Abstract
STUDY QUESTION
How do patients and providers perceive and make decisions about possible reductions of multi-fetal pregnancies?
SUMMARY ANSWER
Physicians may be transferring additional embryos, assuming that patients will later undergo reduction if need be; but decisions to reduce pregnancies are difficult for patients, who may agree to undergo the procedure in advance and later renege.
WHAT IS ALREADY KNOWN
Implanting more than one embryo increases the likelihood that at least one embryo will successfully lead to a child but also that the patient may end up with twins or higher-order multiple births.
STUDY DESIGN, SIZE, DURATION
In-depth interviews of ~1 h each were conducted with 37 ART providers and patients (17 physicians, 10 other health providers and 10 patients) and systematically analyzed.
PARTICIPANTS/MATERIALS, SETTING, METHOD
The telephone interviews explored the participants’ views and decisions regarding pregnancy reduction. The answers were analyzed systematically.
MAIN RESULTS AND THE ROLE OF CHANCE
Providers may be transferring additional embryos, thinking that doing so will increase the likelihood of a ‘take home baby’ and that the patients could undergo reductions, if need be, to avoid the risks and complications of twins or multiple births. Yet patients often appear to have difficulty confronting the prospect of fetal reduction and/or renege on prior agreements to undergo the procedure. Providers should thus be wary and exceedingly careful about these situations.
LIMITATIONS, REASONS FOR CAUTION
The sample size was sufficient for qualitative research designed to elucidate the issues and themes that emerge, but not for statistically analyzing how various groups may differ (e.g. physicians versus patients). Future studies should investigate these issues with larger samples.
WIDER IMPLICATIONS OF THE FINDINGS
These data, the first to examine how IVF providers and patients view and approach decisions regarding the reduction of fetuses, suggest several complications and dilemmas. This information has critical implications for future practice, guidelines, research and education of providers, patients, insurers, policymakers and others.
STUDY FUNDING/COMPETING INTEREST(S)
Funding was provided by grant #UL1 RR024156 from the National Center for Research Resources, the Greenwall Foundation and the John Simon Guggenheim Memorial Foundation. There are no conflicts of interest to declare.
Keywords: multiple pregnancy, in-vitro fertilization, twins, embryos, ethics, policy
Introduction
Twin and other multiple births have increased due to assisted reproductive technologies, raising critical questions about the possibility of fetal reductions. Rates of twins and multiple births have essentially doubled over the past 40 years in many countries, including Europe, the USA and Asia (Osterman et al., 2015; Pison et al., 2015). Yet, risks of maternal and infant complications rise significantly with these births (Practice Committee of the ASRM, 2012). Single embryo transplant (SET) success rates have been rising and efforts have been made to establish SET as the standard of care (Kissin et al., 2015), which is increasingly possible through expanding insurance, appropriate educational materials and inclusion of patients’ partners in discussions (Leese and Denton, 2010; Griffin et al., 2012). Rates of two or more multiple births have thus started to lower (Kulkarni et al., 2013; Pison et al., 2015), yet remain relatively high, at ~19.4% of all European Union births (Kupka et al., 2016). Among cycles using IVF and ICSI, transfers of three and four embryos accounted, respectively, for 14.5 and 1.3% of transfers in Europe, including 49.4 and 9.9% in Greece (Kupka et al., 2016). Twin and triplet deliveries accounted for 18.6 and 0.6% of European IVF/ICSI births, including 41.5 and 3.5% in Greece (Kupka et al., 2016). In 2013, among all US transfers using fresh non-donor oocytes or embryos, 76.4% involved more than one embryo, and 20.7% involved three or more embryos, and for women younger than 35 years, the number of fresh and thawed embryos from non-donor oocytes transferred averaged 1.8 and 1.7, respectively (CDC, 2015). For mothers aged <35 and 35–37, respectively, in the US, 28.3 and 25.5% of births were twins, and ~1% were triplets or more (CDC, 2015).
Transferring more than one embryo increases the chances that one or more embryo will produce a child but also that the patient may have multiple births. Patients with two or more fetuses can reduce the number, but risks include loss of the entire pregnancy (Antsaklis et al. 2004), raising questions of when, how often and how much this option is considered or followed.
Guidelines have sought to reduce the numbers of embryos transferred in various countries, including the UK (HFEA, 2013). The 27 EU countries’ policies vary and more countries are now limiting numbers of embryos transferred (ESHRE, 2009). The UK has progressively lowered the maximum multiple birth rates to 10% (HFEA, 2013). The American Society of Reproductive Medicine (ASRM) allows physicians considerable flexibility in numbers of embryos transferred. For younger patients with a favorable prognosis, ‘providers should only transfer a single embryo, and not more than two embryos’ (Practice Committees of ASRM and SART, 2013).
