Abstract
Objective
Given that aging is associated with higher risk of cognitive decline and dementia, improving early detection of cognitive impairment has become a research and clinical priority. The Montreal Cognitive Assessment (MoCA) is a screening instrument used to assess different aspects of cognition. Despite its widespread use, norms adjusted to the sociodemographics of Quebec-French people are not yet available. Such norms are however important because performance on neuropsychological tests varies according to sociodemographic variables including age, sex, and education. As such, the present study aimed to establish normative data for the MoCA in middle-aged and elderly Quebec-French population.
Method
For that purpose, 1,019 community-dwelling older adults aged between 41 and 98 were recruited. Participants from 12 recruiting sites completed the MoCA. Regression-based normative data were produced and cross-validated with a validation sample (n = 200).
Results
Regression analyses indicated that older age, lower education level, and male sex were associated with poorer MoCA scores. The best predictive model included age (p < .001), education (p < .001), sex (p < .001), and a quadratic term for education (education X education; p < .001). This model explained a significant amount of variance of the MoCA score (p < .001, R2 = 0.26). A regression equation to calculate Z scores is presented.
Conclusions
This study provides normative data for the MoCA test in the middle-aged and elderly French-Quebec people. These data will facilitate more accurate detection and follow-up of the risk of cognitive impairment in this population, taking into account culture, age, education, and sex.
Keywords: Cognitive screening, Cognition, Neuropsychology, Montreal Cognitive Assessment, Aging, Norms
Introduction
The number of individuals aged 60 years or over is expected to at least double by 2,050, reaching approximately 2 billion older individuals worldwide (United Nations, 2013). This demographic trend has important economic, political, and societal implications. In particular, the number of individuals with dementia worldwide is estimated to double every 20 years, from 35.6 million in 2010, to 65.7 million in 2030, to 115.4 million in 2,050 (Prince et al., 2013). Given that aging is the most important risk factor for cognitive decline, detection of cognitive impairment in at-risk middle-aged and elderly individuals has become a research and clinical priority. Moreover, early identification of prodromal dementia is essential in order to detect individuals in which further cognitive decline can be prevented or postponed using early interventions or treatments (Alzheimer's Disease International, 2009).
The Montreal Cognitive Assessment (MoCA; Nasreddine et al., 2005) is a widely used cognitive screening tool that was originally designed for detection of mild cognitive impairment (MCI), a clinical state generally defined as the prodromal stage of several dementias depending on the cognitive impairment observed (Petersen, 2004), and more specifically a prodromal stage of Alzheimer's Disease when mild amnesia is observed (Albert et al., 2011). This test has proved to be sensitive to mild cognitive deficits and to predict future cognitive decline in several cognitively impaired states, including Alzheimer's disease and dementias (see Davis et al., 2015 for complete review), Parkinson's disease (Gill, Freshman, Blender & Ravina, 2008), chronic obstructive pulmonary disease (Villeneuve et al., 2012), rapid eye movement sleep behavior disorder (Gagnon, Postuma, Joncas, Desjardins & Latreille, 2010), Huntington's disease (Mickes et al., 2010; Videnovic et al., 2010), cerebrovascular diseases (Cameron, Ski & Thompson, 2012; Cumming, Bernhardt & Linden, 2011; Pendlebury, Cuthbertson, Welch, Mehta & Rothwell, 2010; Popovic, Seric & Demarin, 2007; Schweizer, Al-Khindi & Macdonald, 2012), human immunodeficiency virus (Overton et al., 2013), traumatic brain injury (de Guise et al., 2013), and cancer (Olson et al., 2011).
