armamentarium of the endoscopist is shared with the interventional radiologist, these treatment techniques are briefly reviewed.
Difficulty in cannulating the papilla may be due to periampullary masses, duodenal diverticula containing the papilla, choledochocele, or papillary stenosis. In these patients, treatment with a rendezvous percutaneous-endoscopic procedure is an option.46 47 48 49 A rendezvous procedure consists of attaining percutaneous transhepatic biliary access and placing a guidewire through the CBD into the duodenum. The endoscopist uses the guidewire to access and negotiate the difficult anatomy, treating as necessary. The percutaneous biliary access is typically removed at the conclusion of the procedure, abrogating the need for a management of a percutaneous biliary tract.
The difficult to reach papilla is most commonly due to postsurgical Roux-en-Y or Billroth 2 anatomy, though it also includes gastric outlet obstruction and duodenal stenosis. Endoscopic treatment of the difficult to reach papilla utilizes an over the balloon technique. This technique includes double-balloon enteroscopy (DBE), single-balloon enteroscopy (SBE), and spiral balloon enteroscopy (SE). DBE and SBE make use of sequential push–pull technique similar to the motion of an inchworm. SE uses rotational motion, similar to a corkscrew. The success rate of cannulating the papilla in a Roux-en-Y or Billroth 2 reconstruction with DBE is 77 to 100% and 88 to 100%, respectively.50 The reported complication rate of DBE ranges from 0 to 19.5%, with perforation being the most common complication.51 A meta-analysis found SBE to have a procedural success rate of 61.7%.52 SE, the newest technique, was able to cannulate the papilla in 10 of 13 (71%) patients with postsurgical anatomy.53
Treatment methods exist for the difficult stone, which is variously defined as a biliary stone diameter larger than 12 mm, or a stone diameter larger than the diameter of the CBD.54 Lithotripsy is the treatment mainstay for difficult stones.
Lithotripsy, or stone fragmentation, is a broad treatment category, which includes intracorporeal and extracorporeal modalities. The intracorporeal methods are ML, electrohydrostatic lithotripsy (EHL), and laser lithotripsy (LL). ML is a commonly employed technique that utilizes a grasper, or basket, to fracture stones. The success rate for biliary stone clearance is 80 to 90%.55 56 57 EHL and LL are different mechanisms by which a similar shockwave is generated to disintegrate a biliary stone. LL has a built-in-target feedback system, making it theoretically safer. Studies on lithotripsy techniques outside of ML are often heterogeneous in their trial arms, making safety and effectiveness comparison difficult. Small trials have found both EHL and LL to be approximately 90% effective in clearing choledocholithiasis.58 59 Extracorporeal lithotripsy has fallen out of favor, and it is used in problem-solving applications, such as treatment refractory stones, or difficult-to-reach intrahepatic stones.
Interventional Radiology
Percutaneous management of choledocholithiasis was first undertaken in 1962 when Dr. Mondet extracted a retained CBD stone through a T-tube using forceps.60 Dr. Burhenne subsequently amassed a series of 661 patients in which stones were extracted with a Dormia basket and T-tube access with a 95% extraction rate.61 The first cases of transhepatic treatment of choledocholithiasis were reported in 1979 by Dotter et al and Perez et al.62 63 The use of percutaneously delivered chemical agents, to dissolve gallstones, was initially seen as promising, but has been nearly completely abandoned due to ineffectiveness and safety concerns.64 65 Percutaneous treatment of choledocholithiasis is accomplished by stone extraction or stone expulsion into the bowel.
Patient Selection
Indications for percutaneous treatment are prior therapy failure, unfavorable anatomy, and stone burden (discussed previously in section “Advanced Endoscopy”), along with medically frail patients, who are deemed unfit for anesthesia, or the complications of ERCP/surgery. Unlike endoscopy and surgery, interventional radiology therapies are often administered with conscious sedation.
Hepatolithiasis, or bile stones within the intrahepatic biliary tree, is a relative indication for percutaneous treatment, as distal stones are difficult to treat endoscopically.66 Cheon et al retrospectively reviewed patients with hepatolithiasis, undergoing treatment by percutaneous methods (97 patients) and peroral cholangioscopy (49 patients). The complete stone clearance rate was significantly higher in percutaneous methods, compared with peroral methods (63.9% vs. 57.1%, respectively, p = 0.015).67
Few contraindications exist for percutaneous-based biliary procedures. They include an uncorrectable coagulopathy, especially for new transhepatic biliary access; lack of a safe percutaneous window often due to intervening bowel; or large volume ascites, which prevents percutaneous tract maturation.
Access
Percutaneous access to the biliary tree is achieved by a variety of methods—namely, T-tube, cholecystostomy tube, and transcystic, along with transhepatic.46 48 68 The most common route of access has migrated from T-tube (1972–1979) to transhepatic (1998–2013), as operative T-tubes are rarely placed.61 69 Transcystic access is not preferred, as it necessitates negotiating a possibly stone-filled gallbladder, and a tortuous cystic duct, with spiral valves of Heister. With transhepatic access, many authors recommend stone removal in two phases.44 70 71 72 The initial phase is percutaneous biliary drainage, to decompress the biliary tree and allow for tract formation. Stone removal is attempted after tract maturation.
