Abstract
Point-of-care (POC) ultrasonography is considered fundamental in emergency medicine training and recently has become a milestone in critical care fellowship programs as well. Currently, there is no such standard requirement for internal medicine residency programs in the United States. We present a new case and briefly review another case at our institution – a community hospital – in which internal medicine house staff trained in ultrasonography were able to uncover unexpected and critical diagnoses that significantly changed patient care and outcomes. We also review the growing evidence of the application of ultrasound in the diagnosis of a myriad of conditions encountered in general internal medicine as well as the mounting data on the ability of internal medicine residents to apply this technology accurately at the bedside. We advocate that the literature has sufficiently established the role of POC ultrasonography in general internal medicine that there should no longer be any delay in giving this an official place in the development of internal medicine trainees. This may be particularly useful in the community hospital setting where 24-h echocardiography or other sonography may not be readily available.
Keywords: ultrasonography, internal medicine, residents, point-of-care, medical education
In 1988, Filly called ultrasound technology ‘the stethoscope of the future’ (1). It was around that time that, much indeed like the stethoscope that is used at the point of patient care, ultrasound began to establish its bedside niche in emergency medicine (2). Since then, competence in ultrasound has become required in emergency medicine training (3, 4). In more recent years, ultrasound has started to become established within the critical care setting as well. A consensus statement by the American College of Chest Physicians has defined competence and established standards for proficiency in ultrasonography for intensivists and pulmonologists alike (5). Facility with various applications of point-of-care (POC) ultrasound is now considered a curricular milestone for graduates of pulmonary and critical care fellowship programs (6). Recognition of the utility of bedside ultrasound has also reached the surgical specialties with the American College of Surgeons offering training programs therein (7).
Despite this growing application of ultrasonography in various disciplines, a similar commitment has yet to be established within the internal medicine community. Competence in ultrasound is not considered a milestone in internal medicine training in the United States (8). A recent national survey of members of the Association of Program Directors in Internal Medicine revealed that only one-fourth of respondents (most of whom were program directors or associate program directors) had any formal curriculum for training their house staff in POC ultrasonography (9). By contrast, in some European nations, bedside ultrasound training is well established as part of medical training (10, 11).
In this article, we present a new case as well as a review of a recent case from our institution in which trained internal medicine residents were able to use POC ultrasonography to reveal unexpected and critical diagnoses that significantly altered a patient's course. We then review the growing evidence that ultrasonography is useful in the evaluation of various conditions encountered in internal medicine as well as the evidence that residents are, indeed, able to apply this technology at the bedside. As such, we contend that there should no longer be any delay in making POC ultrasonography a standard part of internal medicine training.
Cases
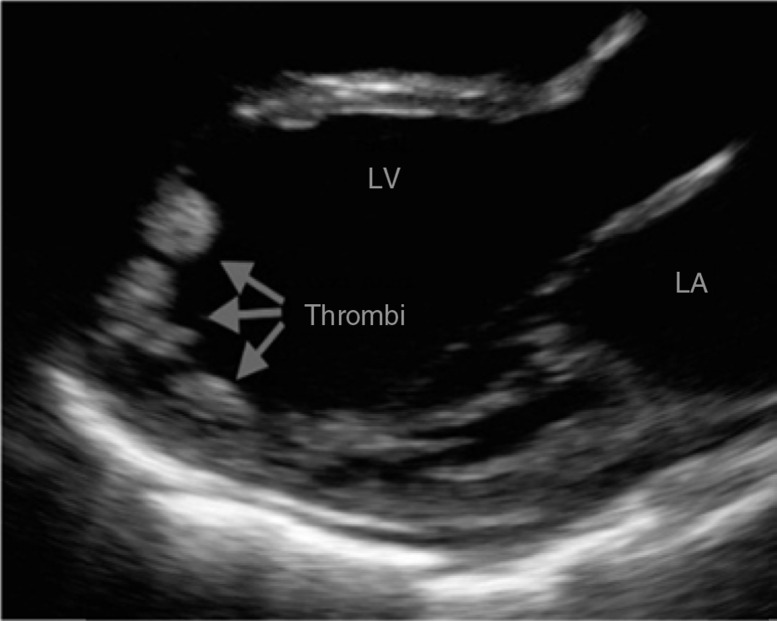
A previously healthy 20-year-old man presented to our community emergency department with nausea, vomiting, and generalized weakness for 1 month. He had undergone an extensive outpatient evaluation with normal imaging and laboratory studies and an esophagogastroduodenoscopy revealing only reflux gastritis. He remained without a diagnosis. Vital signs included a blood pressure of 100/73 mmHg, heart rate 105 bpm, and 95% oxygen saturation on room air. Physical examination revealed a cardiac S3 gallop with trace edema. POC echocardiography was performed by the medical resident, revealing a severely reduced left ventricular ejection fraction with multiple echogenic structures suspicious for thrombi (Fig. 1). Anticoagulation with heparin was initiated. Several hours later, standard echocardiogram confirmed an ejection fraction of 10–15% with three apical thrombi. Pro-brain natriuretic peptide level was over 11,000 pg/ml. The patient was then transferred to a specialized cardiomyopathy service where inotropic and diuretic therapy led to resolution of his gastrointestinal symptoms which were presumed to be from intestinal venous congestion. Pending further studies, the initial presumptive diagnosis was that of viral cardiomyopathy.