Reduction of triplets to singletons provides better results than births of triplets (Haas et al., 2014). Reduction of twin pregnancies to singletons also reduces complications (Hasson et al., 2011; Haas et al., 2015). At one center, from 1986–1999 to 1999–2006, reductions increased to 15.6% of twin pregnancies, lowering pregnancy loss and neonatal complications (Stone et al., 2010). Rates of reduction-induced miscarriage and spontaneous twin pregnancy losses are ~9.12% and 8–10%, respectively (Antsaklis et al. 2004; Evans et al., 2004).
In many countries, the annual number of reductions remains unknown. In 2011, 22 European countries had 343 fetal reductions (Kupka et al., 2016), yet several nations did not provide data. Moreover, whether these reductions were for twin or higher multiple pregnancies is unclear. The number of US reductions is unknown. Among 36 Oregon IVF patients, before embryo transfer, 77% would consider reduction, 67% would consider reducing triplets, while only 6.5% would consider reducing twins (Munks et al., 2007). Among IVF/ICSI patients in India, 83% were counselled about reduction but 61% did not know the procedure was invasive and risked miscarriage. Still, 72% said they knew reduction carries less risk than higher-order pregnancy, 73% said reduction was thus preferable, and 37% had significant moral concerns about reduction. Among these women, 42 reduced, of whom, 40% said they were initially unwilling to do so (Balasubramanyam, 2010).
Yet research remains scant on how patients and providers elsewhere view and approach these issues: not only how often they reduce, but how they perceive and make these decisions. No studies of ART providers’ practices or views concerning these issues have been published since a 2008 study found that 52% of clinicians deviated from guidelines on numbers of embryos to transfer (Jungheim et al., 2010). Extensive literature searches have found no other studies of how providers view these issues: why they do not fully follow SET recommendations, and what challenges they face.
Crucial questions thus remain of why many providers continue to permit twins, despite the risks. Limited resources and insurance may lead many patients to want more than one embryo but significant obstacles often impede increasing insurance coverage. Consequently, exploring what other approaches might help increase reductions is critical. Hence, as part of a study exploring how providers and patients view and make decisions about maximum age limits of patients (Klitzman, 2016), and several other key aspects of IVF, issues concerning numbers of embryos to implant and reductions of pregnancies were investigated.
Materials and methods
As previously described (Klitzman, 2016), 37 in-depth interviews of ~1 h each were conducted with 27 ART providers: 17 physicians (MDs) and 10 other providers (OPs) and 10 patients.
Qualitative methods were chosen because no prior studies have been published examining IVF providers’ and patients’ attitudes and practices and these methods can best elicit the full range and typologies of attitudes, interactions and practices involved, and can inform subsequent quantitative studies. From a theoretical standpoint, Geertz (1973) has advocated studying aspects of individuals’ lives, decisions and social situations not by imposing theoretical structures, but by trying to understand the individuals’ own experiences, drawing on their own words and perspectives to obtain a ‘thick description’. The methods for the present study adapted elements from ‘Grounded Theory’ (Strauss and Corbin, 1990) and were thus informed by techniques of ‘constant comparison’, with data from different contexts compared for similarities and differences, to see whether they suggest hypotheses. These methods have been used in several other studies on key aspects of health behavior and doctor–patient relationships and communications in genetics and other areas (Klitzman and Daya, 2005; Klitzman et al., 2007, 2013; Klitzman, 2012, 2013).
Participants
As summarized in Supplementary Table S1, 37 in-depth interviews of ~1 h each were conducted and subsequently analyzed. Interviewees included 27 ART providers: 17 physicians including 1 physician–patient, 10 other providers (7 mental health providers, 2 nurses and 1 other) including 3 other provider–patients, and 10 patients. Providers were recruited through national ASRM meetings (e.g. PGD and mental health provider interest group meetings), emails and word-of-mouth. The principal investigator (PI) asked individuals at these meetings, for instance, whether they might be interested in participating in an interview study, and if so, the PI subsequently emailed them information about it. Approximately 75% of those asked agreed to participate, and did so. A mental health listserv was also used, which is received by ~60 members (not all of whom are active), of whom 15 responded, and the first 8 respondents were then interviewed. Patients were recruited through providers who had participated and through infertility patient organizations and word-of-mouth. Additional interviews were conducted as background, for informational purposes, with 8 physicians, 9 mental health providers and 14 patients, and these informed, but were not included in, the final formal data analysis. Interviews for the formal data analyses were conducted with each group until ‘saturation’ was reached, i.e. ‘the point at which no new information or themes are observed in the data’ (Guest et al., 2006). Interviewees were from across the US. Interviews were conducted by phone, in order to allow participants to choose when it would be most convenient for them, and because the interviewees resided all over the US, making travel to each of them for a face-to-face interview unfeasible. Providers described interactions with multiple patients they had treated and colleagues, and patients often described interactions with multiple providers and other patients.
