Abstract
Context:
Posterior shoulder instability has become more frequently recognized and treated as a unique subset of shoulder instability, especially in the military. Posterior shoulder pathology may be more difficult to accurately diagnose than its anterior counterpart, and commonly, patients present with complaints of pain rather than instability. “Posterior instability” may encompass both dislocation and subluxation, and the most common presentation is recurrent posterior subluxation. Arthroscopic and open treatment techniques have improved as understanding of posterior shoulder instability has evolved.
Evidence Acquisition:
Electronic databases including PubMed and MEDLINE were queried for articles relating to posterior shoulder instability.
Study Design:
Clinical review.
Level of Evidence:
Level 4.
Results:
In low-demand patients, nonoperative treatment of posterior shoulder instability should be considered a first line of treatment and is typically successful. Conservative treatment, however, is commonly unsuccessful in active patients, such as military members. Those patients with persistent shoulder pain, instability, or functional limitations after a trial of conservative treatment may be considered surgical candidates. Arthroscopic posterior shoulder stabilization has demonstrated excellent clinical outcomes, high patient satisfaction, and low complication rates. Advanced techniques may be required in select cases to address bone loss, glenoid dysplasia, or revision.
Conclusion:
Posterior instability represents about 10% of shoulder instability and has become increasingly recognized and treated in military members. Nonoperative treatment is commonly unsuccessful in active patients, and surgical stabilization can be considered in patients who do not respond. Isolated posterior labral repairs constitute up to 24% of operatively treated labral repairs in a military population. Arthroscopic posterior stabilization is typically considered as first-line surgical treatment, while open techniques may be required in complex or revision settings.
Keywords: instability, shoulder arthroscopy, posterior stabilization
Posterior shoulder instability has become an increasingly recognized and studied subset of shoulder instability and is endemic in the military population. Accurate identification and prompt treatment of posterior glenohumeral pathology may be more difficult than anterior, as patients may present with a spectrum of less obvious clinical complaints. Consequently, posterior instability may go unrecognized, leading to improper diagnoses and delays in treatment.18,36 Care should be taken to distinguish between dislocation, where the humeral head is completely displaced from its articulation with the glenoid, and subluxation, an incomplete or partial dislocation of the joint. It is also vital to differentiate between physiologic posterior laxity, which may be present in the asymptomatic shoulder, and instability, where excessive glenohumeral translation leads to symptoms.37 The term posterior instability may encompass a large spectrum of pathoanatomy involving the labrum, capsule, glenohumeral ligaments, or underlying bony articulation, and it may be used to describe both posterior dislocation and subluxation. The most common type of posterior shoulder instability is recurrent posterior subluxation, and the most common presenting complaint is pain.
Epidemiology
Posterior instability represents 10% of all shoulder instability events in the active, young, military population, but posterior and combined labral repairs comprise up to 40% of operatively treated instability events among that population. Isolated posterior labral repairs constitute up to 24% of operative shoulder instability events, which may be higher than previously reported.12,31,41 Injuries typically occur in athletes participating in high-demand, dynamic posterior loading activities, including weightlifters and football linemen. Recently, posterior instability has also been described in unique populations, including baseball players’ lead shoulders during batting and individuals who participate in rifle shooting.9,20,44 Importantly, most cases of posterior instability in a military setting are not because of single, traumatic events or seizures but rather from repetitive microtrauma from military-specific activities such as pushups, combatives, and weightlifting. Advances in magnetic resonance imaging (MRI) and arthroscopy have been helpful in evolving the understanding of this important distinction.
