Abstract
[Purpose] The aim of the present study was to compare the effect of pre-operative and post-operative physical therapy versus post-operative physical therapy alone on pain and recovery of function after total knee arthroplasty. [Subjects and Methods] Fifty patients (18 males and 32 females) ranging in age from 48 to 80 years (mean 63.28, SD 9.44) participated in a 6-week two-arm randomized rater-blinded trial. One group received pre- and post-operative physical therapy whereas the other group received only post-operative physical therapy. Pain and function were measured with a visual analogue scale and a lower extremity functional scale at baseline (pre-operative) as well as week 3 and week 6 post-operative. [Results] The differences in pain intensity and functional score at week 3 and week 6 post-operative remained statistically insignificant between the two groups. [Conclusion] The reduction of pain and recovery of function was similar in subjects who received pre- and post-operative physical therapy and those who received only post-operative physical therapy after total knee arthroplasty. Additional pre-operative physical therapy did not bring about any further improvement in pain intensity or recovery of function after total knee arthroplasty.
Key words: Total knee arthroplasty, Physical therapy, Pain
INTRODUCTION
Total joint replacement surgeries are increasing worldwide. In the year 2012, more than 84,000 primary total knee arthroplasty (TKA) procedures were performed in the UK, according to data from the National Joint Registry data1). Patients awaiting knee replacement surgery commonly experience difficulty maintaining balance and functional status; these problems further increase as the waiting time for surgery lengthens2).
Post-operative (post-op) physical therapy (PT) after TKA has been identified as an important factor for successful patient outcome. Exercises are widely recommended after TKA to improve walking and activities of daily living3). These include numerous interventions such as exercise, manual techniques, knee taping, electrotherapeutic modalities, and education to implement patient self-management strategies4,5,6). However, the evidence of the effects of pre-operative (pre-op) PT in this population is limited2). Two previous systematic reviews have reported low to moderate quality evidence that pre-op supervised PT reduces pain in patients with hip and knee osteoarthritis prior to joint replacement1, 7) while, in contrast, another study did not find a significant impact of pre-op PT plus education on range of motion, muscle strength or post-op disability8). In addition, Dauty et al. reported no benefit of pre-op and post-op PT in patients undergoing TKA9). Furthermore, in a systematic review, Silkman Baker and McKeon10) did not report positive effects of pre-op rehabilitation compared to other interventions in individuals undergoing TKA.
There are very few studies that address this topic; to the best of our knowledge, no study has compared the effect of pre- and post-op PT versus post-op PT alone after TKA especially on pain and functional recovery. Hence, we compared the effect of pre-op and post-op PT versus only post-op PT on pain and recovery of function after TKA.
SUBJECTS AND METHODS
A prospective randomized rater-blinded trial with assessments at baseline, week 3 and week 6 post-op was used to compare the effect of pre-op and post-op PT (pre-post PT) and post-op PT alone on pain and recovery of function after TKA (Fig. 1). All the participants gave written informed consent approved by the Institutional Ethical Committee (IEC). All the procedures followed the Declaration of Helsinki.
Fig. 1.
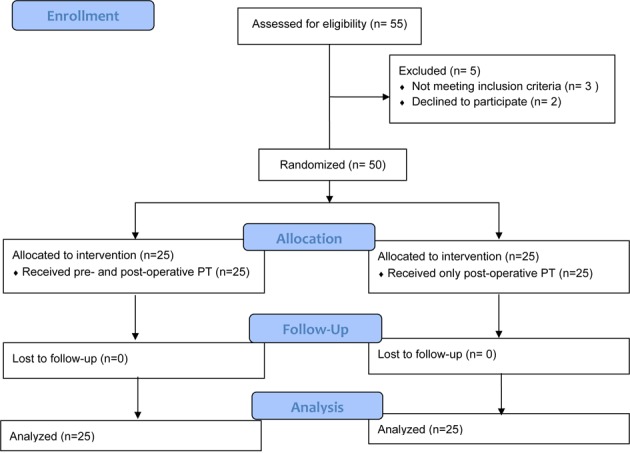
Flow diagram of prospective randomized rater-blinded trial comparing pre- and post-operative PT and Post-operative PT only. PT: physical therapy
Fifty consecutive patients who underwent TKA at Primus Super Specialty Hospital, New Delhi, India, participated in this study. They were randomly divided through the chit box method into two groups (25 subjects in each group)11). One group received pre-post PT whereas the other group received only post PT. The inclusion criterion was a pre-operative diagnosis of primary knee osteoarthritis (OA) by the orthopedic surgeon based on the American College of Rheumatology (ACR) criteria12). Patients were excluded if they had a history of rheumatoid arthritis, cognitive impairment, or ankylosing spondylitis.