Several studies across countries and languages have shown that cognitive performance is influenced by sociodemographic variables such as age, education, and sex. This also applies to the MoCA, as seen in several normative studies in various countries, including Portugal (Freitas, Simoes, Alves & Santana, 2011), Ireland (Kenny et al., 2013), Italy (Conti, Bonazzi, Laiacona, Masina & Coralli, 2015; Santangelo et al., 2015), Japan (Narazaki et al., 2013), China (Lu et al., 2011), Singapore (Ng et al., 2015), and the United States (Malek-Ahmadi et al., 2015; Rossetti, Lacritz, Cullum & Weiner, 2011). According to previous normative studies, two factors—age and education —contribute to explaining up to 49% of the variance in MoCA scores (Freitas et al., 2011). Some studies have also indicated that sex may affect performance on cognitive screening tests, but it has rarely been the case with the MoCA (Conti et al., 2015; Freitas et al., 2011; Kenny et al., 2013; Malek-Ahmadi et al., 2015; Narazaki et al., 2013; Ng et al., 2015; Rossetti et al., 2011; Santangelo et al., 2015). Only one population-based study in Chinese elders found that sex was associated with MoCA test performance, but only in individuals with less than 5 years of education (Lu et al., 2011). Therefore, normative data adjusted for individuals’ sociodemographic characteristics are important to support the clinical use of the MoCA.
Local norms can also be more rigorous than non-cultural specific norms to identify cognitive difficulties in older adults (Arsenault-Lapierre et al., 2011). Indeed, in addition to the influence sociodemographic variables, many subtests of the MoCA require language and semantic treatment of information, such as denomination, verbal episodic memory, repetition, and abstraction. It is well established that performance on such tasks is influenced by psycholinguistic factors (e.g., word frequency or familiarity). It is also established that the psycholinguistic characteristics of a given concept vary cultures and languages. It is thus crucial to develop culturally- and linguistically-adapted norms to the reference population in order to maximize accuracy in the detection of cognitive impairments.
Several methods have been used to produce normative data for cognitive tests and among them is the use of percentiles, Z scores based on means and standard deviations (SD), and Z scores based on a regression model. The regression method has many advantages over the other two. First, the regression approach uses the data as a whole (fitted data from all participants) and normative values do not rely on arbitrary categories. The choice of categories in mean and percentile approaches can have a major impact on normative values: for example, a participant aged on the edge between two categories could be considered normal in a category and not in the other, and this may cause confusion in clinicians. Secondly, by dividing a sample in subcategories, the mean and SD of some cells might be low and likely unrepresentative to the population, especially for the values close to the category boundaries (e.g., low educated young individuals), even when samples are large. For the MoCA test, most studies presented normative data with the means and SD method (Conti et al., 2015; Freitas et al., 2011; Lu et al., 2011; Malek-Ahmadi et al., 2015; Narazaki et al., 2013; Ng et al., 2015; Rossetti et al., 2011; Santangelo et al., 2015) and only one study used the percentiles method (Kenny et al., 2013). Finally, normative data was presented with means and SD in one study, but the authors also used a regression formula to obtain adjusted scores, which gives more precise adjustments to the patient's performance (Conti et al., 2015). This previous study provided both a regression formula and a table with adjustments to be added or subtracted from the raw scores. The obtained adjusted scores then have to be converted in equivalent scores, where 0 is below the norm (unspecified Z or percentile), 4 is equal or better than the 50th percentile, and 1, 2, and 3 being intermediates. Although this approach provides helpful additional information to the original cutoff on the patients’ cognition, it does not provide continuous data on a continuous scale of normality. No normalization study of the MoCA as yet provided a formula to produce Z scores to estimate individual performance on a continuous scale of normality.
The clinical use of the MoCA in Quebec could benefit from population-specific norms and from an alternative method for assessing cognitive performance. The previously available norms in Quebec did not take into account the effect of all the sociodemographic characteristics of the participants (Nasreddine et al., 2005). Moreover, a larger sample size than that of the original norms would contribute to better representation of MoCA test performance among Quebec-French people. As such, the present study aimed to establish normative data for the MoCA test in a middle-aged and elderly Quebec-French population, taking into account the contribution of age, education, and sex on test performance.
Methods
Participants
Researchers across the Province of Québec (Canada) were invited to share anonymized data from healthy volunteers who had completed the MoCA as part of other research studies approved by local Research Ethics Boards. Secondary data from those studies were used in the present normative study. Participants were from 12 recruiting sites, including laboratories from Québec City (5 sites), Trois-Rivières (1 site), Montréal (4 sites), and Sherbrooke (2 sites).