The Columbia University Department of Psychiatry Institutional Review Board approved the study, and all participants gave informed consent.
Instruments
The semi-structured interview questionnaire was drafted drawing on prior literature and explored patients’ and providers’ views, experiences and decisions concerning pregnancy reduction and other critical aspects of ART. Sample questions for providers included, for example, the following questions.
What challenges do you face in your work as an ART provider?
How do you address these challenges?
Have you faced challenges concerning pregnancy reduction? If so, when? What was different about the situation? What did you do? How did you make these decisions?
How do you view these issues?
How have your patients viewed these issues?
What additional thoughts do you have about these issues?
Data analysis
Transcriptions and initial analyses of interviews occurred during the period in which the interviews were being conducted, enhancing validity, and helping to shape subsequent interviews. Once the full set of interviews was completed, subsequent analyses were conducted in two phases, primarily by two trained research assistants (RAs) and the PI. In phase I, they independently examined a subset of interviews to assess factors that shaped participants’ experiences, identifying categories of recurrent themes and issues that were subsequently given codes. The PI and RAs read each interview, systematically coding blocks of text to assign ‘core’ codes or categories (e.g., instances and views of transferring additional embryos, and possible reductions of pregnancies). While reading the interviews, a topic name (or code) was inserted beside each excerpt of the interview to indicate the themes being discussed. The PI and RAs then worked together to reconcile these independently developed coding schemes into a single scheme. Next, a coding manual was prepared, defining each code and examining areas of disagreement until reaching consensus. New themes that did not fit into the original coding framework were discussed, and modifications made in the manual when it was deemed appropriate.
In phase II of the analysis, the PI and RAs independently content-analyzed the data to identify the principal subcategories and ranges of variation within each of the core codes. The sub-themes identified by each coder were reconciled into a single set of ‘secondary’ codes and an elaborated set of core codes. These codes assess subcategories and other situational and social factors. Such subcategories included, for instance, providers’ and patients’ views for versus against reduction or uncertainty about it.
Codes and sub-codes were then used in analysis of all of the interviews. To ensure coding reliability, the PI and an RA analyzed all interviews. Where necessary, multiple codes were used. Similarities and differences were assessed between participants, examining categories that emerged, ranges of variation within categories, and variables that may be involved. Areas of disagreement were examined through closer analysis until consensus was reached. Consistency and accuracy in ratings were checked regularly by comparing earlier and later coded excerpts. Text from the interviews is presented to allow readers to appreciate the richness of the data obtained.
Results
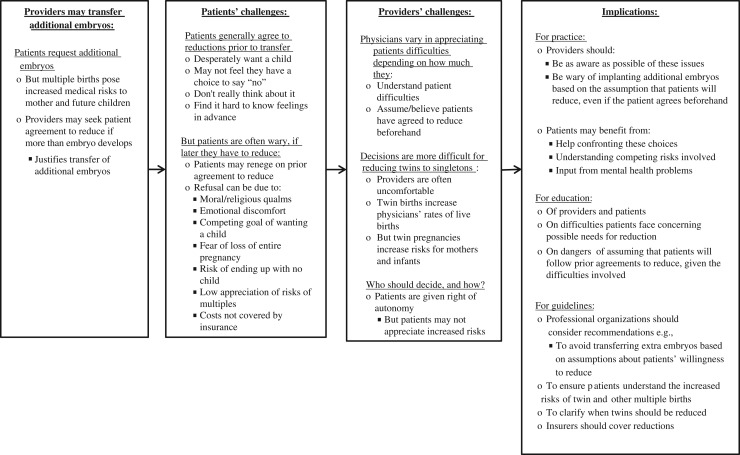
As described below and outlined in Fig. 1, physicians and patients wrestle with whether to reduce the number of fetuses, if more than one develop. Physicians may transfer additional embryos, assuming that patients will later reduce, if needed, but reduction-related decisions prove difficult for patients, who may say ‘yes’ beforehand but later renege.
