Abstract
Context:
Given its young, predominately male demographics and intense physical demands, the US military remains an ideal cohort for the study of anterior shoulder instability.
Evidence Acquisition:
A literature search of PubMed, MEDLINE, and the Cochrane Database was performed to identify all peer-reviewed publications from 1950 to 2016 from US military orthopaedic surgeons focusing on the management of anterior shoulder instability.
Study Design:
Clinical review.
Level of Evidence:
Level 4.
Results:
The incidence of anterior shoulder instability events in the military occurs at an order of magnitude greater than in civilian populations, with rates as high as 3% per year among high-risk groups. With more than 90% risk of a Bankart lesion and high risk for instability recurrence, the military has advocated for early intervention of first-time shoulder instability while documenting up to 76% relative risk reduction versus nonoperative treatment. Preoperative evaluation with advanced radiographic imaging should be used to evaluate for attritional bone loss or “off-track” engaging defects to guide comprehensive surgical management. With complex recurrent shoulder instability and/or cases of clinically significant osseous lesions, potential options such as remplissage, anterior open capsular procedures, or bone augmentation procedures may be preferentially considered.
Conclusion:
Careful risk stratification, clinical evaluation, and selective surgical management for at-risk military patients with anterior shoulder instability can optimize the recurrence risk and functional outcome in this population.
Keywords: anterior, shoulder instability, dislocation, subluxation, military
With minimal bony constraint and a wide functional range of motion, the glenohumeral joint is susceptible to instability. Anterior shoulder instability remains a significant area of focus and debate within the contemporary sports medicine community, particularly as it relates to young athletes. The current literature is replete with investigations evaluating relative risk and optimal management of shoulder instability. Military surgeons have made several landmark contributions toward this end, and this trend has continued into the modern era among American military colleagues.2,5,11,12,18,19,25,38,41-43,48,51,55,57-59,61,63-65 Accordingly, so-called military “warrior athletes” embody a physically active patient subset at high risk for anterior shoulder instability that is ideal for further focus in this article.
Epidemiology
Current estimates indicate that the rates of anterior shoulder dislocations among military cohorts are an order of magnitude greater than that seen in matched civilian counterparts. A rate of 0.08 per 1000 person-years exists among the rural civilian community of Olmstead County, Minnesota, whereas prior investigations from northern Europe report slightly increased rates of 0.17 to 0.24 in a large-scale, urban setting.32,41 Conversely, a nearly 10-fold greater incidence of 1.69 per 1000 person-years exists within the general US military, with increased risk in men, age >30 years, junior enlisted rank, and Army branch of service.44 There is also a greater prevalence of shoulder instability among men >21 years old serving in the Israeli Defense Forces. Service academy cadets,46 new recruits, and those serving in combat deployments4 demonstrate inherently heightened risk for anterior instability events. At the US Military Academy, there are exponentially greater rates of anterior shoulder instability within a cohort with a risky combination of young patients and the rigors of military activity. Shoulder dislocations occurred in 4.35 cadets per 1000 person-years, but subluxation increased the cumulative rate of anterior instability events to nearly 3% per year and comprised up to 85% of all instability events.46 While the morbidity of anterior subluxations (or instability events not requiring formal reduction) have been questioned, further radiographic and clinical data have shown a high preponderance of Bankart and Hill-Sachs lesions among cadets, indicating a significant potential for subsequent recurrence with return to full activity.48
Evaluation
Clinical Examination
In the setting of significant glenoid or bipolar bone loss, shoulder instability may also occur at lower degrees of abduction and/or external rotation and lower energy mechanism of injury, even during sleep. Given the frequency of associated labral lesions or shoulder pathology within military patients,20,21,59,61,62 individuals should be carefully scrutinized for superior and posterior labral extension. Underlying global hyperlaxity or incompetency of the inferior glenohumeral ligament complex should be excluded as factors leading to bi- or multidirectional instability, and this can be elucidated with Gagey testing,1 sulcus sign, and application of the Beighton criteria (ie, score of ≥4). Similarly, posterior instability tests such as the jerk, push-pull, and posterior load and shift tests should be employed to evaluate for instability in this direction.
After primary survey, the shoulder girdle should be carefully evaluated for persistent neurovascular deficits. The axillary nerve is most commonly involved because of its relative proximity with the capsule of the axillary pouch and inferior glenohumeral ligament complex, as well as its tethered position in the quadrilateral space. However, injury to the suprascapular and musculocutaneous nerves and intimal injury or frank dissection of the axillary artery have been described.2 Sensorimotor evaluation of all peripheral nerve dermatomes and muscle strength should be routinely documented.