Percutaneous Treatment
Biliary stones are extracted or expelled into the bowel, with the aid of biliary sphincter dilation (sphincteroplasty) and lithotripsy (Figs. 2 and 3). Percutaneous extraction of stones requires a mature large bore tract, whereas antegrade expulsion typically requires a much smaller bore tract. This tract is a T-tube site, or, now more commonly, a transhepatic drain.
Sphincteroplasty
Several retrospective studies describe the safety and efficacy of sphincteroplasty and transpapillary elimination of bile duct stones. Dilation of the papilla usually preserves its function, based on manometric studies, thus preventing chronic reflux of bowel contents into the biliary tree.44 73 Szulman et al reported a large series of 300 patients treated for choledocholithiasis, utilizing primarily T-tube access.74 Papillary dilation was preformed with balloons 1 to 2 mm larger than the largest stone with a maximum balloon diameter of 20 mm, as stones ranged in size from 4 to 18 mm. Calculi were then pushed into the duodenum. Biliary duct stone removal was successful in 96% of patients and more than 80% of cases were completed in a single treatment session. No major complication, including acute pancreatitis, cholangitis, or bleeding, was encountered. The authors attribute the lack of pancreatitis to the lack of pancreatic duct cannulation and lack of stone fragmentation, together with sphincteroplasty preformed over a guidewire, and the use of external biliary drainage at procedure completion.
A prospective study of 212 consecutive patients describes percutaneous expulsion of bile duct stones into the duodenum, after balloon dilation of the papilla.72 Typically, stones were pushed into the small bowel with a Fogarty-type occlusion balloon; a small subset of patients required lithotripsy. Most procedures were performed by transhepatic access. Technical success in clearing the biliary tree of stones was 93%. Excessive size of calculus was the most common cause of failure. Clinical evidence of mild pancreatitis was identified in 1.6% of patients, which is less than expected rates with ERCP. Approximately 4% of cases were complicated by major hemorrhage, with several patients requiring transcatheter embolization.
The authors conclude that percutaneous antegrade elimination of stones in the biliary tree, with dilation of the papilla, is an effective and safe technique, which maintains the integrity of the sphincter.
Ozcan et al reported the effectiveness of percutaneous bile duct stone removal utilizing a transhepatic approach in 261 symptomatic patients, who had failed or refused endoscopy.75 Complete clearance of bile duct stones was considered a technical success, while reduction of symptoms was regarded as a medical success. Balloon sphincterotomy, matching the largest stone diameter, was preformed with balloons ranging in size from 8 to 20 mm. Stones larger than 15 mm were treated with ML. All stones or fragments were pushed into the duodenum, with an over-the-wire Fogarty balloon. At procedure completion, an external biliary drainage catheter was placed for decompression and delayed cholangiogram assessment of residual stones. Overall technical success was 95.7%; yet it dropped to 61.5% in patients with hepatolithiasis. Overall medical success was 96.9%. Stone clearance was achieved in one session in approximately 95% of cases. Major complication rate was 6.8%, most commonly due to cholangitis, without mention of pancreatitis.
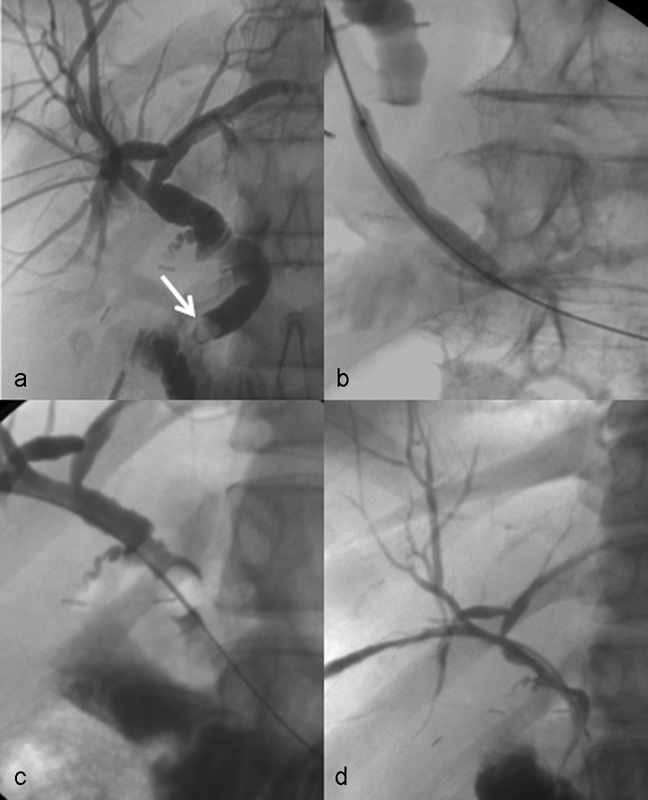
Cholangioscopy
Cholangioscopy is the insertion of a small fiber optic endoscope to allow direct visualization of the biliary tree for diagnostic and therapeutic indications. Advantages over fluoroscopic guidance include lack of ionizing radiation exposure and discrimination of noncalculous filling defects, such as blood clots. Technical advancements in the form of decreased scope diameter are associated with expanded indications and decreased complications.70 With the aid of direct visualization, the interventional radiologist can employ the same techniques available to the endoscopist, including EHL and LL.76 77 78 79
Hwang et al reported a large series of 645 patients treated with percutaneous choledochoscopic stone removal utilizing a T-tube in the majority of cases.80 Transhepatic access was preferred in patients with oriental cholangiohepatitis. Large stones were fragmented with Dormia baskets and EHL, and then extracted through the percutaneous tract. Successful stone extraction rates for both the T-tube and transhepatic routes were high at 96 and 97%, respectively. Intrahepatic stones were more challenging to remove, compared with extrahepatic disease, and often required multiple treatment sessions. Minor complications such as transient hemobilia, fever, and pain were seen in 3 to 5% of cases and managed conservatively. Arterial hemorrhage requiring embolization occurred in 1.9% of the transhepatic cases during tract dilation.