All participants included in the present study were born and raised in the Province of Québec, reported French as their mother tongue and usual language, were at least 40 years of age, and lived independently in the community. All participants were recruited as healthy controls and were considered cognitively non-impaired according to medical history, actual self-reported medical information, and clinical assessments performed at each recruitment site. In most sites, cognition was evaluated through a complete neuropsychological assessment. In all sites, participants self-reported no cognitive decline/impairment and no diagnosed cognitive condition.
MoCA results from 1216 participants were received from the 12 sites (Québec City = 642, Montréal = 332, Trois-Rivières = 120, Sherbrooke = 122). Subsequently, according to exclusion criteria, 197 participants were excluded for: depressive symptoms (n = 37), age under 40 (n = 86), presence of metabolic or cardiac illness (n = 21), other country of origin (n = 20), other psychiatric illness (n = 9), past traumatic brain injury (n = 6), neurological condition (n = 5), and uncorrected vision problems (n = 3). The final normative sample consisted of 1,019 community-dwelling older adults (331 males and 688 females), aged between 41 and 98 (mean age = 67.9 years ± 8.8) and an education level varying between 3 and 23 years (mean education level = 14.4 years ± 3.9; education level was maximum 23 years, which corresponds to a doctoral degree in the Quebec schooling system). When compared to actual Quebec demographics, highly educated participants of all age ranges are overrepresented in our sample, except for participants younger than 44 years old, where participants with low education are overrepresented (85.7%) (Institut de la statistique du Québec, 2006). Women were also slightly overrepresented in most age clusters, except in participants younger than 44 years old.
Materials and Procedures
The original French version of the MoCA (www.mocatest.org) was individually administered to all participants as part of a screening procedure. Trained research professionals or students administered the instrument following its original instructions. The MoCA is a 10- to 15-minute test, which comprises 14 subtests evaluating various cognitive domains. The domains evaluated include attention and concentration, executive functions, memory, language, visuoconstructional and visuospatial skills, conceptual thinking, calculation, and orientation to time and space. The highest possible score is 30. Of note, the suggested 1-point correction for participants with ≤12 years of education was not applied in the present study as the aim was to generate normative data taking into account education level attained.
Statistical Analyses
Prediction of the MoCA score
In order to predict expected MoCA performance according to sociodemographics, a multiple regression analysis was performed for the total score with age, sex, and education as predictors. Interactions between predictors and nonlinear relationships using quadratic terms for age and education were tested. To avoid overfitting and maximize generalizability of the predictions, the best predictive model was determined with a 10-fold cross-validation (Hastie, Tibshirani & Friedman, 2008), retaining the model with the lowest predicted residual sum of squares using SAS 9.4 PROC GLMSELECT (SAS Institute Inc., Cary, NC). Individual predictors’ weight in each model were measured by squared semi-partial correlations (R2). Sex was coded as 1 for men and 0 for women. Inspection of the residuals, condition index, and Cook's distance were used to verify the underlying assumptions of the regression model including outliers, multicolinearity, heteroscedasticity, normality, and nonlinearity. The predictive model was developed using 819 participants. The remaining 200 were randomly selected and used as a validation sample.
Validation of the prediction model
In addition to the cross-validation procedure selecting the best predictors, the predictions of the model were validated by calculating a validation R2 with the validation sample. These predictions were not used to build the predictive model. The validation R2 was computed by the squared correlation between actual and model predicted MoCA scores.
Results
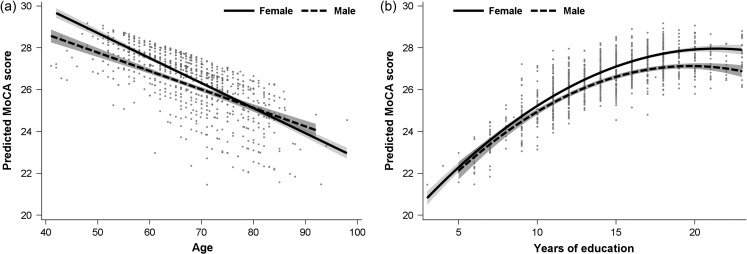
The mean MoCA total scores for the normative and validation samples are provided in Table 1. The best predictive model included age (β = −0.083, SE = 0.01, p < .001), education (β = 0.785, SE = 0.12, p < .001), sex (β = −0.590, SE = 0.17, p < .001), and a quadratic term for education (education X education; β = −0.019, SE = 0.004, p < .001), which explained a significant amount of variance of the MoCA score, F(4, 814) = 71.90, p < 0.001, R2 = 0.261 (adjusted R2 = 0.257). In the retained model, older age, lower education level, and male sex were associated with lower total score. R2 for individual predictors revealed that age (0.120) and education (0.118) explained most of the variance, whereas sex (0.005) and the quadratic term for education (0.018) explained a slight amount. Figure 1 describes the relationships between these variables for men and women. Figure 1a illustrates the predicted MoCA score according the number of years of education and Fig. 1b according to age.
