Abstract
A 35-year-old non-HIV patient developed pulmonary cryptococcosis after the initiation of infliximab. He recovered by fluconazole treatment and completed the therapy for a total of 6 months. However, he experienced a relapse 16 months later during retreatment with infliximab, revealing an interesting clinical course contradicting retreatment. This case also represents the first case of relapsed pulmonary cryptococcosis suspected during treatment with a biologic agent. Both of these aspects generated important clinical questions about the length of pulmonary cryptococcosis treatment and the necessity of introducing a second prophylaxis for such patients.
Keywords: pulmonary cryptococcosis, relapse, infliximab, tumor necrosis factor α inhibitor, biological agents
Introduction
Patients with diseases, such as rheumatoid arthritis and other autoimmune conditions, have greatly benefited from treatment with biologic agents such as antitumor necrosis factor-alpha (anti-TNF-α) and interleukin-6 (IL-6) antagonists. These biologics, however, can trigger the development of certain infectious diseases such as deep-seated mycosis (1). Cryptococcosis, an important cause of mycosis, has high morbidity and mortality rates in immunocompromised patients. We previously reported a patient who developed pulmonary cryptococcosis during anti-TNF-α treatment (2). Because this patient developed pulmonary cryptococcosis again after the completion of 6 months of fluconazole (FLCZ) treatment and subsequent resumption of anti-TNF-α treatments, we herein present a follow-up case report describing this situation, which revealed an interesting clinical course contradicting retreatment.
Case Report
A 35-year-old man with Crohn's disease was referred to our respiratory department due to a high fever and the presence of an infiltrated pulmonary nodule after eight infusions of infliximab (IFX). Pulmonary cryptococcosis was diagnosed in this patient according to positive cryptococcal antigen test results (×16 and ×32) of the bronchoalveolar lavage fluid (BALF). He was subsequently treated with 400 mg/day oral FLCZ. The infiltration of the left lower lobe of the lung gradually improved and was nearly eliminated after 3 months of FLCZ treatment. IFX treatment was resumed 1 month after the initial FLCZ treatment to control the patient's Crohn's disease. He received FLCZ for 6 months, as we previously described (2). IFX therapy was continued once every 8 weeks, and prednisolone was adjusted to approximately 10 mg/day.
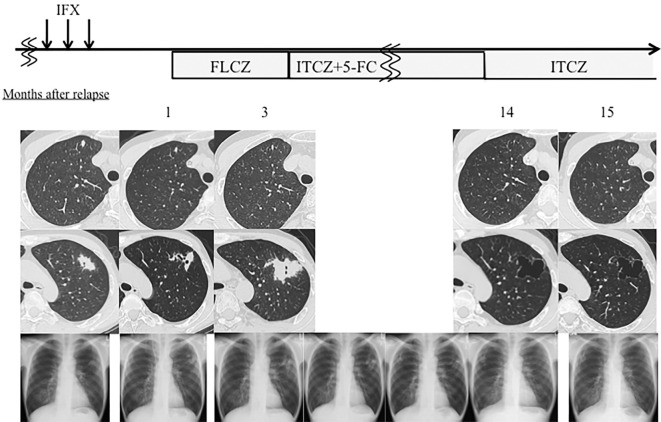
The patient, however, developed a high fever, resistance to β-lactam and levofloxacin antibiotics, general fatigue, and night sweats at 16 months after the completion of FLCZ treatment and 22 months after restarting IFX treatment. Chest radiography and computed tomography (CT) revealed a 3×2 cm mass-like region and a small nodule in the left and right upper lobes of the lung (Fig. 1). He had no symptoms indicating any type of central nervous system infection, such as a headache or consciousness disturbance. He also had no history of significant exposure to birds, including pigeons, or travel abroad around the time of the clinical progression or the onset of the first episode. Laboratory tests revealed a normal leukocyte count (4,300/mm3) and a slightly elevated C-reactive protein level (1.76 mg/dL). The test for serum cryptococcal antigen (Eiken, Tokyo, Japan) was negative, and the β-D-glucan assay level (Wako, Osaka, Japan) was below the cut-off value (3.2 pg/mL). Bronchoscopy with BALF was performed, and a transbronchial lung biopsy (TBLB) was obtained from the left upper lobe region for further examination. The culture and microscopic examinations of the BALF were also negative. BALF cytology revealed periodic acid-Schiff stain-positive bodies, phagocytized by macrophages, which was indicative of Cryptococcus spp. (Fig. 2). The cryptococcal antigen test of the BALF was positive (×2). A histological examination of the TBLB showed granulomatous regions in the lung parenchyma. These findings confirmed the diagnosis of pulmonary cryptococcosis, and retreatment with 300 mg/day oral FLCZ at our outpatient clinic was started. Discontinuation of IFX treatment followed. The mass-like region found in the left upper lobe of the lung, however, deteriorated 2 months after restarting FLCZ. A change to antifungal treatment of 200 mg/day itraconazole (ITCZ) combined with 3 g/day flucytosine was initiated. After the initiation of this treatment, the region of the left upper lobe gradually decreased in size, and finally diminished in size on chest CT performed 10 months after the relapse (Fig. 3). The patient is presently continuing ITCZ treatment, although at a reduced dose of 100 mg/day due to the development of mild liver dysfunction.