Pain and physical functioning were assessed by using the visual analogue scale (VAS) and the lower extremity functional scale (LEFS), respectively. The VAS is a valid and reliable measure of chronic pain intensity13,14,15,16). The LEFS is a 20-item questionnaire designed to measure activity limitation of lower extremities and has an established validity for measuring the lower extremity function in a population of patients with orthopedic problems17,18,19). Each item of the LEFS is scored on a Likert 5-point scale ranging from 0 to 4. LEFS scores range from 0 to 80 points, with higher scores indicating a higher functional level19). The LEFS appears to recognize changes similar or superior to those recognized by the WOMAC physical function subscale in patients undergoing knee or hip arthroplasty20).
A standard parapatellar surgical approach was used. The average length of hospital stay was 5 days. All the participants were given oral analgesics to control pain. While admitted to the hospital before TKA, all the patients in the pre-post PT group received daily PT sessions of approximately 30 minutes duration. It included strengthening and mobility exercises, proper techniques of transfers, and gait training with assistive devices (stick or walker). The participants were instructed to repeat these exercises 2–3 times a day. Similar exercises were given to the post-op PT group after surgery. After discharge from the hospital, the patients received 12 sessions of PT, twice a week for 6 weeks, comprised mainly strengthening and mobility exercises as well as gait training. In addition, all the patients received 20 minutes of conventional transcutaneous electrical nerve stimulation (TENS) to minimize pain. All the patients were instructed to repeat these exercises at home. In the present study, the component of exercise protocol was based on a previously published study3).
Data analysis was done by using IBM SPSS Statistics 21 (Statistical package for the
Social Sciences, IBM, Inc. Chicago, IL, USA). Repeated measure analysis of variance (ANOVA) with Bonferroni adjustments for multiple comparisons was used to study the changes in dependent variables over time. Univariate ANOVA was used to compare the dependent variables at each level between the two groups. Descriptive data was presented as means and standard deviations (SD). A p value of<0.05 was considered to be statistically significant.
RESULTS
Fifty patients (18 males and 32 females) who underwent TKA agreed to participate in the study. The differences in age and weight of two groups were found to be statistically insignificant (average age 63.53 vs. 66.55 years; average weight 90.83 vs. 93.75 kg.; p>0.05). Tables 1 and 2 indicate intra-group comparison of the results. Both groups showed statistically significant reduction in pain intensity and improved functional score at the end of the study (p<0.05). Mean reduction of pain intensity in the pre-post PT group was 7; in the post-op PT group, it was 6.3. Mean improvement of functional score in the pre-post PT group was 37; in the post-op PT group, it was 42.4. Post hoc analysis revealed significant reduction of pain intensity among baseline, week 3, and week 6 and between week 3 and week 6 (p<0.01) in both groups. Similarly, significant improvement in functional score was noted among baseline, week 3, and week 6 and between week 3 and week 6 (p<0.01) in the post-op PT group. However, non-significant improvement in functional score was noted between baseline and week 3 and between week 3 and week 6 in the pre-post PT group (p>0.05). A significant improvement in functional score was noted between baseline and week 6 in the pre-post PT group (p<0.001). Tables 3 and 4 indicate inter group results. There were statistically insignificant differences in pain intensity and functional score between the pre-post PT and post-op PT groups (p>0.05) at baseline and at week 3 and week 6 post-op.
