Abstract
Background:
Ankle sprains represent a common injury in emergency departments, but little is known about common complications, procedures, and charges associated with ankle sprains in emergency departments.
Hypothesis:
There will be a higher incidence of ankle sprains among younger populations (≤25 years old) and in female patients. Complications and procedures will differ between ankle sprain types. Lateral ankle sprains will have lower health care charges relative to medial and high ankle sprains.
Study Design:
Descriptive epidemiological study.
Level of Evidence:
Level 3.
Methods:
A cross-sectional study of the 2010 Nationwide Emergency Department Sample was conducted. Outcomes such as charges, complications, and procedures were compared using propensity score matching between lateral and medial as well as lateral and high ankle sprains.
Results:
The sample contained 225,114 ankle sprains. Female patients sustained more lateral ankle sprains (57%). After propensity score adjustment, lateral sprains incurred greater charges than medial ankle sprains (median [interquartile range], $1008 [$702-$1408] vs $914 [$741-$1108]; P < 0.01). Among complications, pain in the limb (1.92% vs 0.52%, P = 0.03), sprain of the foot (2.96% vs 0.70%, P < 0.01), and abrasion of the hip/leg (1.57% vs 0.35%, P = 0.03) were more common in lateral than medial ankle sprain events. Among procedures, medial ankle sprains were more likely to include diagnostic radiology (97.91% vs 83.62%, P < 0.01) and less likely to include medications than lateral ankle sprains (0.87% vs 2.79%, P < 0.01). Hospitalizations were more common following high ankle sprains than lateral ankle sprains (24 [6.06%] vs 1 [0.25%], P < 0.01).
Conclusion:
Ankle sprain emergency department visits account for significant health care charges in the United States. Age- and sex-related differences persist among the types of ankle sprains.
Clinical Relevance:
The health care charges associated with ankle sprains indicate the need for additional preventive measures. There are age- and sex-related differences in the prevalence of ankle sprains that suggest these demographics may be risk factors for ankle sprains.
Keywords: sprains, ankle, Nationwide Emergency Department Sample, propensity score matching
Lateral ankle sprains (LASs) are often considered a benign injury with no lasting consequences. However, at least one-third of individuals who sustain an LAS will experience residual symptoms.6,7,14,15,19 These symptoms, often termed “chronic ankle instability” (CAI), can significantly alter an individual’s health and function by causing him or her to become less active over their life span.21 CAI is also a major contributing factor in the development of posttraumatic ankle osteoarthritis.8,20
Epidemiological studies have described the incidence rates of LAS in active-duty military service members5 and military cadets in the United States23 as well as the general European population.4,9 An estimated 628,026 ankle sprains occurred annually between 2002 and 2006, with sex, age, race, and athletic involvement all affecting the incidence rate of ankle sprain determined using the National Electronic Injury Surveillance System (NEISS) database.24 While the identification of demographic risk factors may help implement preventive measures, no study has characterized the common complications or treatments associated with acute ankle sprains presenting to emergency departments in the United States.
Though often untreated, research demonstrates that LAS can result in considerable time lost to injury, as approximately 25% of those who sprain their ankles are unable to attend school or work for at least 1 week.3 Unfortunately, cost estimates for the treatment of LAS in the United States are severely outdated,16 and no cost estimates exist for medial and high ankle sprains. Therefore, the purpose of this study was to generate national incidence and cost estimates for lateral, medial, and high ankle sprains as well as determine whether complications and procedures undertaken differ among ankle sprain types.
Methods
The 2010 Nationwide Emergency Department Sample (NEDS)11 was used to assess cross-sectional data on acute ankle sprain visits. NEDS is a nationwide data set developed as a part of the Healthcare Cost and Utilization Project (HCUP), a federal-state-industry partnership sponsored by the Agency for Healthcare Research and Quality (AHRQ).11 NEDS is a 20% stratified sample of 950 emergency departments spread across 30 states within the United States. Only those cases with a primary diagnosis (first diagnosis listed) of ankle sprain were included in this investigation, regardless of concomitant injury.
