Abstract
Background.
The Lithuanian Perinatology Program, orders issued by the Ministry of Health, regulating the care and treatment of mothers and their infants, and the well-running perinatal care system helped to improve the diagnostics and treatment of pregnancy pathology. Over the last 20 years, Lithuania has experienced significant improvements in the maternal and perinatal health.
Materials and methods.
Data was collected from the official statistics database, Medical Data of Births, provided by the Institute of Hygiene Health Information Centre, Vilnius University Faculty of Medicine, and the Vilnius University Centre of Neonatology in 1995–2014.
Results.
The average maternal age at delivery ranged from 25.8 years in 1995 to 28.8 years in 2014. The comparison of 2001 and 2014 data shows that the incidence of gestational diabetes increased by 6.7 times due to the improved diagnosis. The percentage of hypertensive disorders decreased from 6.1% in 1997 to 3.2% in 2014. Between 1995 and 2014, the prevalence of anemia among pregnant women declined by half. The marked decrease in respiratory, urinary, genital and other diseases was observed among pregnant women. From 1995 to 2014, in Lithuania there were 67 maternal deaths related to pregnancy and childbirth. Hemorrhage and infections during pregnancy, delivery and the postpartum period are considered the most common causes of maternal death.
Keywords: Lithuanian perinatology centres, maternal morbidity, mortality
Abstract
LIETUVOS NĖŠČIŲJŲ LIGŲ DINAMIKA 1995–2014 METAIS
Santrauka
Lietuvoje veikianti perinatologijos programa, Sveikatos apsaugos ministerijos įsakymai, reglamentuojantys nėščiųjų, gimdyvių ir naujagimių priežiūrą bei gydymą, ir gerai veikianti nėščiųjų priežiūros visų grandžių sistema leido pagerinti patologinių nėštumo būklių diagnostiką ir gydymą. Per dvidešimt pastarųjų metų Lietuvos nėščiųjų, gimdyvių ir moterų po gimdymo sveikata itin pagerėjo. Pirmą kartą gimdančių moterų amžius padidėjo nuo 25,8 (1995) iki 28,8 metų (2014). Lyginant 2001 ir 2014 m. duomenis, nėščiųjų diabeto atvejų dėl pagerėjusios getacinio diabeto diagnostikos padaugėjo 6,7 karto. Nėščiųjų, sirgusių hipertenzinėmis būklėmis, sumažėjo nuo 6,1 (1997) iki 3,2 % (2014). Lyginant 1995 ir 2014 m. duomenis, mažakraujyste sergančiųjų nėščiųjų sumažėjo perpus. Sergamumas kvėpavimo organų, inkstų ir šlapimo takų, lytinių organų ir kitomis ligomis taip pat sumenko. 1995–2014 m. Lietuvoje mirė 67 nėščiosios ir gimdyvės. Dažniausios mirties priežastys buvo kraujavimas nėštumo laikotarpiu, gimdymo metu ir po gimdymo bei infekcinės komplikacijos.
Raktažodžiai: Lietuvos perinatologijos centrai, nėščiųjų ir gimdyvių sergamumas ir mirtingumas
INTRODUCTION