Figure 1.
Challenges concerning reduction of fetuses.
Transferring additional embryos if patient agrees to later reduction, if needed
Doctors may transfer more than one embryo because they assume that they can later reduce the number of fetuses, if more than one develop. When transferring two or more embryos, providers often discuss beforehand with patients possible needs for later reduction. We have a long checklist of complicated issues…how many embryos go back? Would they do an induced reduction? An amniocentesis? If somebody won't do a fetal reduction, we would never put back more than three embryos. [MD#13] Providers may thus assume that patients will both indicate, beforehand, willingness to reduce and will consent later, if needed.
Challenges faced by patients
Patients generally agree to reductions prior to transfer
Patients generally agree beforehand to reduce later, if needed, but, if desperate to have a child, may not fully grasp, anticipate or appreciate the risks of twins or multiples. We basically had to sign: if the pregnancy was higher than three multiples, we would reduce. We didn't really think it through at the time. I just thought, ‘Let's do this. We need to do this.’ [Patient#9]
Patients may thus agree to potential later reduction because it is a precondition for transfer. If reduction is ultimately needed, then patients face stresses and risks to the whole pregnancy and often reassess. I don't know that I would have been able to say, ‘Sure, go ahead and take one of the fetuses.’ Because when you do that, you could lose the whole pregnancy. With all we had been through, to lose one because we electively decided to do that would have been terrible. Until you're in the actual situation, you really wouldn't know; at the time it was such a far-off possibility that it really wasn't in my mind. It also wasn't in my mind that I should worry about having multiple children. Just getting one child is difficult. You're so desperate to have a child that you think, ‘Hey, two, three, four would be just as good.’ [Patient#9]
Women with infertility thus wrestle with emotional, not simply statistical, issues, feeling desperate for a child, leading them to discount the increased risks.
Patients are often wary, if they later have to reduce
Decisions to reduce can be excruciating, and transferring extra embryos can thus prove problematic later. One physician told a patient: ‘Your likelihood of success is probably <5%’. I put back three. I didn't believe she'd ever get embryos again. She's now 10 weeks pregnant with triplets, and decided not to reduce, thank you very much. So you don't know what's going to happen. You inform and educate patients, and hope you make the right recommendations. [MD#7] Refusals from patients can surprise physicians, who may feel their only choice is to accept the patients’ refusals.
Patients can vary in the nature and strength of their references and reasons, and physicians face choices of how much to try to convince patients. This woman elected not to reduce. I encouraged her to think about it. She wasn't completely adverse to reduction. She didn't say: ‘I will never reduce. It's against my moral or religious beliefs.’ But, ultimately, she didn't like the idea, and continued the pregnancy. [MD#7]
Even for politically pro-choice patients, undergoing reduction can evoke moral/religious qualms. Patients who have been trying longer to get pregnant may be especially reluctant: We had to discuss those options and what to do with extra embryos; and those religious factors appear. Luckily, we didn't have to face that choice. It would've been very difficult, after trying for so long, to then reduce the pregnancy. [Patient#5]
Patients may refuse reduction because of the medical risks to both themselves and the entire pregnancy. If reducing the pregnancy would have ‘ensured’ that the other babies would be okay, I'd have done it. [Patient#5]
Patients must thus weigh multiple risks and uncertainties: needs for reduction (potential complications for twins) against possible loss of the entire pregnancy. Since patients have long sought children, unsuccessfully, abortion can feel very counterintuitive. For people who've tried so hard to get pregnant, eliminating one of the fetuses is not easy. Then, in reducing, some women have unfortunately lost the entire pregnancy. Patients don't lose the pregnancy too often. But when it happens, it's a real tragedy. [OP#4] Sacrificing the whole pregnancy may be relatively unlikely, but very traumatic.