Radiographic Evaluation
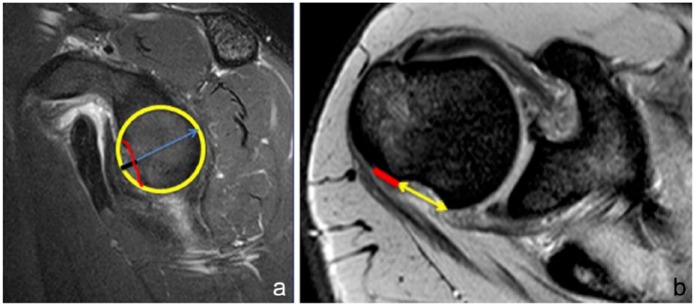
Magnetic resonance imaging (MRI), with or without intra-articular gadolinium, may help identify the extent of labral tear or associated humeral avulsion of the glenohumeral ligament (HAGL), tissue medialization, chondral pathology, capsular volume or redundancy, and characterization of glenohumeral bone loss. For more precise quantification and localization of evident bipolar osseous involvement, computed tomography (CT) with 2- and 3-dimensional reconstructions may also be considered. Three-dimensional CT reconstruction is currently considered the gold standard for the evaluation of bone loss,10,53 although MRI has also demonstrated consistent correlation with CT in many studies.27,34 Several techniques for classifying attritional glenoid bone loss6,7 and Hill-Sachs lesions51 have been described, and more than 20% to 25% anterior-inferior glenoid loss has been suggested as a critical threshold for increased failure with isolated labral repair.13,33,50 More recently, the lower limit of this bone loss has been questioned, with so-called “subcritical” bone loss of 13.5% leading to suboptimal outcomes with arthroscopic treatment.58 Additionally, others have recommended use of the so-called “glenoid track” concept based off 3-dimensional CT reconstructions to preoperatively ascertain whether a Hill-Sachs lesion is engaging (ie, “off track”) and requires additional (eg, remplissage) or more aggressive initial management (Figure 1).24,37,66
Figure 1.
(a) Calculation of the glenoid track. The inferior two-thirds of the glenoid approximates a circle, and the diameter of this circle represents the expected diameter of the glenoid. The glenoid track is calculated as 0.83 × diameter (yellow circle). Bone loss (red line) is measured as the distance from the edge of the circle to the edge of the remaining bone (black line) and is subtracted from the glenoid track measure. (b) Calculation of the Hill-Sachs lesion (HSL). On sagittal view, demonstrating the maximum bone defect, the HSL is the distance from the insertion of the rotator cuff to the medial edge of the HSL. The yellow line represents the Hill-Sachs defect, and the red line represents the bone bridge between it and the insertion of the cuff. These lines are added together to characterize the Hill-Sachs lesion used in the calculation of the glenoid track.
Risk Stratification
Several patient-specific factors have long been recognized as risks for recurrence of shoulder instability. Taken together, they reflect the demographics of a military population quite closely and explain why this pathology is so commonly encountered among the US active-duty population. Chief among these risk factors is young age. In his classic 1956 article, Rowe56 stratified recurrence risk for anterior instability by age. Patients between the ages of 10 and 20 years incurred an 83% recurrence rate, those 20 to 40 years had 63% recurrence, and patients older than 40 years suffered only 16% recurrence.56 Multiple other studies have confirmed young age as a risk factor in both conservatively and operatively treated unstable shoulders. Activity level has also been a well-recognized risk for failure. Most traumatic shoulder instability is the result of an athletic activity, and contact and collision athletes are certainly at increased risk for recurrence.3,44,56 Finally, male sex is a well-recognized risk factor for recurrence of instability. A recent meta-analysis concluded that male sex placed those with a first-time dislocation at more than 3-fold greater risk for recurrence than their female counterparts.42 Thus, the typical clinical picture for the unstable shoulder is a young man who is involved in competitive sports and particular contact activities. As this is also the picture of the active duty man, it is no wonder the military provides such a rich experience in treating the unstable shoulder.