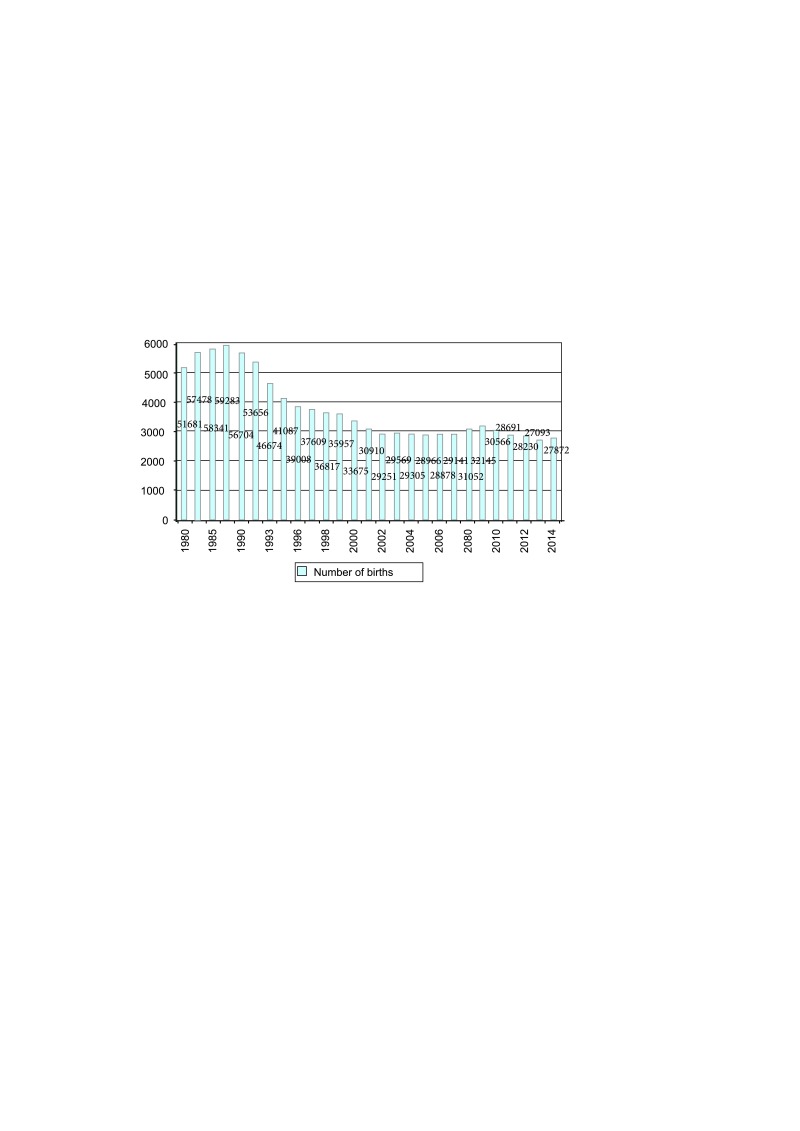
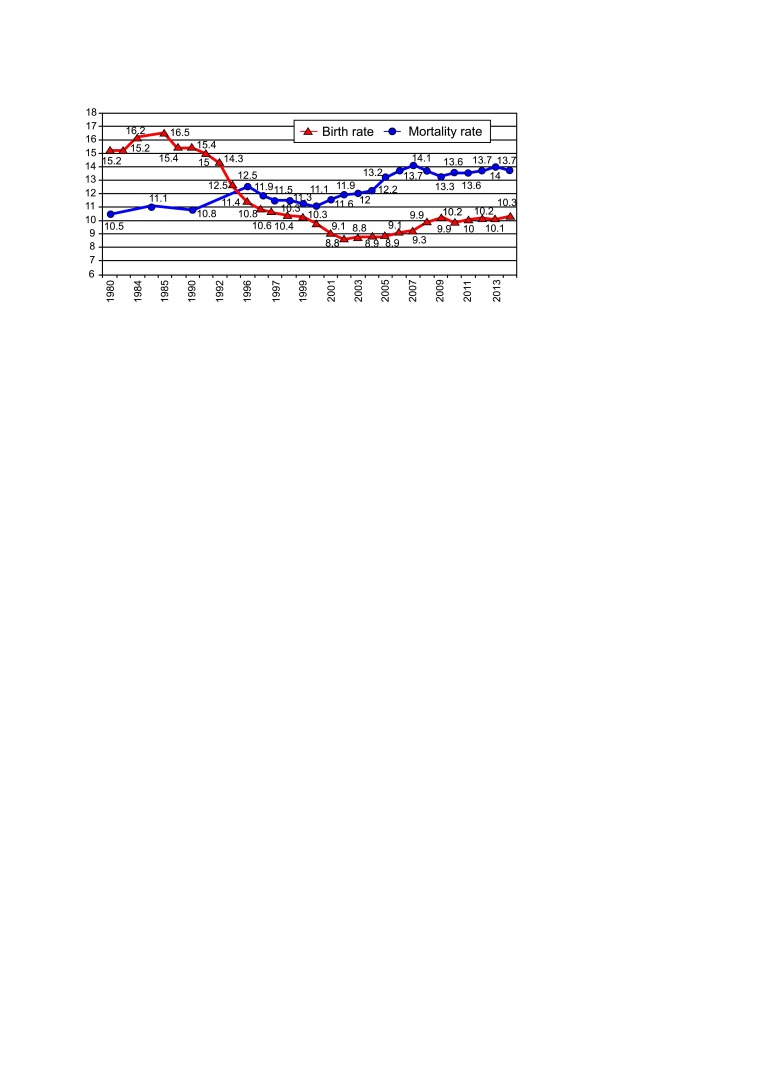
The current Lithuanian demographic situation, low birthrate, and negative natural population growth make physicians, especially obstetricians and gynaecologists, neonatologists, perinatologists and family doctors, commit themselves to giving all possible help to every pregnant woman to have a healthy baby. External factors such as poor nutrition, smoking, lack of physical activity, and changing living conditions can affect the infant’s health. Maternal morbidity has a great effect on the fetus growth and health. During the last 20 years, the number of childbirths was continuously decreasing and the changes in the mortality curve for general population were not positive (Figs. 1, 2). The natural population growth became negative since 1995, whereas not so long ago, 80 years before, Lithuanian demographic indicators were quite different and very promising. About 85% of children, born in 1934–1936, were rural children, and only 15% were born in towns (7). Many babies were born in families and only a small part of births were to unmarried women. We have withstood the test of the epoch trends and today we face the challenges of the Lithuanian perinatal medicine in the light of the last 20 years.
After the restoration of Lithuanian Independence in 1990, it was possible to develop the perinatal and neonatal healthcare system corresponding to the situation in our country and international standards. The Order of the Health Minister of 19 December 1990 (1) legitimated the registration of the preterm birth from the 22nd week of gestation and 500 g body mass according to the WHO recommendations. The Medical Data of Birth published in 1993 on the initiative of the Vilnius University Neonatology Clinics and perinatologists (6) allow systematizing the data related with the fetal, neonatal and prenatal health and setting directions leading to high-quality life for new generations.
Lithuania took the first steps towards the medicine reform. The Order of the Health Minister of 26 February 1992 No. 74 (2) approved the Program for Prevention of Perinatal, Neonatal, Hereditary Diseases and Congenital Defects. The main objective of this program was to reduce morbidity and mortality during the perinatal period – pregnancy, childbirth and the postpartum, to decrease the incidence of central nervous system disorders during pregnancy and childbirth, and to control congenital anomalies. To implement this objective based on the regional principle the following three-stage perinatology system has been created: in-patient obstetric and neonatal care units were equipped with the necessary facilities, and two perinatology centres were established in Vilnius and Kaunas.