Patients may also resist reduction because insurance often does not reimburse the cost. A lot of insurers don't cover it. [MD#9] Patients also vary based on various factors, e.g., whether they already have offspring. Usually, patients who choose to reduce already have one to two children, and don't think they can handle twins. [Patient#9]
Challenges for providers
Physicians vary in appreciating patients’ difficulties
Providers differ in how much they believe patients’ prior agreements to reduce, and appreciate patients’ struggles. The doctors feel it's a pretty easy, rational decision: ‘You've got to reduce, because it's going to be safer for you and the baby.’ [OP#4] Other clinicians recognize that desperate patients cannot fully anticipate these tradeoffs. Whenever patients say, ‘I'm okay with reductions.’ I always think inside, ‘No, you're not.’ They have no perspective. You can't blame them: they just want to have a baby. [MD#9]
Reducing twin pregnancies to singletons is harder
Patients and providers appear more willing to reduce three fetuses to two than two to one, feeling that the data that twins face more risks than singletons are insufficiently compelling. Women reduce with three. However, usually with two, they don't feel the absolute necessity, because it's safe, though it's a tougher pregnancy. [OP#4] Yet twin pregnancies are not wholly ‘safe’ but ‘safer’. Reducing from two to one fetuses also makes some physicians uncomfortable. Proponents of more active reduction propose going from two to one, but we struggle with it. As a practice, it makes us uncomfortable: three to one or three to two doesn't seem to bother anybody, but reducing twins to one makes people uncomfortable. Most twins are okay. [MD#9]
Providers often let twins continue to term, but feel ‘uncomfortable’ with the elevated risks, seeing the goals of establishing pregnancies and terminating fetuses as clashing. We're about helping people get pregnant, not get pregnant and then have a termination. [MD#9]
Who should decide and how?
Questions surface of who, ultimately, should make these decisions (providers versus patients), and how. Physicians often felt that ultimately, the decision was the patient's. To go from two to one is usually a patient decision. We don't do reductions here. We send those to major academic medical centers. [MD#9] The fact that other physicians, not infertility specialists, perform reductions may also make it easier for infertility specialists to transfer additional embryos.
Clinicians often thought that they should recommend what they feel is best, but that ultimately patients should choose. A gestational surrogate got pregnant with quadruplets. Ultimately, they elected not to reduce. She was a little premature, but the kids are doing okay. I think I have a responsibility, as unpleasant as it may be, to strongly recommend things, if there is a reason to do so. [MD#7] This physician describes this patient's refusal (to have her surrogate pregnancy reduced) to exemplify tensions concerning how much to challenge patients’ wishes for additional embryos and recommend surgery: how far exactly clinicians’ responsibilities go. Countering patients’ wishes can feel ‘unpleasant’.
Providers may disagree with the patient's decision, but feel their influence and role are limited. One woman refused to reduce any of her three fetuses: Even though she got pregnant with triplets, I don't know that I made the wrong decision. The outcome just isn't what I wanted. If somebody said, ‘She's 26 years old, you can only put one embryo back in,’ I'm not sure that it would've been the right decision, because it's important to allow people that level of autonomy. [MD#7] This physician acknowledges potential problems in simply following patients’ autonomy, yet ultimately abdicates to patients the decision of how many embryos to transfer.
Weighing competing principles
Although most providers saw the decision to reduce or not as the patient's, due to autonomy, countervailing ethical principles arose, e.g., social justice, that twins with severe complications will require many resources in under-resourced healthcare systems. We wrestle with the competing ethical areas of patient autonomy versus the physicians’ social responsibility to do what's right for society… [Twins] have premature delivery and use up resources rapidly. [MD#1]
Discussion
These data, the first to examine how IVF providers and patients view and make decisions regarding fetal reductions, suggest several complications and dilemmas. Patients frequently have difficulty confronting the prospect of reduction and/or renege on prior agreements to reduce. Despite efforts to increase SET (Kissin et al., 2015) and evidence that it has fewer complications, patients and providers in many countries still frequently transfer more than one embryo (Practice Committees of the ASRM and SART, 2013; Haas et al., 2014), posing critical questions of why and what can be done. The present data suggest that many providers transfer additional embryos to increase the odds of a birth and assume that patients could reduce, if necessary, to avoid the risks faced by twins or multiple births. Patients may agree beforehand to a reduction, but later refuse. Providers should thus be wary about transferring additional embryos based on these assumptions, recognizing more fully the inaccuracy of these assumptions, and these patients’ difficulties and later refusals.
These decisions are hard for both providers and patients because of competing sets of risks and benefits, including potential harms (to mothers and children) with twins versus dangers of reduction (to the mother through surgery, and future child if the pregnancy is lost). Patients may feel they do not need to be concerned about increased risks of complications with twins, since the odds of each risk are <50%: 53.3% of twins are not premature and 61.2% have normal birth weights (Sazonova et al., 2013). However, from public health, institutional and systems perspectives, twin pregnancies result, cumulatively, in thousands of infants and mothers with complications.
