Abstract
[Purpose] The aim of this case study was to investigate whether a method of mental practice (MP) using an inverse video of a subject’s unaffected limb to complement the vividness of motor imagery (MI) would be effective for improving affected upper limb function. [Subjects and Methods] The participant was 60-year-old male in the chronic stage of stroke recovery with left sided hemiparesis. The design of the study was AB method of Single-System-Design. He performed the MP as a home program with DVD. The intervention lasted 30 minutes a session, twice a day, 5 times a week, over 6 weeks. The DVD was created using inverse video of his unaffected upper limb. Primary outcome measures were used the Fugl-Meyer Assessment for upper limb (FMA) and the Motor Activity Log (MAL) 3 times each baseline, intervention and follow-up. The subjective vividness of MI was assessed by the Visual Analog Scale (VAS). [Results] FMA and MAL score during intervention was improved significantly comparing to baseline, and maintained in withdrawal. VAS score was improved in withdrawal comparing to baseline. [Conclusion] Results suggested that effect of mental practice for stroke patients increased by vividness of motor imagery was improved by the inverse video.
Key words: Stroke, Mental practice, Inverse video
INTRODUCTION
Recent studies have shown that mental practice (MP) is which motor imagery (MI) is performed repeatedly can improve motor functions in patients after stroke; these effects have been demonstrated in clinical studies using randomized controlled trials1,2,3,4,5). An important aspect in mental practice is how vividly an individual can perform MI. To complement the vividness of MI, previous clinical studies used audio or visual guides during intervention and reported improvement of upper limb function and ADL1, 3).
However, there are some studies that vividness of MI differs depending on the specific features of the tasks and the subject’s ability to MI6, 7). Prior study reported that the vividness of MI was correlated with corticospinal excitability during MI8) and effect of MP was influenced by the vividness of MI. Particularly, in patients with severe sensory disturbance after stroke, excitability of the corticospinal tract of the affected side and ability for MI were significantly lower than in healthy controls and patients with pure motor strokes9). Therefore, it is more difficult for patients with sensory disturbance to perform MI vividly, which hinders demonstration of a significant effect of MP. Furthermore, since the effectiveness of MP differs depending on the method used to support MI, there is currently no effective and reproducible clinical method of MP.
Therefore, this case study investigated whether a method of MP using an inverse video of a subject’s unaffected limb to complement the vividness of MI would be effective for improving affected upper limb function. In this study, we examined effects of how this MP using single-case design.
SUBJECTS AND METHODS
The patient was a 60-year-old man with left-sided moderate hemiparesis and severe sensory torpor resulting from a cerebral hemorrhage that occurred 5 years before the intervention. Immediately after the onset, he received 3 hours of standard inpatient rehabilitation every day for 6 months. Since discharge from the hospital, he received 1 hour of standard outpatient occupational therapy (OT) once a week. ADL was 60 points in Barthel Index (BI). No cognitive deficits were noted. His main complaint was “I can’t perform the imagination that my left hand is moving.” His basic characteristics are shown in Table 1. The patient agreed to participate in the study and signed an informed consent form approved by the Miharadai Hospital ethics committee.
Table 1. Participant’s information.
| Diagnosis | Cerebral hemorrhage (Pontine) | |
| Left hemiplegia | ||
| Motor function | Brunnstrom stage | 5/6 |
| FMA | 47/66 | |
| Sensory function | Superficial sensation | severe hypoesthesia |
| Deep sensation | severe hypoesthesia | |
| ADL | Barthel Index | 60/100 |
| Functinal Independence Measure | 95/126 | |
This single-subject study was conducted using an A-B-A design. The data obtained in phase A was used as a baseline to evaluate the effect of intervention in phase B. Phase A was then used as follow-up. The participant performed MP as a home program with a DVD in addition to following an outpatient OT program. The intervention lasted 30 minutes per session, twice a day, 5 times a week, over 6 weeks. The DVD was created using an inverse video of his unaffected upper limb such that it appeared as if his affected arm was moving. He performed kinesthetic motor imagery. To create with inverse video, GOM-ENCODER of free software was used. The MI task used for MP adopted four actions that he was seeking to improve: 1) supporting weight with a hand on a desk, 2) grasping a handrail, 3) turning over a page the newspaper, and 4) holding a cup (Fig. 1). He performed in the same frequency and content of the outpatient OT in clinics during the study period.
