Abstract
Objective:
The tendency to react with fear to anxiety-related sensations (anxiety sensitivity) and the inability to tolerate distressing psychological or physiological states (distress intolerance) are implicated in the comorbidity between affective psychopathology and cannabis use disorders. Emotionally vulnerable cannabis users may be particularly apt to use cannabis to cope with distress, which may both lead to and maintain its problematic use (e.g., dependence, craving). The current study tested a comprehensive model of anxiety sensitivity and distress intolerance as predictors of the number of cannabis dependence symptoms and problems, and severity of cannabis craving following deprivation from cannabis, and the mediating role of cannabis coping motives.
Method:
Participants (n = 103; mean age = 21.2 years, SD = 4.3; 35.9% female) were non–treatment-seeking frequent cannabis users. Data were cross-sectional in nature. Anxiety sensitivity was assessed via self-report, and distress intolerance was assessed via both self-report and breath-holding duration.
Results:
Greater perceived distress intolerance, but not breath-holding duration or anxiety sensitivity, was associated with a greater number of cannabis dependence symptoms and problems and elevated cannabis craving. These relations were mediated by cannabis coping motives.
Conclusions:
Findings provide specificity for the etiologic mechanisms related to emotional vulnerability and maintenance of cannabis problems. Perceived distress intolerance appears to be uniquely related to maladaptive coping motives for cannabis use, which could be meaningfully targeted in interventions for emotionally vulnerable cannabis users.
It is estimated that 43%–48% of individuals with cannabis use disorders also have a comorbid anxiety or mood disorder (e.g., Buckner et al., 2012; Conway et al., 2006; Cougle et al., 2011; Stinson et al., 2006; Tournier et al., 2003). Negative-reinforcement motivational models of substance use (Baker et al., 2004; McCarthy et al., 2010) provide a framework for understanding how individuals may use and rely on cannabis to acutely cope with situational negative affect (Haney et al., 1999; McDonald et al., 2003; Metrik et al., 2011; Phan et al., 2008) which, in the absence of alternative strategies for managing negative affect, may promote heightened drug use (Metrik et al., in press; Moitra et al., 2015). Importantly, there is recognition that how individuals interpret and respond to distressing psychological or physiological states is linked to the maintenance of problematic substance use (e.g., Brown et al., 2005). Specifically, sensitivity to, and intolerance of, unpleasant physiological and psychological states may amplify the experience of distress, which may in turn motivate avoidance-focused behaviors (e.g., Brown et al., 2008; Tull et al., 2007). Two transdiagnostic vulnerability factors that appear to be predictors of both problematic substance use and affective psychopathology are anxiety sensitivity and distress intolerance.
Anxiety sensitivity, defined as the tendency to catastrophize and misinterpret the meaning of anxiety-relevant interoceptive sensations (Reiss et al., 1986), is associated with the development and maintenance of affective symptoms and disorders (Naragon-Gainey, 2010; Olatunji & Wolitzky-Taylor, 2009) and problematic substance use, including cannabis use (Buckner et al., 2011; Johnson et al., 2010). When experiencing physiological distress, individuals high in anxiety sensitivity become acutely fearful because of beliefs that these somatic sensations have harmful physical, psychological, or social consequences (Taylor et al., 2007), which may amplify the experience of distress and promote coping-focused cannabis use (Bonn-Miller et al., 2007; Comeau et al., 2001; Mitchell et al., 2007; Zvolensky et al., 2009). Indeed, cannabis coping motives mediate the relation between anxiety sensitivity and risk for cannabis dependence (Johnson et al., 2010).
Distress intolerance, defined as one’s perceived or objective inability to withstand aversive psychological or physiological states (e.g., stress, frustration, anxiety, pain), is implicated in the development and maintenance of psychopathology (Leyro et al., 2010) and is a key vulnerability factor associated with problematic substance use (Brandon et al., 2003; Vujanovic et al., 2011). Perceived and objective (behaviorally measured) distress intolerance are considered distinct constructs and hold differential associations with psychological symptoms and quality of life indices (Bernstein et al., 2011). Theoretically, perceived distress intolerance is considered to precede attempts to regulate or cope with distress states, whereas behavioral acts to withstand distress can be considered response-focused emotion regulation (Bernstein et al., 2011).
The majority of the distress intolerance–cannabis literature has focused exclusively on perceived distress intolerance. For example, cannabis users who perceive that they are less apt to handle mental distress endorse stronger coping motives for cannabis use (Potter et al., 2011; Zvolensky et al., 2009) and report more cannabis use and cannabis use problems (Buckner et al., 2007; Dvorak & Day, 2014). Moreover, coping motives appear to explain the relation between perceived distress intolerance and severity of cannabis problems (Bujarski et al., 2012). Initial evidence indicates that lower perceived distress intolerance, but not objective (behaviorally measured) distress intolerance, is associated with reductions in cannabis use during a self-guided quit attempt (Hasan et al., 2015), which suggests that one’s belief about his or her inability to persist in goal-directed behavior in the context of distress, relative to actual (in vivo) inability, may be more closely linked to cannabis use. Thus, it is possible that perceived versus actual inability to tolerate distress may be uniquely linked to cannabis coping motives, although these associations have not yet been examined.
Importantly, examination of the structural relations between anxiety sensitivity (fear that anxiety sensations are harmful) and distress intolerance (perceived or actual ability to withstand distress) suggests that these constructs are distinct lower-order facets that comprise a shared higher-order factor of “emotional sensitivity and tolerance” (Bernstein et al., 2009; McHugh & Otto, 2012). It is worth noting that although these constructs are related, they may differentially present across and within individuals. For example, an individual may be fearful of internal sensations (high anxiety sensitivity) but hold strong beliefs about his or her ability to withstand distress states (low perceived distress intolerance) and be capable of persisting in goal-directed activity in the face of distress states (low objective distress intolerance). Anxiety sensitivity and distress intolerance are posited to inform distinct negative-reinforcement motivational pathways for substance use (e.g., Kassel & Unrod, 2000; Kassel et al., 2003).
Specifically, a high anxiety sensitive cannabis user would be very fearful of experiencing arousal because of concerns about the negative consequences of such sensations, and he or she may use cannabis in an effort to avoid feared (anticipated) physiological arousal sensations. A cannabis user with high perceived inability to tolerate distress states may use cannabis to eliminate distress based on the belief that he or she would be unable to otherwise withstand the distress state. Relatedly, in the context of a stressor, a cannabis user who was behaviorally unable to withstand distress may be more likely to initiate cannabis use as a “low-effort” strategy for escaping distress. It is important to understand the unique associations between these constructs in order to (a) increase understanding of specific vulnerability factors that are most strongly related to coping-motivated cannabis use, which would (b) inform tailoring of therapeutic interventions to be used in the treatment of coping-oriented cannabis use. Thus, a simultaneous test of these emotional sensitivity/intolerance factors would provide increased specificity in our understanding of transdiagnostic emotional processes that may be linked to cannabis use.