Patient age was classified into categories ranging from pediatric (≤13 years) to geriatric admissions (≥65 years). Mean emergency department charges were calculated based on the charge data provided for each visit including necessary inpatient expenses. Incidence estimates were calculated using the discharge weight included in the NEDS data set for each type of ankle sprain and then stratified by age and sex.24 Descriptive statistics (ie, counts, frequencies, averages) were calculated to assess population and cohort characteristics. The most common complications were identified using ICD-9-CM (International Classification of Diseases, Ninth Revision, Clinical Modification) codes by consolidating secondary diagnoses (see Appendix 1, available at http://sph.sagepub.com/content/by/supplemental-data). The Clinical Classifications Software (CCS) for services and procedures was applied to the ankle sprain diagnosis codes (ICD-9-CM codes) to group the most common procedures into meaningful categories (Appendix 1). Hospitalizations were determined by merging the supplemental inpatient file provided in the NEDS.
To obtain homogenous groups and to reduce bias, a propensity score analysis between lateral and medial as well as lateral and high ankle sprains was performed. Propensity scores were calculated using a logistic regression model. Four covariates including age, sex, median household income, and primary payer were used to generate propensity scores. These outcomes were used because of descriptive differences among ankle sprain types. After estimating the propensity score, groups were matched using a 1:1 nearest neighbor (greedy-type) matching algorithm.13 Matching was performed without replacement, and unpaired ankle sprains were excluded (Figure 1). Propensity score–matched analyses did not include the discharge weights, as sample restriction negates the validity of the weights.
Figure1.
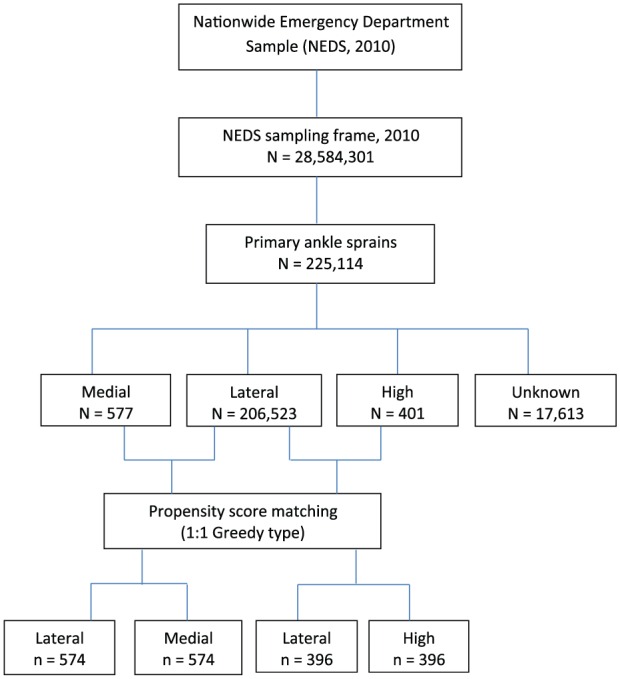
Flow diagram for sample selection and analysis.
Characteristics of demographics and outcomes were compared between propensity score–matched groups using frequencies and chi-square tests. The Wilcoxon-Mann-Whitney test compared total charges between propensity score–matched groups. Statistical significance was established at P ≤ 0.05 using SAS 9.4 software (SAS Institute Inc).
Results
There were 225,114 ankle sprains identified, with LAS being the most common (Table 1). This equates to an overall estimated incidence rate of 3.29 ankle sprains per 1000 person-years. Estimated incidence rates of 3.02, 0.0086, 0.0062, and 2.55 per 1000 person-years were identified for lateral, medial, high, and unknown ankle sprains, respectively. The majority of patients in lateral, medial, and unknown ankle sprain groups were female.