Management
Early Nonoperative Treatment
While glenohumeral reduction, brief sling immobilization, and graduated involvement with physical therapy are well established after an acute anterior instability event, debate still lingers on the ideal method for subsequent management. The Bankart lesion, or other labral tear variant such as a glenolabral articular disruption (GLAD) or anterior labral periosteal sleeve avulsion (ALPSA), is usually a “lesion of necessity” for subsequent shoulder instability and is present among 79% and 100% of patients with first-time shoulder dislocations.2,12,31,48 However, despite the high prevalence of this pathoanatomy, rates of recurrent instability may vary more widely depending on the demographic patient sample, particularly among those of younger age. Despite best clinical practices, nonoperative management of primary anterior shoulder instability is associated with significant short-term morbidity, with increased time lost to injury, subsequent instability events in 39% to 94% of patients, and the potential for worsening chondrolabral and ligamentous pathology.29-31,48,53,59,65 Longer-term studies have also demonstrated a 75% unsatisfactory outcome with nonoperative management of anterior shoulder instability.30
Nevertheless, nonoperative initial management may play a role in situations such as the in-season athlete. An accelerated rehabilitation program for the in-season athlete desiring an early return to function has been advocated. In a civilian athletic population with in-season instability events, 87% of athletes returned to in-season competition, with 41% of those sustaining an additional instability event and two-thirds of patients requiring eventual surgery.14 With in-season instability in an intercollegiate population of service academy athletes, 73% returned to play at a mean 5 days while 64% of athletes sustained an additional instability event in season.22
First-Time Traumatic Dislocation
Controversy exists in management decisions in the first-time dislocator. Traditional treatment has dictated a trial of conservative management, with surgery reserved for those in whom this approach fails. However, this classic dogma has been challenged by several well-performed studies, both within and outside of the military setting. Within the West Point cadet population, both showed significant relative risk reduction (92% vs 16%65 and 80% vs 14%,2 respectively) in subsequent shoulder instability with primary arthroscopic stabilization at short-term follow-up using a glenoid staple and transglenoid repair technique. Using a suture anchor technique, persistent benefits of early arthroscopic Bankart repair with excellent functional and patient-reported outcomes at long term were seen at a mean 11.7-year follow-up in young military patients.45 Six patients (14.3%) sustained recurrent dislocation and required revision stabilization, while 9 patients (21.4%) indicated subsequent subluxation events. A prospective randomized control trial comparing arthroscopic repair with nonoperative treatment among 24 young, male military servicemembers (mean age, 22.4 years) presenting to a single center with primary anterior dislocation was performed.12 At mean 3-year follow-up, 75% of patients randomized to the nonoperative treatment experienced failure, whereas only 1 in 9 patients (11.1%) experienced recurrent instability. Among high-risk civilian demographics, this paradigm shift has gained significant support, including several level 1 studies30,31,53 and Markov decision modeling.35 Arthroscopic Bankart repair has a dramatically lower recurrent dislocation rate (7% vs 38%), improved patient-reported outcomes, and greater levels of return to sport than patients receiving arthroscopic lavage.53 Economic and decision analysis has also established arthroscopic stabilization as the preferred treatment strategy and a more cost-effective method than nonoperative management in patients aged 15 to 25 years.9,17
Recurrent Instability
Despite earlier surgical interventions among military cohorts, many servicemembers still present with untreated recurrent anterior instability. With chronic persistent subluxations or dislocation, capsular stretch, inferior glenohumeral ligament laxity, and labral tear extension may exacerbate underlying pathology and contribute to the development of bidirectional instability or other potential pain generators. The arthroscopic Bankart repair has long been an established treatment for anterior shoulder instability, while rates of the historical gold standard—open Bankart repair—have demonstrated continued decline among practicing surgeons.47 No statistically significant differences were seen in a randomized controlled trial of West Point cadets undergoing open and arthroscopic Bankart repair for anterior subluxation.43 In an earlier level 1 trial of 61 military patients, comparable clinical outcomes were seen between open and arthroscopic stabilization for recurrent shoulder instability, although open procedures had significantly longer operative times and greater losses in motion.11 Open Bankart repair was associated with failure in revision surgery among 3865 triservice military patients, although this may be susceptible to selection or indication bias. Other investigators have reported contrary results, demonstrating 2 times the failure rate for arthroscopic fixation compared with an open approach in a level 1 study.39 In contact athletes, arthroscopic stabilization demonstrated 2 times the failure rate compared with an open approach.54 Thus, there remains significant controversy in the operative management of anterior shoulder instability, and while both approaches hold merit, further study is necessary to determine the nuance of application of various techniques.
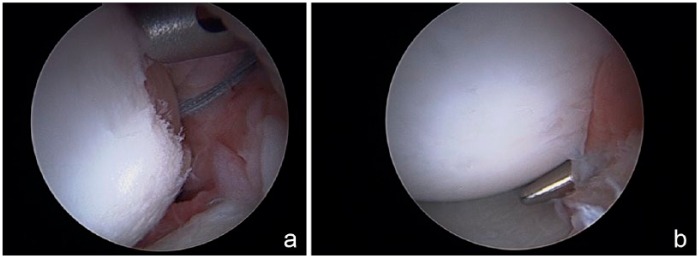
Primary shoulder instability is characteristically associated with shallow, on-track Hill-Sachs lesions,23 while repeated instability events lead to a heightened risk of further bony erosion and engaging bipolar defects.16,40,49 More complex osseous lesions must be critically evaluated to ensure comprehensive management. While the glenoid has traditionally been the area of focus, characteristics of the Hill-Sachs lesion have recently received increased attention.15,27 Though often ill-defined, clinically significant humeral-based defects may be effectively treated with remplissage as a nonanatomic complement to arthroscopic anterior stabilization (Figure 2). A randomized clinical trial comparing remplissage and Bankart reconstruction to Bankart alone demonstrated no recurrences in the combined group compared with 20% recurrence in the isolated group.26 Patients with moderate bone loss and engaging Hill-Sachs lesions had no recurrence after primary instability repair with combined remplissage and Bankart repair (0%).36 There was less success in revision surgery, with a recurrence rate of 36% in that population.