Therefore, the present study tested one empirically driven model of the concurrent direct associations of anxiety sensitivity, perceived distress intolerance, and behavioral intolerance of physical distress states in terms of multiple indicators of problematic cannabis use as follows: (a) number of cannabis dependence symptoms, (b) number of cannabis use problems, and (c) severity of cannabis craving following 15 hours of deprivation. Consistent with negative-reinforcement models of drug addiction, the mediating role of cannabis coping motives was also examined. Based on findings from a prior study of emotional sensitivity/intolerance and motivational processes underlying problematic alcohol use (Howell et al., 2010), it was hypothesized that perceived distress intolerance would be uniquely linked to coping motives for use, which in turn would be related to problematic cannabis use (cannabis dependence symptoms, problems, and severity of cannabis craving). Data were obtained from participants who completed baseline assessments during an experimental study of the effects of cannabis administration on processing of emotional stimuli among frequent cannabis users (Metrik et al., 2015).
Method
Participants
Participants (n = 103; Mage = 21.2 years, SD = 4.32; 35.9% female) were non-treatment-seeking frequent cannabis users recruited from the community who met the following inclusion criteria: native English speakers, 18–44 years of age, non-Hispanic White (due to genetic aims of the parent study; Metrik et al., 2015), cannabis use at least 2 days per week in the past month and at least weekly in the past 6 months, and self-reported ability to abstain from cannabis for 24 hours without withdrawal. Exclusion criteria were intent to quit or receive treatment for cannabis use disorder; positive urine toxicology test result for drugs other than cannabis; pregnancy; nursing; past-month depressive, manic, and/or panic disorders (due to cannabis administration procedures used in the parent study) according to criteria in the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV; American Psychiatric Association, 1994); psychotic or suicidal state as assessed by the Structured Clinical Interview for DSM-IV Disorders Non-Patient Edition (SCID-I/NP; First et al., 2002); contraindicated medical issues by physical exam; and smoking more than 20 tobacco cigarettes per day. Participants reported using cannabis on an average of 72.1% (SD = 21.4%) of days in the 60 days before baseline, with a mean of 2.03 (SD = 1.22) times a day. Furthermore, 13.6% of the sample met criteria for past-year DSM-IV cannabis dependence, and an average of 3.6 (SD = 2.9; observed range = 0–13) problems related to cannabis use were reported. The median reported family income bracket of participants was $60,000-$69,000 annually.
Procedure
The current study involves a secondary data analysis of baseline data from a sample recruited for a larger parent study (Metrik et al., 2015). Participants completed a battery of interview and self-report assessments. As part of the experimental study, participants abstained from cannabis and tobacco smoking for 15 hours before the session. An alveolar carbon monoxide (CO) of ≤ 6 ppm (verified with a Smokerlyzer, Bedfont Scientific Ltd., Maidstone, Kent, England) was used to confirm no recent cannabis or tobacco smoking (Cooper & Haney, 2009; Metrik et al. 2015), and zero breath alcohol concentration was verified with an Alco-Sensor IV (Intoximeters, Inc., St Louis, MO). Tobacco smokers were permitted to smoke a tobacco cigarette following the CO test to prevent nicotine withdrawal. Participants were compensated upon study completion. One participant was missing data on a key predictor measure and thus was excluded from the presented analyses. The study was approved by the Institutional Review Board at Brown University, and informed consent was completed before initiation of study procedures.
Measures
Timeline Followback Interview.
The Timeline Followback (Sobell & Sobell, 1996) was conducted at baseline for the 60 days before the visit and used to characterize the sample in terms of cannabis use and the presence of cigarette smoking.
Structured Clinical Interview for DSM-IV Disorders–Non-Patient Edition.
The SCID-I/NP (First et al., 2002) was used to assess DSM-IV Axis I diagnoses and a symptom count for the number of cannabis dependence symptoms, which included the presence of cannabis withdrawal per DSM-5 criteria (American Psychiatric Association, 2013). Thus, the possible symptom count ranged from 0 to 7 (observed range: 0–6).
Marijuana Problems Scale.
The Marijuana Problems Scale (MPS; Stephens et al., 2000) is a self-report 22-item questionnaire that evaluates problems experienced in the past 90 days related to cannabis use. A total count of combined minor and serious problems was used. The MPS has strong internal consistency (Peters et al., 2011; Stephens et al., 2000). Internal consistency of MPS items was α = .76.
Marijuana Craving Questionnaire.
The Marijuana Craving Questionnaire (MCQ; Budney et al., 2003) is a 10-item self-report assessment of subjective cannabis craving. Participants were asked to respond to items (rated on a 1 = strongly disagree to 7 = strongly agree scale) according to how they were thinking or feeling “right now,” with higher scores indicating greater subjective cannabis craving. Items are averaged to yield a total craving score (possible range: 1–7; observed range: 1–6). Internal consistency of the MCQ items was α = .90. The MCQ was administered following a 15-hour deprivation period. The typical onset of cannabis withdrawal symptoms and craving is approximately observed within 24–48 hours after cessation (Budney et al., 2004); thus, the MCQ scores in the current study can be conceptualized as an index of the tendency to experience cannabis craving following deprivation (in contrast to cue-induced craving).1 In addition, the MCQ was correlated with a measure of cannabis withdrawal even in this sample of users (r = .41, p < .05) who self-reported the ability to abstain from cannabis for 24 hours without withdrawal.2
Comprehensive Marijuana Motives Questionnaire.
The Comprehensive Marijuana Motives Questionnaire (CMMQ; Lee et al., 2007, 2009) is a 36-item self-report assessment of motives for cannabis use, which yields 19 subscales of different types of motives. Participants are asked to rate on a 1 (almost never/never) to 7 (almost always/always) scale, how often they used cannabis for a number of listed reasons in several domains including coping. Three items were used to derive a mean composite coping subscale score to assess coping motives for cannabis use. The coping subscale items have good psychometric properties (Lee et al., 2009). Internal consistency of CMMQ coping items was α = .79.
Anxiety Sensitivity Index-3.
The Anxiety Sensitivity Index-3 (ASI-3; Taylor et al., 2007) is an 18-item self-report measure of the tendency to fear sensations associated with anxiety. Items are rated on a scale from 0 (very little) to 4 (very much) and summed to create a total score. The scale includes some items from the original Anxiety Sensitivity Index (Reiss et al., 1986). The ASI-3 is psychometrically sound (Farris et al., 2015; Taylor et al., 2007). Internal consistency of ASI-3 items was α = .81.
Distress Tolerance Scale.
The Distress Tolerance Scale (DTS; Simons et al., 2005) includes 15 items rated on a 5-point Likert-type scale ranging from 1 (strongly agree) to 5 (strongly disagree), assessing respondents’ perceived ability to experience and endure negative emotional states. Items are summed and a mean score is computed; possible range is 1–5, with higher scores reflecting greater tolerance (lower intolerance) for distress. This scale has good psychometric properties, including high internal consistency and convergent validity (Simons et al., 2005). Internal consistency of DTS items was α = .89.
Breath-Holding Duration Task.