Burton et al described a 71-patient series utilizing EHL for the treatment of biliary stones by a predominate percutaneous approach.79 A mature tract was required for the placement of an 18F working sheath. EHL stone fragmentation was guided by direct choledochoscopy and stone fragments were removed via the sheath. Number of stones, and stone size, varied from 200 stones to a 40-mm size stone. A single treatment session was sufficient in most patients. EHL successfully fragmented stones in 97% of cases and all major stone fragments were removed in 94% of cases. All major complications (7%) were related to the initial biliary drainage, or tract dilation, rather than the EHL component. The authors concluded that intracorporeal EHL is a safe and effective procedure that improves the success of percutaneous and endoscopic biliary stone removal. They also note several advantages of EHL, compared with other forms of intracorporeal lithotripsy—inexpensive equipment cost, availability as it is routinely used in urologic stone removal, and its safety profile.
LL for complicated intra- or extrahepatic bile duct stones was evaluated in a 22-patient cohort. Patients had failed ERCP, or were not candidates for ERCP. A transhepatic approach, with placement of a 9F vascular sheath into the biliary system, allowed for ureteroscope and holmium laser fiber placement. Biliary stones were fragment with direct visualization and adjunct fluoroscopy. Fragmented stones were flushed through the papilla into the duodenum. An internal–external biliary catheter was left at the procedure completion. After a delayed cholangiogram, demonstrating no residual stones, transhepatic access was removed. In nearly 95% of cases, all stones were fragmented and flushed into the small bowel, with approximately 80% of cases completed in one treatment session. No tract complications were encountered, likely due to the relatively small working sheath size.
Cholangioscopy yields improved success rates for treatment of intrahepatic stones. A study of 165 patients with intrahepatic stones were treated by percutaneous transhepatic cholangioscopy and lithotripsy with 5-year follow-up.81 Complete stone removal was achieved in 80% of cases, representing an improvement over the aforementioned 61.5% clearance rate, under fluoroscopic guidance. Recurrent intrahepatic stones were detected in 32.6% of patients with a mean 58-month follow-up.
Complications
Complications of percutaneous biliary stone procedures have decreased with experience. In 1989, Stokes et al reported a major complication rate of 17% with 4% mortality rate utilizing a transhepatic approach.82 Similarly in 1991, Bonnel et al reported a major complication rate of 22% with 8% mortality rate.83 In 2007, Oh et al analyzed complications of transhepatic cholangioscopy.84 The overall major complication rate had improved to 8.2% with no deaths. Modern sphincteroplasty series identify a 5% morbidity rate, including a small risk of pancreatitis, and a mortality rate of 1.4%.44 72 Although ERCP is most commonly utilized to manage choledocholithiasis, it carries an overall complication rate of 8 to 12%, with a major complication rate similar to percutaneous therapy.25 26 Recurrence of choledocholithiasis varies upon etiology, with high recurrence rates expected in hepatolithiasis (22–50%).3
Conclusion
Choledocholithiasis is the presence of stones in the CBD, typically from a gallbladder origin. The diagnosis of choledocholithiasis is confirmed with advanced imaging techniques, including MRCP and ERCP. Endoscopy has replaced surgery as the cornerstone of therapy, as it is successful in treating most patients. Difficult stone burden and difficult biliary anatomy (postoperative) require advanced surgical, endoscopic, and percutaneous techniques to extract or expel biliary stones. Percutaneous treatment of choledocholithiasis, including the use of cholangioscopy, is safe and effective, often with the preservation of the biliary sphincter, which reduces long-term complications.