Table 1.
Samples’ characteristics
| Sample (N) | Age M ± SD | Female % | Education M ± SD | MoCA score | |
|---|---|---|---|---|---|
| M (SD) | Range | ||||
| Normative (819) | 67.8 ± 8.8 | 67.3% | 14.4 ± 3.8 | 26.4 ± 2.7 | 13–30 |
| Validation (200) | 67.9 ± 8.8 | 68.5% | 14.4 ± 4.0 | 26.5 ± 2.7 | 16–30 |
Note: MoCA = Montreal Cognitive Assessment; M = Mean; SD = Standard Deviation.
Fig. 1.
Effect of age, sex, and education on the regression model. Shaded ribbons on each side of the curves denote 95% confidence intervals. (a) illustrates the effect of age on the regression-predicted MoCA score depending on the sex of participants. (b) illustrates the effect of age on the regression-predicted MoCA score for both sexes.
The validation procedure revealed a validation R2 of 0.304, which was higher than the R2 of the predictive model. Thus, the validation showed adequate explained variance in an independent sample of individuals.
Based on the results from the regression model, the equation to calculate the expected score given the age, education level, and sex of the participants is reported in Table 2. To calculate the patient's Z score, the expected score is subtracted from the real score, and then divided by the square root of the mean square residual. The application of this equation in clinical practice will be explained in the discussion.
Table 2.
Information used to calculate Z scores with sociodemographic variables for the MoCA total score
| Equations to calculate Z scores |
| Z = (Real score − Expected score) / Square root of the mean square residual |
| Z = (Real score − (25.186–0.083 A + 0.785 E–0.590 S – 0,019 E × E)) / 2.29 |
Note: E = Education in years; A = Age in years; S = Sex (0 = women and 1 = men).
Discussion
The aim of the present study was to establish normative data for the total MoCA score in a Quebec-French population and to determine the impact of sociodemographic factors on test performance. As expected, the total MoCA score was lower as age increased, which is in line with previous normative studies using the same test (Freitas et al., 2011; Kenny et al., 2013; Lu et al., 2011; Malek-Ahmadi et al., 2015; Narazaki et al., 2013; Rossetti et al., 2011; Santangelo et al., 2015). Total MoCA score was higher with higher education level, which is again consistent with previous normative studies using the MoCA (Freitas et al., 2011; Kenny et al., 2013; Lu et al., 2011; Malek-Ahmadi et al., 2015; Narazaki et al., 2013; Rossetti et al., 2011; Santangelo et al., 2015). Finally, in the present study, sex was associated with total MoCA score, which is not in line with most of previous studies using this test (Freitas et al., 2011; Kenny et al., 2013; Malek-Ahmadi et al., 2015; Narazaki et al., 2013; Rossetti et al., 2011). However, our large sample could be responsible for this significant sex effect, as its relative contribution to prediction is small. According to our results, sociodemographic variables accounted for 26.1% of variance in MoCA performance. This proportion of variance is similar to that obtained elsewhere. Indeed, Malek-Ahmadi and colleagues (2015) obtained R2 for age and education of, respectively, 0.10 and 0.05, whereas Ng and colleagues (2015) obtained R2 of, respectively, 0.069 and up to 0.162. Moreover, other studies reported higher R2 (Freitas et al., 2011; Santangelo et al., 2015), but included additional predictors to sociodemographic variables, such as the urban or rural living environment. Such comparisons were not possible in the present sample, because all participants were recruited in research centers located in urban environments.