Fig 1.
Births in Lithuania, 1980–2014
Fig 2.
Birth and mortality rates in Lithuania, 1980–2014
Taking into account the positive changes in the Lithuanian socioeconomic development, the Ministry of Health issued and perfected the orders regulating the care of mothers and their babies to help the purposeful team of obstetricians gynaecologists and neonatologists. Orders of the Minister of Health No. 117 (4) and No. 900 of September 2013 (5) were issued.
The systemic work in Lithuania and the great help of the Switzerland’s Government were fruitful: Lithuania achieved the same level as the developed countries concerning the following indicators: perinatal and neonatal mortality ratios were reduced, we started medical birth registry and analysis. The aim of this paper is to summarize the 1995–2014 changes in the demographic and morbidity indicators and to compare them with the statistics of the maternal health in Europe.
MATERIALS AND METHODS
A retrospective analysis of the data was performed. Data were collected from the official statistics database Medical Data of Births, provided by the Institute of Hygiene Health Information Centre, Vilnius University Faculty of Medicine, and the Vilnius University Centre of Neonatology. In this study we have analysed the 1995–2014 data on maternal morbidity in Lithuania and the related factors: age, smoking, pregnancy pathology and maternal morbidity. We compared these data with the official data of the European Perinatal Health Report 2004–2010 published in 2013 (8). The large for gestation fetuses weighing over 4 000 g were considered as macrosomia. All the provided data is in numbers (percentage). Maternal mortality ratio was counted as the number of women who have died from pregnancy-related causes while pregnant or within 42 days after delivery per 100 000 live births.
RESULTS
During the 1995–2014 period, there were 633 078 childbirths and 642 583 neonates, i. e. 9 505 newborns more than births (6).
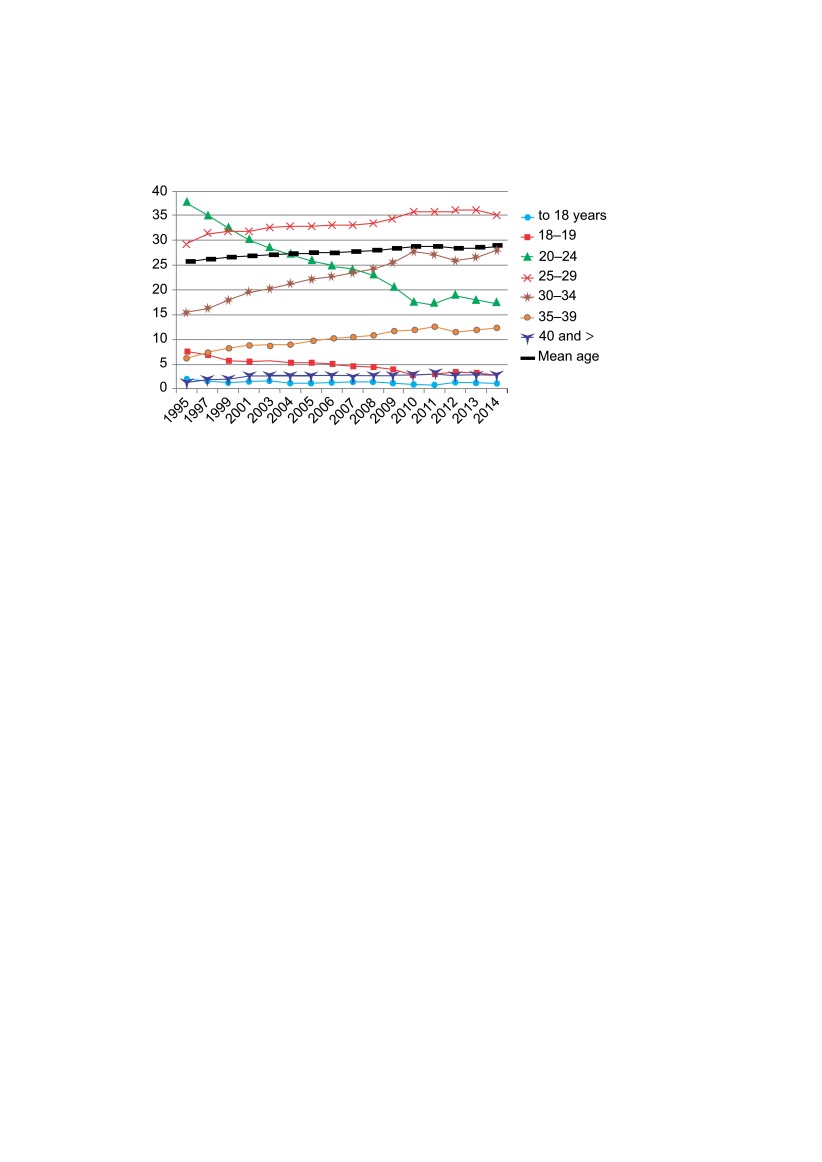
Maternal age. With a decrease of births in Lithuania, childbearing and pregnancy age increased. There was a substantial increase in the proportion of pregnancy at elder age. In 2014, this ratio was 28.8 years, as compared to 25.8 years in 1995. In 2014, the proportion of mothers aged 18–19 was almost threefold lower than that in 1995, 3 123 (7.6%) in 1995 and 819 (2.9%) in 2014, respectively. The number of mothers in the age group of 20–24 years decreased by 3 times in this period, from 15 572 (37.9%) to 4 890 (17.5%). The rate of mothers aged 30–34 increased from 6 327 (15.4%) to 7 780 (27.9%). The percentage of 40 years old and elder mothers doubled, from 575 (1.4%) to 803 (2.9%). The reasons for late childbearing can be low female mortality, social status, long-lasting education, career, and financial issues (Fig. 3).