Figure 1.
Chest radiography and computed tomography (CT) on relapse. Chest CT shows a small nodule in the right upper lobe of the lung and a 3×2 cm mass-like region is observed on an air bronchogram.
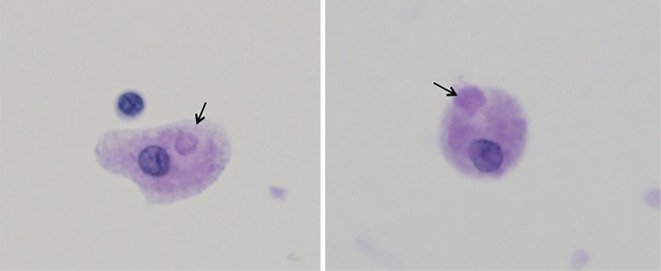
Figure 2.
Pictures of bronchoalveolar lavage fluid cytology (400×). Round bodies suspicious of Cryptococcus spp. phagocytized by macrophages can be seen on periodic acid-Schiff-stained sections.
Figure 3.
Clinical course after relapse. IFX: infliximab, FLCZ: fluconazole, ITCZ: itraconazole, 5-FC: flucytosine. Arrows show IFX administrations.
Discussion
As most cases of pulmonary cryptococcosis are believed to result from the reactivation of a dormant infection (3), we suspected that our case relapsed from a previous infection. However, we could not rule out the possibility of reinfection with other strainsof Cryptococcus because the sites of lung lesions differed between the two episodes. Although a genetic analysis of the pathogens is necessary to confirm whether this case was a relapse or a reinfection, unfortunately, we could not obtain pathogen specimens at both episodes.
According to the guidelines of the Infectious Diseases Society of America, primary antifungal cryptococcal prophylaxis for human immunodeficiency virus (HIV)-infected patients is not routinely recommended. If the availability of antiretroviral therapy (ART) is limited, and high levels of antiretroviral drug resistance and disease burden exist, then primary prophylaxis may be considered (3). Vibhagool et al. reported that secondary prophylaxis for cryptococcal meningitis could be safely discontinued in HIV-infected patients exhibiting sustained immunological and virologic responses to ART for >3 months after the completion of a minimum of 12 months of antifungal therapy (4). Six to 12 months of maintenance therapy is recommended (3) for organ transplant or non-HIV patients. On the other hand, in the Japanese non-HIV population, 6 months of azole treatment is suggested for pulmonary cryptococcosis patients with underlying diseases (5). Interestingly, our patient had completed 6 months of treatment with FLCZ and experienced relapse >1 year later.
In patients with pulmonary tuberculosis, which is also a subacute infectious disease often occurring in patients with impaired cellular immunity like cryptococcosis, secondary prophylaxis is not required even in patients receiving biological agents if standard tuberculosis therapy had been performed (6). On the other hand, no sufficient evidence about secondary prophylactic treatment in cryptococcosis patients with biological agents exists, likely because cryptococcosis is a relatively uncommon infectious disease. The evidence from this case suggests that it may be safe to continue antifungal agents in conjunction with the administration of biologic agents.