Figure 2.
(a) Arthroscopic view of a right shoulder from the anterior superior portal. A Hill-Sachs lesion is visualized with suture anchor placed through the infraspinatus tendon and capsule and inserted into the posterior aspect of the defect. The drill guide is positioned for the second anterior anchor. (b) After completion of the remplissage, the tendon is approximated at the edge of the articular cartilage defect, effectively excluding the Hill-Sachs defect from the joint.
Cases of combined and/or critical bone loss (with or without engagement) are indicated for anterior bone block procedures. In one of the largest surveys of isolated labral repairs among 3854 military patients, only 5% of the cohort underwent revision stabilization for subsequent instability, but an additional 8.8% underwent shoulder-related medical discharge at short-term, postoperative follow-up.63 Contrary to previously established thresholds, lower Western Ontario Shoulder Instability (WOSI) scores were seen after arthroscopic Bankart reconstruction in military patients with subcritical glenoid bone loss of greater than 13.5%, even in patients who did not sustain a recurrence of instability.58 The additive effect of bipolar, subcritical bone loss compromises the biomechanical efficacy of the Bankart procedure, even with as little as 2 mm anterior glenoid defect.1 These studies underscore the importance of patient-reported measures in outcome reporting, careful scrutiny of preoperative imaging, and personalized surgical management, as these extend beyond the traditional limited endpoints of instability recurrence and surgical revision.
Revision Setting
When prior arthroscopic or open stabilization fails, it is of paramount importance to critically evaluate the reasons for failure. Traumatic anterior instability may recur with continued at-risk activity, but technical error (eg, inadequate mobilization or tissue tensioning, poor anchor position, compromised knot security, and/or inadequate points of fixation), unrecognized pathology, bone loss, diminished tissue quality, patient noncompliance, and/or inadequate rehabilitation are more common contributing factors. With technical errors and minimal bone loss, revision anterior capsulolabral reconstruction may be appropriately considered with recurrent instability or positional apprehension.
Alternatively, anterior glenoid augmentation may also have merit, and sources of bone graft may include the coracoid, iliac crest, distal clavicle,60 and allograft sources. The modified Latarjet procedure offers benefits related to its reconstitution of normal glenoid stock8,28 but also exhibits inherent advantages because of its so-called “sling effect” with associated conjoint tendon transfer (Figure 3). In a previous series of 64 military patients with a high preponderance of failed prior procedure (78%) and subsequent Latarjet (91%), nearly 70% of patients were able to return to high-demand occupational function after anterior bone block surgery, and 23% reported apprehension or transient subluxation, although no episodes of anterior dislocation were noted.64 A 15.2% rate of recurrent instability was seen among Navy Midshipmen at a mean 7 years after modified Bristow procedure, indicating a slightly lower recurrence rate in the primary treatment setting.57 With larger glenoid defects, the Eden-Hybinette procedure (ie, tricortical iliac crest) or distal tibial allograft transplantation may be more effective to reconstruct the native anatomy.8,28,52 More recently, distal clavicular autograft for replacing glenoid rim defects with minimal donor site morbidity and use of an arthroscopic technique has been suggested (Figure 4).
Figure 3.
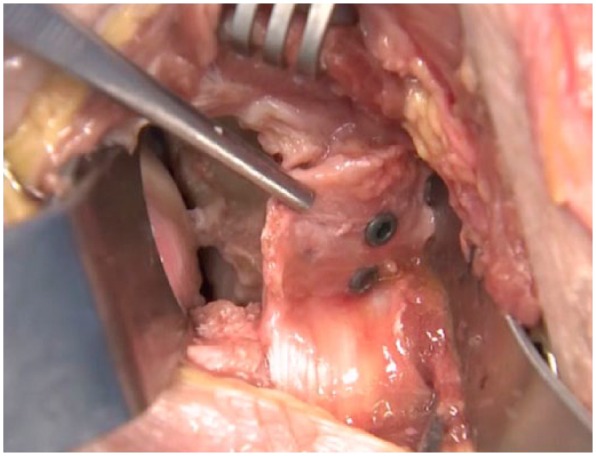
A right shoulder at the completion of Latarjet bone block transfer. A Fukuda retractor retracts the humeral head and a glenoid retractor is placed medially. A pair of forceps is placed on the edge of the coracoacromial ligament, which will be used for capsular reconstruction. The 2 visualized screws are placed through the coracoid bone block parallel with the glenoid surface.