Table 1.
Characteristics of demographics of ankle sprains in National Emergency Department Sample, 2010
| Type | Lateral, n (%) | Medial, n (%) | High, n (%) | Unknown, n (%) | Total, n (%) |
|---|---|---|---|---|---|
| Total ankle injuries of each type | 206,523 (91.74) | 577 (0.26) | 401 (0.18) | 17,613 (7.82) | 225,114 |
| Sex | |||||
| Male | 89,175 (43.18) | 279 (48.35) | 202 (50.37) | 8577 (48.70) | 98,223 (43.64) |
| Female | 117,338 (56.82) | 298 (51.65) | 199 (49.63) | 9036 (51.30) | 126,871 (56.36) |
| Age, y | |||||
| ≤13 | 28,746 (13.92) | 102 (17.68) | 39 (9.73) | 2102 (11.93) | 30,989 (13.77) |
| 14-17 | 29,332 (14.20) | 115 (19.93) | 76 (18.95) | 2198 (12.48) | 31,721 (14.09) |
| 18-25 | 41,713 (20.20) | 109 (18.89) | 84 (20.95) | 3204 (18.19) | 45,110 (20.04) |
| 26-35 | 39,935 (19.34) | 92 (15.94) | 90 (22.44) | 3529 (20.04) | 43,646 (19.39) |
| 36-49 | 37,813 (18.31) | 96 (16.64) | 67 (16.71) | 3924 (22.28) | 41,900 (18.61) |
| 50-64 | 19,979 (9.67) | 46 (7.97) | 31 (7.73) | 1874 (10.64) | 21,930 (9.74) |
| ≥65 | 9005 (4.36) | 17 (2.95) | 14 (3.49) | 782 (4.44) | 9818 (4.36) |
| Median household income, $ | |||||
| ≤40,999 | 66,696 (32.88) | 331 (57.57) | 116 (29.29) | 4588 (26.60) | 71,731 (32.45) |
| 41,000-50,999 | 59,788 (28.99) | 110 (19.13) | 143 (36.11) | 4267 (24.74) | 63,308 (28.64) |
| 51,000-66,999 | 42,723 (21.06) | 74 (12.87) | 78 (19.70) | 4358 (25.27) | 47,233 (21.37) |
| ≥67,000 | 34,613 (17.07) | 60 (1.43) | 59 (14.90) | 4032 (23.38) | 38,764 (17.54) |
| Primary payer | |||||
| Medicare | 15,680 (7.63) | 25 (4.34) | 32 (8.14) | 1289 (7.38) | 17,026 (7.60) |
| Medicaid | 53,524 (26.04) | 112 (19.44) | 90 (22.90) | 3713 (21.27) | 57,439 (25.65) |
| Private insurance | 82,326 (40.05) | 285 (49.48) | 162 (41.22) | 7806 (44.72) | 90,579 (40.44) |
| Self-pay | 38,300 (18.63) | 122 (21.18) | 76 (19.34) | 3193 (18.29) | 41,691 (18.62) |
| No charge | 1317 (0.64) | 0 | 2 (0.51) | 73 (0.42) | 1392 (0.62) |
| Other | 14,388 (7.0) | 32 (5.56) | 31 (7.89) | 1382 (7.92) | 15,833 (7.07) |
| Total charges, $ | |||||
| <1000 | 97,900 (47.40) | 337 (58.41) | 191 (47.63) | 7461 (42.36) | 105,889 (47.04) |
| 1000-5000 | 107,168 (51.89) | 234 (40.55) | 175 (43.64) | 9881 (56.10) | 117,458 (52.18) |
| 5001-10,000 | 1054 (0.51) | 3 (0.52) | 5 (1.25) | 112 (0.64) | 1174 (0.52) |
| >10,000 | 401 (0.19) | 3 (0.52) | 30 (7.48) | 159 (0.90) | 593 (0.26) |
| Complications | |||||
| Pain in joint, ankle and foot | 17,268 (8.36) | 37 (6.41) | 15 (3.74) | 1391 (7.90) | |
| Sprain of foot NOS (sprain of foot, unspecified site) | 7891 (3.82) | 4 (0.69) | 6 (1.50) | 172 (0.98) | |
| Lower leg injury NOS (knee, leg, ankle, and foot injury) | 5303 (2.57) | 11 (1.90) | NA | 236 (1.34) | |