Financial considerations can also arise. To save money, patients who want more than one child may oppose reductions. Physicians may also have conflicts of interest: in the competitive IVF market of many countries, doctors may try to retain and please, rather than ‘lose’ patients. Twins also increase the reported success per cycle rates of providers. Potential retrospective regret occasionally led to these interviewees transferring additional embryos, but did not clearly emerge as a factor for or against reduction.
In making these decisions, providers often prioritize patient autonomy over other ethical considerations but also have professional duties toward beneficence and non-maleficence to future children (who, as twins, may encounter complications) and to the mother’. Providers who transfer additional embryos frequently compel patients to struggle later with dilemmas about reduction and surgery. Providers also have responsibilities to justice, given the social costs of complications with twins.
Providers transferring additional embryos may thus be overvaluing autonomy; overestimating patients’ willingness to undergo reduction; and underappreciating risks twins face, emotional and financial difficulties patients confront, and patients’ minimization or denial of risks of twins (given desires for a child) and agreements to reduction solely as a precondition for transfer; and broader societal costs.
Clinicians may feel they have no responsibilities for these difficulties concerning reduction but they are generating problems that can cause harm. Providers may ignore these responsibilities and risks, partly since they themselves do not perform reductions or treat infants with subsequent complications and since twins can increase their revenue and success rates.
These data have critical implications for clinicians, patients, insurers, policymakers, researchers and others. In deciding how many embryos to transfer, providers should be as aware as possible of patients’ reluctance to reduce and how difficult reduction can be for patients, leading many patients to concur initially, and then renege. Providers should realize that patients may, at transfer, agree to potential future reductions because it is condition of the transfer, rather than reflecting the patients’ genuine consent or understanding of the risks.
Education of patients and providers is critical to ensure that they understand these issues, risks and inaccurate assumptions as much as possible. Such education can heighten awareness of the needs to pursue SET.
These data have implications for future research to investigate, among larger samples in various countries: how providers and patients perceive and make these decisions; how often providers and patients discuss possible reductions when transferring two or more embryos and once pregnancies of two or more fetuses result; how often physicians transfer more than one embryo due to assumptions about patients’ willingness to reduce then recommend or perform reductions; how often patients agree and then renege and which patients do so; what factors are involved (e.g., existence of prior children, religion, number of prior unsuccessful cycles and years of treatment) and how often births of twins or higher multiples result from patients reneging.
Professional organizations and governmental agencies in various countries should address these issues through recommendations and guidelines, to ensure that providers do not assume that transferring additional embryos is possible because of potential reduction. Governments can mandate that clinics publish data, including numbers of embryos transferred per cycle, and heighten transparency, further motivating adherence to SET. US providers report to SART and CDC live births per transfer, not per embryo transferred (SART, 2016) and hence commonly transfer more than one embryo, increasing reported birth rates. Reporting requirements in the US and in many other countries should thus change to require disclosures of success rates per embryo. Moreover, only 11 of 27 European countries in 2011 had individual clinic data publically available (Kupka et al., 2016). In 2006, clinic reporting was voluntary in most European countries (ESHRE, 2009). Reporting on twins’ complications could also further promote SET. Some countries (e.g., Belgium) link SET to reimbursement (De Neubourg et al., 2014). Insurers could cover several cycles if SET occurs, reducing costs of complications. Arguably, patients alone should not decide numbers of embryos transferred, except in certain cases, e.g., repeated IVF failure, if additional embryos significantly increase rates of success, but not of twins.
Patients perceive risks of additional embryos and twins not in isolation, but as part of larger tradeoffs, and are far more concerned with potential benefits (i.e. a child). Many, though not all, providers are more aware of the risks twins face, but tend to discount these dangers due to beliefs that the physicians’ primary goal is furthering, not impeding, childbirth, and that patients’ autonomy should prevail. Clinicians feel that increased odds of producing a child outweighs increased risks of twin complications. Beliefs about patient autonomy further justify this calculation, partly because these clinicians themselves do not treat these complications.
Physicians see the number of embryos transferred as the patients’ decision, but occasionally consider challenging patients’ refusals to reduce. These views are not contradictory, however; these providers benefit from multiple transfers, but are not harmed by refusals to reduce. Moreover, multiple transfers often lead to singletons, not twins, obviating the need for reductions.
These data have several potential limitations. The sample size is sufficient for qualitative research to elucidate the issues and themes that emerge, but not for statistically analyzing how different groups (e.g. male versus female physicians) may vary. Future studies can investigate these issues with larger samples.
These data are the first to examine how IVF providers and patients view and make decisions regarding the reduction of fetuses and thus have critical implications for future practice, guidelines, research and education of providers, patients, policymakers and others.