Figure 4.

Distal clavicle transfer to bone using suture anchors demonstrating the potential of an autograft distal clavicle to reconstruct anterior glenoid bone loss.
Conclusion
Within the US military, anterior shoulder instability is a common source of disability that may have long-term repercussions on upper extremity function and occupational outcomes. Young, active male servicemembers and other high-risk subsets with first-time anterior instability should be carefully evaluated for primary arthroscopic Bankart repair. There is still no consensus on the ideal management of complex, recurrent anterior shoulder instability or cases of failed primary anterior stabilization. Isolated primary or revision Bankart repair, either arthroscopic or open, should be considered with limited anterior glenoid involvement and reasonable tissue quality. Alternatively, other potential options such as remplissage or anterior glenoid bone augmentation procedures should be preferentially considered for off-track or clinically significant bipolar defects.
Footnotes
The following authors declared potential conflicts of interest: Brett D. Owens, MD, is a paid consultant for MTF/Conmed and Mitek and receives royalties from Springer, Elsevier, and Slack. John M. Tokish, MD, is a paid consultant for Arthrex and Dupey-Mitek.
References
- 1. Arciero RA, Parrino A, Bernhardson AS, et al. The effect of a combined glenoid and Hill-Sachs defect on glenohumeral stability: a biomechanical cadaveric study using 3-dimensional modeling of 142 patients. Am J Sports Med. 2015;43:1422-1429. [DOI] [PubMed] [Google Scholar]
- 2. Arciero RA, Wheeler JH, Ryan JB, McBride JT. Arthroscopic Bankart repair versus nonoperative treatment for acute, initial anterior shoulder dislocations. Am J Sports Med. 1994;22:589-594. [DOI] [PubMed] [Google Scholar]
- 3. Balg F, Boileau P. The instability severity index score. A simple pre-operative score to select patients for arthroscopic or open shoulder stabilisation. J Bone Joint Surg Br. 2007;89:1470-1477. [DOI] [PubMed] [Google Scholar]
- 4. Belmont PJ Jr, Goodman GP, Waterman B, DeZee K, Burks R, Owens BD. Disease and nonbattle injuries sustained by a U.S. Army Brigade Combat Team during Operation Iraqi Freedom. Mil Med. 2010;175:469-476. [DOI] [PubMed] [Google Scholar]
- 5. Bernhardson AS, Bailey JR, Solomon DJ, Stanley M, Provencher MT. Glenoid bone loss in the setting of an anterior labroligamentous periosteal sleeve avulsion tear. Am J Sports Med. 2014;42:2136-2140. [DOI] [PubMed] [Google Scholar]
- 6. Bhatia S, Ghodadra NS, Romeo AA, et al. The importance of the recognition and treatment of glenoid bone loss in an athletic population. Sports Health. 2011;3:435-440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bhatia S, Saigal A, Frank RM, et al. Glenoid diameter is an inaccurate method for percent glenoid bone loss quantification: analysis and techniques for improved accuracy. Arthroscopy. 2015;31:608-614. [DOI] [PubMed] [Google Scholar]
- 8. Bhatia S, Van Thiel GS, Gupta D, et al. Comparison of glenohumeral contact pressures and contact areas after glenoid reconstruction with Latarjet or distal tibial osteochondral allografts. Am J Sports Med. 2013;41:1900-1908. [DOI] [PubMed] [Google Scholar]
- 9. Bishop JA, Crall TS, Kocher MS. Operative versus nonoperative treatment after primary traumatic anterior glenohumeral dislocation: expected-value decision analysis. J Shoulder Elbow Surg. 2011;20:1087-1094. [DOI] [PubMed] [Google Scholar]
- 10. Bishop JY, Jones GL, Rerko MA, Donaldson C; MOON Shoulder Group. 3-D CT is the most reliable imaging modality when quantifying glenoid bone loss. Clin Orthop Relat Res. 2013;471:1251-1256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bottoni CR, Smith EL, Berkowitz MJ, Towle RB, Moore JH. Arthroscopic versus open shoulder stabilization for recurrent anterior instability: a prospective randomized clinical trial. Am J Sports Med. 2006;34:1730-1737. [DOI] [PubMed] [Google Scholar]