Table 1. Comparison of VAS score over time in each group.
| Groups | Pre-op | 3 weeks post-op | 6 weeks post-op |
|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | |
| Pre- and post-op PT | 8.9 ± 0.9 | 4.7 ± 1.3* | 1.9 ± 1.4#† |
| Post-op PT only | 8.7 ± 1.0 | 4.1 ± 1.6* | 2.4 ± 1.3#† |
VAS: Visual analogue scale; SD: standard deviation; PT: physical therapy. *Difference between preoperatively (pre-op) and week 3, p<0.001. #Difference between week 3 and week 6, p<0.001. †Difference between pre-op and week 6 post-op, p<0.001
Table 2. Comparison of LEFS score over time in each group.
| Groups | Pre-op | 3 weeks post-op | 6 weeks post-op |
|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | |
| Pre-and post-op PT | 18.9 ± 10.1 | 28.6 ± 11.4 | 55.9 ± 15.9† |
| Post-op PT only | 15.6 ± 9.1 | 30.2 ± 12.8* | 58.0 ± 13.5#† |
LEFS: Lower extremity functional scale; SD: standard deviation; PT: physical therapy. *Difference between preoperatively (pre-op) and week 3 post-op functional score, p<0.001. #Difference between week 3 post-op and week 6 post-op, p<0.001. †Difference between pre-op and week 6 post-op, p<0.001
Table 3. Comparison of VAS score between pre- and post-operative PT and post-operative PT alone.
| Variables | Pre- and post-op PT | Post-op PT only |
|---|---|---|
| Mean ± SD | Mean ± SD | |
| Pre-op | 8.9 ± 0.9 | 8.7 ± 1.0 |
| 3 weeks post-op | 4.7 ± 1.3 | 4.1 ± 1.6 |
| 6 weeks post-op | 1.9 ± 1.4 | 2.4 ± 1.3 |
VAS: Visual analogue scale; SD: standard deviation; PT: physical therapy
Table 4. Comparison of LEFS score between the pre- and post-operative PT and the post-operative PT only.
| Variables | Pre-and post-op PT | Post-op PT only |
|---|---|---|
| Mean ± SD | Mean ± SD | |
| Pre-op | 18.9 ± 10.1 | 15.6 ± 9.1 |
| 3 weeks post-op | 28.6 ± 11.4 | 30.2 ± 12.8 |
| 6 weeks post-op | 55.9 ± 15.9 | 58.0 ± 13.5 |
LEFS: Lower extremity functional scale; SD: standard deviation; PT: physical therapy
DISCUSSION
The aim of this study was to compare the effect of pre-op and post-op PT versus post-op PT alone on pain and recovery of function after TKA. During the first post-op month, a significant reduction in pain and improvements in physical function were reported in both the groups. However, there was no difference between the two groups.
In the available literature on efficacy of exercise in TKA patients, most of the studies have focused either only on pre-op or post-op exercises. Only a few studies have compared the two. Similar to our study, previous studies have also questioned any additional benefit of the addition of pre-op exercises in patients undergoing joint arthroplasty, especially for the knee1, 8, 21). Neither a PT program to strengthen upper or lower limb strength nor exercises to improve knee range of motion and strength have been shown to add to the degree of improvement after TKA2, 22,23,24). However, targeted post-op care following pre-op assessments has been shown to decrease the length of hospital stay25).
Post-op management after arthroplasty surgery has been widely studied. Various studies have reported its effect on decreasing pain and length of stay after surgery25, 26). Still, there is no standard protocol available27). Most of the available studies focused on pain reduction, strength gain, or mobility after knee replacement surgeries. Fewer studies have taken the quality of life, the return to work and daily activities, or the physical functioning as a whole as outcome measures in such studies. Data on quality of life recovery after surgery plays an important role in deciding the standard of care for patients28). Hence, along with pain reduction, we decided to include the LEFS, which is a measure of activity limitation.
Although PT has been shown to be very effective in the management of arthritis and its prevention and progression29,30,31,32), this study suggests that additional pre-op PT did not bring about any further improvement in pain intensity or function after TKA. The reduction of pain and recovery of function were similar in subjects who received pre-op and post-op PT and those who received only post-op PT after TKA.
The present study had some potential limitations. The pre-op PT was given only during the hospital stay. The average hospital stay was 5 days; therefore, the number of sessions received during pre-op PT might not have been enough to bring about a significant change in the outcome. In addition, there was no follow-up after 6 weeks; therefore, the long-term effects of these interventions remain unclear. In the future study, in addition to pain and function, the assessment of the quadriceps and hamstring muscle strength, knee range of motion, and the gait parameters is warranted.
In conclusion, the reduction of pain and recovery of function were similar in subjects who received pre- and post-op PT and those who received only post-op PT after TKA. Additional pre-op PT did not bring about any further improvement in pain intensity and function after TKA.