The significant association with sex in the present study could be explained by cultural aspect of Quebec's population, similar to what was suggested for the Chinese population by Lu and colleagues (2011). Those authors interpreted the sex difference they observed to a cultural context in China, in which less educated women were viewed as being in less contact with current events and had lower socioeconomic status than men. A similar condition might exist in Quebec men, but available data do not allow clear interpretation of this possibility, as its contribution to prediction is small. Our findings support the utility of developing culture-specific MoCA norms, because they bring evidence of the influence of sex on MoCA performance in French-speaking Quebecers, which was not the case in other cultures, except Chinese. Our study also benefits from an added clinical value because of the wide range of ages covered in our sample. Indeed, by including participants as young as 40 years old, we also enable the use of our norms to clinicians investigating for cognitive impairments occurring in disorders other than dementia and Alzheimer's disease.
Based on our regression model, an equation to predict a MoCA score was derived (see Table 2). For example, a 75-year-old man with 11 years of education, obtains a total score of 22/30 on the MoCA. According to the original procedure and norms (Nasreddine et al., 2005), the patient's education level is ≤12 years and one point would normally be added to his total score. Despite the addition of one point, the score of the patient would still fall below the standard cutoff of 26/30 and would suggest that follow-up for possible MCI be considered. In the present study, no point was added for low education because this variable was considered in the development of the regression equation. According to the regression equation derived from the data of the present study, the patient's expected score would be: 25.186−0.083 (75) + 0.785 (11)−0.590 (1)−0.019 (11*11) = 24.71. To calculate the patient's Z score, the expected score is subtracted from the real score, and then divided by the square root of the mean square residual: (22–24.71) / 2.29 = −1.18. This Z score would be considered clinically normal (over Z = −1.5) despite the fact that the raw MoCA score in this hypothetical case was <26. This example illustrates the necessity of having norms adjusted for several sociodemographics when determining performance on the MoCA. In order to facilitate calculation of a Z score based on the equation reported in Table 2, an MS Excel® document was prepared for clinicians and is available in Supplementary Data.
Up to date, the MoCA has been widely used in Quebec as a dementia-screening tool with a cutoff of 26. A recent review found that the MoCA had a good sensitivity, allowing detection of over 94% of individuals with dementia in all observed settings (Davis et al., 2015). The same review underlined the low specificity of the MoCA, with over 40% of normal controls being false positives when their score falls below 26. The use of regression-based norms correcting for sociodemographics will be an important addition for clinicians, as it has been reported to maximize specificity, whereas compromising sensitivity (O'Connell & Tuokko, 2010). Therefore, clinicians will now have access to information that should maximize both sensitivity and specificity of their diagnostics. But further research should be carried out to explore the comparative efficacy of cutoffs and sociodemographic-corrected norms in clinical screening settings.
The present study used a regression-based approach to calculate normative data for the total MoCA score, instead of typical normalization methods (e.g., percentiles or standard Z scores calculated from a mean and SD only). The former approach leads to better estimation of a person's MoCA performance because it takes specific demographics into account, which is critical for a screening tool. Indeed, these regression-based norms offer clinicians a nuanced appreciation of the patient's performance. Although the use of a cutoff point alone may be sufficient in some clinical settings by simply informing on the necessity to request a complete neuropsychological assessment, others could benefit from using additional continuous normative values. As mentioned in the previous paragraph, maximized sensitivity and specificity will help clinicians refine their judgment to decide whether a complete assessment is required. Taking into account the important sums and the time at stake for every complete neuropsychological assessment, more comprehensive patient care could benefit some clinical settings. A limitation of the use of means and SD for Z-score calculation is the use of arbitrary categories to obtain comparison means and SD. These categories may lead to important disparities between two similar sociodemographic profiles that fall into different age or education categories. For example, we separated participants according to their sex, according to their years of education (≤12 or ≥13) and according to their age (60 and under, or 61 to 70, or 71 to 80, or 81 and over). Using means and SD of these categories, a man with 12 years of education with a raw MoCA score of 23, means and SD would give a Z score of −1.76 at 60 years old and a Z score of −1.08 at age of 61, which is a notable difference (0.68) for aging a single year. However, using our regression-based norms he would get a Z score of −1.44 at 60 and −1.40 at 61. So, the effect of normal cognitive aging is clearly better reflected using the regression-based norms compared to the usual use of arbitrary categories stratifying for age and education. In a similar way, whereas this 60 years old man with 12 years of education has a Z score of −1.76 using categories, he would have a Z score of −2.15 with 13 years of education (difference of 0.39). Using our regression-based norms, he would get a Z score of −1.44 with 12 years of education and of −1.58 with 13 (difference of 0.14). Again, the use of regression-based norms in this example likely better reflects the effect of education on cognitive performance.