The Breath-Holding Duration Task (Asmundson & Stein, 1994) is a behavioral assessment of distress intolerance. During the task, participants are asked to hold their breath for as long as they can while being timed with a stopwatch. Breath-holding duration is time to exhalation. This task has frequently been used as measure of physical distress intolerance (Brown et al., 2009; Hajek et al., 1987), with shorter durations of breath-holding indicating greater intolerance of physical distress. Research has suggested that breath-holding duration maintains unique predictive value beyond the effects of physical health conditions, active substance use, and anxiety sensitivity (Hogan et al., 2015).
Data analytic strategy
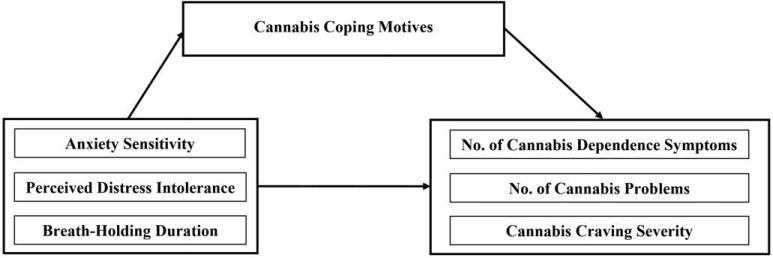
Preliminary descriptive analyses were conducted to examine bivariate (zero-order Pearson’s correlation) associations. Primary analyses were conducted in AMOS 22.0 (Arbuckle, 2013), and path modeling using maximum likelihood imputation and estimation were employed. A path model was constructed to examine the mediating role of cannabis coping motives in the association between anxiety sensitivity (ASI-3) and distress intolerance (DTS, breath-holding duration), and three criterion variables: (a) number of cannabis dependence symptoms, (b) number of cannabis-related problems, and (c) cannabis craving severity. All variables were entered into a single path model. See Figure 1 for conceptual model. Model fit was assessed using the comparative fit index (CFI) and the root mean square error of approximation (RMSEA). CFI is a goodness-of-fit measure of the amount of variance and covariance in the data set accounted for by the implied model, with values .90 or above considered acceptable fit (Kline, 2011). An RMSEA of .05 or less indicates good model fit, and RMSEA under .10 is considered to be in the acceptable range (Kline, 2011).
Figure 1.
Conceptual model. No. = number. Note: All variables entered into one path model.
Results
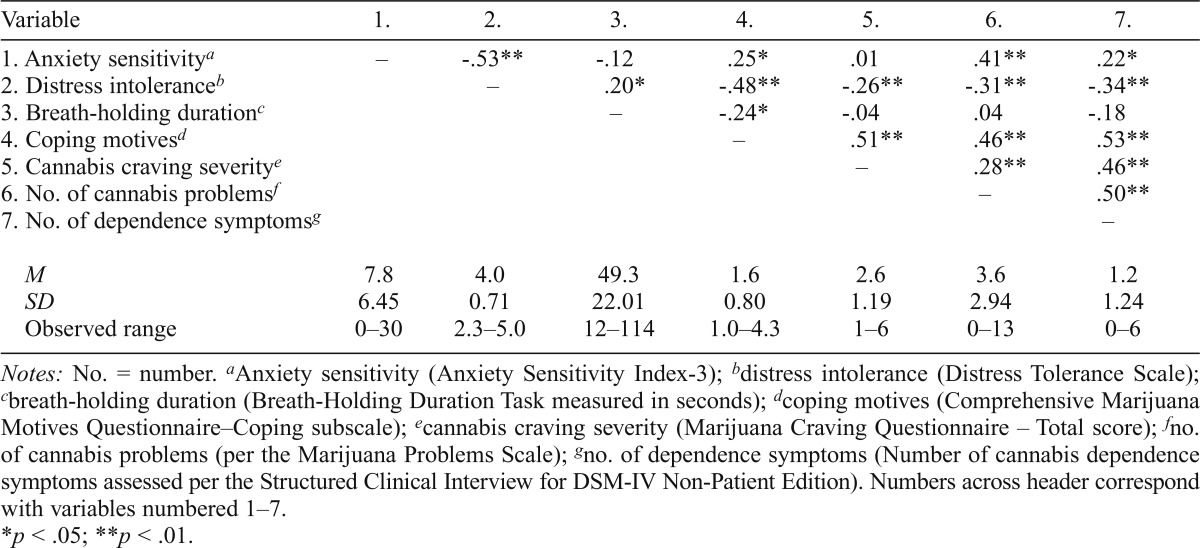
Bivariate correlations are presented in Table 1. The three criterion variables were significantly intercorrelated (medium-sized associations). Cannabis coping motives were significantly positively associated with all three criterion variables. The ASI-3 and DTS were significantly negatively associated, and the two distress intolerance measures were positively associated. The ASI-3 and breath-holding duration were not significantly associated. Mean scores on the ASI-3 were low (M = 7.8, SD = 6.5). Average scores on the DTS were slightly higher (although still within 1 SD) relative to other reported means among cannabis users (e.g., Zvolensky et al., 2009). Anxiety sensitivity was positively and significantly associated with cannabis coping motives as well as cannabis problems and cannabis dependence symptoms (medium-sized associations), although it was not significantly associated with cannabis craving severity. Distress intolerance measures (DTS and breath-holding duration) were significantly negatively correlated with cannabis coping motives. Only the DTS was significantly negatively associated with all criterion outcome variables (small- to medium-sized associations).
Table 1.
Bivariate correlations and descriptive overview (n = 103)
| Variable | 1. | 2. | 3. | 4. | 5. | 6. | 7. |
| 1. Anxiety sensitivitya | – | -.53** | -.12 | .25* | .01 | .41** | .22* |
| 2. Distress intoleranceb | – | .20* | -.48** | -.26** | -.31** | -.34** | |
| 3. Breath-holding durationc | – | -.24* | -.04 | .04 | -.18 | ||
| 4. Coping motivesd | – | .51** | .46** | .53** | |||
| 5. Cannabis craving severitye | – | .28** | .46** | ||||
| 6. No. of cannabis problemf | – | .50** | |||||
| 7. No. of dependence symptomsg | – | ||||||
| M | 7.8 | 4.0 | 49.3 | 1.6 | 2.6 | 3.6 | 1.2 |
| SD | 6.45 | 0.71 | 22.01 | 0.80 | 1.19 | 2.94 | 1.24 |
| Observed range | 0–30 | 2.3–5.0 | 12–114 | 1.0–4.3 | 1–6 | 0–13 | 0–6 |
Notes: No. = number.
Anxiety sensitivity (Anxiety Sensitivity Index-3);
distress intolerance (Distress Tolerance Scale);
breath-holding duration (Breath-Holding Duration Task measured in seconds);
coping motives (Comprehensive Marijuana Motives Questionnaire–Coping subscale);
cannabis craving severity (Marijuana Craving Questionnaire – Total score);
no. of cannabis problems (per the Marijuana Problems Scale);
no. of dependence symptoms (Number of cannabis dependence symptoms assessed per the Structured Clinical Interview for DSM-IV Non-Patient Edition). Numbers across header correspond with variables numbered 1–7.
p <.05;
p <.01.