Supplementary data
Supplementary data are available at http://humrep.oxfordjournals.org/
Acknowledgements
The author would like to thank Daniel Marcus-Toll and Bela Fishbeyn for their assistance with data analysis, and Patricia Contino and Sarah Kiskadden-Bechtel for their assistance with the preparation of the manuscript.
Author's role
The author is solely responsible for conception, analysis, writing and editing of this paper.
Funding
Funding was provided by grant number UL1 RR024156 from the National Center for Research Resources, the Greenwall Foundation and the John Simon Guggenheim Foundation.
Conflict of interest
The author has no conflicts of interest to report.
References
- Antsaklis A, Souka AP, Daskalakis G, Papantoniou N, Koutra P, Kavalakis Y, Mesogitis S. Pregnancy outcome after multifetal pregnancy reduction. J Matern Fetal Neonatal Med 2004;16:27–31. [DOI] [PubMed] [Google Scholar]
- Balasubramanyam S. Knowledge and attitudes of women towards multiple embryo transfer, fetal reduction and multiple pregnancy. Int J Infertility Fetal Med 2010;1:31–34. [Google Scholar]
- Centers for Disease Control and Prevention, American society for Reproductive Medicine, Society for Assisted Reproductive Technology. 2013 Assisted Reproductive Technology National Summary Report. Atlanta, Georgia; US Department of Health and Human Services, 2015 http://www.cdc.gov/art/pdf/2013-report/art_2013_national_summary_report.pdf (9 September 2016, date last accessed).
- De Neubourg D, Peeraer K, Debrock S, D'Hooghe T. Belgium model of coupling reimbursement of ART costs to restriction in number of embryos transferred. BMJ 2014;348:g1559. [DOI] [PubMed] [Google Scholar]
- European Society of Human Reproduction and Embryology Comparative Analysis of Medically Assisted Reproduction in the EU: Regulation and Technologies – Final Report (2009). http://ec.europa.eu/health/blood_tissues_organs/docs/study_eshre_en.pdf. (8 August 2016, date last accessed).
- Evans MI, Kaufman MI, Urban AJ, Britt DW, Fletcher JC. Fetal reduction from twins to a singleton: a reasonable consideration. Obstet Gynecol 2004;104:102–109. [DOI] [PubMed] [Google Scholar]
- Geertz C. Interpretation of Cultures: Selected Essays. New York: Basic Books, 1973. [Google Scholar]
- Griffin D, Brown L, Feinn R, Jacob MC, Scranton V, Egan J, Nulsen J. Impact of an educational intervention and insurance coverage on patients’ preferences to transfer multiple embryos. Reprod Biomed Online 2012;25:204–208. [DOI] [PubMed] [Google Scholar]
- Guest G, Bunce A, Johnson L. How many interviews are enough? An experiment with data saturation and variability. Field Methods 2006;18:59–82. [Google Scholar]
- Haas J, Mohr Sasson A, Barzilay E, Mazaki Tovi S, Orvieto R, Weisz B, Lipitz S, Yinon Y. Perinatal outcome after fetal reduction from twin to singleton: to reduce or not to reduce. Fertil Steril 2015;103:428–432. [DOI] [PubMed] [Google Scholar]
- Haas J, Hourvitz A, Dor J, Yinon Y, Elizur S, Mazaki-Tovi S. Pregnancy outcome of early pregnancy reduction: triplets to twins versus triplets to singletons. Reprod Biomed Online 2014;29:717–721. [DOI] [PubMed] [Google Scholar]
- Hasson J, Shapira A, Many A, Jaffa A, Har-Toov J. Reduction of twin pregnancy to singleton: does it improve pregnancy outcome. J Matern Fetal Neonatal Med 2011;24:1362–1366. [DOI] [PubMed] [Google Scholar]
- The Human Fertilisation and Embryology Authority (HFEA) Report: Fertility Treatment 2013: Trends and Figures. http://www.hfea.gov.uk/docs/HFEA_Fertility_Trends_and_Figures_2013.pdf/. (8 August 2016, date last accessed).