| Pain in limb | 4464 (2.16) | NA | 9 (2.24) | 417 (2.37) | |
| Joint effusion-ankle (effusion of joint, ankle, and foot) | 3620 (1.75) | 16 (2.77) | NA | 282 (1.60) | |
| Swelling of limb | 3068 (1.49) | NA | 7 (1.75) | 435 (2.47) | |
| Procedures | |||||
| Other diagnostic radiology and related techniques | 185,443 (89.79) | 564 (97.75) | 364 (90.77) | 13,723 (77.91) | |
| Traction, splints, and other wound care | 43,500 (21.06) | 72 (12.48) | 91 (22.69) | 3619 (20.55) | |
| Durable medical equipment and supplies | 16,978 (8.22) | 25 (4.33) | 30 (7.48) | 1215 (6.90) | |
| Other therapeutic procedures | 9720 (4.71) | 29 (5.03) | 19 (4.78) | 846 (4.80) | |
| Medications (injections and other forms) | 8699 (4.21) | 5 (0.87) | 38 (9.48) | 551 (3.31) |
NA, not applicable; NOS, not otherwise specified.
Using the sample weights provided by the NEDS, we estimated the nationwide incidence of ankle sprains to be 1,016,282 cases in 2010 (Table 2). The median emergency department charges per event for all types of ankle sprains were $1029 (interquartile range [IQR], $723-$1457). However, charge information is missing for approximately 17% of ankle sprain observations. Missing charge data for emergency department visits and hospitalizations were excluded.
Table 2.
Projected national incidence of ankle sprains in the United States in 2010
| Type | Lateral, n (%) | Medial, n (%) | High, n (%) | Unknown, n (%) | Total, n (%) |
|---|---|---|---|---|---|
| Total primary ankle injuries | 932,868 | 2,672 | 1918 | 78,824 | 1,016,282 |
| Sex | |||||
| Male | 402,696 (43.14) | 1304 (48.83) | 966 (50.37) | 38,452 (48.78) | 443,419 (43.63) |
| Female | 530,123 (56.83) | 1367 (51.17) | 952 (49.63) | 40,372 (51.22) | 572,815 (56.37) |
| Age, y | |||||
| ≤13 | 128,820 (13.81) | 457 (17.10) | 177 (9.22) | 9445 (11.98) | 138,899 (13.66) |
| 14-17 | 131,930 (14.14) | 526 (19.68) | 376 (19.59) | 9716 (12.33) | 142,548 (14.02) |
| 18-25 | 189,789 (20.34) | 524 (19.61) | 398 (20.76) | 14,472 (18.36) | 205,183 (20.19) |
| 26-35 | 180,708 (19.37) | 428 (16.02) | 449 (23.41) | 15,828 (20.08) | 197,414 (19.43) |
| 36-49 | 170,754 (18.30) | 440 (16.47) | 302 (15.76) | 17,622 (22.36) | 189,119 (18.61) |
| 50-64 | 90,308 (9.68) | 222 (8.33) | 150 (7.81) | 8363 (10.61) | 99,044 (9.75) |
| ≥65 | 40,558 (4.35) | 74 (2.78) | 66 (3.45) | 3376 (4.28) | 44,075 (4.34) |
| Total charges, $ | |||||
| Mean (SEM) (SD) | 1211.15 (2.48) (2400.24) | 1178.82 (99.50) (5143.19) | 3204.47 (439.02) (19,229.35) | 1428.64 (19.80) (5561.28) | 1231.69 (2.88) (2912.20) |
| Median (IQR) | 1025 (718-1,451) | 912 (738-1114) | 1034 (737-1396) | 1086 (775-1495) | 1029 (723-1457) |
IQR, interquartile range; SEM, standard error of mean.