References
- 1.Williams E J Green J Beckingham I Parks R Martin D Lombard M; British Society of Gastroenterology. Guidelines on the management of common bile duct stones (CBDS) Gut 20085771004–1021. [DOI] [PubMed] [Google Scholar]
- 2.Gurusamy K S, Giljaca V, Takwoingi Y. et al. Ultrasound versus liver function tests for diagnosis of common bile duct stones. Cochrane Database Syst Rev. 2015;2(2):CD011548. doi: 10.1002/14651858.CD011548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.European Association for the Study of the Liver (EASL). Electronic address: easloffice@easloffice.eu . EASL Clinical Practice Guidelines on the prevention, diagnosis and treatment of gallstones. J Hepatol. 2016;65(1):146–181. doi: 10.1016/j.jhep.2016.03.005. [DOI] [PubMed] [Google Scholar]
- 4.Yadav D, Agarwal N, Pitchumoni C S. A critical evaluation of laboratory tests in acute pancreatitis. Am J Gastroenterol. 2002;97(6):1309–1318. doi: 10.1111/j.1572-0241.2002.05766.x. [DOI] [PubMed] [Google Scholar]
- 5.Qiao T, Ma R H, Luo X B, Yang L Q, Luo Z L, Zheng P M. The systematic classification of gallbladder stones. PLoS ONE. 2013;8(10):e74887. doi: 10.1371/journal.pone.0074887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Portincasa P, Moschetta A, Palasciano G. Cholesterol gallstone disease. Lancet. 2006;368(9531):230–239. doi: 10.1016/S0140-6736(06)69044-2. [DOI] [PubMed] [Google Scholar]
- 7.Brink M A, Slors J F, Keulemans Y C. et al. Enterohepatic cycling of bilirubin: a putative mechanism for pigment gallstone formation in ileal Crohn's disease. Gastroenterology. 1999;116(6):1420–1427. doi: 10.1016/s0016-5085(99)70507-x. [DOI] [PubMed] [Google Scholar]
- 8.Flass T, Narkewicz M R. Cirrhosis and other liver disease in cystic fibrosis. J Cyst Fibros. 2013;12(2):116–124. doi: 10.1016/j.jcf.2012.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vítek L, Carey M C. New pathophysiological concepts underlying pathogenesis of pigment gallstones. Clin Res Hepatol Gastroenterol. 2012;36(2):122–129. doi: 10.1016/j.clinre.2011.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stinton L M Myers R P Shaffer E A Epidemiology of gallstones Gastroenterol Clin North Am 2010392157–169., vii [DOI] [PubMed] [Google Scholar]
- 11.Kaufman H S Magnuson T H Lillemoe K D Frasca P Pitt H A The role of bacteria in gallbladder and common duct stone formation Ann Surg 19892095584–591., discussion 591–592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Einstein D M, Lapin S A, Ralls P W, Halls J M. The insensitivity of sonography in the detection of choledocholithiasis. AJR Am J Roentgenol. 1984;142(4):725–728. doi: 10.2214/ajr.142.4.725. [DOI] [PubMed] [Google Scholar]
- 13.Cronan J J. US diagnosis of choledocholithiasis: a reappraisal. Radiology. 1986;161(1):133–134. doi: 10.1148/radiology.161.1.3532178. [DOI] [PubMed] [Google Scholar]
- 14.Maple J T, Ben-Menachem T, Anderson M A. et al. The role of endoscopy in the evaluation of suspected choledocholithiasis. Gastrointest Endosc. 2010;71(1):1–9. doi: 10.1016/j.gie.2009.09.041. [DOI] [PubMed] [Google Scholar]
- 15.Hunt D R. Common bile duct stones in non-dilated bile ducts? An ultrasound study. Australas Radiol. 1996;40(3):221–222. doi: 10.1111/j.1440-1673.1996.tb00389.x. [DOI] [PubMed] [Google Scholar]
- 16.Gibson R N, Vincent J M, Speer T, Collier N A, Noack K. Accuracy of computed tomographic intravenous cholangiography (CT-IVC) with iotroxate in the detection of choledocholithiasis. Eur Radiol. 2005;15(8):1634–1642. doi: 10.1007/s00330-004-2606-8. [DOI] [PubMed] [Google Scholar]
- 17.Cabada Giadás T, Sarría Octavio de Toledo L, Martínez-Berganza Asensio M T. et al. Helical CT cholangiography in the evaluation of the biliary tract: application to the diagnosis of choledocholithiasis. Abdom Imaging. 2002;27(1):61–70. doi: 10.1007/s00261-001-0043-6. [DOI] [PubMed] [Google Scholar]
- 18.Vitellas K M Keogan M T Spritzer C E Nelson R C MR cholangiopancreatography of bile and pancreatic duct abnormalities with emphasis on the single-shot fast spin-echo technique Radiographics 2000204939–957., quiz 1107–1108, 1112 [DOI] [PubMed] [Google Scholar]