Fig. 1.
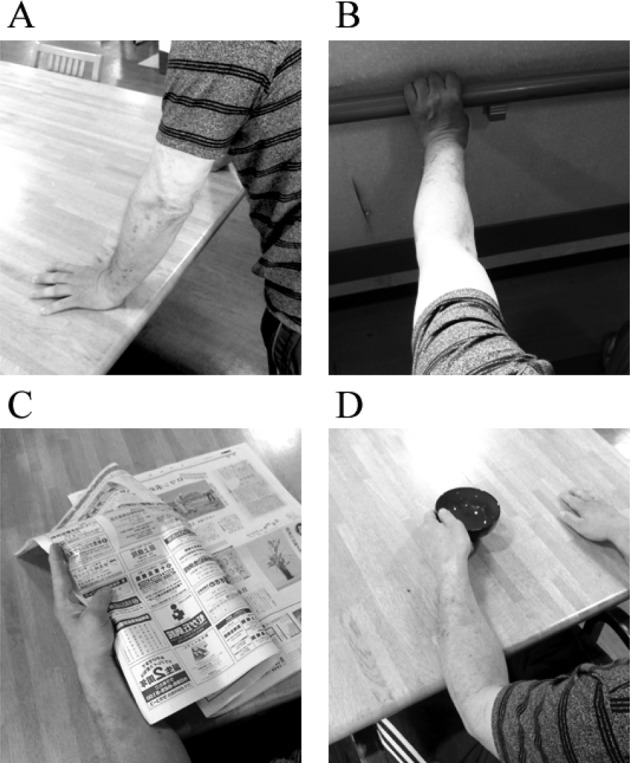
The MI task of four actions used for MP. A) supporting weight with a hand on a desk, B) grasping a handrail, C) turning over a page the newspaper, and D) holding a cup
Primary outcome measures were the Fugl-Meyer Assessment for the upper extremity (FMA)10) and the Motor Activity Log (MAL) for functions of upper extremity11). We assessed 3 times each at baseline, intervention and follow-up. The motor abilities of the paretic upper limb were assessed with the FMA. The arm motor component of FMA consists of 30 items that evaluate basic arm function and 3 items that evaluate coordination and speed. MAL is a structured questionnaire in which 14 specific ADLs are rated on a 6-point scale (0 to 5). The questionnaire gathers information on how well and how often ADLs are performed using the affected arm in the home environment. MAL was evaluated in two methods the amount of use of upper movement (AOU) and the quality of upper movement (QOM). During each phase, vividness of the subject’s MI was determined by self-evaluation using a visual analogue scale (VAS)12,13,14); the subject marked a location on a 100-mm horizontal line according to the vividness of his imagery. All measurements were conducted by an occupational therapist not involved in the MP application.
Visual analysis and the 2-standard deviation (2-SD) band method were used to analyze the FMA and the MAL data (AOU and QOM). This method involves computing the mean and 2-SD values of baseline data. If at least two consecutive data points in the intervention phase fall outside the 2-SD band, changes from baseline to intervention are regarded as significant15).
RESULTS
Compared to the baseline, the FMA and the AOU scores were improved significantly during intervention and were maintained at follow-up, whereas the QOM score showed no significant improvement (Table 2). The VAS score was improved at follow-up comparing to baseline. The patient’s holding and grasping ability improved, and got to be able to use a handrail with his left hand.