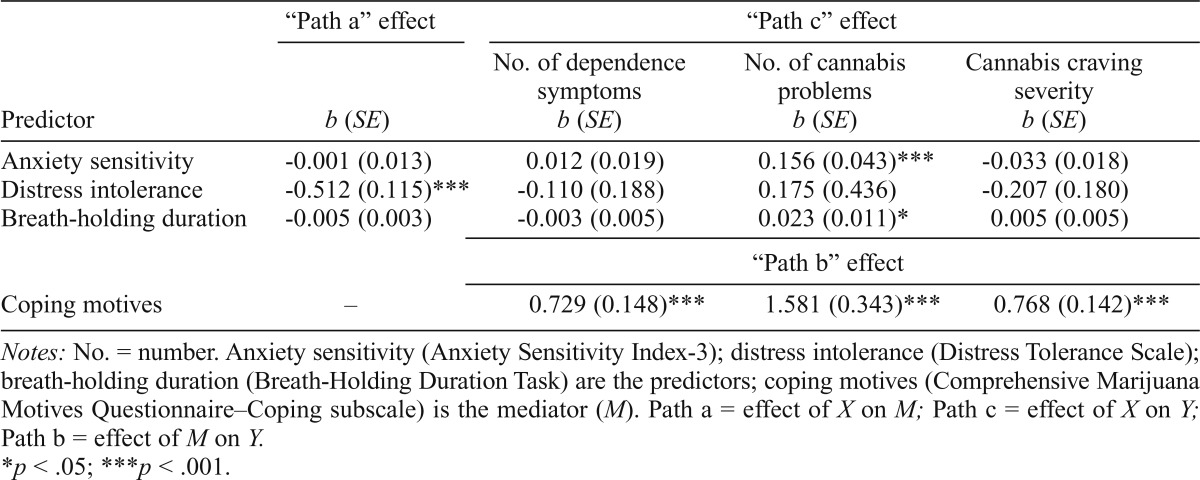
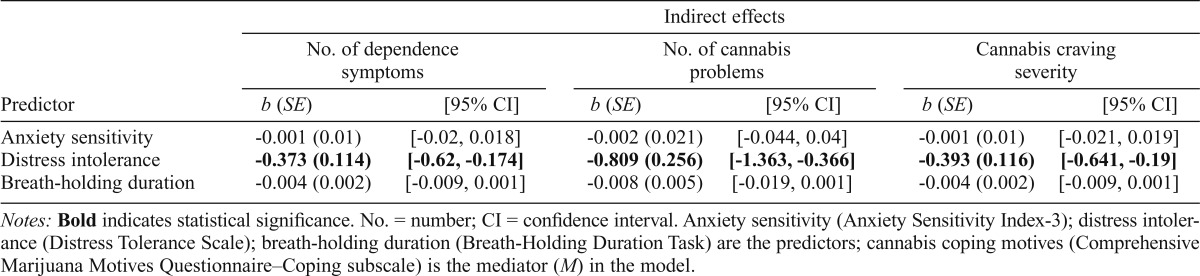
Mediation results
Next, a path model was constructed and examined in terms of its consistency with the theoretical model (Figure 1). In the proposed path model, model fit was good, χ2(1) = 1.43, p = .232; CFI = .99; RMSEA = .07. Informed by significant bivariate intercorrelations, the ASI-3 and DTS were allowed to correlate, and the DTS and breath-holding duration were allowed to correlate. Additionally, all three criterion variables were interrelated, and thus were allowed to correlate in the path model. Results are presented in Table 2. The ASI-3 and breath-holding duration were significantly associated with cannabis problems; the DTS was not uniquely linked to any cannabis outcomes. After accounting for correlations between predictors, only perceived distress intolerance (DTS) was significantly negatively associated with cannabis coping motives. Coping motives were significantly and positively associated with cannabis dependence symptoms, problems, and craving severity (ps < .001). The mediation (indirect) effects were examined using RMediation (Tofighi & MacKinnon, 2011) (Table 3). Results indicated that only the DTS significantly and negatively predicted the number of cannabis dependence symptoms, number of cannabis problems, and cannabis craving severity, which was accounted for by cannabis coping motives.
Table 2.
Results from path model
| “Path a” effect |
“Path c” effect |
|||
| Predictor | b (SE) | No. of dependence symptoms b (SE) | No. of cannabis problems b (SE) | Cannabis craving severity b (SE) |
| Anxiety sensitivity | -0.001 (0.013) | 0.012(0.019) | 0.156 (0.043)*** | -0.033 (0.018) |
| Distress intolerance | -0.512 (0.115)*** | -0.110(0.188) | 0.175 (0.436) | -0.207 (0.180) |
| Breath-holding duration | -0.005 (0.003) | -0.003 (0.005) | 0.023 (0.011)* | 0.005 (0.005) |
| “Path b” effect | ||||
| Coping motives | – | 0.729 (0.148)*** | 1.581 (0.343)*** | 0.768 (0.142)*** |
Notes: No. = number. Anxiety sensitivity (Anxiety Sensitivity Index-3); distress intolerance (Distress Tolerance Scale); breath-holding duration (Breath-Holding Duration Task) are the predictors; coping motives (Comprehensive Marijuana Motives Questionnaire-Coping subscale) is the mediator (M). Path a = effect of X on M; Path c = effect of X on Y; Path b = effect of M on Y.
p < .05;
p < .001.
Table 3.
Indirect effects via cannabis coping motives
| Indirect effects |
||||||
| No. of dependence symptoms |
No. of cannabis problems |
Cannabis craving severity |
||||
| Predictor | b (SE) | [95% CI] | b (SE) | [95% CI] | b (SE) | [95% CI] |
| Anxiety sensitivity | -0.001 (0.01) | [-0.02, 0.018] | -0.002 (0.021) | [-0.044, 0.04] | -0.001 (0.01) | [-0.021, 0.019] |
| Distress intolerance | -0.373 (0.114) | [-0.62, -0.174] | -0.809 (0.256) | [-1.363, -0.366] | -0.393 (0.116) | [-0.641, -0.19] |
| Breath-holding duration | -0.004 (0.002) | [-0.009, 0.001] | -0.008 (0.005) | [-0.019, 0.001] | -0.004 (0.002) | [-0.009, 0.001] |
Notes: Bold indicates statistical significance. No. = number; CI = confidence interval. Anxiety sensitivity (Anxiety Sensitivity Index-3); distress intolerance (Distress Tolerance Scale); breath-holding duration (Breath-Holding Duration Task) are the predictors; cannabis coping motives (Comprehensive Marijuana Motives Questionnaire-Coping subscale) is the mediator (M) in the model.
Discussion
The current study aimed to examine the unique predictive effects of anxiety sensitivity, perceived distress intolerance (of psychological distress), and behavioral distress intolerance (of respiratory distress) in terms of cannabis-related outcomes, and the mediating role of cannabis coping motives. Findings indicated that, at a bivariate level, all three indices of emotional vulnerability (ASI-3, DTS, and breath-holding duration) were associated with cannabis coping motives. This set of results replicates the findings from other studies that have documented the association between anxiety sensitivity and perceived distress intolerance in terms of cannabis coping motives among cannabis users (Bujarski et al., 2012; Johnson et al., 2010; Zvolensky et al., 2009). Moreover, the current findings are novel given that they implicate objectively measured distress intolerance (of respiratory distress) in terms of cannabis coping motives, at least at the bivariate level.