Another interesting point in our patient was the resistance to FLCZ treatment. We considered two hypotheses for this phenomenon. The first hypothesis is an acquired resistance to FLCZ; however, we could not confirm this, as our patient was culture negative. Bicanic et al. analyzed relapse cases of HIV-associated cryptococcal meningitis after FLCZ monotherapy and found that 76% of culture-positive relapse cases were associated with reduced susceptibility to FLCZ (7). The second hypothesis is a paradoxical reaction. The occurrence of paradoxical responses after the discontinuation of anti-TNF-α agents in patients with tuberculosis infection has been reported (8,9). Our patient's condition deteriorated between 2 and 3 months after the cessation of infliximab, which is consistent with a paradoxical reaction such as immune reconstitution inflammatory syndrome seen in HIV patients treated with ART (10,11).
To the best of our knowledge, this is the first case report describing a possible relapse of pulmonary cryptococcosis during treatment with a biological agent. An accumulation of such cases is necessary to determine the duration of antifungal treatment and the necessity for secondary prophylaxis in these cases.
The authors state that they have no Conflict of Interest (COI).
References
- 1. Morrison VA. Immunosuppression associated with novel chemotherapy agents and monoclonal antibodies. Clin Infect Dis 59 Suppl 5: S360-S364, 2014. [DOI] [PubMed] [Google Scholar]
- 2. Takazono T, Izumikawa K, Yoshioka S, et al. Possible pulmonary cryptococcosis in a patient with Crohn's disease during anti-tumor necrosis factor-alpha treatment: a case report and literature review. Jpn J Infect Dis 65: 461-464, 2012. [DOI] [PubMed] [Google Scholar]
- 3. Perfect JR, Dismukes WE, Dromer F, et al. Clinical practice guidelines for the management of cryptococcal disease: 2010 update by the Infectious Diseases Society of America. Clin Infect Dis 50: 291-322, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Vibhagool A, Sungkanuparph S, Mootsikapun P, et al. Discontinuation of secondary prophylaxis for cryptococcal meningitis in human immunodeficiency virus-infected patients treated with highly active antiretroviral therapy: a prospective, multicenter, randomized study. Clin Infect Dis 36: 1329-1331, 2003. [DOI] [PubMed] [Google Scholar]
- 5. Kohno S, Kakeya H, Izumikawa K, et al. Clinical features of pulmonary cryptococcosis in non-HIV patients in Japan. J Infect Chemother 21: 23-30, 2015. [DOI] [PubMed] [Google Scholar]
- 6. Singh JA, Furst DE, Bharat A, et al. 2012 update of the 2008 American College of Rheumatology recommendations for the use of disease-modifying antirheumatic drugs and biologic agents in the treatment of rheumatoid arthritis. Arthritis Care Res (Hoboken) 64: 625-639, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bicanic T, Harrison T, Niepieklo A, Dyakopu N, Meintjes G. Symptomatic relapse of HIV-associated cryptococcal meningitis after initial fluconazole monotherapy: the role of fluconazole resistance and immune reconstitution. Clin Infect Dis 43: 1069-1073, 2006. [DOI] [PubMed] [Google Scholar]
- 8. Garcia Vidal C, Rodriguez Fernández S, Martínez Lacasa J, et al. Paradoxical response to antituberculous therapy in infliximab-treated patients with disseminated tuberculosis. Clin Infect Dis 40: 756-759, 2005. [DOI] [PubMed] [Google Scholar]
- 9. Moureau C, Pothen L, Wilmes D, Yombi JC, Coche E, Hainaut P. Paradoxical response to tuberculosis treatment in a patient receiving tumor necrosis factor-alpha antagonist. Am J Med 125: e9-e10, 2012. [DOI] [PubMed] [Google Scholar]
- 10. Hirsch HH, Kaufmann G, Sendi P, Battegay M. Immune reconstitution in HIV-infected patients. Clin Infect Dis 38: 1159-1166, 2004. [DOI] [PubMed] [Google Scholar]
- 11. Shelburne SA 3rd, Darcourt J, White AC Jr, et al. The role of immune reconstitution inflammatory syndrome in AIDS-related Cryptococcus neoformans disease in the era of highly active antiretroviral therapy. Clin Infect Dis 40: 1049-1052, 2005. [DOI] [PubMed] [Google Scholar]