Table 2. Statistic analysis of each outcome measure.
| Protocol | Baseline | Intervention | Follow-up | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 1st | 2nd | 3rd | 1st | 2nd | 3rd | 1st | 2nd | 3rd | |
| FMA | 47 | 49 | 50 | 48 | 52* | 53* | 56* | 55* | 54* |
| Average+2SD | 51.7 | ||||||||
| AOU | 0.5 | 0.8 | 0.5 | 0.9* | 0.9* | 1.1* | 1.0* | 1.2* | 1.0* |
| Average+2SD | 0.88 | ||||||||
| QOM | 0.7 | 0.9 | 0.7 | 0.9 | 0.9 | 1.0 | 0.8 | 1.1* | 0.8 |
| Average+2SD | 1.03 | ||||||||
| VAS | 51 | 64 | 87 | ||||||
2-SD band method*>Baseline Average+2SD. If at least two consecutive data points in the intervention phase fall outside the 2-SD band, changes from baseline to intervention are regarded as significant.
DISCUSSION
In this study, the FMA and AOU score improved significantly in the intervention period in association with the method of MP using an inverse video of a subject’s unaffected limb, and maintained improvement in the follow up period. Previous studies have shown that brain regions activated during MI are similar to those activated during motor execution16, 17). MP can assist motor execution and effectively improve motor functions18). Moreover, previous study have reported that kinesthetic MI is more effective in motor learning of upper limb than the visual MI18). And it has also been reported that the vividness of the MI affects the effects of MI6). In this case study, FMA and AOU scores improved significantly in the intervention phase and were maintained in the follow-up phase.
In addition, the VAS score improved after intervention, suggesting that the use of the inverse video helped the patient to perform kinesthetic MI vividly as if his arm was actually moving, which improved the FMA score. Regarding AOU, the MI tasks performed in this study were those that the subject hoped to improve and had been implemented in outpatient OT. MI combined with actual actions has been shown to be more effective for MP19). Our subject received outpatient OT only once a week, but MI was combined as additional self-training, which likely helped improve the actions used for the MI task. Moreover, the increased frequency of upper limb use in his daily life might have contributed to the preservation of improved functions.
Another reason for the effectiveness of MP in this case might be that watching the inverse video of his own unaffected hand made the subject feel like his affected hand was moving; this made him perform MI easier and motivated him to continue training. These points have been shown as important factors for the success of MP7, 20). Furthermore, as we selected using DVD, the subject was able to perform MP training easily at home or in a work environment, which helped the subject ensure the time for MP constantly. Managing the environment for continuous training is also considered as an important factor for the effective MP. Moreover, previous study have shown that a minimum of a 30 minutes practice at least once per day is required for effective MP21). This study secured enough time for training compared to the previous studies.
Therefore, this study suggested that an inverse video of a subject’s unaffected limb seems to be an effective tool for assistance of MI in performing MP. Next, we aim to evaluate a method of MP support using tablet devices and develop a method for convenient and easy use of an inverse video. In future research, it will be necessary to consider approaching multiple cases with randomized controlled trial to establish the effective method of neuro-rehabilitation.