The main limitation of the present study was the use of an incidental sampling method, which resulted in overrepresentation of highly educated individuals in most age groups. The overrepresentation of women in our sample compared to Quebec demographics is another limitation of our sample, although it is not possible to clearly determine its impact on the obtained results. Indeed, the observed proportion of women (65.5%) is consistent with what can be found in most of other studies in which women accounted for between 60 and 68.3% of the sample (Freitas et al., 2011; Malek-Ahmadi et al., 2015; Narazaki et al., 2013; Ng et al., 2015; Rossetti et al., 2011; Santangelo et al., 2015). Although a random sampling method would have been preferable, the present study represents a practical and relevant starting point for establishing MoCA norms for the Quebec-French population. Also, although all examiners followed the original instructions for administration and scoring of the MoCA, common training was not provided across recruitment sites, so some degree of variability may have existed between the examiners. Another limitation of this study is that the present norms are limited to French-speaking Quebecers. Moreover, in the current sample there were relatively few individuals in the 40–49 and 80+ age categories. As a consequence, clinicians should be careful when using these norms in non-French speaking Quebec residents and in Quebeckers aged 40–49 or >80 years. Future research should consider possible language variations and assess differences between French and English speaking populations living in Quebec. Future normative studies should also recruit more participants <50 and >80 years old.
In conclusion, this study is the first to provide normative data for the MoCA in the middle-aged and elderly French Quebeckers. These data will facilitate more accurate detection and follow-up of the risk of cognitive impairment in this population, taking into account culture, language, age, education, and sex. Furthermore, the use of the present normative data by Quebec's clinicians will provide them with a second insight on whether patients should be referred for an extensive neuropsychological evaluation, potentially saving time and money to both patients and healthcare providers.
Supplementary Material
Acknowledgements
None.
Supplementary Data
Supplementary material is available at Archives of Clinical Neuropsychology online.
Funding
This work was supported by the Réseau québécois de recherche sur le vieillissement, the Canadian Institutes of Health Research and the Natural Sciences and Engineering Research Council of Canada. As this is a secondary use of the data, grants were obtained in order to fund the initial research projects.
Conflict of Interest
None declared.
References
- Albert M. S., DeKosky S. T., Dickson D., Dubois B., Feldman H. H., Fox N. C., et al. (2011). The diagnosis of mild cognitive impairment due to Alzheimer's disease: recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimer's & Dementia, 7 (3), 270–279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alzheimer's Disease International (2009). World Alzheimer Report. Retrieved from http://www.alz.co.uk/research/files/WorldAlzheimerReport-ExecutiveSummary.pdf.