Prior to matching, there were significant differences between lateral and medial ankle sprain groups (Table 3 in Appendix 2, http://sph.sagepub.com/content/by/supplemental-data). Specifically, patients with lateral sprains were older (P < 0.01), more likely to be female (P = 0.01), and less likely to use private insurance as their primary payer (P < 0.01). Following 1:1 matching, all covariates were statistically indistinguishable (P > 0.05), achieving balance among 574 lateral and medial ankle sprains.
Prior to matching, patients with lateral sprains relative to high ankle sprains were older (P = 0.01), more likely to be female (P = 0.003), and more likely to be in the first quartile of median household income than patients with high ankle sprains (P = 0.01) (Table 4 in Appendix 2). Propensity score 1:1 matching resulted in 396 lateral and high ankle sprain patients with statistically indistinguishable (P > 0.05) covariates between groups, achieving balance.
LAS incurred greater charges than medial ankle sprains despite a greater number of hospitalizations in the medial group (P < 0.01) (Table 5 in Appendix 2). There were 4 (0.69%) hospitalizations for medial sprains compared with none for lateral sprains (P = 0.04). Among the most common complications associated with lateral and medial sprains, pain in the limb (P = 0.03), sprain of the foot (P < 0.01), and abrasion of hip and leg (P = 0.03) were significantly more common in the lateral group (Tables 1 and 2 and Tables 3-5 in Appendix 2). Among the most common procedures, patients with medial ankle sprain were more likely to use other diagnostic radiology and related techniques (P < 0.01) and less likely to use medications than patients with lateral (P < 0.01) ankle sprains.
Following 1:1 matching, the lateral and high groups had similar total charges for an emergency department event (P = 0.97). In-patient admission was significantly greater for high ankle sprains compared with LAS (P < 0.01). Among the most common complications, patients with LAS were more likely to have pain in the joint, ankle, and foot (P < 0.01) and lower leg injury (P = 0.03) than patients with high ankle sprain. Among the most common procedures, high ankle sprain patients were more likely to use traction, splints, and other wound care than those with LAS (P = 0.09).
Discussion
The current estimated incidence for lateral ankle sprains is consistent with—albeit higher than—that reported by Waterman et al24 (2.15) for the general US population but significantly lower than those reported in the general population of Europe (6.96 and 5.27).4,9 Vosseller et al22 reported 1821 high ankle sprains from the State Inpatient Database and State Emergency Department Databases of 8 states (2.09 per 100,000 person-years) in 2009. The observed 1821 high ankle sprains is significantly higher than the current weighted national estimate.
Like previous investigations, the current data indicate that the peak incidence of ankle sprains generally occurs in the second to third decade of life. For example, Vosseller et al22 reported the peak incidence of high ankle sprains occurred between 18 and 34 years of age. However, the authors reported the lowest incidence between 0 and 17 years of age. This is contrary to the current data from the 0- to 17-year-old age group, which had the second largest incidence of high ankle sprains. The current investigation also revealed that female patients sustained more lateral ankle sprains than male patients. This is consistent with previous work2,10 but contrasts with the work of Waterman et al.24 The current high ankle sprain results (no sex differences) are also contrary to those of Vosseller et al,22 who reported that men had an increased incidence rate.