- 12. Bottoni CR, Wilckens JH, DeBerardino TM, et al. A prospective, randomized evaluation of arthroscopic stabilization versus nonoperative treatment in patients with acute, traumatic, first-time shoulder dislocations. Am J Sports Med. 2002;30:576-580. [DOI] [PubMed] [Google Scholar]
- 13. Burkhart SS, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy. 2000;16:677-694. [DOI] [PubMed] [Google Scholar]
- 14. Buss DD, Lynch GP, Meyer CP, Huber SM, Freehill MQ. Nonoperative management for in-season athletes with anterior shoulder instability. Am J Sports Med. 2004;32:1430-1433. [DOI] [PubMed] [Google Scholar]
- 15. Buza JA 3rd, Iyengar JJ, Anakwenze OA, Ahmad CS, Levine WN. Arthroscopic Hill-Sachs remplissage: a systematic review. J Bone Joint Surg Am. 2014;96:549-555. [DOI] [PubMed] [Google Scholar]
- 16. Cetik O, Uslu M, Ozsar BK. The relationship between Hill-Sachs lesion and recurrent anterior shoulder dislocation. Acta Orthop Belg. 2007;73:175-178. [PubMed] [Google Scholar]
- 17. Crall TS, Bishop JA, Guttman D, Kocher M, Bozic K, Lubowitz JH. Cost-effectiveness analysis of primary arthroscopic stabilization versus nonoperative treatment for first-time anterior glenohumeral dislocations. Arthroscopy. 2012;28:1755-1765. [DOI] [PubMed] [Google Scholar]
- 18. DeBerardino TM, Arciero RA, Taylor DC. Arthroscopic stabilization of acute initial anterior shoulder dislocation: the West Point experience. J South Orthop Assoc. 1996;5:263-271. [PubMed] [Google Scholar]
- 19. DeBerardino TM, Arciero RA, Taylor DC, Uhorchak JM. Prospective evaluation of arthroscopic stabilization of acute, initial anterior shoulder dislocations in young athletes. Two- to five-year follow-up. Am J Sports Med. 2001;29:586-592. [DOI] [PubMed] [Google Scholar]
- 20. Dickens JF, Kilcoyne KG, Giuliani J, Owens BD. Circumferential labral tears resulting from a single anterior glenohumeral instability event: a report of 3 cases in young athletes. Am J Sports Med. 2012;40:213-217. [DOI] [PubMed] [Google Scholar]
- 21. Dickens JF, Kilcoyne KG, Haniuk E, Owens BD. Combined lesions of the glenoid labrum. Phys Sportsmed. 2012;40:102-108. [DOI] [PubMed] [Google Scholar]
- 22. Dickens JF, Owens BD, Cameron KL, et al. Return to play and recurrent instability after in-season anterior shoulder instability: a prospective multicenter study. Am J Sports Med. 2014;42:2842-2850. [DOI] [PubMed] [Google Scholar]
- 23. Di Giacomo G, Golijanin P, Sanchez G, Provencher MT. Radiographic analysis of the Hill-Sachs lesion in anteroinferior shoulder instability after first-time dislocations. Arthroscopy. 2016;32:1509-1514. [DOI] [PubMed] [Google Scholar]
- 24. Di Giacomo G, Itoi E, Burkhart SS. Evolving concept of bipolar bone loss and the Hill-Sachs lesion: from “engaging/non-engaging” lesion to “on-track/off-track” lesion. Arthroscopy. 2014;30:90-98. [DOI] [PubMed] [Google Scholar]
- 25. Feagin JA., Jr. Elastic arm-torso harness. J Sports Med. 1974;2:99-101. [DOI] [PubMed] [Google Scholar]
- 26. Franceschi F, Papalia R, Rizzello G, et al. Remplissage repair—new frontiers in the prevention of recurrent shoulder instability: a 2-year follow-up comparative study. Am J Sports Med. 2012;40:2462-2469. [DOI] [PubMed] [Google Scholar]
- 27. Garcia GH, Wu HH, Liu JN, Huffman GR, Kelly JD 4th. Outcomes of the remplissage procedure and its effects on return to sports: average 5-year follow-up. Am J Sports Med. 2016;44:1124-1130. [DOI] [PubMed] [Google Scholar]
- 28. Ghodadra N, Gupta A, Romeo AA, et al. Normalization of glenohumeral articular contact pressures after Latarjet or iliac crest bone-grafting. J Bone Joint Surg Am. 2010;92:1478-1489. [DOI] [PubMed] [Google Scholar]
- 29. Hovelius L. Shoulder dislocation in Swedish ice hockey players. Am J Sports Med. 1978;6:373-377. [DOI] [PubMed] [Google Scholar]
- 30. Jakobsen BW, Johannsen HV, Suder P, Søjbjerg JO. Primary repair versus conservative treatment of first-time traumatic anterior dislocation of the shoulder: a randomized study with 10-year follow-up. Arthroscopy. 2007;23:118-123. [DOI] [PubMed] [Google Scholar]
- 31. Kirkley A, Werstine R, Ratjek A, Griffin S. Prospective randomized clinical trial comparing the effectiveness of immediate arthroscopic stabilization versus immobilization and rehabilitation in first traumatic anterior dislocations of the shoulder: long-term evaluation. Arthroscopy. 2005;21:55-63. [DOI] [PubMed] [Google Scholar]