Fig. 1.
Transthoracic echocardiogram in the parasternal long axis view. A significantly dilated left ventricle is seen with three intracavitary masses. Video demonstrated severe global hypokinesis.
We recently reported another case demonstrating the impact of POC ultrasonography – that of an 84-year-old man with a history of esophageal cancer (in remission) and deep venous thrombosis on warfarin who presented with shortness of breath (12). Echocardiogram on the day of admission revealed a low normal ejection fraction with signs of elevated right-sided pressures and no pericardial effusion. The clinical diagnosis was congestive heart failure and his symptoms improved after several days of diuretics. On the fifth day of hospitalization, however, the patient was found to be hypotensive and lethargic. Laboratory studies revealed a creatinine steadily rising to 3.5 mg/dl, an INR of 3.5, and fractional excretion of sodium of 0.3%. The assessment was that of over-diuresis with prerenal acute kidney injury, but he did not respond to small boluses of intravenous fluids. Due to progressive decompensation overnight, POC ultrasonography was performed by the internal medicine resident. Unexpectedly, this revealed a moderate pericardial effusion with right atrial and right ventricular collapse consistent with tamponade physiology (Fig. 2). The patient was urgently transferred to a tertiary care center where pericardiocentesis yielded 750 cc of frank blood. Postprocedure, the patient's urine output and kidney function normalized. Pericardial fluid analysis did not reveal infection or malignancy. Positron emission tomography/computed tomography (PET/CT) was negative for any sign of recurrence of his esophageal cancer. Warfarin was discontinued and a repeat echocardiogram, 4 weeks later, showed no pericardial effusion. The final diagnosis was that of spontaneous hemopericardium in the setting of coagulopathy.
Fig. 2.
Transthoracic echocardiogram in the four-chamber apical view. A pericardial effusion is noted with associated right atrial and right ventricular inversion consistent with tamponade physiology.
Discussion
Ultrasound is a useful adjunctive tool in the assessment of the internal medicine patient
In the last decade, there has been a steadily growing body of research on the utility of ultrasonography for a myriad of conditions commonly seen in internal medicine. In fact, when compared to standard imaging, ultrasound has often yielded similar – if not better – results. This is particularly well demonstrated in the realm of pulmonary disease. A recent meta-analysis including over 1,000 patients demonstrated a high sensitivity (94.1%) and specificity (92.4%) for ultrasonography in the diagnosis of pulmonary edema (13). Ultrasound has also proven to be better than chest X-ray (CXR) and comparable to CT for pneumonia and lung consolidation (14, 15). Two recent meta-analyses, both including over 1,000 patients, confirmed these findings with a sensitivity of 94–97% and specificity of 94–96% for the diagnosis of pneumonia. The area under the receiver operating characteristic (ROC) curve was consistently high (0.98–0.99) with useful positive and negative likelihood ratios (16, 17). Lung ultrasound can also be used to follow patients for resolution of their pneumonia similar to CXR and CT (18).
With regard to pneumothorax, the data are even stronger. Ultrasound can outperform radiography by several measures and is quite comparable to CT while being much faster (19–21). Ultrasonography is also useful in patients with unknown causes of dyspnea. Lichtenstein et al. (22) have published a well-known algorithm that uses a variety of sonographic lung findings to help narrow the differential diagnosis in patients presenting with respiratory insufficiency. Similarly, a recent, large multicenter study demonstrated that ultrasound can distinguish cardiogenic from non-cardiogenic dyspnea better than clinical assessment, CXR, or brain natriuretic peptide levels (23).