Broadly, the most common procedures align with the general standard of care associated with ankle sprains. Differences in procedure rates among the different types of ankle sprains may be due to standard of care differences among emergency departments. For example, the higher percentage of diagnostic radiography used for medial relative to lateral ankle sprains may be due to concerns about fractures through open growth plates, as a higher percentage of medial relative to lateral ankle sprain events were in patients 17 years old or younger. Previous research has estimated that 80% to 98% of patients reporting to emergency departments for ankle sprains undergo radiography, which is consistent with the current observation. However, fewer than 15% of patients receiving radiography have a fracture.18 The Ottawa Ankle Rules17 have a pooled sensitivity of 97.6% (95% CI, 96.6%-98.9%)2 with a pooled negative likelihood ratio of 0.08 for the ankle.1 In short, the Ottawa Ankle Rules could significantly reduce emergency department costs associated with lateral ankle sprains. Significant variability was noted in charge data, particularly in the medial and high ankle sprain groups. This is most likely due to the hospitalization costs associated with a select number of individuals in those groups. The required use or lack of use of the Ottawa Ankle Rules is just one example of how protocol differences could also increase variability in charge data.
An important limitation of our study is the lack of a gold standard for diagnosis of lateral ankle sprains. Multiple grading scales make comparison of diagnostic evidence and intervention effectiveness difficult.23,24 The NEDS database is also not without limitations. First, the incidence rates are based on attendance and therefore may be underestimated because a high percentage of individuals do not seek medical treatment for ankle sprains12 or may seek care from another health care provider. Similarly, the data are reported as emergency department events and not individuals; therefore, individuals may have reported multiple ankle sprains. Second, the NEDS database does not provide the mechanism of injury or a racial category. Waterman et al24 previously demonstrated that race may influence lateral ankle sprain incidence. Finally, NEDS only provides charges associated with the observed condition and not the actual health care costs. Therefore, the charges reported in this investigation should be used as an estimate only.
Conclusion
Lateral ankle sprains represent the vast majority of ankle sprain events and associated health care charges. There is a higher incidence of ankle sprains among younger populations (≤25 years) and in female patients. Complications and procedures differ among ankle sprain types. Lateral ankle sprains have greater health care charges relative to medial ankle sprains and comparable emergency department event charges as high ankle sprains.
Supplementary Material
Supplementary Material
Footnotes
The authors report no potential conflicts of interest in the development and publication of this article.
References
- 1. Bachman LM, Kolb E, Koller MT, Steurer J, ter Riet G. Accuracy of Ottawa ankle rules to exclude fractures of the ankle and mid-foot: systematic review. BMJ. 2003;326:417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Beynnon BD, Vacek PM, Murphy D, Alosa D, Paller D. First-time inversion ankle ligament trauma: the effects of sex, level of competition, and sport on the incidence of injury. Am J Sports Med. 2005;33:1485-1491. [DOI] [PubMed] [Google Scholar]
- 3. de Bie RA, de Vet HC, van den Wildenberg FA, Lenssen T, Knipschild PG. The prognosis of ankle sprains. Int J Sports Med. 1997;18:285-289. [DOI] [PubMed] [Google Scholar]
- 4. Bridgman SA, Clement D, Downing A, Walley G, Phair I, Maffulli N. Population based epidemiology of ankle sprains attending accident and emergency units in the West Midlands of England and a survey of UK practice for severe ankle sprains. Emerg Med J. 2003;20:508-510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Cameron KL, Owens BD, DeBerardino TM. Incidence of ankle sprains among active-duty members of the United States Armed Services between 1998 through 2006. J Athl Train. 2010;45:29-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Fong DT, Hong YL, Chan LK, Yung PS, Chan KM. A systematic review on ankle injury and ankle sprain in sports. Sports Med. 2007;37:73-94. [DOI] [PubMed] [Google Scholar]
- 7. Hiller CE, Nightingale EJ, Raymond J, et al. Prevalence and impact of chronic musculoskeletal ankle disorders in the community. Arch Phys Med Rehabil. 2012;93:1801-1807. [DOI] [PubMed] [Google Scholar]
- 8. Hirose K, Murakami G, Minowa T, Kura H, Yamashita T. Lateral ligament injury of the ankle and associated articular cartilage degeneration in the talocrural joint: anatomic study using elderly cadavers. J Orthop Sci. 2004;9:37-43. [DOI] [PubMed] [Google Scholar]
- 9. Holmer P, Sondergaard L, Konradsen L, Nielsen PT, Jorgensen LN. Epidemiology of sprains in the lateral ankle and foot. Foot Ankle Int. 1994;15:72-74. [DOI] [PubMed] [Google Scholar]
- 10. Hosea TM, Carey CC, Harrer MF. The gender issue: epidemiology of ankle injuries in athletes who participate in basketball. Clin Orthop Relat Res. 2000;(372):45-49. [DOI] [PubMed] [Google Scholar]
- 11. Introduction to the HCUP Nationwide Emergency Department Sample (NEDS) 2012. Rockville, MD: Agency for Healthcare Research and Quality; 2014. https://www.hcup-us.ahrq.gov/db/nation/neds/IntroductionNEDS2012_updatedFeb2015.pdf. Accessed March 15, 2015.