- 32. Krøner K, Lind T, Jensen J. The epidemiology of shoulder dislocations. Arch Orthop Trauma Surg. 1989;108:288-290. [DOI] [PubMed] [Google Scholar]
- 33. Lo IK, Parten PM, Burkhart SS. The inverted pear glenoid: an indicator of significant glenoid bone loss. Arthroscopy. 2004;20:169-174. [DOI] [PubMed] [Google Scholar]
- 34. Markenstein JE, Jaspars KC, van der Hulst VP, Willems WJ. The quantification of glenoid bone loss in anterior shoulder instability; MR-arthro compared to 3D-CT. Skeletal Radiol. 2014;43:475-483. [DOI] [PubMed] [Google Scholar]
- 35. Mather RC 3rd, Orlando LA, Henderson RA, Lawrence JT, Taylor DC. A predictive model of shoulder instability after a first-time anterior shoulder dislocation. J Shoulder Elbow Surg. 2011;20:259-266. [DOI] [PubMed] [Google Scholar]
- 36. McCabe MP, Weinberg D, Field LD, O’Brien MJ, Hobgood ER, Savoie FH 3rd. Primary versus revision arthroscopic reconstruction with remplissage for shoulder instability with moderate bone loss. Arthroscopy. 2014;30:444-450. [DOI] [PubMed] [Google Scholar]
- 37. Metzger PD, Barlow B, Leonardelli D, Peace W, Solomon DJ, Provencher MT. Clinical application of the “glenoid track” concept for defining humeral head engagement in anterior shoulder instability: a preliminary report. Orthop J Sports Med. 2013;1(2):2325967113496213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Milgrom C, Mann G, Finestone A. A prevalence study of recurrent shoulder dislocations in young adults. J Shoulder Elbow Surg. 1998;7:621-624. [DOI] [PubMed] [Google Scholar]
- 39. Mohtadi NG, Chan DS, Hollinshead RM, et al. A randomized clinical trial comparing open and arthroscopic stabilization for recurrent traumatic anterior shoulder instability: two-year follow-up with disease-specific quality-of-life outcomes. J Bone Joint Surg Am. 2014;96:353-360. [DOI] [PubMed] [Google Scholar]
- 40. Nakagawa S, Ozaki R, Take Y, Iuchi R, Mae T. Relationship between glenoid defects and Hill-Sachs lesions in shoulders with traumatic anterior instability. Am J Sports Med. 2015;43:2763-2773. [DOI] [PubMed] [Google Scholar]
- 41. Nordqvist A, Petersson CJ. Incidence and causes of shoulder girdle injuries in an urban population. J Shoulder Elbow Surg. 1995;4:107-112. [DOI] [PubMed] [Google Scholar]
- 42. Olds M, Ellis R, Donaldson K, Parmar P, Kersten P. Risk factors which predispose first-time traumatic anterior shoulder dislocations to recurrent instability in adults: a systematic review and meta-analysis. Br J Sports Med. 2015;49:913-922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Owens BD, Cameron KL, Peck KY, et al. Arthroscopic versus open stabilization for anterior shoulder subluxations. Orthop J Sports Med. 2015;3(1):2325967115571084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Owens BD, Dawson L, Burks R, Cameron KL. Incidence of shoulder dislocation in the United States military: demographic considerations from a high-risk population. J Bone Joint Surg Am. 2009;91:791-796. [DOI] [PubMed] [Google Scholar]
- 45. Owens BD, DeBerardino TM, Nelson BJ, et al. Long-term follow-up of acute arthroscopic Bankart repair for initial anterior shoulder dislocations in young athletes. Am J Sports Med. 2009;37:669-673. [DOI] [PubMed] [Google Scholar]
- 46. Owens BD, Duffey ML, Nelson BJ, DeBerardino TM, Taylor DC, Mountcastle SB. The incidence and characteristics of shoulder instability at the United States Military Academy. Am J Sports Med. 2007;35:1168-1173. [DOI] [PubMed] [Google Scholar]
- 47. Owens BD, Harrast JJ, Hurwitz SR, Thompson TL, Wolf JM. Surgical trends in Bankart repair: an analysis of data from the American Board of Orthopaedic Surgery certification examination. Am J Sports Med. 2011;39:1865-1869. [DOI] [PubMed] [Google Scholar]
- 48. Owens BD, Nelson BJ, Duffey ML, et al. Pathoanatomy of first-time, traumatic, anterior glenohumeral subluxation events. J Bone Joint Surg Am. 2010;92:1605-1611. [DOI] [PubMed] [Google Scholar]