Smoking during pregnancy may be considered the most important preventable factor associated with adverse pregnancy outcomes. It can impair normal fetal growth and thus increase the risk of low birth weight, preterm birth, and some congenital anomalies. Smoking cessation during pregnancy thus serves as an indicator of the quality of antenatal preventive health services. During the 1995–2014 period, the percentage of Lithuanian pregnant smokers varied insignificantly: 4.8% in 2004, 4.5% in 2010, and 5% in 2014. About 40% of women stopped smoking during their pregnancy.
Fig 3.
Different maternal age groups, percentage of all pregnancies
During the 1995–2014 period, an increase in macrosomia cases was observed. About 14–16 women in 100 gave birth to the newborns weighing 4 000 g and more. This rate was the least in 2001–2004, 3 983 (13.5%) – 4 319 (13.9%), and the highest in 2008–2010, 4 453 (14.4%) – 5 041 (15.5%). Poor nutrition is not the only determinant of macrosomia, but this factor has a great influence on the mother’s overweight and also on the baby’s weight.
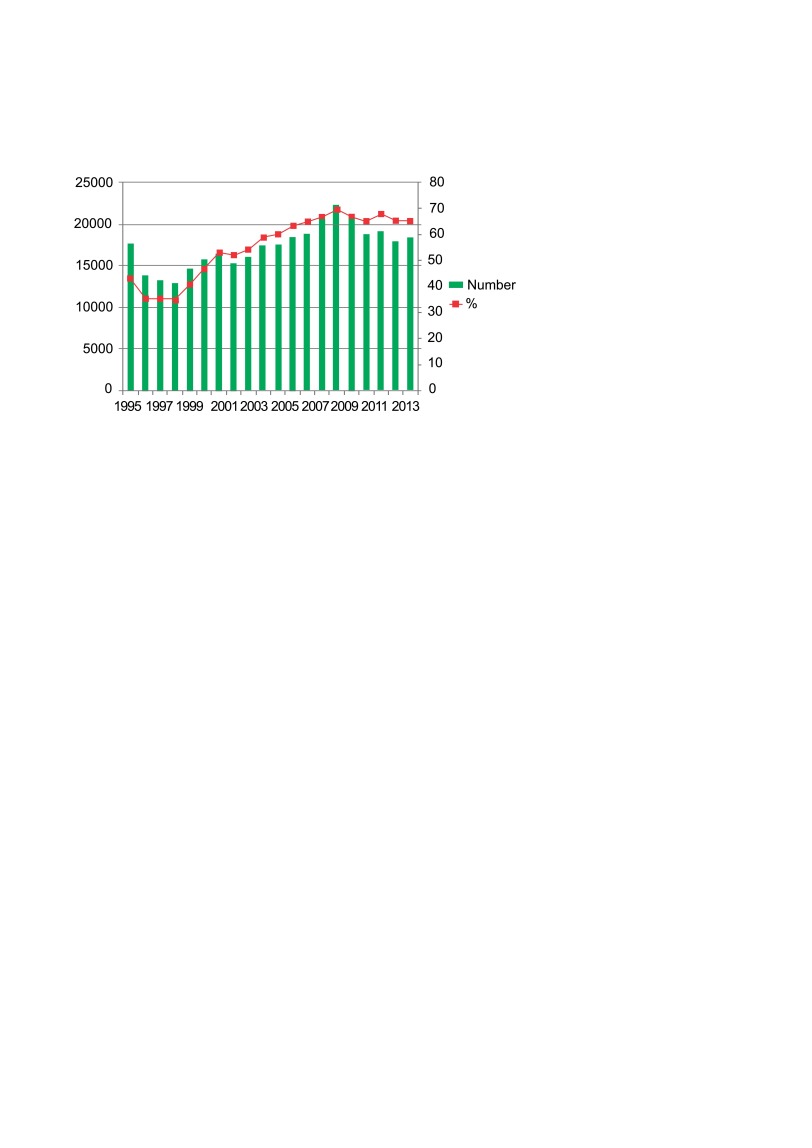
On the one hand, the published data reveals that 66% of Lithuanian pregnant women had no comorbidities in 2014, while 20 years ago there were 40% of such women. On the other hand, the rates of pregnancy pathology have been decreasing during the last 20 years. Thus we can state that there were positive changes in the health of fertile age women (Fig. 4).