- 12. McKay GD, Goldie PA, Payne WR, Oakes BW. Ankle injuries in basketball: injury rate and risk factors. Br J Sports Med. 2001;35:103-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Parsons LS. Reducing bias in a propensity score matched-pair sample using greedy matching techniques. In: Proceedings of the Twenty-sixth Annual SAS Users Group International Conference Cary, NC: SAS Institute; 2001:214-226. [Google Scholar]
- 14. Peters JW, Trevino SG, Renstrom PA. Chronic lateral ankle instability. Foot Ankle. 1991;12:182-191. [DOI] [PubMed] [Google Scholar]
- 15. Smith RW, Reischl SF. Treatment of ankle sprains in young athletes. Am J Sports Med. 1986;14:465-471. [DOI] [PubMed] [Google Scholar]
- 16. Soboroff SH, Pappius EM, Komaroff AL. Benefits, risks, and costs of alternative approaches to the evaluation and treatment of severe ankle sprain. Clin Orthop Relat Res. 1984;(183):160-168. [PubMed] [Google Scholar]
- 17. Stiell IG, Greenberg GH, McKnight RD, Nair RC, McDowell I, Worthington JR. A study to develop clinical decision rules for the use of radiography in acute ankle injuries. Ann Emerg Med. 1992;21:384-390. [DOI] [PubMed] [Google Scholar]
- 18. Sujitkumar P, Hadfield JM, Yates DW. Sprain or fracture? An analysis of 2000 ankle injuries. Arch Emerg Med. 1986;3:101-106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Swenson D, Yard E, Fields S, Comstock R. Patterns of recurrent injuries among US high school athletes, 2005-2008. Am J Sports Med. 2009;37:1586-1589. [DOI] [PubMed] [Google Scholar]
- 20. Valderrabano V, Hintermann B, Horisberger M, Fung TS. Ligamentous posttraumatic ankle osteoarthritis. Am J Sports Med. 2006;34:612-620. [DOI] [PubMed] [Google Scholar]
- 21. Verhagen RA, de Keizer G, van Dijk CN. Long-term follow-up of inversion trauma of the ankle. Arch Orthop Trauma Surg. 1995;114:92-96. [DOI] [PubMed] [Google Scholar]
- 22. Vosseller JT, Karl JW, Greisberg JK. Incidence of syndesmotic injury. Orthopedics. 2014;37:e226-e229. [DOI] [PubMed] [Google Scholar]
- 23. Waterman BR, Belmont PJ, Jr, Cameron KL, DeBerardino TM, Owens BD. Epidemiology of ankle sprain at the United States Military Academy. Am J Sports Med. 2010;38:797-803. [DOI] [PubMed] [Google Scholar]
- 24. Waterman BR, Owens BD, Davey S, Zacchilli MA, Belmont PJ., Jr. The epidemiology of ankle sprains in the United States. J Bone Joint Surg Am. 2010;92:2279-2284. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