Volume status is also a dilemma frequently encountered by the internist. This can be particularly difficult to assess outside the intensive care unit (ICU) where pulmonary artery catheters and stroke volume monitors are absent. However, multiple studies have demonstrated the usefulness of sonographic inferior vena cava (IVC) and cardiac evaluation in non-ICU patients (24, 25). Notably, Guiotto et al. (26) showed that ultrasound assessment of the IVC can guide volume removal by ultrafiltration. This can be particularly valuable with hemodialysis patients on the general medical floor in whom the determination of how much volume to remove is not usually done via very objective or precise means.
With regard to the abdomen, sonography has exhibited excellent sensitivity and specificity in diagnosis of small bowel obstruction (27). In addition, sonographic techniques have long been described for diverticulitis and appendicitis and have very good specificity when compared to CT (28, 29). Interestingly, inflammatory bowel disease can be distinguished from non-inflammatory disease by ultrasound as well. In a study by Novak et al. (30), sonography demonstrated high specificity and negative predictive value in comparison with gold standard endoscopy in patients presenting with abdominal pain and diarrhea. Likewise, with regard to patients presenting with possible nephrolithiasis, POC ultrasound was similar in accuracy compared to both conventional radiology department ultrasound and CT scan without differences in outcomes (31).
Clearly, many of the conditions that are encountered in the internal medicine setting can be evaluated quite well with ultrasonography. The question that naturally follows is whether providers on the general medical floor – particularly internal medicine house staff – are able to apply this technology at the POC.
Ultrasound can be used effectively by residents on general medical floor patients
There is indeed growing literature demonstrating that POC ultrasound performed by medical residents can change the course of patient care. In nearly 200 patients undergoing cardiac and abdominal sonography, Andersen et al. (32) showed that approximately one-third had an additional diagnosis uncovered or the primary diagnosis changed completely. In the pulmonary realm, Filopei et al. (33) demonstrated how ultrasound increased residents’ diagnostic accuracy compared to clinical assessment alone – particularly for chronic obstructive pulmonary disease (COPD), pneumonia, pleural effusion, and pulmonary edema. Residents are also able to perform and interpret abdominal sonography of the kidneys comparable to radiologists; they can evaluate the abdominal aorta comparable to vascular surgeons and sonographers as well (34, 35). Similar findings have been shown with estimating volume status and diagnosing various cardiac pathologies compared to history and physical examination (36, 37). Interestingly, in one study, the use of portable cardiac ultrasound by residents changed management in 40% of cases and solidified prior management decisions in 76% (37). More specifically, residents are able to assess left ventricular function, pleural and pericardial effusion, and even valvular disease accurately compared to cardiologists (38).
What is particularly remarkable is that extensive training is not needed for residents to acquire and interpret images effectively. After training on 20 patients, house staff were able to accurately identify left ventricular dysfunction with sensitivity, specificity, and positive and negative predictive values close to or well over 90% (39). After a 5-h module, medicine residents could diagnose certain kidney conditions with high sensitivity and specificity compared to attending radiologists (34). Similarly, with a half-day workshop, 84% of residents in one study were able to independently evaluate the abdominal aorta compared to only 16% beforehand (40). In fact, many studies demonstrating accurate resident-performed ultrasound show that only a cumulative total training time of several hours to – at most – a few days is needed (35, 36, 40, 41). Understandably, these skills need to be reinforced with regular practice lest they wane over time (41).
Given the above, it is not surprising that POC ultrasonography can impact quality measures and costs. When lung ultrasound was implemented, Peris et al. (42) demonstrated a clear reduction in the number of CXRs and CT scans performed without any decrement in outcomes in one population. When used to guide thoracentesis, ultrasonography decreases complication rates, costs of hospitalization, and lengths of stay (42, 43). Furthermore, in an age where hospital readmission rates are closely monitored, IVC ultrasound by residents can be predictive and preventative, reducing rates from 30 to 4% in one recent study (44). Other studies have shown similar predictive power (45, 46). Razi et al. (39) demonstrated how residents are able to perform POC echocardiography not only accurately but also nearly a full 24 h before formal echocardiogram results are available to confirm their findings. Delays in imaging are known to cause increased hospital lengths of stay (47).