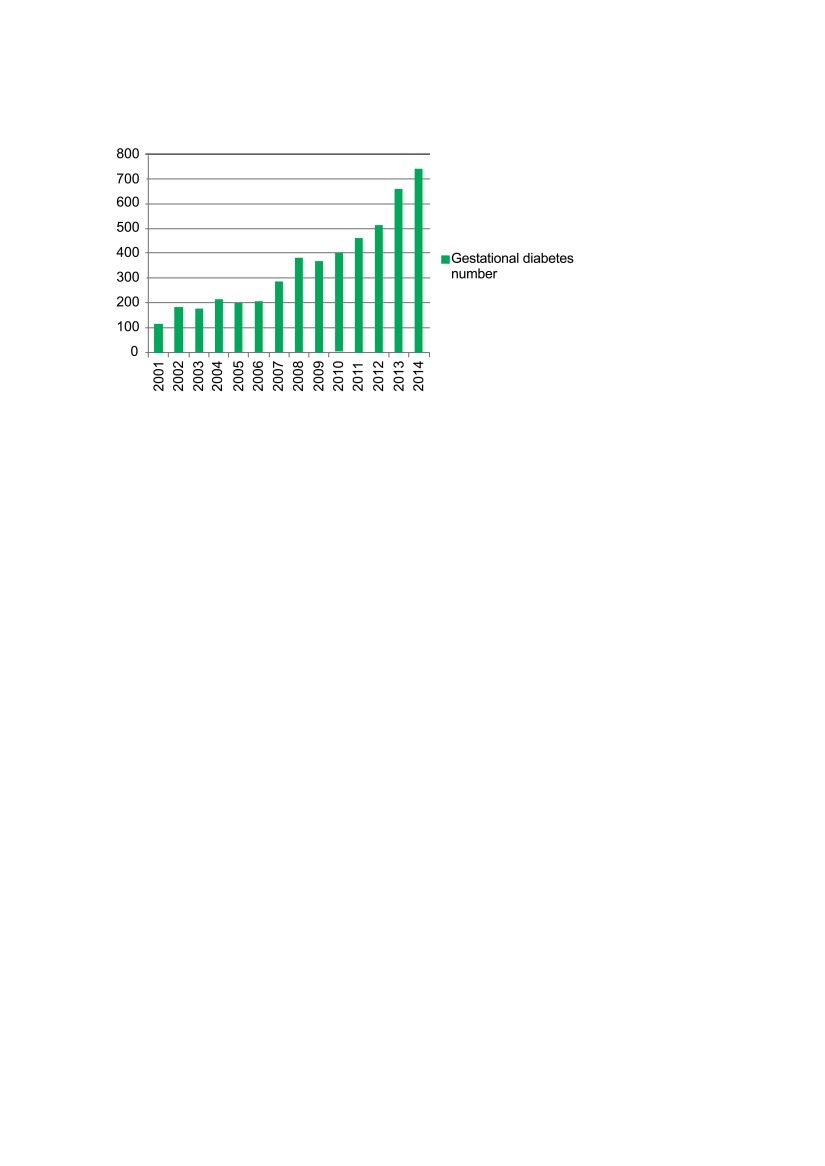
Evaluating maternal morbidity during the period of interest, the greatest increase observed was in the proportion of gestational diabetes. In 2004, there were 219 (0.7%) cases of gestational diabetes in pregnant women, as compared with 413 (1.3%) in 2010, and 757 (2.7%) cases in 2014 (Fig. 5). It is most likely that the increase was related to the released order of the Ministry of Health, concerning prenatal care in Lithuania, and the recommendation to perform the screening test of glucose tolerance in the high risk pregnant women population. From 2004 to 2014, the number of pregnant women with type II diabetes increased by 8 times, i. e. from 3 (0.0%) to 26 pregnant women (0.1%). This can be related to the elder age of mothers and the higher body mass index in the Lithuanian population.
Fig 4.
Lithuanian healthy pregnant women, 1995–2014
Fig 5.
Gestational diabetes in Lithuania, 2001–2014
The number of urinary infections also decreased. The complications of these diseases are often severe. For example, urosepsis is one of the maternal death causes. The percentage of urinary infections in 2014 decreased by more than one third: it was 1 165 (4.2%) as compared to 617 (6.7%) in 1995. Genital infections are closely related with kidney and urinary infections. Up to 2 000 cases were diagnosed to every third or fourth pregnant woman. The highest ratio of genital infections in the period between 1995 and 2000 was reported in 1998 – 11 775 (32%), later this ratio decreased, and in 2014 it fell to 3 556 (12.8%). Over the 2004–2014 period, the percentage of respiratory diseases in pregnant women decreased by one third (34%), 2 363 (8.1%) in 2004 and 1 554 (5.6%) in 2014, respectively.