- 19.Baron R L, Tublin M E, Peterson M S. Imaging the spectrum of biliary tract disease. Radiol Clin North Am. 2002;40(6):1325–1354. doi: 10.1016/s0033-8389(02)00045-3. [DOI] [PubMed] [Google Scholar]
- 20.Choi I Y, Yeom S K, Cha S H. et al. Diagnosis of biliary stone disease: T1-weighted magnetic resonance cholangiography with Gd-EOB-DTPA versus T2-weighted magnetic resonance cholangiography. Clin Imaging. 2014;38(2):164–169. doi: 10.1016/j.clinimag.2013.11.001. [DOI] [PubMed] [Google Scholar]
- 21.Sugiyama M, Atomi Y, Hachiya J. Magnetic resonance cholangiography using half-Fourier acquisition for diagnosing choledocholithiasis. Am J Gastroenterol. 1998;93(10):1886–1890. doi: 10.1111/j.1572-0241.1998.00543.x. [DOI] [PubMed] [Google Scholar]
- 22.Giljaca V, Gurusamy K S, Takwoingi Y. et al. Endoscopic ultrasound versus magnetic resonance cholangiopancreatography for common bile duct stones. Cochrane Database Syst Rev. 2015;2(2):CD011549. doi: 10.1002/14651858.CD011549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Verma D, Kapadia A, Eisen G M, Adler D G. EUS vs MRCP for detection of choledocholithiasis. Gastrointest Endosc. 2006;64(2):248–254. doi: 10.1016/j.gie.2005.12.038. [DOI] [PubMed] [Google Scholar]
- 24.Williams E J, Taylor S, Fairclough P. et al. Risk factors for complication following ERCP; results of a large-scale, prospective multicenter study. Endoscopy. 2007;39(9):793–801. doi: 10.1055/s-2007-966723. [DOI] [PubMed] [Google Scholar]
- 25.Bergman J J, Rauws E A, Fockens P. et al. Randomised trial of endoscopic balloon dilation versus endoscopic sphincterotomy for removal of bile duct stones. Lancet. 1997;349(9059):1124–1129. doi: 10.1016/S0140-6736(96)11026-6. [DOI] [PubMed] [Google Scholar]
- 26.Freeman M L, Nelson D B, Sherman S. et al. Complications of endoscopic biliary sphincterotomy. N Engl J Med. 1996;335(13):909–918. doi: 10.1056/NEJM199609263351301. [DOI] [PubMed] [Google Scholar]
- 27.Massarweh N N, Devlin A, Elrod J A, Symons R G, Flum D R. Surgeon knowledge, behavior, and opinions regarding intraoperative cholangiography. J Am Coll Surg. 2008;207(6):821–830. doi: 10.1016/j.jamcollsurg.2008.08.011. [DOI] [PubMed] [Google Scholar]
- 28.Gurusamy K S, Giljaca V, Takwoingi Y. et al. Endoscopic retrograde cholangiopancreatography versus intraoperative cholangiography for diagnosis of common bile duct stones. Cochrane Database Syst Rev. 2015;2(2):CD010339. doi: 10.1002/14651858.CD010339.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Machi J, Tateishi T, Oishi A J. et al. Laparoscopic ultrasonography versus operative cholangiography during laparoscopic cholecystectomy: review of the literature and a comparison with open intraoperative ultrasonography. J Am Coll Surg. 1999;188(4):360–367. doi: 10.1016/s1072-7515(98)00313-5. [DOI] [PubMed] [Google Scholar]
- 30.Machi J, Johnson J O, Deziel D J. et al. The routine use of laparoscopic ultrasound decreases bile duct injury: a multicenter study. Surg Endosc. 2009;23(2):384–388. doi: 10.1007/s00464-008-9985-x. [DOI] [PubMed] [Google Scholar]
- 31.Tranter S E, Thompson M H. Comparison of endoscopic sphincterotomy and laparoscopic exploration of the common bile duct. Br J Surg. 2002;89(12):1495–1504. doi: 10.1046/j.1365-2168.2002.02291.x. [DOI] [PubMed] [Google Scholar]
- 32.Martin D J, Vernon D R, Toouli J. Surgical versus endoscopic treatment of bile duct stones. Cochrane Database Syst Rev. 2006;2(2):CD003327. doi: 10.1002/14651858.CD003327.pub2. [DOI] [PubMed] [Google Scholar]
- 33.Cuschieri A, Lezoche E, Morino M. et al. E.A.E.S. multicenter prospective randomized trial comparing two-stage vs single-stage management of patients with gallstone disease and ductal calculi. Surg Endosc. 1999;13(10):952–957. doi: 10.1007/s004649901145. [DOI] [PubMed] [Google Scholar]
- 34.Rhodes M, Sussman L, Cohen L, Lewis M P. Randomised trial of laparoscopic exploration of common bile duct versus postoperative endoscopic retrograde cholangiography for common bile duct stones. Lancet. 1998;351(9097):159–161. doi: 10.1016/s0140-6736(97)09175-7. [DOI] [PubMed] [Google Scholar]