- Arsenault-Lapierre G., Whitehead V., Belleville S., Massoud F., Bergman H., & Chertkow H. (2011). Mild cognitive impairment subcategories depend on the source of norms. Journal of Clinical and Experimental Neuropsychology, 33 (5), 596–603. [DOI] [PubMed] [Google Scholar]
- Cameron J., Ski C. F., & Thompson D. R. (2012). Screening for determinants of self-care in patients with chronic heart failure. Heart, Lung & Circulation, 21 (12), 806–808. [DOI] [PubMed] [Google Scholar]
- Conti S., Bonazzi S., Laiacona M., Masina M., & Coralli M. V. (2015). Montreal Cognitive Assessment (MoCA)-Italian version: regression based norms and equivalent scores. Neurological Sciences, 36 (2), 209–214. [DOI] [PubMed] [Google Scholar]
- Cumming T. B., Bernhardt J., & Linden T. (2011). The montreal cognitive assessment: short cognitive evaluation in a large stroke trial. Stroke, 42 (9), 2642–2644. [DOI] [PubMed] [Google Scholar]
- Davis D. H. J., Creavin S. T., Yip J. L. Y., Noel-Storr A. H., Brayne C., & Cullum S. (2015). Montreal Cognitive Assessment for the diagnosis of Alzheimer's disease and other dementias. Cochrane Database of Systematic Reviews (Online), (10), CD010775. DOI: 10.1002/14651858.CD010775.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Guise E., Leblanc J., Champoux M. C., Couturier C., Alturki A. Y., Lamoureux J., et al. (2013). The mini-mental state examination and the Montreal Cognitive Assessment after traumatic brain injury: an early predictive study. Brain Injury, 27 (12), 1428–1434. [DOI] [PubMed] [Google Scholar]
- Freitas S., Simoes M. R., Alves L., & Santana I. (2011). Montreal Cognitive Assessment (MoCA): normative study for the Portuguese population. Journal of Clinical and Experimental Neuropsychology, 33 (9), 989–996. [DOI] [PubMed] [Google Scholar]
- Gagnon J. F., Postuma R. B., Joncas S., Desjardins C., & Latreille V. (2010). The Montreal Cognitive Assessment: a screening tool for mild cognitive impairment in REM sleep behavior disorder. Movement Disorders, 25 (7), 936–940. [DOI] [PubMed] [Google Scholar]
- Gill D. J., Freshman A., Blender J. A., & Ravina B. (2008). The Montreal cognitive assessment as a screening tool for cognitive impairment in Parkinson's disease. Movement Disorders, 23 (7), 1043–1046. [DOI] [PubMed] [Google Scholar]
- Hastie T., Tibshirani R., & Friedman J. (2008). The elements of statistical learning. Data mining, inference, and prediction. Stanford, California: Springer. [Google Scholar]
- Institut de la statistique du Québec (2006). Population de 25 ans et plus, selon le plus haut degré de scolarité atteint, le sexe et le groupe d’âge Québec, 2006. Retrieved from http://www.stat.gouv.qc.ca/donstat/societe/education/etat_scolr/tab1_niv_sco_2006.htm.
- Kenny R. A., Coen R. F., Frewen J., Donoghue O. A., Cronin H., & Savva G. M. (2013). Normative values of cognitive and physical function in older adults: findings from the Irish Longitudinal Study on Ageing. Journal of the American Geriatrics Society, 61 (Suppl 2), S279–S290. [DOI] [PubMed] [Google Scholar]
- Lu J., Li D., Li F., Zhou A., Wang F., Zuo X., et al. (2011). Montreal cognitive assessment in detecting cognitive impairment in Chinese elderly individuals: a population-based study. Journal of Geriatric Psychiatry and Neurology, 24 (4), 184–190. [DOI] [PubMed] [Google Scholar]
- Malek-Ahmadi M., Powell J. J., Belden C. M., O'Connor K., Evans L., Coon D. W., et al. (2015). Age- and education-adjusted normative data for the Montreal Cognitive Assessment (MoCA) in older adults age 70–99. Neuropsychology, Development, and Cognition. Section B, Aging, Neuropsychology and Cognition, 22, 1–7. [DOI] [PubMed] [Google Scholar]
- Mickes L., Jacobson M., Peavy G., Wixted J. T., Lessig S., Goldstein J. L., et al. (2010). A comparison of two brief screening measures of cognitive impairment in Huntington's disease. Movement Disorders, 25 (13), 2229–2233. [DOI] [PubMed] [Google Scholar]