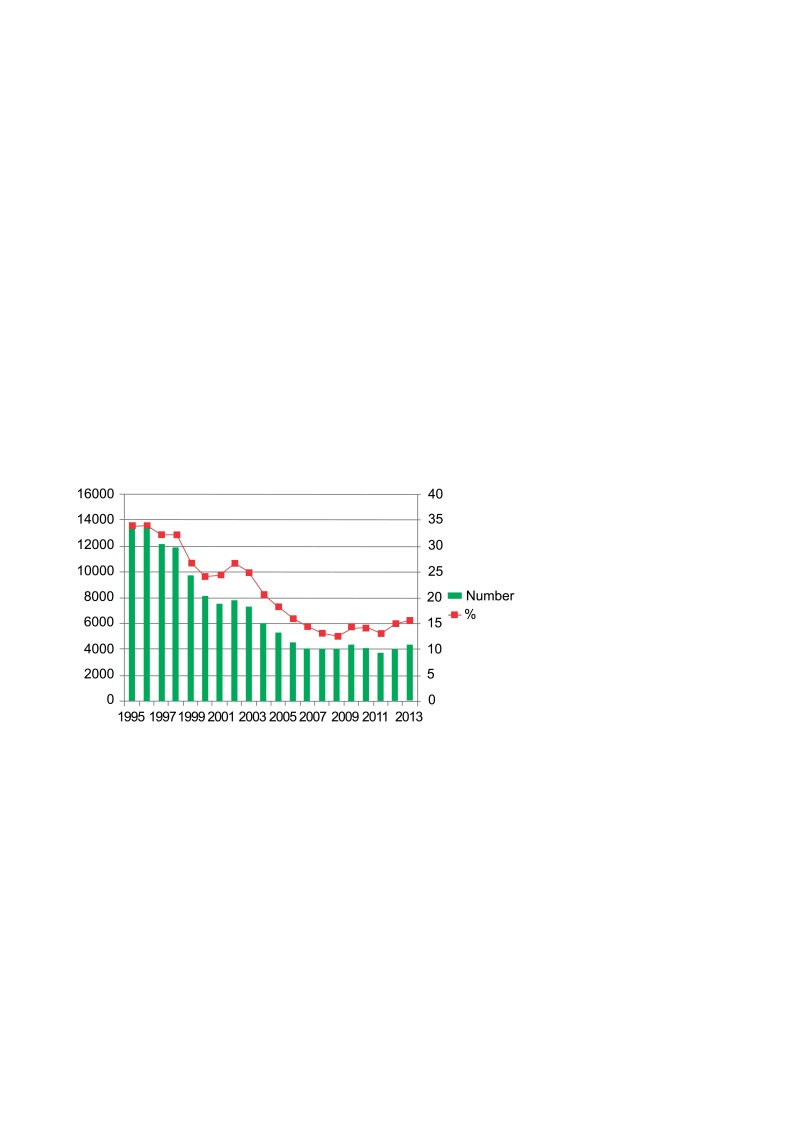
Some diseases are typical of pregnancy. One of them is pregnancy-related anemia. The proportion of pregnant women with anemia decreased by half: it was diagnosed to 4 385 (15.7%) pregnant women in 2014 as compared to 13 886 (34%) in 1995. These changes occurred due to the introduction of blood serum ferritin tests to clinical practice and iron therapy (Fig. 6).
Fig 6.
Pregnancy-related anemia in Lithuania, 1995–2014
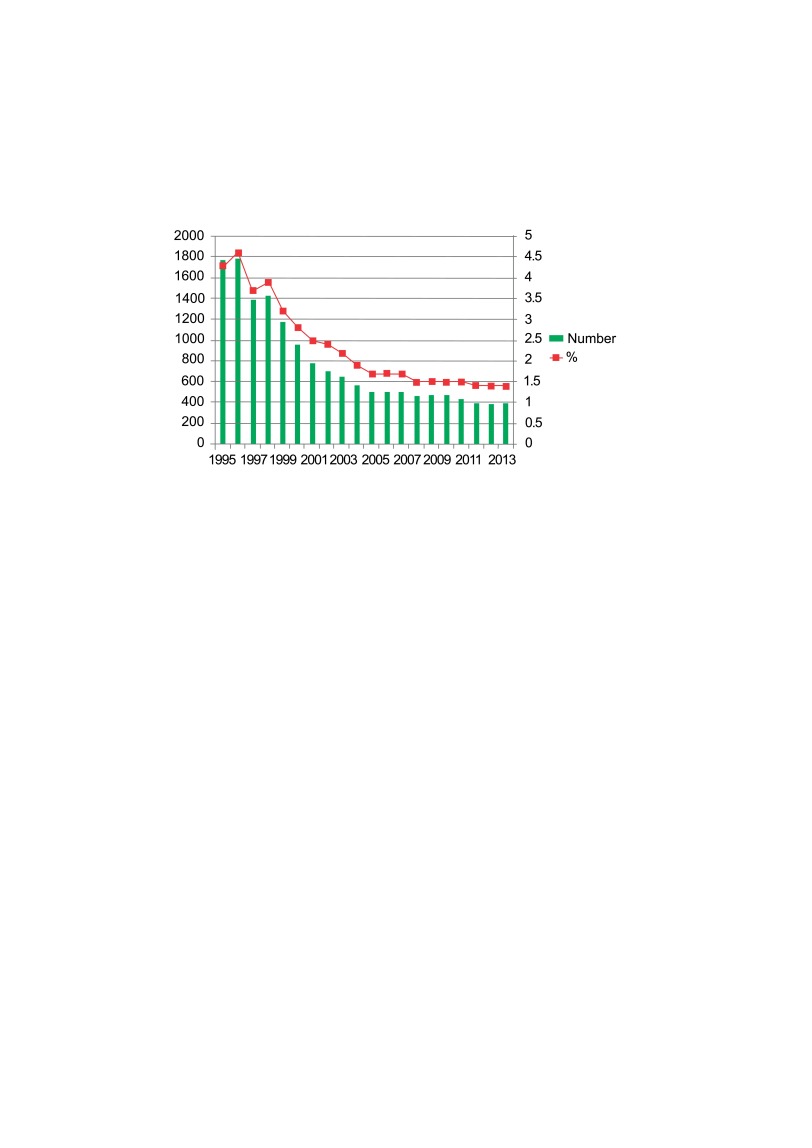
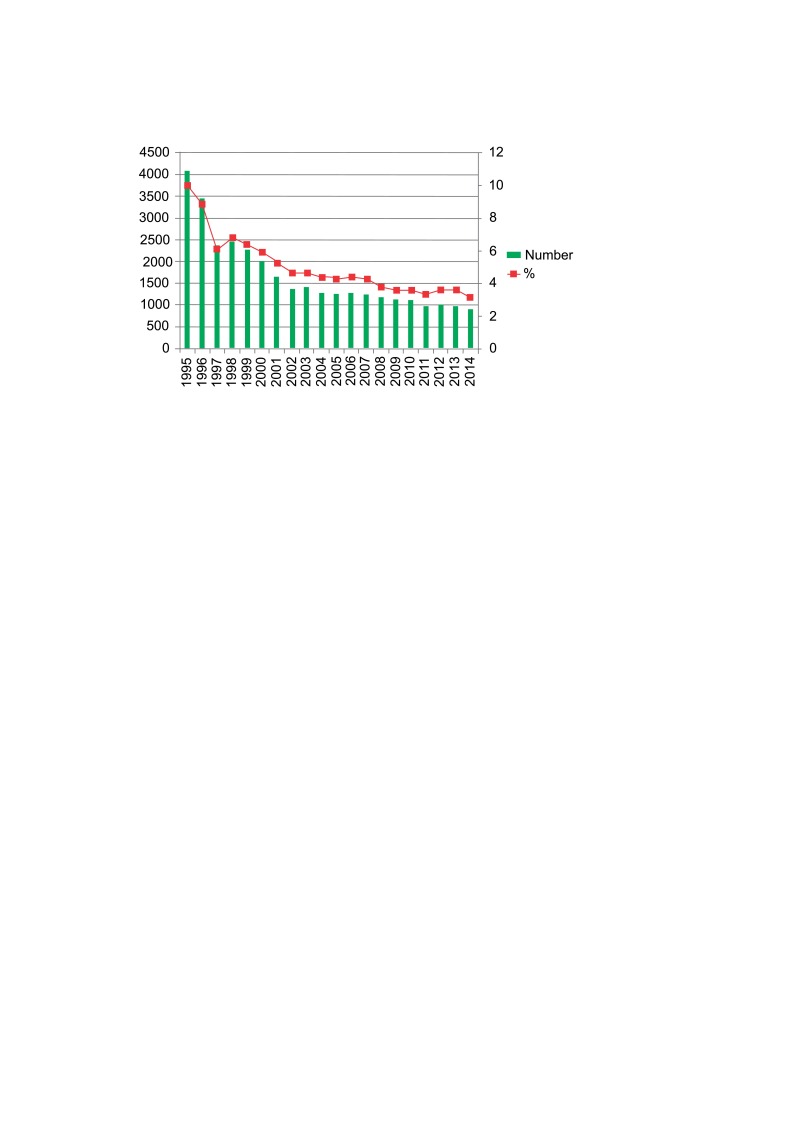
There was a decrease in the proportion of cardiovascular diseases and hypertensive disorders. In the 20-year period, the significant decrease of cardiovascular diseases morbidity ratio by two thirds was noted: 1 774 (4.3%) in 1995 and 393 (1.4%) in 2014 (Fig. 7). Similarly, the threefold reduction of hypertensive disorders rate was reported (1995: 4 075, 10% vs 2014: 899, 3.2%) (Fig. 8). The risk factors of hypertensive disorders in pregnancy – the first pregnancy, age elder than 35 years, multiple pregnancy, overweight, obesity, family history – are also specific for the studied period in Lithuania. The incidence of preeclampsia did not change: about 1.3–1.9% of mothers were diagnosed with this pathology annually.
Data on preterm rupture of membranes, genital infections and threatened abortion are interdependent. Thus, in case of decrease in genital infections, preterm ruptures of membranes also decrease, and positive changes are observed in threatened abortion incidence. The rate of premature birth in Lithuania is 5–6%.