- 35.Richardson J F, Lee J G, Smith B R, Nguyen B, Pham K P, Nguyen N T. Laparoscopic transgastric endoscopy after Roux-en-Y gastric bypass: case series and review of the literature. Am Surg. 2012;78(10):1182–1186. [PubMed] [Google Scholar]
- 36.Arregui M E, Davis C J, Arkush A M, Nagan R F. Laparoscopic cholecystectomy combined with endoscopic sphincterotomy and stone extraction or laparoscopic choledochoscopy and electrohydraulic lithotripsy for management of cholelithiasis with choledocholithiasis. Surg Endosc. 1992;6(1):10–15. doi: 10.1007/BF00591180. [DOI] [PubMed] [Google Scholar]
- 37.Koo K P, Traverso L W. Do preoperative indicators predict the presence of common bile duct stones during laparoscopic cholecystectomy? Am J Surg. 1996;171(5):495–499. doi: 10.1016/s0002-9610(97)89611-0. [DOI] [PubMed] [Google Scholar]
- 38.Perissat J, Huibregtse K, Keane F B, Russell R C, Neoptolemos J P. Management of bile duct stones in the era of laparoscopic cholecystectomy. Br J Surg. 1994;81(6):799–810. doi: 10.1002/bjs.1800810606. [DOI] [PubMed] [Google Scholar]
- 39.Geron N, Reshef R, Shiller M, Kniaz D, Eitan A. The role of endoscopic retrograde cholangiopancreatography in the laparoscopic era. Surg Endosc. 1999;13(5):452–456. doi: 10.1007/pl00022936. [DOI] [PubMed] [Google Scholar]
- 40.Tham T C, Lichtenstein D R, Vandervoort J. et al. Role of endoscopic retrograde cholangiopancreatography for suspected choledocholithiasis in patients undergoing laparoscopic cholecystectomy. Gastrointest Endosc. 1998;47(1):50–56. doi: 10.1016/s0016-5107(98)70298-6. [DOI] [PubMed] [Google Scholar]
- 41.Freeman M L. Complications of endoscopic retrograde cholangiopancreatography: avoidance and management. Gastrointest Endosc Clin N Am. 2012;22(3):567–586. doi: 10.1016/j.giec.2012.05.001. [DOI] [PubMed] [Google Scholar]
- 42.Wojtun S, Gil J, Gietka W, Gil M. Endoscopic sphincterotomy for choledocholithiasis: a prospective single-center study on the short-term and long-term treatment results in 483 patients. Endoscopy. 1997;29(4):258–265. doi: 10.1055/s-2007-1004186. [DOI] [PubMed] [Google Scholar]
- 43.Hawes R H, Cotton P B, Vallon A G. Follow-up 6 to 11 years after duodenoscopic sphincterotomy for stones in patients with prior cholecystectomy. Gastroenterology. 1990;98(4):1008–1012. doi: 10.1016/0016-5085(90)90026-w. [DOI] [PubMed] [Google Scholar]
- 44.García-Vila J H, Redondo-Ibáñez M, Díaz-Ramón C. Balloon sphincteroplasty and transpapillary elimination of bile duct stones: 10 years' experience. AJR Am J Roentgenol. 2004;182(6):1451–1458. doi: 10.2214/ajr.182.6.1821451. [DOI] [PubMed] [Google Scholar]
- 45.Doi S, Yasuda I, Mukai T. et al. Comparison of long-term outcomes after endoscopic sphincterotomy versus endoscopic papillary balloon dilation: a propensity score-based cohort analysis. J Gastroenterol. 2013;48(9):1090–1096. doi: 10.1007/s00535-012-0707-8. [DOI] [PubMed] [Google Scholar]
- 46.Okuno M, Iwashita T, Yasuda I. et al. Percutaneous transgallbladder rendezvous for enteroscopic management of choledocholithiasis in patients with surgically altered anatomy. Scand J Gastroenterol. 2013;48(8):974–978. doi: 10.3109/00365521.2013.805812. [DOI] [PubMed] [Google Scholar]
- 47.Patel M, Levitin A, Chahal P. Hybrid percutaneous-endoscopic drainage of cholelithiasis and choledocholithiasis. Gastrointest Endosc. 2015;81(4):1013–1014. doi: 10.1016/j.gie.2014.10.034. [DOI] [PubMed] [Google Scholar]
- 48.Banerjee B, Harshfield D L, Teplick S K. Percutaneous transcholecystic approach to the rendezvous procedure when transhepatic access fails. J Vasc Interv Radiol. 1994;5(6):895–898. doi: 10.1016/s1051-0443(94)71633-x. [DOI] [PubMed] [Google Scholar]
- 49.Matsubayashi H, Maeda A, Fukutomi A, Ono H. A case of choledocholithiasis treated by parallel cannulation along with PTGBD rendezvous. Can J Gastroenterol. 2009;2(1):36–38. doi: 10.1007/s12328-008-0036-x. [DOI] [PubMed] [Google Scholar]
- 50.Kato H, Tsutsumi K, Harada R, Okada H, Yamamoto K. Short double-balloon enteroscopy is feasible and effective for endoscopic retrograde cholangiopancreatography in patients with surgically altered gastrointestinal anatomy. Dig Endosc. 2014;26 02:130–135. doi: 10.1111/den.12251. [DOI] [PubMed] [Google Scholar]