Conflict of interest
None declared.
Acknowledgments
The project was full financially supported by King Saud University, Vice Deanship of Research Chairs, Rehabilitation Research Chair.
REFERENCES
- 1.Kwok IH, Paton B, Haddad FS: Does pre-operative physiotherapy improve outcomes in primary total knee arthroplasty?—a systematic review. J Arthroplasty, 2015, 30: 1657–1663. [DOI] [PubMed] [Google Scholar]
- 2.Ackerman IN, Bennell KL: Does pre-operative physiotherapy improve outcomes from lower limb joint replacement surgery? A systematic review. Aust J Physiother, 2004, 50: 25–30. [DOI] [PubMed] [Google Scholar]
- 3.Büker N, Akkaya S, Akkaya N, et al. : Comparison of effects of supervised physiotherapy and a standardized home program on functional status in patients with total knee arthroplasty: a prospective study. J Phys Ther Sci, 2014, 26: 1531–1536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim SM, Kim SR, Lee YK, et al. : The effect of mechanical massage on early outcome after total knee arthroplasty: a pilot study. J Phys Ther Sci, 2015, 27: 3413–3416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Demircioglu DT, Paker N, Erbil E, et al. : The effect of neuromuscular electrical stimulation on functional status and quality of life after knee arthroplasty: a randomized controlled study. J Phys Ther Sci, 2015, 27: 2501–2506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Petterson SC, Mizner RL, Stevens JE, et al. : Improved function from progressive strengthening interventions after total knee arthroplasty: a randomized clinical trial with an imbedded prospective cohort. Arthritis Rheum, 2009, 61: 174–183. [DOI] [PubMed] [Google Scholar]
- 7.Wallis JA, Taylor NF: Pre-operative interventions (non-surgical and non-pharmacological) for patients with hip or knee osteoarthritis awaiting joint replacement surgery—a systematic review and meta-analysis. Osteoarthritis Cartilage, 2011, 19: 1381–1395. [DOI] [PubMed] [Google Scholar]
- 8.Beaupre LA, Lier D, Davies DM, et al. : The effect of a preoperative exercise and education program on functional recovery, health related quality of life, and health service utilization following primary total knee arthroplasty. J Rheumatol, 2004, 31: 1166–1173. [PubMed] [Google Scholar]
- 9.Dauty M, Genty M, Ribinik P: Physical training in rehabilitation programs before and after total hip and knee arthroplasty. Ann Readapt Med Phys, 2007, 50: 462–468, 455–461. [DOI] [PubMed] [Google Scholar]
- 10.Silkman Baker C, McKeon JM: Does preoperative rehabilitation improve patient-based outcomes in persons who have undergone total knee arthroplasty? A systematic review. PM R, 2012, 4: 756–767. [DOI] [PubMed] [Google Scholar]
- 11.Singh G: Randomization made easy for small size controlled clinical trials. JIAMSE, 2006, 16: 75–78. [Google Scholar]
- 12.Altman R, Asch E, Bloch D, et al. Diagnostic and Therapeutic Criteria Committee of the American Rheumatism Association: Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Arthritis Rheum, 1986, 29: 1039–1049. [DOI] [PubMed] [Google Scholar]
- 13.McCormack HM, Horne DJ, Sheather S: Clinical applications of visual analogue scales: a critical review. Psychol Med, 1988, 18: 1007–1019. [DOI] [PubMed] [Google Scholar]
- 14.Gaston-Johansson F: Measurement of pain: the psychometric properties of the Pain-O-Meter, a simple, inexpensive pain assessment tool that could change health care practices. J Pain Symptom Manage, 1996, 12: 172–181. [DOI] [PubMed] [Google Scholar]
- 15.Todd KH, Funk KG, Funk JP, et al. : Clinical significance of reported changes in pain severity. Ann Emerg Med, 1996, 27: 485–489. [DOI] [PubMed] [Google Scholar]
- 16.Kelly AM: Does the clinically significant difference in visual analog scale pain scores vary with gender, age, or cause of pain? Acad Emerg Med, 1998, 5: 1086–1090. [DOI] [PubMed] [Google Scholar]