Unfortunately, in 1995–2014 there were 67 maternal deaths in Lithuania related to pregnancy and childbirth. Over the 1995–2014 period, the maternal mortality ratio varied between 20.3/100 000 live births to 0.00/100 000, with 15.09/100 000 live births being the average of the first decade (1995–2004) and 6.26/100 000, the average of the last decade (2005–2014) (Fig. 9).
Fig 7.
Cardiovascular diseases in pregnant women in Lithuania, 1995–2014
Fig 8.
Hypertensive disorders in pregnant women in Lithuania, 1995–2014
Fig 9.
Maternal death ratios in Lithuania, 1995–2014
DISCUSSION
The data of the European Perinatal Health Report 2004–2010 show that the maternal age in all European Union countries increased. The only exception was Finland, there the mean maternal age decreased. The prime childbearing age in Europe is 25–35 years. The maternal age in Europe varies widely, and this might have an impact on the health of mothers and infants. According to the literature, early and late childbearing are associated with higher than average rates of growth restriction, preterm birth, perinatal mortality, and even congenital anomalies. Overall, teenage pregnancies are uncommon in Europe with a median of 2.7% of births to mothers aged younger than 20 years. However, some countries of Eastern Europe, including Lithuania with 3.8%, have higher proportions. In the UK there are a higher proportion of very young mothers (over 5%).