- 51.Moreels T G. Altered anatomy: enteroscopy and ERCP procedure. Best Pract Res Clin Gastroenterol. 2012;26(3):347–357. doi: 10.1016/j.bpg.2012.03.003. [DOI] [PubMed] [Google Scholar]
- 52.Inamdar S, Slattery E, Sejpal D V. et al. Systematic review and meta-analysis of single-balloon enteroscopy-assisted ERCP in patients with surgically altered GI anatomy. Gastrointest Endosc. 2015;82(1):9–19. doi: 10.1016/j.gie.2015.02.013. [DOI] [PubMed] [Google Scholar]
- 53.Wagh M S, Draganov P V. Prospective evaluation of spiral overtube-assisted ERCP in patients with surgically altered anatomy. Gastrointest Endosc. 2012;76(2):439–443. doi: 10.1016/j.gie.2012.04.444. [DOI] [PubMed] [Google Scholar]
- 54.Stefanidis G, Christodoulou C, Manolakopoulos S, Chuttani R. Endoscopic extraction of large common bile duct stones: a review article. World J Gastrointest Endosc. 2012;4(5):167–179. doi: 10.4253/wjge.v4.i5.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sorbi D, Van Os E C, Aberger F J. et al. Clinical application of a new disposable lithotripter: a prospective multicenter study. Gastrointest Endosc. 1999;49(2):210–213. doi: 10.1016/s0016-5107(99)70488-8. [DOI] [PubMed] [Google Scholar]
- 56.Cipolletta L, Costamagna G, Bianco M A. et al. Endoscopic mechanical lithotripsy of difficult common bile duct stones. Br J Surg. 1997;84(10):1407–1409. [PubMed] [Google Scholar]
- 57.Chang W H, Chu C H, Wang T E, Chen M J, Lin C C. Outcome of simple use of mechanical lithotripsy of difficult common bile duct stones. World J Gastroenterol. 2005;11(4):593–596. doi: 10.3748/wjg.v11.i4.593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Arya N, Nelles S E, Haber G B, Kim Y I, Kortan P K. Electrohydraulic lithotripsy in 111 patients: a safe and effective therapy for difficult bile duct stones. Am J Gastroenterol. 2004;99(12):2330–2334. doi: 10.1111/j.1572-0241.2004.40251.x. [DOI] [PubMed] [Google Scholar]
- 59.Hochberger J, Bayer J, May A. et al. Laser lithotripsy of difficult bile duct stones: results in 60 patients using a rhodamine 6G dye laser with optical stone tissue detection system. Gut. 1998;43(6):823–829. doi: 10.1136/gut.43.6.823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Mondet A F. Technic of blood extraction of calculi in residual lithasis of the choledochus [in Spanish] Bol Trab Soc Cir B Aires. 1962;46:278–290. [PubMed] [Google Scholar]
- 61.Burhenne H J. Garland lecture. Percutaneous extraction of retained biliary tract stones: 661 patients. AJR Am J Roentgenol. 1980;134(5):889–898. doi: 10.2214/ajr.134.5.889. [DOI] [PubMed] [Google Scholar]
- 62.Dotter C T, Bilbao M K, Katon R M. Percutaneous transhepatic gallstone removal by needle tract. Radiology. 1979;133(1):242–243. doi: 10.1148/133.1.242. [DOI] [PubMed] [Google Scholar]
- 63.Perez M R, Oleaga J A, Freiman D B, McLean G L, Ring E J. Removal of a distal common bile duct stone through percutaneous transhepatic catheterization. Arch Surg. 1979;114(1):107–109. doi: 10.1001/archsurg.1979.01370250109024. [DOI] [PubMed] [Google Scholar]
- 64.Thistle J L, May G R, Bender C E. et al. Dissolution of cholesterol gallbladder stones by methyl tert-butyl ether administered by percutaneous transhepatic catheter. N Engl J Med. 1989;320(10):633–639. doi: 10.1056/NEJM198903093201004. [DOI] [PubMed] [Google Scholar]
- 65.Kim G, Malayaman S N, Green M S. Use of methyl tert-butyl ether for the treatment of refractory intrahepatic biliary strictures and bile casts: a modern perspective. Case Rep Surg. 2015;2015:408175. doi: 10.1155/2015/408175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Yasuda H, Takada T, Kawarada Y. et al. Unusual cases of acute cholecystitis and cholangitis: Tokyo Guidelines. J Hepatobiliary Pancreat Surg. 2007;14(1):98–113. doi: 10.1007/s00534-006-1162-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Cheon Y K, Cho Y D, Moon J H, Lee J S, Shim C S. Evaluation of long-term results and recurrent factors after operative and nonoperative treatment for hepatolithiasis. Surgery. 2009;146(5):843–853. doi: 10.1016/j.surg.2009.04.009. [DOI] [PubMed] [Google Scholar]