Point-of-care ultrasonography is particularly useful in the community hospital setting
Synthesizing the aforementioned data, there is likely no more appropriate environment for POC ultrasound training of internal medicine house staff than the community hospital. In these settings, urgent or overnight echocardiography or thoracic ultrasound is often not readily available. Community hospitals are not usually designed to provide highly specialized services such as at a tertiary care center, but it is crucial, nonetheless, to identify patients in need of such therapies. Our cases resulted in the appropriate and necessary transfer of the patient to a university center. Given such experiences at our institution, we are currently working to formalize POC ultrasonography in our house staff curriculum and highly encourage other community hospital programs to do so as well.
Conclusion
Our cases demonstrate the diagnostic impact of POC ultrasonography in the hands of trained medical residents – especially in the community hospital setting. Providers on the general medical floor – particularly medical residents – are able to use this highly adaptive technology quite effectively, including in settings where urgent formal studies may not be easily accessible. A thorough medical history and detailed physical examination will remain cornerstones of diagnosis but, nevertheless, technology that can improve accuracy should be embraced. Rene Laennec met some degree of resistance when he introduced the first stethoscope in 1,821 but soon enough this new technology became an icon of the medical profession (48). Similarly, in the training of its newest physicians, the internal medicine specialty needs to accept its newest ‘stethoscope’. The time is now.
Conflict of interest and funding
The authors have not received any funding or benefits from industry or elsewhere to conduct this study.
References
- 1.Filly R. Ultrasound: The stethoscope of the future, alas. Radiology. 1988;167(2):400. doi: 10.1148/radiology.167.2.3282260. [DOI] [PubMed] [Google Scholar]
- 2.Jehle D, Davis E, Evans T, Harchelroad F, Martin M, Zaiser K, et al. Emergency department sonography by emergency physicians. Am J Emerg Med. 1989;7(6):605–11. doi: 10.1016/0735-6757(89)90283-0. [DOI] [PubMed] [Google Scholar]
- 3.Akhtar S, Theodoro D, Gaspari R, Tayal V, Sierzenski P, Lamantia J, et al. Resident training in emergency ultrasound: Consensus recommendations from the 2008 Council of Emergency Medicine Residency Directors Conference. Acad Emerg Med. 2009;16(Suppl 2):S32–6. doi: 10.1111/j.1553-2712.2009.00589.x. [DOI] [PubMed] [Google Scholar]
- 4.The Accreditation Council for Graduate Medical Education and the American Board of Emergency Medicine: The Emergency Medicine Milestone Project. Available from: https://www.abem.org/public/docs/default-source/migrated-documents-and-files/em-milestones.pdf?sfvrsn=6 [cited 1 July 2016].
- 5.Mayo PH, Beaulieu Y, Doelken P, Feller-Kopman D, Harrod C, Kaplan A, et al. American College of Chest Physicians/La Société de Réanimation de Langue Française statement on competence in critical care ultrasonography. Chest. 2009;135(4):1050–60. doi: 10.1378/chest.08-2305. [DOI] [PubMed] [Google Scholar]
- 6.Fessler HE, Addrizzo-Harris D, Beck JM, Buckley JD, Pastores SM, Piquette CA, et al. Entrustable professional activities and curricular milestones for fellowship training in pulmonary and critical care medicine: Report of a multisociety working group. Chest. 2014;146(3):813–34. doi: 10.1378/chest.14-0710. [DOI] [PubMed] [Google Scholar]
- 7.Staren ED, Knudson MM, Rozychi GS, Harness JK, Wherry DC, Shackford SR. An evaluation of the American College of Surgeons’ ultrasound education program. Am J Surg. 2006;191(4):489–96. doi: 10.1016/j.amjsurg.2005.10.023. [DOI] [PubMed] [Google Scholar]
- 8.The Accreditation Council for Graduate Medical Education and the American Board of Internal Medicine: The Internal Medicine Milestone Project. Available from: http://www.abim.org/program-directors-administrators/milestones.aspx [cited 1 July 2016].