REFERENCES
- 1.Page SJ, Levine P, Sisto S, et al. : A randomized efficacy and feasibility study of imagery in acute stroke. Clin Rehabil, 2001, 15: 233–240. [DOI] [PubMed] [Google Scholar]
- 2.Sharma N, Pomeroy VM, Baron JC: Motor imagery: a backdoor to the motor system after stroke? Stroke, 2006, 37: 1941–1952. [DOI] [PubMed] [Google Scholar]
- 3.Liu KP, Chan CC, Lee TM, et al. : Mental imagery for promoting relearning for people after stroke: a randomized controlled trial. Arch Phys Med Rehabil, 2004, 85: 1403–1408. [DOI] [PubMed] [Google Scholar]
- 4.Page SJ, Murray C, Hermann V, et al. : Retention of motor changes in chronic stroke survivors who were administered mental practice. Arch Phys Med Rehabil, 2011, 92: 1741–1745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Riccio I, Iolascon G, Barillari MR, et al. : Mental practice is effective in upper limb recovery after stroke: a randomized single-blind cross-over study. Eur J Phys Rehabil Med, 2010, 46: 19–25. [PubMed] [Google Scholar]
- 6.Mulder T, Zijlstra S, Zijlstra W, et al. : The role of motor imagery in learning a totally novel movement. Exp Brain Res, 2004, 154: 211–217. [DOI] [PubMed] [Google Scholar]
- 7.Schuster C, Hilfiker R, Amft O, et al. : Best practice for motor imagery: a systematic literature review on motor imagery training elements in five different disciplines. BMC Med, 2011, 9: 75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Williams J, Pearce AJ, Loporto M, et al. : The relationship between corticospinal excitability during motor imagery and motor imagery ability. Behav Brain Res, 2012, 226: 369–375. [DOI] [PubMed] [Google Scholar]
- 9.Liepert J, Greiner J, Nedelko V, et al. : Reduced upper limb sensation impairs mental chronometry for motor imagery after stroke: clinical and electrophysiological findings. Neurorehabil Neural Repair, 2012, 26: 470–478. [DOI] [PubMed] [Google Scholar]
- 10.Fugl-Meyer AR, Jääskö L, Leyman I, et al. : The post-stroke hemiplegic patient. 1. a method for evaluation of physical performance. Scand J Rehabil Med, 1975, 7: 13–31. [PubMed] [Google Scholar]
- 11.Uswatte G, Taub E, Morris D, et al. : Reliability and validity of the upper-extremity Motor Activity Log-14 for measuring real-world arm use. Stroke, 2005, 36: 2493–2496. [DOI] [PubMed] [Google Scholar]
- 12.Ikeda K, Higashi T, Sugawara K, et al. : The effect of visual and auditory enhancements on excitability of the primary motor cortex during motor imagery: a pilot study. Int J Rehabil Res, 2012, 35: 82–84. [DOI] [PubMed] [Google Scholar]
- 13.Lotze M, Halsband U: Motor imagery. J Physiol Paris, 2006, 99: 386–395. [DOI] [PubMed] [Google Scholar]
- 14.Ohno K, Higashi T, Sugawara K, et al. : Excitability changes in the human primary motor cortex during observation with motor imagery of chopstick use. J Phys Ther Sci, 2011, 23: 703–706. [Google Scholar]
- 15.Nourbakhsh MR, Ottenbacher KJ: The statistical analysis of single-subject data: a comparative examination. Phys Ther, 1994, 74: 768–776. [DOI] [PubMed] [Google Scholar]
- 16.Solodkin A, Hlustik P, Chen EE, et al. : Fine modulation in network activation during motor execution and motor imagery. Cereb Cortex, 2004, 14: 1246–1255. [DOI] [PubMed] [Google Scholar]
- 17.Stephan KM, Fink GR, Passingham RE, et al. : Functional anatomy of the mental representation of upper extremity movements in healthy subjects. J Neurophysiol, 1995, 73: 373–386. [DOI] [PubMed] [Google Scholar]
- 18.Nilsen DM, Gillen G, Gordon AM: Use of mental practice to improve upper-limb recovery after stroke: a systematic review. Am J Occup Ther, 2010, 64: 695–708. [DOI] [PubMed] [Google Scholar]
- 19.Ertelt D, Small S, Solodkin A, et al. : Action observation has a positive impact on rehabilitation of motor deficits after stroke. Neuroimage, 2007, 36: T164–T173. [DOI] [PubMed] [Google Scholar]
- 20.Braun SM, van Haastregt JC, Beurskens AJ, et al. : Feasibility of a mental practice intervention in stroke patients in nursing homes; a process evaluation. BMC Neurol, 2010, 10: 74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Page SJ, Dunning K, Hermann V, et al. : Longer versus shorter mental practice sessions for affected upper extremity movement after stroke: a randomized controlled trial. Clin Rehabil, 2011, 25: 627–637. [DOI] [PMC free article] [PubMed] [Google Scholar]