Pathoanatomy
Posterior instability may occur over a large spectrum, from subtle posterior subluxation causing minimal symptoms to frank posterior dislocation. Both traumatic and atraumatic mechanisms may produce posterior instability. A thorough understanding of these differing mechanisms will help the clinician accurately identify underlying pathology and guide treatment. Primary injury mechanisms may include (1) repetitive microtrauma leading to attenuation injuries to the posterior capsule and labrum (most common in the military population); (2) acute, traumatic posterior force resulting in shearing at the chondrolabral junction and subsequent capsulolabral detachment; and (3) insidious onset laxity resulting in stretching of the posterior capsule and passive stabilizers.10
Posterior instability may also present as a secondary effect of abnormal underlying anatomy, including glenoid retroversion, large reverse Hill-Sachs injury, and glenoid dysplasia.36 Less commonly, especially among military members, an underlying connective tissue disorder such as Ehlers-Danlos syndrome may predispose a patient to posterior instability.38 Voluntary or habitual shoulder dislocators should be approached cautiously as a separate subgroup. These patients should be differentiated from positional dislocators. Positional dislocators are able to subluxate or dislocate their shoulder by altering scapular positioning, although the maneuver causes pain and discomfort. The habitual dislocator involves the so-called “party trick” shoulder, which is typically less painful or even painless. While positional dislocators may benefit from stabilization, surgical intervention should be avoided in voluntary dislocators secondary to reported poorer postoperative outcomes.26,35
Posterior labral injuries are commonly associated with concurrent intra-articular pathology, including anterior labral tears, superior labral anterior posterior (SLAP) tears, and reverse humeral avulsion of the glenohumeral ligament (rHAGL).21 In fact, in a series of 231 shoulder stabilizations for instability in a military population, isolated posterior stabilizations comprised 24% while combined injuries comprised 19% of shoulder stabilizations.41 Consequently, military providers must have a heightened awareness for detecting posterior instability among military members. Glenoid retroversion beyond the average 5° to 10° has been shown to be a risk factor for developing subsequent posterior instability in a prospective study of healthy subjects. For every 1° increase in glenoid retroversion, the risk for posterior instability increases 17%.29
Clinical Presentation
As previously noted, accurate identification of posterior instability may be difficult due to a wide variation in clinical complaints. Frank posterior dislocations will typically present with the shoulder held in an adducted, internally rotated position. A high index of suspicion should be maintained in patients presenting with shoulder pain after seizure, electrocution, or alcohol intoxication. Posterior dislocations can present in the acute or chronic setting. In chronic locked dislocations, the examiner may notice a profound loss of external rotation and a mechanical block.
Recurrent posterior subluxation, the most common form of posterior instability, may not present with instability but rather with pain and/or weakness. Some patients may report symptoms only at the end of activity when the dynamic muscle stabilizers around the glenohumeral joint become fatigued. The classic mechanism for posterior instability involves a posteriorly directed force to a forward flexed, internally rotated, and adducted arm. A detailed description of the offending activity, the position of the arm, and how force was applied may lead the clinician to an accurate diagnosis. Attention should be paid to weightlifters performing bench press or pushups, where posteriorly directed loads are imparted onto the shoulder. As military members are required to perform pushups to meet individual physical requirements, military providers should maintain a high index of suspicion in patients complaining of shoulder pain. Pushups are the major contributing factor in military patients who develop posterior shoulder instability.
A detailed physical examination of the shoulder will assist the clinician in accurate diagnosis of posterior instability. Shoulder range of motion and strength should be assessed and compared with the contralateral shoulder. Commonly, active and passive range of motion may be normal and symmetric, with the exception of throwers who commonly have increased physiologic external rotation and posterior capsular laxity in the throwing shoulder.8 The clinician should evaluate for atrophy, scapulothoracic dyskinesis, and scapular winging. The Beighton score may be used to assess generalized ligamentous laxity, which has been shown to correlate with shoulder instability.5 Specific physical examination tests include the posterior load-and-shift, the jerk test, and the posterior apprehension test.30 The posterior load-and-shift examination and apprehension tests may be performed in the seated or supine position. The “push-pull,” a modification of the posterior load-and-shift, may also be beneficial to stabilize the scapula and control the distal extremity. The combination of the jerk test and the Kim test has been shown to be 97% sensitive for the detection of a posteroinferior labral tear.22 A comprehensive evaluation for instability should include physical examination testing for anterior and superior labral tears, as these conditions may coexist. If the patient has a positive sulcus sign in addition to the maneuvers described above, this would suggest multidirectional instability with a primary posterior component.
Imaging
Radiographic workup for the shoulder should include anteroposterior and axillary views. Posterior dislocation, posterior glenoid bone loss, glenoid dysplasia, and posterior subluxation of the humeral head may be noted on the axillary view (Figure 1). MRI is helpful for evaluating the posterior labrum, the posterior capsule, and the remainder of the intra-articular structures. In the acute setting, intra-articular contrast may not be needed as the labrum is typically well visualized in the presence of a hemarthrosis; however, intra-articular contrast may be more helpful in a chronic setting to aid in delineation of tears. Surgeons should be aware that while anterior labral anatomy is quite variable due to the sublabral foramen, the posterior labrum tends to be more homogenous in appearance among patients. A subchondral cleft (labrum and capsule attached but no tear) is suspicious for pathology and can be associated with instability; however, this may also be a normal finding.6 Axial views are useful to evaluate for labral tears (which may extend anteriorly or superiorly), posterior humeral head subluxation, and reverse Hill-Sachs injuries to the anterior humeral head (Figure 2). Coronal views may be helpful to rule out a posterior rHAGL. If the clinician suspects glenoid retroversion or dysplasia, a computed tomography (CT) scan with 3-dimensional reconstructions may be performed to allow the clinician a better understanding of the underlying anatomy (Figure 3). It cannot be overstated that imaging should be scrutinized for concurrent pathology.