Extending prior work (Bujarski et al., 2012; Zvolensky et al., 2009), current findings indicated that only perceived distress intolerance was uniquely associated with overall stronger urges to use cannabis to cope with negative emotions, which was associated with having more cannabis dependence and problems, based on the short-term tension reduction effect of cannabis (Metrik et al., 2011). Moreover, the current study included an assessment of craving (consistent with the DSM-5 diagnostic system) in addition to the current DSM-IV diagnostic assessment of cannabis dependence, which omits the craving criterion. Thus, the present findings increase generalizability of perceived distress intolerance as a predictor of a broader categorization of cannabis use disorder, consistent with DSM-5 (American Psychiatric Association, 2013).
The current findings inform motivational-based mechanisms related to problematic cannabis use. Individuals’ perception of their own limited capacity to withstand distress may be a cognitive risk factor for problematic cannabis use, driven by the tendency to rely on cannabis to eliminate distress. The tendency to be fearful of the consequences of somatic sensations (anxiety sensitivity) appears to be related to coping-motivated cannabis use, most likely for attenuation of fears about anticipated physical states, although it may be a less prominent risk factor for maladaptive cannabis use. Importantly, perceived distress intolerance and anxiety sensitivity are cognitive processes that influence how individuals interpret distress states and thus precede actual attempts to regulate or cope with distress. In contrast, one’s behavioral ability to withstand distress is reflective of response-focused emotion regulation. Thus, behavioral measurement of distress tolerance, or persistence in a distressing task (such as breath-holding), may be useful in assessingwhether changes in perception to distress intolerance influence actual capacity to withstand in vivo distress (Farris & Metrik, 2016). It would be important to consider a range of behavioral measures of distress intolerance—including those that tap intolerance of mental distress (e.g., frustration) and alternative physical distress states (e.g., pain)—in addition to respiratory distress, as examined in the current study.
Several study limitations warrant discussion. First, the data used were cross-sectional in nature, which limits hypothesis testing related to causality. For example, in the current data, it is unknown how problematic cannabis use may have served to promote or exacerbate anxiety sensitivity and distress intolerance. Future prospective modeling is needed to directly empirically evaluate the extent to which perceived distress intolerance may further maintain problematic patterns of cannabis use. Second, because of the genetic aims of the parent study, the current sample included participants who were exclusively White, thereby potentially limiting the generalizability of the current findings. Third, individuals were excluded from the study on the basis of self-reported inability to abstain from using cannabis for at least 24 hours without experiencing withdrawal symptoms. Specifically, potential participants were asked, “Do you think you can avoid using cannabis for 24 hours without feeling very anxious or like you can’t sit still, or feeling very irritable or angry?” It is possible that participants who subjectively perceived that they were unable to handle distress associated with cannabis eprivation and experience strong withdrawal symptoms (including craving) were not sampled here. However, it is worth noting the variability in self-reported cannabis craving (observed range was not restricted).
Fourth, cannabis users were excluded on the basis of having a past-month affective or panic disorder based on the experimental procedures of the parent study, which included cannabis administration (Metrik et al., 2015). This exclusion criterion may have resulted in lower overall average scores on the ASI-3 and a somewhat restricted range (observed range: 0–30). Thus, although the current findings may represent a more conservative test of the nature of emotional vulnerability and cannabis use, these findings suggest that even among frequent cannabis users without affective/panic psychopathology, perceived distress intolerance is linked (at least cross-sectionally) to dependence processes. Last, there are many potential ways to further extend this line of work. For example, it would be meaningful to explore the intricacies of perceived distress intolerance (per the DTS subfactors; Simons & Gaher, 2005) and anxiety sensitivity (per ASI-3 subfactors; Taylor et al., 2007) in terms of coping motives for cannabis use, or alternative motivational processes underlying cannabis use.
Collectively, these data underscore the importance of clinically assessing and addressing individuals’ perception of their ability to tolerate psychological distress, and targeting beliefs about one’s ability to cope with distress states—presumably by increasing access to and use of alternative coping skills (Buckner et al., 2014, 2016). For example, a distress tolerance treatment program has been developed for substance users to specifically increase skills to tolerate distress and control behaviors in the context of emotional distress (Bornovalova et al., 2012), which is largely informed by Dialectical Behavioral Therapy (DBT; Linehan, 1993; Linehan et al., 1999) and Acceptance and Commitment Therapy (ACT; Hayes et al., 1999). In addition, teaching coping skills such as urge surfing could be helpful for cannabis users not only to develop increased awareness of bodily sensations experienced when having cravings but also to decrease perceptions of intolerable distress. Importantly, teaching distress tolerance skills alone (to increase behavioral capacity to withstand distress) may be insufficient if perceptions and beliefs about one’s inability to tolerate distress are not addressed.
Cannabis users could also benefit from psychoeducation regarding the cyclical nature of distress and cannabis use, and how low-effort escape behaviors (like cannabis use) presumably encourage further reliance on cannabis and can increase anxiety and affective problems in the long run. Increasing individuals’ willingness and confidence in their ability to tolerate and experience discomfort, manage craving, and develop alternative adaptive coping skills (Baer et al., 1999; Litt et al., 2008) may attenuate reliance on cannabis, reduce the intensity of cannabis use disorder symptoms, and facilitate cannabis cessation efforts.
Acknowledgments
All authors contributed in a significant way to this article and have all read and approved the final manuscript. The authors have no financial relationship with the study sponsor and no conflicts of interest to disclose. The authors gratefully acknowledge Suzanne Sales, Timothy Souza, Samuel Fricchione, Netesha Reid, and Amy Mochel for their contributions to the parent project.
Footnotes
This study was funded by National Institute on Drug Abuse Grant R03 DA027484, awarded to Jane Metrik and Valerie S. Knopik. Marcel O. Bonn-Miller’s work on this project was supported by the Veterans Affairs Center of Excellence in Substance Abuse Treatment and Education. Samantha G. Farris is supported by a pre-doctoral National Research Service Award from the National Institute on Drug Abuse (F31-DA035564-03). The funding sources had no role other than financial support. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs.
Cue reactivity was completed in a separate visit, and indeed cue exposure significantly increased scores on the MCQ following presentation of cannabis vs. neutral cues (Metrik et al., 2015). Of note, average MCQ scores following the presentation of neutral cues were identical to the MCQ scores at baseline (following 15-hour deprivation).