The percentage of elder mothers, defined as women giving birth at 35 years or older, ranged from 10.9% in Romania to 34.7% in Italy. In most of the countries at least 20% of births were to women aged 35 years or more, and the proportion of births in this age group increased substantially in almost every country. Only Finland experienced a decrease in this proportion between 2004 and 2010. In 2010, in Lithuania 14.9% of pregnant women were aged 35 years and more. From 2004 to 2010, the number increased by over 3%. The increase was relatively small in the United Kingdom (under 1%), and larger (over 5%) in Italy, Estonia, Hungary, the Czech Republic and Spain. Encouraging earlier childbearing may require policies to support young parents and working mothers, as well as informing the public about possible consequences of having children at later age.
In many European countries more than 10% of women continued smoking during their pregnancy. Lithuania has the lowest proportion in Europe, i. e. less than 5% of pregnant smokers, as compared with 15% in Northern Ireland, 16% in Wales, 17.1% in France, and 19% in Scotland. Countries that had data points for 2004 and 2010 reported slightly lower proportions of smokers in the last trimester in 2010 – by about 1–3%. Although in Lithuania there is no specific differentiation of smokers in pregnancy trimesters, we have data that about 40% of women stop smoking while being pregnant. Pregnancy care is considered the best time for providing information of the adverse effects of smoking on fetal and infant health. It must be noted that having high quality and comparable information on smoking before and during pregnancy should be a priority.
In Europe maternal deaths are rare, but it is strongly recommended that an analysis of their causes is essential for developing policies to reduce the death ratio. According to the data of the European Perinatal Health Report 2006– 2010, the highest ratios were observed in Latvia and Romania with 24.5 and 21.0 per 100 000 live births, respectively, compared to 2.5 in Italy, 2.6 in both Austria and Estonia, and 2.9 in Poland. Lithuania is somewhere in an intermediate position – the maternal death ratio is 4.1/100 000 live births for the mentioned period. The main causes of maternal death are obstetrical hemorrhage and hypertensive disorders (0.87/100 000 and 0.72/100 000 live births, respectively). Infections during pregnancy (chorioamnionitis, sepsis) and amniotic fluid embolisms are rather common causes of maternal mortality. In the last 20 years, there were 67 maternal deaths in Lithuania related to pregnancy and childbirth, as compared to 400 maternal deaths annually in the interwar years.
CONCLUSIONS
1. The Lithuanian Perinatology Program, orders issued by the Ministry of Health, regulating the care and treatment of mothers and their infants, and the well-running perinatal care system helped to improve the diagnostics and treatment of pregnancy pathology.
2. Over the last 20 years, Lithuania has experienced significant improvements in the perinatal health. The marked decrease in cardiovascular, respiratory, urinary and genital morbidity was observed among pregnant women. The percentage of gestational diabetes increased by 6.7 times due to improved diagnostics.
3. There were 67 maternal deaths related to pregnancy and childbirth in Lithuania during 1995–2014. Hemorrhage and infections during pregnancy, delivery and the postpartum period are considered the most common causes of maternal death.
References
- Lietuvos Respublikos sveikatos apsaugos ministro 1990 m. Gruodžio 19 d. įsakymas Nr. 417 „Dėl naujagimio (vaisiaus) gyvybingumo kriterijų ir registravimo tvarkos pakeitimų“. Lithuanian. [Google Scholar]
- Lietuvos Respublikos sveikatos apsaugos ministro 1992 m. Vasario 26 d. įsakymas Nr. 74 „Dėl perinatalinės, neonatalinės paveldimų ligų ir įgimtų vystymosi defektų profilaktikos programos vykdymo“. Lithuanian. [Google Scholar]
- Lietuvos Respublikos sveikatos apsaugos ministro 1999 m. Lapkričio 19 d. įsakymas Nr. 499 „Dėl akušerijos paslaugų teikimo“, Žin., Nr. 99-2870 (1999). Lithuanian. [Google Scholar]
- Lietuvos Respublikos sveikatos apsaugos ministro 1999 m. Kovo 15 d. įsakymas Nr. 117 „Dėl nėščiųjų, gimdyvių ir naujagimių sveikatos priežiūros tvarkos patvirtinimo“, Žin., Nr. 28-811 (1999). Lithuanian. [Google Scholar]
- Lietuvos Respublikos sveikatos apsaugos ministro 2013 m. Rugsėjo 23 d. įsakymas Nr. V-900 „Dėl nėščiųjų, gimdyvių ir naujagimių sveikatos priežiūros tvarkos aprašo patvirtinimo“, Žin., Nr. 102- 5056 (2013). Lithuanian. [Google Scholar]
- Gimimų medicininiai duomenys 1993, 1994, 1995 ... 2014 m. [Medical Data of Births in Lithuania]. Higienos instituto Sveikatos informacijos centras, Vilniaus universiteto Medicinos fakultetas, Vilniaus universiteto Neonatologijos centras. Lithuanian: Available from: www.hi.lt [Google Scholar]
- Kauno sveikatos biuletenis, 1934–1936 metai. Lithuanian. [Google Scholar]
- Euro-Peristat Project with SCPE and EUROCAT. European Perinatal Health Report. The health and care of pregnant women and babies in Europe in 2010. May 2013. [Google Scholar]