- Jungheim ES, Ryan GL, Levens ED, Cunningham AF, Macones GA, Carson KR, Beltsos AN, Odem RR. Embryo transfer practices in the United States: a survey of clinics registered with the Society for Assisted Reproductive Technology. Fertil Steril 2010;94:1432–1436. [DOI] [PubMed] [Google Scholar]
- Kissin DM, Boulet SL, Adashi EY. Yes, elective single-embryo transfer should be the standard of care In: Carrell DT, Schlegel PN, Racowsky C, Gianaroli L (eds). Biennial Review of Infertility, Vol. 4 (Part 4). New York: Springer International Publishing, 2015,177–187. [Google Scholar]
- Klitzman R, Daya S. Challenges and changes in spirituality among doctors who become patients. Soc Sci Med 2005;61:2396–2406. [DOI] [PubMed] [Google Scholar]
- Klitzman R, Thorne D, Williamson J, Chung W, Marder K. Disclosures of Huntington disease risk within families: patterns of decision-making and implications. Am J Med Genet 2007;143A:1835–1849. [DOI] [PubMed] [Google Scholar]
- Klitzman R. Institutional review board community members: who are they, what do they do, and whom do they represent. Acad Med 2012;87:975–981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klitzman R, Appelbaum PS, Fyer A, Martinez J, Buquez B, Wynn J et al. . Researchers’ views on return of incidental genomic research results: qualitative and quantitative findings. Genet Med 2013;15:888–895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klitzman R. How good does the science have to be in proposals submitted to Institutional Review Boards? An interview study of Institutional Review Board personnel. Clin Trials 2013;10:761–766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klitzman R. How old is too old? Challenges faced by clinicians concerning age cutoffs for patients undergoing in vitro fertilization. Fertil Steril 2016. doi:10.1016/j.fertnstert.2016.03.030.pii: S0015-0282(16)39058-6 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- Kulkarni AD, Jamieson DJ, Jones HW, Kissin DM, Gallo MF, Macaluso M, Adashi EY. Fertility treatments and multiple births in the United States. New Engl J Med 2013;369:2218–2225. [DOI] [PubMed] [Google Scholar]
- Kupka MS, D'Hooghe T, Ferraretti AP, de Mouzon J, Erb K, Castilla JA, Calhaz-Jorge C, De Geyter C, Goossens V. The European IVF-monitoring (EIM) Consortium for the European Society of Human Reproduction and Embryology (ESHRE). Assisted reproductive technology in Europe, 2011: results generated from European registers by ESHRE. Hum Reprod 2016;31:233–248. [DOI] [PubMed] [Google Scholar]
- Leese B, Denton J. Attitudes towards single embryo transfer, twin and higher order pregnancies n patients undergoing infertility treatment: a review. Hum Fertil 2010;13. Published online 8 Feb 2010. [DOI] [PubMed] [Google Scholar]
- Munks EB, Edelman AB, Jensen JT, Nichols MD, Burry K, Patton P. IVF patients’ attitudes toward pregnancy reduction. J Reprod Med 2007;52:635–638. [PubMed] [Google Scholar]
- Osterman MJ, Kochanek KD, MacDorman MF, Strobino DM, Guyer B. Annual summary of vital statistics: 2012–2013. Pediatrics 2015;135:1115–1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pison G, Monden C, Smits J. Twinning rates in developed countries: trends and explanations. Popul Dev Rev 2015;41:629–649. [Google Scholar]
- The Practice Committee of the American Society for Reproductive Medicine Multiple gestation associated with infertility therapy: an American Society for Reproductive Medicine Practice Committee opinion. Fertil Steril 2012;97:825–834. [DOI] [PubMed] [Google Scholar]
- The Practice Committee of the American Society for Reproductive Medicine and the Practice Committee of the Society for Assisted Reproductive Technology Criteria for number of embryos to transfer: committee opinion. Fertil Steril 2013;99:44–46. [DOI] [PubMed] [Google Scholar]
- SART CORS National Summary Report 2016: All SART Member Clinics. https://www.sartcorsonline.com/rptCSR_PublicMultYear.aspx?ClinicPKID=0 (8 August 2016, date last accessed).
- Sazonova A, Källen K, Thurin-Kjellberg A, Wennerholm UB, Bergh C. Neonatal and maternal outcomes comparing women undergoing two in vitro fertilization (IVF) singleton pregnancies and women undergoing one IVF twin pregnancy. Fertil Steril 2013;99:731–737. [DOI] [PubMed] [Google Scholar]
- Stone J, Belogolovkin V, Matho A, Berkowitz RL, Moshier E, Eddleman K. Evolving trends in 2000 cases of multifetal pregnancy reduction: a single-center experience. Am J Obstet Gynecol 2010;197:394.e1–394.e4. [DOI] [PubMed] [Google Scholar]
- Strauss A, Corbin J. Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory. Newbury Park, CA: Sage Publications, 1990. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.