The inability to avoid using cannabis without feeling anxious in 24 hours accounted for 11.5% of all telephone screens; thus, this was not a prominent reason for exclusion. We believe this further clarifies that the sample was still representative of cannabis users who clearly endorse withdrawal symptoms even after 15 hours of cannabis deprivation.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: Author; 1994. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Arlington, VA: Author; 2013. [Google Scholar]
- Arbuckle J. L. IBM SPSS Amos 22.0 user's guide. Chicago, IL: IBM Corporation; 2013. [Google Scholar]
- Asmundson G. G., Stein M. B. Triggering the false suffocation alarm in panic disorder patients by using a voluntary breath-holding procedure. American Journal of Psychiatry. 1994;151:264–266. doi: 10.1176/ajp.151.2.264. [DOI] [PubMed] [Google Scholar]
- Baer J. S., Kivlahan D. R., Donovan D. M. Integrating skills training and motivational therapies. Implications for the treatment of substance dependence. Journal of Substance Abuse Treatment. 1999;17:15–23. doi: 10.1016/s0740-5472(98)00072-5. doi:10.1016/S0740-5472(98)00072-5. [DOI] [PubMed] [Google Scholar]
- Baker T. B., Piper M. E., McCarthy D. E., Majeskie M. R., Fiore M. C. Addiction motivation reformulated: An affective processing model of negative reinforcement. Psychological Review. 2004;111:33–51. doi: 10.1037/0033-295X.111.1.33. doi:10.1037/0033-295X.111.1.33. [DOI] [PubMed] [Google Scholar]
- Bernstein A., Marshall E. C., Zvolensky M. J. Multi-method evaluation of distress tolerance measures and construct(s): Concurrent relations to mood and anxiety psychopathology and quality of life. Journal of Experimental Psychopathology. 2011;2:386–399. [Google Scholar]
- Bernstein A., Zvolensky M. J., Vujanovic A. A., Moos R. Integrating anxiety sensitivity, distress tolerance, and discomfort intolerance: A hierarchical model of affect sensitivity and tolerance. Behavior Therapy. 2009;40:291–301. doi: 10.1016/j.beth.2008.08.001. doi:10.1016/j.beth.2008.08.001. [DOI] [PubMed] [Google Scholar]
- Bonn-Miller M. O., Zvolensky M. J., Bernstein A. Marijuana use motives: Concurrent relations to frequency of past 30-day use and anxiety sensitivity among young adult marijuana smokers. Addictive Behaviors. 2007;32:49–62. doi: 10.1016/j.addbeh.2006.03.018. doi:10.1016/j.addbeh.2006.03.018. [DOI] [PubMed] [Google Scholar]
- Bonn-Miller M. O., Zvolensky M. J., Marshall E. C., Bernstein A. Incremental validity of anxiety sensitivity in relation to marijuana withdrawal symptoms. Addictive Behaviors. 2007;32:1843–1851. doi: 10.1016/j.addbeh.2006.12.016. doi:10.1016/j.addbeh.2006.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bornovalova M. A., Gratz K. L., Daughters S. B., Hunt E. D., Lejuez C. W. Initial RCT of a distress tolerance treatment for individuals with substance use disorders. Drug and Alcohol Dependence. 2012;122:70–76. doi: 10.1016/j.drugalcdep.2011.09.012. doi:10.1016/j.drugalcdep.2011.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brandon T. H., Herzog T. A., Juliano L. M., Irvin J. E., Lazev A. B., Simmons V. N. Pretreatment task persistence predicts smoking cessation outcome. Journal of Abnormal Psychology. 2003;112:448–456. doi: 10.1037/0021-843x.112.3.448. doi:10.1037/0021-843X.112.3.448. [DOI] [PubMed] [Google Scholar]
- Brown R. A., Lejuez C. W., Kahler C. W., Strong D. R., Zvolensky M. J. Distress tolerance and early smoking lapse. Clinical Psychology Review. 2005;25:713–733. doi: 10.1016/j.cpr.2005.05.003. doi:10.1016/j.cpr.2005.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown R. A., Lejuez C. W., Strong D. R., Kahler C. W., Zvolensky M. J., Carpenter L. L., Price L. H. A prospective examination of distress tolerance and early smoking lapse in adult self-quitters. Nicotine & Tobacco Research. 2009;11:493–502. doi: 10.1093/ntr/ntp041. doi:10.1093/ntr/ntp041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown R. A., Palm K. M., Strong D. R., Lejuez C. W., Kahler C. W., Zvolensky M. J., Gifford E. V. Distress tolerance treatment for early-lapse smokers: Rationale, program description, and preliminary findings. Behavior Modification. 2008;32:302–332. doi: 10.1177/0145445507309024. doi:10.1177/0145445507309024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner J. D., Ecker A. H., Beighley J. S., Zvolensky M. J., Schmidt N. B., Shah S. M., Carroll K. M. Integrated cognitive behavioral therapy for comorbid cannabis use and anxiety disorders. Clinical Case Studies. 2016;15:68–83. doi: 10.1177/1534650115590857. doi:10.1177/1534650115590857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner J. D., Keough M. E., Schmidt N. B. Problematic alcohol and cannabis use among young adults: The roles of depression and discomfort and distress tolerance. Addictive Behaviors. 2007;32:1957–1963. doi: 10.1016/j.addbeh.2006.12.019. doi:10.1016/j.addbeh.2006.12.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner J. D., Zvolensky M. J., Schmidt N. B. Cannabis-related impairment and social anxiety: The roles of gender and cannabis use motives. Addictive Behaviors. 2012;37:1294–1297. doi: 10.1016/j.addbeh.2012.06.013. doi:10.1016/j.addbeh.2012.06.013. [DOI] [PubMed] [Google Scholar]
- Buckner J. D., Zvolensky M. J., Schmidt N. B., Carroll K. M., Schatschneider C., Crapanzano K. Integrated cognitive behavioral therapy for cannabis use and anxiety disorders: Rationale and development. Addictive Behaviors. 2014;39:495–496. doi: 10.1016/j.addbeh.2013.10.023. doi:10.1016/j.addbeh.2013.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner J. D., Zvolensky M. J., Smits J. A., Norton P. J., Crosby R. D., Wonderlich S. A., Schmidt N. B. Anxiety sensitivity and marijuana use: An analysis from ecological momentary assessment. Depression and Anxiety. 2011;28:420–426. doi: 10.1002/da.20816. doi:10.1002/da.20816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Budney A. J., Hughes J. R., Moore B. A., Vandrey R. Review of the validity and significance of cannabis withdrawal syndrome. American Journal of Psychiatry. 2004;161:967–977. doi: 10.1176/appi.ajp.161.11.1967. [DOI] [PubMed] [Google Scholar]
- Budney A. J., Moore B. A., Vandrey R. G., Hughes J. R. The time course and significance of cannabis withdrawal. Journal of Abnormal Psychology. 2003;112:393–402. doi: 10.1037/0021-843x.112.3.393. doi:10.1037/0021-843X.112.3.393. [DOI] [PubMed] [Google Scholar]
- Bujarski S. J., Norberg M. M., Copeland J. The association between distress tolerance and cannabis use-related problems: The mediating and moderating roles of coping motives and gender. Addictive Behaviors. 2012;37:1181–1184. doi: 10.1016/j.addbeh.2012.05.014. doi:10.1016/j.addbeh.2012.05.014. [DOI] [PubMed] [Google Scholar]