- 68.Atar E, Neiman C, Ram E, Almog M, Gadiel I, Belenky A. Percutaneous trans-papillary elimination of common bile duct stones using an existing gallbladder drain for access. Isr Med Assoc J. 2012;14(6):354–358. [PubMed] [Google Scholar]
- 69.Kint J F, van den Bergh J E, van Gelder R E. et al. Percutaneous treatment of common bile duct stones: results and complications in 110 consecutive patients. Dig Surg. 2015;32(1):9–15. doi: 10.1159/000370129. [DOI] [PubMed] [Google Scholar]
- 70.Cannavale A, Bezzi M, Cereatti F. et al. Combined radiological-endoscopic management of difficult bile duct stones: 18-year single center experience. Therap Adv Gastroenterol. 2015;8(6):340–351. doi: 10.1177/1756283X15587483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Nagashima I, Takada T, Shiratori M, Inaba T, Okinaga K. Percutaneous transhepatic papillary balloon dilation as a therapeutic option for choledocholithiasis. J Hepatobiliary Pancreat Surg. 2004;11(4):252–254. doi: 10.1007/s00534-003-0851-x. [DOI] [PubMed] [Google Scholar]
- 72.García-García L, Lanciego C. Percutaneous treatment of biliary stones: sphincteroplasty and occlusion balloon for the clearance of bile duct calculi. AJR Am J Roentgenol. 2004;182(3):663–670. doi: 10.2214/ajr.182.3.1820663. [DOI] [PubMed] [Google Scholar]
- 73.Minami A, Nakatsu T, Uchida N. et al. Papillary dilation vs sphincterotomy in endoscopic removal of bile duct stones. A randomized trial with manometric function. Dig Dis Sci. 1995;40(12):2550–2554. doi: 10.1007/BF02220440. [DOI] [PubMed] [Google Scholar]
- 74.Szulman C, Giménez M, Sierre S. Antegrade papillary balloon dilation for extrahepatic bile duct stone clearance: lessons learned from treating 300 patients. J Vasc Interv Radiol. 2011;22(3):346–353. doi: 10.1016/j.jvir.2010.11.015. [DOI] [PubMed] [Google Scholar]
- 75.Ozcan N, Kahriman G, Mavili E. Percutaneous transhepatic removal of bile duct stones: results of 261 patients. Cardiovasc Intervent Radiol. 2012;35(3):621–627. doi: 10.1007/s00270-011-0190-2. [DOI] [PubMed] [Google Scholar]
- 76.Ray A A, Davies E T, Duvdevani M, Razvi H, Denstedt J D. The management of treatment-resistant biliary calculi using percutaneous endourologic techniques. Can J Surg. 2009;52(5):407–412. [PMC free article] [PubMed] [Google Scholar]
- 77.Cheung M T, Wai S H, Kwok P C. Percutaneous transhepatic choledochoscopic removal of intrahepatic stones. Br J Surg. 2003;90(11):1409–1415. doi: 10.1002/bjs.4327. [DOI] [PubMed] [Google Scholar]
- 78.Sullivan K L, Bagley D H Jr, Gordon S J. et al. Transhepatic laser lithotripsy of choledocholithiasis: initial clinical experience. J Vasc Interv Radiol. 1991;2(3):387–391. doi: 10.1016/s1051-0443(91)72268-9. [DOI] [PubMed] [Google Scholar]
- 79.Burton K E, Picus D, Hicks M E. et al. Fragmentation of biliary calculi in 71 patients by use of intracorporeal electrohydraulic lithotripsy. J Vasc Interv Radiol. 1993;4(2):251–256. doi: 10.1016/s1051-0443(93)71846-1. [DOI] [PubMed] [Google Scholar]
- 80.Hwang M H, Tsai C C, Mo L R. et al. Percutaneous choledochoscopic biliary tract stone removal: experience in 645 consecutive patients. Eur J Radiol. 1993;17(3):184–190. doi: 10.1016/0720-048x(93)90101-r. [DOI] [PubMed] [Google Scholar]
- 81.Yeh Y H, Huang M H, Yang J C, Mo L R, Lin J, Yueh S K. Percutaneous trans-hepatic cholangioscopy and lithotripsy in the treatment of intrahepatic stones: a study with 5 year follow-up. Gastrointest Endosc. 1995;42(1):13–18. doi: 10.1016/s0016-5107(95)70236-9. [DOI] [PubMed] [Google Scholar]
- 82.Stokes K R Falchuk K R Clouse M E Biliary duct stones: update on 54 cases after percutaneous transhepatic removal Radiology 1989170(3, Pt 2):999–1001. [DOI] [PubMed] [Google Scholar]
- 83.Bonnel D H, Liguory C E, Cornud F E, Lefebvre J F. Common bile duct and intrahepatic stones: results of transhepatic electrohydraulic lithotripsy in 50 patients. Radiology. 1991;180(2):345–348. doi: 10.1148/radiology.180.2.2068295. [DOI] [PubMed] [Google Scholar]
- 84.Oh H C, Lee S K, Lee T Y. et al. Analysis of percutaneous transhepatic cholangioscopy-related complications and the risk factors for those complications. Endoscopy. 2007;39:731–736. doi: 10.1055/s-2007-966577. [DOI] [PubMed] [Google Scholar]