Figure 1.

Axial radiograph demonstrating a locked posterior glenohumeral dislocation.
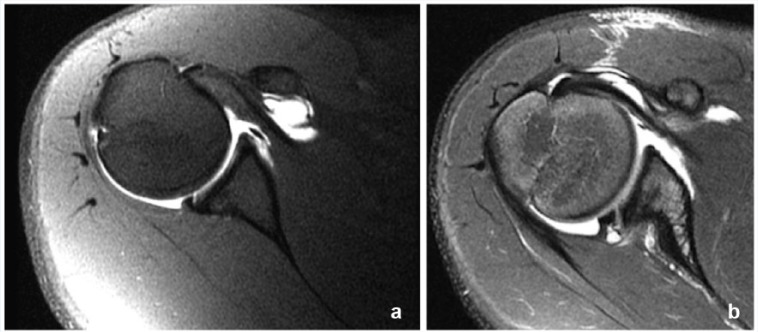
Figure 2.
(a) T2-weighted axial magnetic resonance image demonstrating a posterior labral tear. (b) Posterior labral tear with paralabral cyst.
Figure 3.
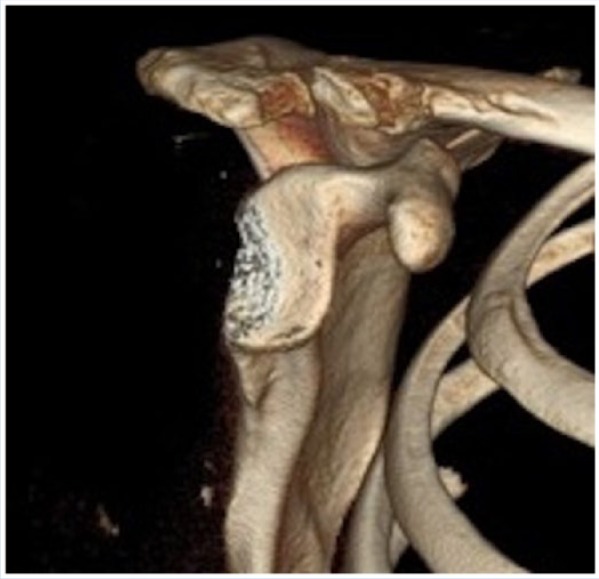
Three-dimensional computed tomography reconstruction of the glenoid performed with subtraction of the humeral head. Note the significant posterior glenoid bone loss.
Surgical Treatment
Patients who experience recurrent shoulder pain, instability, or functional limitations after a course of conservative treatment over 3 to 6 months may be considered candidates for surgery. We consider surgical treatment for the patient with a symptomatic posterior labral tear, unilateral posterior instability with a patulous or incompetent posterior capsule, or in select multidirectional instability patients with predominantly posterior symptoms. While surgery may be successfully performed through both open and arthroscopic techniques, arthroscopy affords the surgeon the ability to address concurrent intra-articular pathology in the same setting.
Patients with excessive glenoid dysplasia (retroversion >15°) as well as patients with posterior bone loss should be counseled that soft tissue repair may be at increased risk for failure due to altered underlying bony support.32 While glenoid osteotomy is typically only considered in revision settings, we may in rare instances consider a primary bony procedure in patients with more than 25 degrees of retroversion. Surgical options may include glenoid osteotomy, posterior bone block, or osteoarticular augment. No maximum acceptable radiographic limit for retroversion has yet been established by the current literature. Posterior bone block augmentation may also be considered for patients with marked posterior bone loss in whom soft tissue repair may likewise fail. Chronic, locked posterior shoulder dislocations may require open treatment via subscapularis transfer or tenodesis, humeral head allograft reconstruction, or shoulder arthroplasty in severe cases.13,14,47
Arthroscopic repair may be successfully performed in the beach-chair (Figure 4) or lateral positions. Important surgical considerations include not only repair of the labral tear but also retensioning of the inferior glenohumeral ligament. Labral repair is commonly performed with the use of suture anchors placed into the glenoid at the chondrolabral junction to reapproximate and retension the labrum and capsule (Figure 5). Capsular plication may be performed concurrently to reduce capsular volume and, thus, limit glenohumeral translation. Thermal capsulorraphy, which initially gained popularity for treating shoulder instability given the technical ease of the procedure, has been largely abandoned over concerns for high failure rates, stiffness, and nerve irritation.19,28
Figure 4.