- 9.Schnobrich D, Gladding S, Olson A, Duran-Nelson A. Point-of-care ultrasound in internal medicine: A National Survey of Educational Leadership. J Grad Med Educ. 2013;5(3):498–502. doi: 10.4300/JGME-D-12-00215.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Arienti V, Di Giulio R, Cogliati C, Accogli E, Aluigi L, Corazza GR, et al. Bedside ultrasonography (US), echoscopy and US point of care as a new kind of stethoscope for internal medicine departments: The training program of the Italian Internal Medicine Society. Intern Emerg Med. 2014;9(7):805–14. doi: 10.1007/s11739-014-1113-4. [DOI] [PubMed] [Google Scholar]
- 11.Hoppman R, Cook T, Hunt P, Fowler S, Paulman L, Wells J, et al. Ultrasound in medical education: A vertical curriculum at the University of South Caroline School of Medicine. J S C Med Assoc. 2006;102(10):330–4. [PubMed] [Google Scholar]
- 12.Singh G, Sabath B. Over-diuresis or cardiac tamponade? An unusual case of acute kidney injury and early closure. J Community Hosp Intern Med Perspect. 2016;6(2):31357. doi: 10.3402/jchimp.v6.31357. doi: http://dx.doi.org/10.3402/jchimp.v6.31357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Al Deeb M, Barbic S, Featherstone R, Dankoff J, Barbic D. Point-of-care ultrasonography for the diagnosis of acute cardiogenic pulmonary edema in patients presenting with acute dyspnea: A systematic review and meta-analysis. Acad Emerg Med. 2014;21(8):843–52. doi: 10.1111/acem.12435. [DOI] [PubMed] [Google Scholar]
- 14.Nazerian P, Volpicelli G, Vanni S, Gigli C, Betti L, Bartolucci M, et al. Accuracy of lung ultrasound for the diagnosis of consolidations when compared to chest computed tomography. Am J Emerg Med. 2015;33(5):620–5. doi: 10.1016/j.ajem.2015.01.035. [DOI] [PubMed] [Google Scholar]
- 15.Liu Z, Lian R, Tao Y, Gu C, Zhang G. Lung ultrasonography: An effective way to diagnose community-acquired pneumonia. Emerg Med J. 2015;32:433–8. doi: 10.1136/emermed-2013-203039. [DOI] [PubMed] [Google Scholar]
- 16.Hu QJ, Shen YC, Jia LQ, Guo SJ, Long HY, Pang CS, et al. Diagnostic performance of lung ultrasound in the diagnosis of pneumonia: A bivariate meta-analysis. Int J Clin Exp Med. 2014;7(1):115–21. [PMC free article] [PubMed] [Google Scholar]
- 17.Chavez M, Shams N, Ellington L, Naithani N, Gilman RH, Steinhoff MC, et al. Lung ultrasound for the diagnosis of pneumonia in adults: A systematic review and meta-analysis. Respir Res. 2014;15:50–9. doi: 10.1186/1465-9921-15-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Reissig A, Copetti R, Mathis G, Mempel C, Schuler A, Zechner P, et al. Lung ultrasound in the diagnosis and follow-up of community-acquired pneumonia: A prospective, multicenter, diagnostic accuracy study. Chest. 2012;142(4):965–72. doi: 10.1378/chest.12-0364. [DOI] [PubMed] [Google Scholar]
- 19.Ding W, Shen Y, Yang J, He X, Zhang M. Diagnosis of pneumothorax by radiography and ultrasonography: A meta-analysis. Chest. 2011;140(4):859–66. doi: 10.1378/chest.10-2946. [DOI] [PubMed] [Google Scholar]
- 20.Blaivas M, Lyon M, Duggal S. A prospective comparison of supine chest radiography and bedside ultrasound for the diagnosis of traumatic pneumothorax. Acad Emerg Med. 2005;12(9):844–9. doi: 10.1197/j.aem.2005.05.005. [DOI] [PubMed] [Google Scholar]
- 21.Zhang M, Liu Z, Yang J, Gan JX, Xu SW, You XD, et al. Rapid detection of pneumothorax by ultrasonography in patients with multiple trauma. Crit Care. 2006;10(4):R112. doi: 10.1186/cc5004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lichtenstein DA, Mezière GA. Relevance of lung ultrasound in the diagnosis of acute respiratory failure: The BLUE protocol. Chest. 2008;134(1):117–25. doi: 10.1378/chest.07-2800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pivetta E, Goffi A, Lupia E, Tizzani M, Porrino G, Ferreri E, et al. Lung ultrasound-implemented diagnosis of acute decompensated heart failure in the ED: A SIMEU multicenter study. Chest. 2015;148(1):202–10. doi: 10.1378/chest.14-2608. [DOI] [PubMed] [Google Scholar]