- Comeau N., Stewart S. H., Loba P. The relations of trait anxiety, anxiety sensitivity, and sensation seeking to adolescents’ motivations for alcohol, cigarette, and marijuana use. Addictive Behaviors. 2001;26:803–825. doi: 10.1016/s0306-4603(01)00238-6. doi:10.1016/S0306-4603(01)00238-6. [DOI] [PubMed] [Google Scholar]
- Conway K. P., Compton W., Stinson F. S., Grant B. F. Lifetime comorbidity of DSM-IV mood and anxiety disorders and specific drug use disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry. 2006;67:247–258. doi: 10.4088/jcp.v67n0211. doi:10.4088/JCP.v67n0211. [DOI] [PubMed] [Google Scholar]
- Cooper Z. D., Haney M. Comparison of subjective, pharmacokinetic, and physiological effects of marijuana smoked as joints and blunts. Drug and Alcohol Dependence. 2009;103:107–113. doi: 10.1016/j.drugalcdep.2009.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cougle J. R., Bonn-Miller M. O., Vujanovic A. A., Zvolensky M. J., Hawkins K. A. Posttraumatic stress disorder and cannabis use in a nationally representative sample. Psychology of Addictive Behaviors. 2011;25:554–558. doi: 10.1037/a0023076. doi:10.1037/a0023076. [DOI] [PubMed] [Google Scholar]
- Dvorak R. D., Day A. M. Marijuana and self-regulation: Examining likelihood and intensity of use and problems. Addictive Behaviors. 2014;39:709–712. doi: 10.1016/j.addbeh.2013.11.001. doi:10.1016/j.addbeh.2013.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farris S. G., Metrik J. Acute effects of cannabis on breath-holding duration. Experimental and Clinical Psychopharmacology. 2016;24:305–312. doi: 10.1037/pha0000075. doi: 10.1037/pha0000075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First M. B., Spitzer R. L., Gibbon M., Williams J. B. W. Structured Clinical Interview for DSMIV-TR Axis I Disorders, Research Version, Non-patient Edition (SCID-I/NP) New York, NY: Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- Hajek P., Belcher M., Stapleton J. Breath-holding endurance as a predictor of success in smoking cessation. Addictive Behaviors. 1987;12:285–288. doi: 10.1016/0306-4603(87)90041-4. doi:10.1016/0306-4603(87)90041-4. [DOI] [PubMed] [Google Scholar]
- Haney M., Ward A. S., Comer S. D., Foltin R. W., Fischman M. W. Abstinence symptoms following smoked marijuana in humans. Psychopharmacology. 1999;141:395–404. doi: 10.1007/s002130050849. doi:10.1007/s002130050849. [DOI] [PubMed] [Google Scholar]
- Hasan N. S., Babson K. A., Banducci A. N., Bonn-Miller M. O. The prospective effects of perceived and laboratory indices of distress tolerance on cannabis use following a self-guided quit attempt. Psychology of Addictive Behaviors. 2015;29:933–940. doi: 10.1037/adb0000132. doi:10.1037/adb0000132. [DOI] [PubMed] [Google Scholar]
- Hayes S. C., Strosahl K. D., Wilson K. G. Acceptance and commitment therapy: An experiential approach to behavior change. New York, NY: Guilford Press; 1999. [Google Scholar]
- Hogan J., Farris S. G., Brandt C. P., Schmidt N. B., Zvolensky M. J. Predictors of breath-holding duration among treatment-seeking tobacco users. Journal of Substance Use. 2015;20:27–32. doi:10.3109/14659891.2014.884176. [Google Scholar]
- Howell A. N., Leyro T. M., Hogan J., Buckner J. D., Zvolensky M. J. Anxiety sensitivity, distress tolerance, and discomfort intolerance in relation to coping and conformity motives for alcohol use and alcohol use problems among young adult drinkers. Addictive Behaviors. 2010;35:1144–1147. doi: 10.1016/j.addbeh.2010.07.003. doi:10.1016/j.addbeh.2010.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson K., Mullin J. L., Marshall E. C., Bonn-Miller M. O., Zvolensky M. Exploring the mediational role of coping motives for marijuana use in terms of the relation between anxiety sensitivity and marijuana dependence. American Journal on Addictions. 2010;19:277–282. doi: 10.1111/j.1521-0391.2010.00041.x. doi:10.1111/j.1521-0391.2010.00041.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kassel J. D., Stroud L. R., Paronis C. A. Smoking, stress, and negative affect: Correlation, causation, and context across stages of smoking. Psychological Bulletin. 2003;129:270–304. doi: 10.1037/0033-2909.129.2.270. doi:10.1037/0033-2909.129.2.270. [DOI] [PubMed] [Google Scholar]
- Kassel J. D., Unrod M. Smoking, anxiety, and attention: Support for the role of nicotine in attentionally mediated anxiolysis. Journal of Abnormal Psychology. 2000;109:161–166. doi: 10.1037//0021-843x.109.1.161. doi:10.1037/0021-843X.109.1.161. [DOI] [PubMed] [Google Scholar]
- Kline R. B. Principles and practice of structural equation modeling (3rd ed.) New York, NY: Guilford Press; 2011. [Google Scholar]
- Lee C. M., Neighbors C., Hendershot C. S., Grossbard J. R. Development and preliminary validation of a comprehensive marijuana motives questionnaire. Journal of Studies on Alcohol and Drugs. 2009;70:279–287. doi: 10.15288/jsad.2009.70.279. doi:10.15288/jsad.2009.70.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee C. M., Neighbors C., Woods B. A. Marijuana motives: Young adults’ reasons for using marijuana. Addictive Behaviors. 2007;32:1384–1394. doi: 10.1016/j.addbeh.2006.09.010. doi:10.1016/j.addbeh.2006.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leyro T. M., Zvolensky M. J., Bernstein A. Distress tolerance and psychopathological symptoms and disorders: A review of the empirical literature among adults. Psychological Bulletin. 2010;136:576–600. doi: 10.1037/a0019712. doi:10.1037/a0019712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linehan M. M. Cognitive behavioral treatment of borderline personality disorder. New York, NY: Guilford Press; 1993. [Google Scholar]
- Linehan M. M., Schmidt H., III, Dimeff L. A., Craft J. C., Kanter J., Comtois K. A. Dialectical behavior therapy for patients with borderline personality disorder and drug-dependence. American Journal on Addictions. 1999;8:279–292. doi: 10.1080/105504999305686. doi:10.1080/105504999305686. [DOI] [PubMed] [Google Scholar]
- Litt M. D., Kadden R. M., Kabela-Cormier E., Petry N. M. Coping skills training and contingency management treatments for marijuana dependence: Exploring mechanisms of behavior change. Addiction. 2008;103:638–648. doi: 10.1111/j.1360-0443.2008.02137.x. doi:10.1111/j.1360-0443.2008.02137.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarthy D. E., Curtin J. J., Piper M. E., Baker T. B. Negative reinforcement: Possible clinical implications of an integrative model. In: Kassel J. D., editor. Substance abuse and emotion. Washington, DC: American Psychological Association; 2010. pp. 15–42. [Google Scholar]