- 49. Ozaki R, Nakagawa S, Mizuno N, Mae T, Yoneda M. Hill-Sachs lesions in shoulders with traumatic anterior instability: evaluation using computed tomography with 3-dimensional reconstruction. Am J Sports Med. 2014;42:2597-2605. [DOI] [PubMed] [Google Scholar]
- 50. Piasecki DP, Verma NN, Romeo AA, Levine WN, Bach BR Jr, Provencher MT. Glenoid bone deficiency in recurrent anterior shoulder instability: diagnosis and management. J Am Acad Orthop Surg. 2009;17:482-493. [DOI] [PubMed] [Google Scholar]
- 51. Provencher MT, Frank RM, Leclere LE, et al. The Hill-Sachs lesion: diagnosis, classification, and management. J Am Acad Orthop Surg. 2012;20:242-252. [DOI] [PubMed] [Google Scholar]
- 52. Provencher MT, Ghodadra N, LeClere L, Solomon DJ, Romeo AA. Anatomic osteochondral glenoid reconstruction for recurrent glenohumeral instability with glenoid deficiency using a distal tibia allograft. Arthroscopy. 2009;25:446-452. [DOI] [PubMed] [Google Scholar]
- 53. Rerko MA, Pan X, Donaldson C, Jones GL, Bishop JY. Comparison of various imaging techniques to quantify glenoid bone loss in shoulder instability. J Shoulder Elbow Surg. 2013;22:528-534. [DOI] [PubMed] [Google Scholar]
- 54. Rhee YG, Ha JH, Cho NS. Anterior shoulder stabilization in collision athletes: arthroscopic versus open Bankart repair. Am J Sports Med. 2006;34:979-985. [DOI] [PubMed] [Google Scholar]
- 55. Rokous JR, Feagin JA, Abbott HG. Modified axillary roentgenogram. A useful adjunct in the diagnosis of recurrent instability of the shoulder. Clin Orthop Relat Res. 1972;82:84-86. [PubMed] [Google Scholar]
- 56. Rowe CR. Prognosis in dislocations of the shoulder. J Bone Joint Surg Am. 1956;38-A:957-977. [PubMed] [Google Scholar]
- 57. Schroder DT, Provencher MT, Mologne TS, Muldoon MP, Cox JS. The modified Bristow procedure for anterior shoulder instability: 26-year outcomes in Naval Academy midshipmen. Am J Sports Med. 2006;34:778-786. [DOI] [PubMed] [Google Scholar]
- 58. Shaha JS, Cook JB, Song DJ, et al. Redefining “critical” bone loss in shoulder instability: functional outcomes worsen with “subcritical” bone loss. Am J Sports Med. 2015;43:1719-1725. [DOI] [PubMed] [Google Scholar]
- 59. Taylor DC, Arciero RA. Pathologic changes associated with shoulder dislocations. Arthroscopic and physical examination findings in first-time, traumatic anterior dislocations. Am J Sports Med. 1997;25:306-311. [DOI] [PubMed] [Google Scholar]
- 60. Tokish JM, Fitzpatrick K, Cook JB, Mallon WJ. Arthroscopic distal clavicular autograft for treating shoulder instability with glenoid bone loss. Arthrosc Tech. 2014;3:e475-e481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Tokish JM, McBratney CM, Solomon DJ, Leclere L, Dewing CB, Provencher MT. Arthroscopic repair of circumferential lesions of the glenoid labrum. J Bone Joint Surg Am. 2009;91:2795-2802. [DOI] [PubMed] [Google Scholar]
- 62. Waterman BR, Arroyo W, Heida K, Burks R, Pallis M. SLAP repairs with combined procedures have lower failure rate than isolated repairs in a military population: surgical outcomes with minimum 2-year follow-up. Orthop J Sports Med. 2015;3(8):2325967115599154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Waterman BR, Burns TC, McCriskin B, Kilcoyne K, Cameron KL, Owens BD. Outcomes after Bankart repair in a military population: predictors for surgical revision and long-term disability. Arthroscopy. 2014;30:172-177. [DOI] [PubMed] [Google Scholar]
- 64. Waterman BR, Chandler PJ, Teague E, Provencher MT, Tokish JM, Pallis MP. Short-term outcomes of glenoid bone block augmentation for complex anterior shoulder instability in a high-risk population. Arthroscopy. 2016;32:1784-1790. [DOI] [PubMed] [Google Scholar]
- 65. Wheeler JH, Ryan JB, Arciero RA, Molinari RN. Arthroscopic versus nonoperative treatment of acute shoulder dislocations in young athletes. Arthroscopy. 1989;5:213-217. [DOI] [PubMed] [Google Scholar]
- 66. Yamamoto N, Itoi E, Abe H, et al. Contact between the glenoid and the humeral head in abduction, external rotation, and horizontal extension: a new concept of glenoid track. J Shoulder Elbow Surg. 2007;16:649-656. [DOI] [PubMed] [Google Scholar]