- 24.Blehar DJ, Dickman E, Gaspari R. Identification of congestive heart failure via respiratory variation of inferior vena cava diameter. Am J Emerg Med. 2009;27(1):71–5. doi: 10.1016/j.ajem.2008.01.002. [DOI] [PubMed] [Google Scholar]
- 25.Nguyen VT, Ho JE, Ho CY, Givertz MM, Stevenson LW. Handheld echocardiography offers rapid assessment of clinical volume status. Am Heart J. 2008;156(3):537–42. doi: 10.1016/j.ahj.2008.04.015. [DOI] [PubMed] [Google Scholar]
- 26.Guiotto G, Masarone M, Paladino F, Ruggiero E, Scott S, Verde S, et al. Inferior vena cava collapsibility to guide fluid removal in slow continuous ultrafiltration: A pilot study. Intensive Care Med. 2010;36(4):692–6. doi: 10.1007/s00134-009-1745-4. [DOI] [PubMed] [Google Scholar]
- 27.Unluer E, Yavaşi O, Eroğlu O, Yilmaz C, Akarca FK. Ultrasonography by emergency medicine and radiology residents for the diagnosis of small bowel obstruction. Eur J Emerg Med. 2010;17(5):260–4. doi: 10.1097/MEJ.0b013e328336c736. [DOI] [PubMed] [Google Scholar]
- 28.Johansson E, Rydh A, Riklund A. Ultrasound, computed tomography, and laboratory findings in the diagnosis of appendicitis. Acta Radiologica. 2007;48(3):267–73. doi: 10.1080/02841850601182162. [DOI] [PubMed] [Google Scholar]
- 29.van Randen A, Lameris W, van Es H, van Heesewijk HP, van Ramshorst B, Ten Hove W, et al. A comparison of the accuracy of ultrasound and computed tomography in common diagnoses causing acute abdominal pain. Eur Radiol. 2011;21(7):1535–45. doi: 10.1007/s00330-011-2087-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Novak KL, Jacob D, Kaplan G, Boyce E, Ghosh S, Ma I, et al. Point of care ultrasonography accurately distinguishes inflammatory from noninflammatory disease in patients presenting with abdominal pain and diarrhea. Can J Gastroenterol Hepatol. 2016;2016:7. doi: 10.1155/2016/4023065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Smith-Bindman R, Aubin C, Bailitz J, Bengiamin RN, Camargo CA, Jr, Corbo J, et al. Ultrasonography versus computed tomography for suspected nephrolithiasis. N Engl J Med. 2014;371(12):1100–10. doi: 10.1056/NEJMoa1404446. [DOI] [PubMed] [Google Scholar]
- 32.Andersen G, Graven T, Skjetne K, Mjølstad OC, Kleinau JO, Olsen O, et al. Diagnostic influence of routine point-of-care pocket-size ultrasound examinations performed by medical residents. J Ultrasound Med. 2015;34(4):627–36. doi: 10.7863/ultra.34.4.627. [DOI] [PubMed] [Google Scholar]
- 33.Filopei J, Siedenburg H, Rattner P, Fukaya E, Kory P. Impact of pocket ultrasound use by internal medicine housestaff in the diagnosis of dyspnea. J Hosp Med. 2014;9(9):594–7. doi: 10.1002/jhm.2219. [DOI] [PubMed] [Google Scholar]
- 34.Caronia J, Panagopoulos G, Devita M, Tofighi B, Mahdavi R, Levin B, et al. Focused renal sonography performed and interpreted by internal medicine residents. J Ultrasound Med. 2013;32(11):2007–12. doi: 10.7863/ultra.32.11.2007. [DOI] [PubMed] [Google Scholar]
- 35.Bailey RP, Ault M, Greengold NL, Rosendahl T, Cossman D. Ultrasonography performed by primary care residents for abdominal aortic aneurysm screening. J Gen Intern Med. 2001;16(12):845–9. doi: 10.1111/j.1525-1497.2001.01128.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Brennan J, Blair J, Goonewardena S, Ronan A, Shah D, Vasaiwala S, et al. A comparison by medicine residents of physical examination versus hand-carried ultrasound for estimation of right atrial pressure. Am J Cardiol. 2007;99(11):1614–16. doi: 10.1016/j.amjcard.2007.01.037. [DOI] [PubMed] [Google Scholar]