- McDonald J., Schleifer L., Richards J. B., de Wit H. Effects of THC on behavioral measures of impulsivity in humans. Neuropsychopharmacology. 2003;28:1356–1365. doi: 10.1038/sj.npp.1300176. doi:10.1038/sj.npp.1300176. [DOI] [PubMed] [Google Scholar]
- McHugh R. K., Otto M. W. Refining the measurement of distress intolerance. Behavior Therapy. 2012;43:641–651. doi: 10.1016/j.beth.2011.12.001. doi:10.1016/j.beth.2011.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metrik J., Aston E. R., Kahler C. W., Rohsenow D. J., McGeary J. E., Knopik V S. Marijuana’s acute effects on cognitive bias for affective and marijuana cues. Experimental and Clinical Psychopharmacology. 2015;23:339–350. doi: 10.1037/pha0000030. doi:10.1037/pha0000030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metrik J., Jackson K., Bassett S., Zvolensky M. J., Seal K., Borsari B. E. The mediating roles of coping, sleep, and anxiety motives in cannabis use and problems among returning veterans with PTSD and MDD. Psychology of Addictive Behaviors. in press doi: 10.1037/adb0000210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metrik J., Kahler C. W., McGeary J. E., Monti P. M., Rohsenow D. J. Acute effects of marijuana smoking on negative and positive affect. Journal of Cognitive Psychotherapy. 2011;25:31–46. doi: 10.1891/0889-8391.25.1.31. doi:10.1891/0889-8391.25.1.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell H., Zvolensky M. J., Marshall E. C., Bonn-Miller M. O., Vujanovic A. A. Incremental validity of coping-oriented marijuana use motives in the prediction of affect-based psychological vulnerability. Journal of Psychopathology and Behavioral Assessment. 2007;29:277–288. doi:10.1007/s10862-007-9047-z. [Google Scholar]
- Moitra E., Christopher P. P., Anderson B. J., Stein M. D. Coping-motivated marijuana use correlates with DSM-5 cannabis use disorder and psychological distress among emerging adults. Psychology of Addictive Behaviors. 2015;29:627–632. doi: 10.1037/adb0000083. doi:10.1037/adb0000083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naragon-Gainey K. Meta-analysis of the relations of anxiety sensitivity to the depressive and anxiety disorders. Psychological Bulletin. 2010;136:128–150. doi: 10.1037/a0018055. doi:10.1037/a0018055. [DOI] [PubMed] [Google Scholar]
- Olatunji B. O., Wolitzky-Taylor K. B. Anxiety sensitivity and the anxiety disorders: A meta-analytic review and synthesis. Psychological Bulletin. 2009;135:974–999. doi: 10.1037/a0017428. doi:10.1037/a0017428. [DOI] [PubMed] [Google Scholar]
- Peters E. N., Nich C., Carroll K. M. Primary outcomes in two randomized controlled trials of treatments for cannabis use disorders. Drug and Alcohol Dependence. 2011;118:408–416. doi: 10.1016/j.drugalcdep.2011.04.021. doi:10.1016/j.drugalcdep.2011.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phan K. L., Angstadt M., Golden J., Onyewuenyi I., Popovska A., de Wit H. Cannabinoid modulation of amygdala reactivity to social signals of threat in humans. Journal of Neuroscience. 2008;28:2313–2319. doi: 10.1523/JNEUROSCI.5603-07.2008. doi:10.1523/JNEUROSCI.5603-07.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Potter C. M., Vujanovic A. A., Marshall-Berenz E. C., Bernstein A., Bonn-Miller M. O. Posttraumatic stress and marijuana use coping motives: The mediating role of distress tolerance. Journal of Anxiety Disorders. 2011;25:437–443. doi: 10.1016/j.janxdis.2010.11.007. doi:10.1016/j.janxdis.2010.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reiss S., Peterson R. A., Gursky D. M., McNally R. J. Anxiety sensitivity, anxiety frequency and the prediction of fearfulness. Behaviour Research and Therapy. 1986;24:1–8. doi: 10.1016/0005-7967(86)90143-9. doi:10.1016/0005-7967(86)90143-9. [DOI] [PubMed] [Google Scholar]
- Simons J. S., Gaher R. M. The Distress Tolerance Scale: Development and validation of a self-report measure. Motivation and Emotion. 2005;29:83–102. doi:10.1007/s11031-005-7955-3. [Google Scholar]
- Sobell L. C., Sobell M. B. Timeline Followback user’s guide: A calendar method for assessing alcohol and drug use. Toronto, Ontario: Addiction Research Foundation; 1996. [Google Scholar]
- Stephens R. S., Roffman R. A., Curtin L. Comparison of extended versus brief treatments for marijuana use. Journal of Consulting and Clinical Psychology. 2000;68:898–908. doi:10.1037/0022-006X.68.5.898. [PubMed] [Google Scholar]
- Stinson F. S., Ruan W. J., Pickering R., Grant B. F. Cannabis use disorders in the USA: Prevalence, correlates and co-morbidity. Psychological Medicine. 2006;36:1447–1460. doi: 10.1017/S0033291706008361. doi:10.1017/S0033291706008361. [DOI] [PubMed] [Google Scholar]
- Taylor S., Zvolensky M. J., Cox B. J., Deacon B., Heimberg R. G., Ledley D. R., Cardenas S. J. Robust dimensions of anxiety sensitivity: Development and initial validation of the Anxiety Sensitivity Index-3. Psychological Assessment. 2007;19:176–188. doi: 10.1037/1040-3590.19.2.176. doi:10.1037/1040-3590.19.2.176. [DOI] [PubMed] [Google Scholar]
- Tofighi D., MacKinnon D. P. RMediation: An R package for mediation analysis confidence intervals. Behavior Research Methods. 2011;43:692–700. doi: 10.3758/s13428-011-0076-x. doi:10.3758/s13428-011-0076-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tournier M., Sorbara F., Gindre C., Swendsen J. D., Verdoux H. Cannabis use and anxiety in daily life: A naturalistic investigation in a non-clinical population. Psychiatry Research. 2003;118:1–8. doi: 10.1016/s0165-1781(03)00052-0. doi:10.1016/S0165-1781(03)00052-0. [DOI] [PubMed] [Google Scholar]
- Tull M. T., Schulzinger D., Schmidt N. B., Zvolensky M. J., Lejuez C. W. Development and initial examination of a brief intervention for heightened anxiety sensitivity among heroin users. Behavior Modification. 2007;31:220–242. doi: 10.1177/0145445506297020. doi:10.1177/0145445506297020. [DOI] [PubMed] [Google Scholar]
- Vujanovic A. A., Bernstein A., Litz B. T. Traumatic stress. In: Zvolensky M. J., Bernstein A., Vujanovic A. A., editors. Distress tolerance. New York, NY: Guilford Press; 2011. [Google Scholar]
- Zvolensky M. J., Marshall E. C., Johnson K., Hogan J., Bernstein A., Bonn-Miller M. O. Relations between anxiety sensitivity, distress tolerance, and fear reactivity to bodily sensations to coping and conformity marijuana use motives among young adult marijuana users. Experimental and Clinical Psychopharmacology. 2009;17:31–42. doi: 10.1037/a0014961. doi:10.1037/a0014961. [DOI] [PMC free article] [PubMed] [Google Scholar]