- 17.Watson CJ, Propps M, Ratner J, et al. : Reliability and responsiveness of the lower extremity functional scale and the anterior knee pain scale in patients with anterior knee pain. J Orthop Sports Phys Ther, 2005, 35: 136–146. [DOI] [PubMed] [Google Scholar]
- 18.Pua YH, Cowan SM, Wrigley TV, et al. : The lower extremity functional scale could be an alternative to the western Ontario and McMaster universities osteoarthritis index physical function scale. J Clin Epidemiol, 2009, 62: 1103–1111. [DOI] [PubMed] [Google Scholar]
- 19.Binkley JM, Stratford PW, Lott SA, et al. North American Orthopaedic Rehabilitation Research Network: The Lower Extremity Functional Scale (LEFS): scale development, measurement properties, and clinical application. Phys Ther, 1999, 79: 371–383. [PubMed] [Google Scholar]
- 20.Stratford PW, Kennedy DM, Hanna SE: Condition-specific western Ontario McMaster osteoarthritis index was not superior to region-specific lower extremity functional scale at detecting change. J Clin Epidemiol, 2004, 57: 1025–1032. [DOI] [PubMed] [Google Scholar]
- 21.Jordan RW, Smith NA, Chahal GS, et al. : Enhanced education and physiotherapy before knee replacement; is it worth it? A systematic review. Physiotherapy, 2014, 100: 305–312. [DOI] [PubMed] [Google Scholar]
- 22.D’Lima DD, Colwell CW, Jr, Morris BA, et al. : The effect of preoperative exercise on total knee replacement outcomes. Clin Orthop Relat Res, 1996, (326): 174–182. [DOI] [PubMed] [Google Scholar]
- 23.Rooks DS, Huang J, Bierbaum BE, et al. : Effect of preoperative exercise on measures of functional status in men and women undergoing total hip and knee arthroplasty. Arthritis Rheum, 2006, 55: 700–708. [DOI] [PubMed] [Google Scholar]
- 24.Rodgers JA, Garvin KL, Walker CW, et al. : Preoperative physical therapy in primary total knee arthroplasty. J Arthroplasty, 1998, 13: 414–421. [DOI] [PubMed] [Google Scholar]
- 25.Oldmeadow LB, McBurney H, Robertson VJ, et al. : Targeted postoperative care improves discharge outcome after hip or knee arthroplasty. Arch Phys Med Rehabil, 2004, 85: 1424–1427. [DOI] [PubMed] [Google Scholar]
- 26.Lenssen AF, Crijns YH, Waltjé EM, et al. : Efficiency of immediate postoperative inpatient physical therapy following total knee arthroplasty: an RCT. BMC Musculoskelet Disord, 2006, 7: 71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Youm T, Maurer SG, Stuchin SA: Postoperative management after total hip and knee arthroplasty. J Arthroplasty, 2005, 20: 322–324. [DOI] [PubMed] [Google Scholar]
- 28.Ethgen O, Bruyère O, Richy F, et al. : Health-related quality of life in total hip and total knee arthroplasty. A qualitative and systematic review of the literature. J Bone Joint Surg Am, 2004, 86-A: 963–974. [DOI] [PubMed] [Google Scholar]
- 29.Ettinger WH, Jr, Burns R, Messier SP, et al. : A randomized trial comparing aerobic exercise and resistance exercise with a health education program in older adults with knee osteoarthritis. The Fitness Arthritis and Seniors Trial (FAST). JAMA, 1997, 277: 25–31. [PubMed] [Google Scholar]
- 30.Tanaka R, Ozawa J, Kito N, et al. : Efficacy of strengthening or aerobic exercise on pain relief in people with knee osteoarthritis: a systematic review and meta-analysis of randomized controlled trials. Clin Rehabil, 2013, 27: 1059–1071. [DOI] [PubMed] [Google Scholar]
- 31.Anwer S, Alghadir A: Effect of isometric quadriceps exercise on muscle strength, pain, and function in patients with knee osteoarthritis: a randomized controlled study. J Phys Ther Sci, 2014, 26: 745–748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Anwer S, Alghadir A, Brismée JM: Effect of home exercise program in patients with knee osteoarthritis: a systematic review and meta-analysis. J Geriatr Phys Ther, 2016, 39: 38–48. [DOI] [PubMed] [Google Scholar]