- 37.Croft L, Duvall WL, Goldman ME. A pilot study of the clinical impact of hand-carried cardiac ultrasound in the medical clinic. Echocardiography. 2006;23(6):439–46. doi: 10.1111/j.1540-8175.2006.00240.x. [DOI] [PubMed] [Google Scholar]
- 38.Mjølstad O, Andersen G, Dalen H, Graven T, Skjetne K, Kleinau JO, et al. Feasibility and reliability of point-of-care pocket-size echocardiography performed by medical residents. Eur Heart J Cardiovasc Imaging. 2013;14(12):1195–202. doi: 10.1093/ehjci/jet062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Razi R, Estrada JR, Doll J, Spencer KT. Bedside hand-carried ultrasound by internal medicine residents versus traditional clinical assessment for the identification of systolic dysfunction in patients admitted with decompensated heart failure. J Am Soc Echocardiogr. 2011;24(12):1319–24. doi: 10.1016/j.echo.2011.07.013. [DOI] [PubMed] [Google Scholar]
- 40.Skalski J, Elrashidi M, Reed DA, McDonald FS, Bhagra A. Using standardized patients to teach point-of-care ultrasound-guided physical examination skills to internal medicine residents. J Grad Med Educ. 2015;7(1):95–7. doi: 10.4300/JGME-D-14-00178.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kelm D, Ratelle JT, Azeem N, Bonnes SL, Halvorsen AJ, Oxentenko AS, et al. Longitudinal ultrasound curriculum improves long-term retention among internal medicine residents. J Grad Med Educ. 2015;7(3):454–7. doi: 10.4300/JGME-14-00284.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Peris A, Tutino L, Zagli G, Batacchi S, Cianchi G, Spina R, et al. The use of point-of-care bedside lung ultrasound significantly reduces the number of radiographs and computed tomography scans in critically ill patients. Anesth Analg. 2010;111(3):687–92. doi: 10.1213/ANE.0b013e3181e7cc42. [DOI] [PubMed] [Google Scholar]
- 43.Patel PA, Ernst FR, Gunnarsson CL. Ultrasonography guidance reduces complications and costs associated with thoracentesis procedures. J Clin Ultrasound. 2012;40(3):135–41. doi: 10.1002/jcu.20884. [DOI] [PubMed] [Google Scholar]
- 44.Laffin L, Patel AR, Saha N, Barbat J, Hall JK, Cain M, et al. Inferior vena cava measurement by focused cardiac ultrasound in acute decompensated heart failure prevents hospital readmission. J Am Coll Cardiol. 2014;63(12 Suppl):A542. [Google Scholar]
- 45.Goonewardena SN, Gemignani A, Ronan A, Vasaiwala S, Blair J, Brennan JM, et al. Comparison of hand-carried ultrasound assessment of the inferior vena cava and N-terminal pro-brain natriuretic peptide for predicting readmission after hospitalization for acute decompensated heart failure. JACC Cardiovasc Imaging. 2008;1(5):595–601. doi: 10.1016/j.jcmg.2008.06.005. [DOI] [PubMed] [Google Scholar]
- 46.Carbone F, Bovio M, Rosa GM, Ferrando F, Scarrone A, Murialdo G, et al. Inferior vena cava parameters predict re-admission in ischaemic heart failure. Eur J Clin Invest. 2014;44(4):341–9. doi: 10.1111/eci.12238. [DOI] [PubMed] [Google Scholar]
- 47.Cournane S, Conway R, Creagh D, Byrne DG, Sheehy N, Silke B. Radiology imaging delays as independent predictors of length of hospital stay for emergency medical admissions. Clin Radiol. 2016;71(9):912–18. doi: 10.1016/j.crad.2016.03.023. [DOI] [PubMed] [Google Scholar]
- 48.Forbes J. A treatise on the diseases of the chest by R.T.H. Laennec. Translated from French to English. 1st American ed. Philadelphia, PA: James Webster; 1823. [Google Scholar]