- Narazaki K., Nofuji Y., Honda T., Matsuo E., Yonemoto K., & Kumagai S. (2013). Normative data for the montreal cognitive assessment in a Japanese community-dwelling older population. Neuroepidemiology, 40 (1), 23–29. [DOI] [PubMed] [Google Scholar]
- Nasreddine Z. S., Phillips N. A., Bédirian V., Charbonneau S., Whitehead V., Collin I., et al. (2005). The Montreal Cognitive Assessment, MoCA: A brief screening tool for mild cognitive impairment In Journal of the American Geriatrics Society, 53 (pp. 695–699). [DOI] [PubMed] [Google Scholar]
- Ng T. P., Feng L., Lim W. S., Chong M. S., Lee T. S., Yap K. B., et al. (2015). Montreal Cognitive Assessment for screening mild cognitive impairment: variations in test performance and scores by education in Singapore. Dementia and Geriatric Cognitive Disorders, 39 (3–4), 176–185. [DOI] [PubMed] [Google Scholar]
- O'Connell M. E., & Tuokko H. (2010). Age corrections and dementia classification accuracy. Archives of Clinical Neuropsychology, 25 (2), 126–138. [DOI] [PubMed] [Google Scholar]
- Olson R., Tyldesley S., Carolan H., Parkinson M., Chhanabhai T., & McKenzie M. (2011). Prospective comparison of the prognostic utility of the Mini Mental State Examination and the Montreal Cognitive Assessment in patients with brain metastases. Supportive Care in Cancer, 19 (11), 1849–1855. [DOI] [PubMed] [Google Scholar]
- Overton E. T., Azad T. D., Parker N., Demarco Shaw D., Frain J., Spitz T., et al. (2013). The Alzheimer's disease-8 and Montreal Cognitive Assessment as screening tools for neurocognitive impairment in HIV-infected persons. Journal of Neurovirology, 19 (1), 109–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pendlebury S. T., Cuthbertson F. C., Welch S. J., Mehta Z., & Rothwell P. M. (2010). Underestimation of cognitive impairment by Mini-Mental State Examination versus the Montreal Cognitive Assessment in patients with transient ischemic attack and stroke: a population-based study. Stroke, 41 (6), 1290–1293. [DOI] [PubMed] [Google Scholar]
- Petersen R. C. (2004). Mild cognitive impairment as a diagnostic entity. Journal of Internal Medicine, 256 (Le), 183–194. [DOI] [PubMed] [Google Scholar]
- Popovic I. M., Seric V., & Demarin V. (2007). Mild cognitive impairment in symptomatic and asymptomatic cerebrovascular disease. Journal of the Neurological Sciences, 257 (1–2), 185–193. [DOI] [PubMed] [Google Scholar]
- Prince M., Bryce R., Albanese E., Wimo A., Ribeiro W., & Ferri C. P. (2013). The global prevalence of dementia: a systematic review and metaanalysis. Alzheimer's & Dementia, 9 (1), 63–75 e62. [DOI] [PubMed] [Google Scholar]
- Rossetti H. C., Lacritz L. H., Cullum C. M., & Weiner M. F. (2011). Normative data for the Montreal Cognitive Assessment (MoCA) in a population-based sample. Neurology, 77 (9), 1272–1275. [DOI] [PubMed] [Google Scholar]
- Santangelo G., Siciliano M., Pedone R., Vitale C., Falco F., Bisogno R., et al. (2015). Normative data for the Montreal Cognitive Assessment in an Italian population sample. Neurological Sciences, 36 (4), 585–591. [DOI] [PubMed] [Google Scholar]
- Schweizer T. A., Al-Khindi T., & Macdonald R. L. (2012). Mini-Mental State Examination versus Montreal Cognitive Assessment: rapid assessment tools for cognitive and functional outcome after aneurysmal subarachnoid hemorrhage. Journal of the Neurological Sciences, 316 (1–2), 137–140. [DOI] [PubMed] [Google Scholar]
- United Nations, Department of Economic and Social Affairs, Population Division (2013). World Population Ageing 2013. ST/ESA/SER.A/348 . [Google Scholar]
- Videnovic A., Bernard B., Fan W., Jaglin J., Leurgans S., & Shannon K. M. (2010). The Montreal Cognitive Assessment as a screening tool for cognitive dysfunction in Huntington's disease. Movement Disorders, 25 (3), 401–404. [DOI] [PubMed] [Google Scholar]
- Villeneuve S., Pepin V., Rahayel S., Bertrand J. A., de Lorimier M., Rizk A., et al. (2012). Mild cognitive impairment in moderate to severe COPD: a preliminary study. Chest, 142 (6), 1516–1523. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.