(a) Operative view of beach-chair setup with use of an arm positioner. (b) Posterolateral portal for anchor placement. Portal is placed in line with the posterior border of the distal clavicle. (c) Operative view of anchor placement through the posterolateral portal.
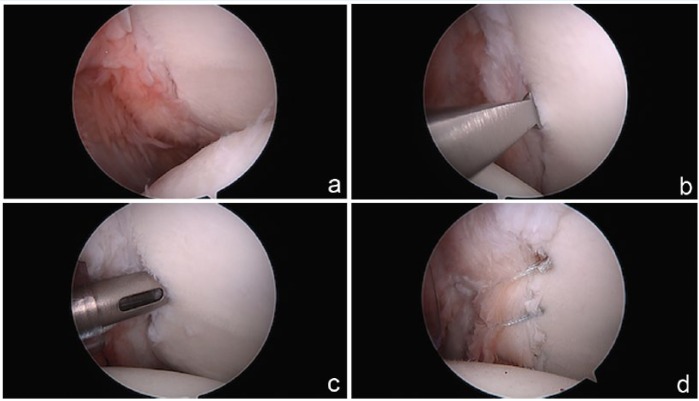
Figure 5.
(a) Arthroscopic view of a posterior labral tear. (b) Liberation of the labrum from the glenoid in preparation for repair. (c) Drilling in preparation for anchor placement through the posterolateral portal. (d) Completed posterior labral repair via knotless technique viewed from the anterosuperior portal.
Revision surgery requires careful consideration of any patient factors that contributed to failure and an understanding of the underlying anatomy that may have predisposed the patient to failure. Arthroscopic revision repair may be considered in the setting of an acute reinjury or concurrent intra-articular pathology. In many cases, the surgeon may need to address underlying multidirectional instability through a variety of techniques, including capsular plication, rotator interval closure, or open capsular shift.7 Bone loss or significant glenoid retroversion may need to be addressed, especially in the revision setting, with posterior bone block augmentation or glenoid osteotomy.
Clinical Outcomes
Reported clinical outcomes after arthroscopic posterior stabilization are good to excellent, with high patient satisfaction and low reported recurrence rates.3,10,11,24 In the largest prospective study to date for isolated posterior instability, Bradley et al4 reported excellent results in 200 patients undergoing labral repair with or without capsular plication; 94% of patients were satisfied with the results and would undergo surgery again, 90% of patients returned to sports—although only 64% returned at the same level of play—and 7% of patients reported persistent instability after surgery (62.5% of those patients had signs of multidirectional instability at the time of revision surgery). Contact athletes had similar outcomes to noncontact athletes in this population. In a large systematic review of 396 shoulders in 6 different studies, Leivadiotou and Ahrens23 reported a 92.5% return to sport and 5.37% recurrence rate after arthroscopic stabilization; 81% of patients reported a single traumatic episode prior to surgical intervention.
Excellent results have also been reported in athletic and throwing populations whose activity demands theoretically predispose them to greater failure rates. Pennington et al33 reported a 93% return to sport in 75 athletes at 2 years postoperatively, with 82% reporting no limitations. Similarly, McClincy et al25 reported no differences in clinical outcomes in a case-matched comparison of throwing versus nonthrowing athletes undergoing posterior shoulder stabilization. Pediatric athletic populations with posterior shoulder instability have also been studied. Wooten et al48 reported 92% satisfaction, 67% return to play with no restrictions, and an 8% failure rate in 25 athletes age 18 years or younger.
Bottoni et al2 retrospectively compared 30 military patients (31 shoulders) who underwent posterior stabilization: 19 via arthroscopic technique and 12 via open technique. Recurrence rates were similar between the 2 groups; however, the authors reported a statistically significant improvement in outcomes scores among the arthroscopic group.2 A recent large meta-analysis also suggested that patients treated arthroscopically have superior outcomes compared with patients who undergo open procedures with respect to stability, recurrence of instability, patient satisfaction, return to sport, and return to previous level of play.11
Management of Instability with Posterior Glenoid Bone Loss or Glenoid Retroversion
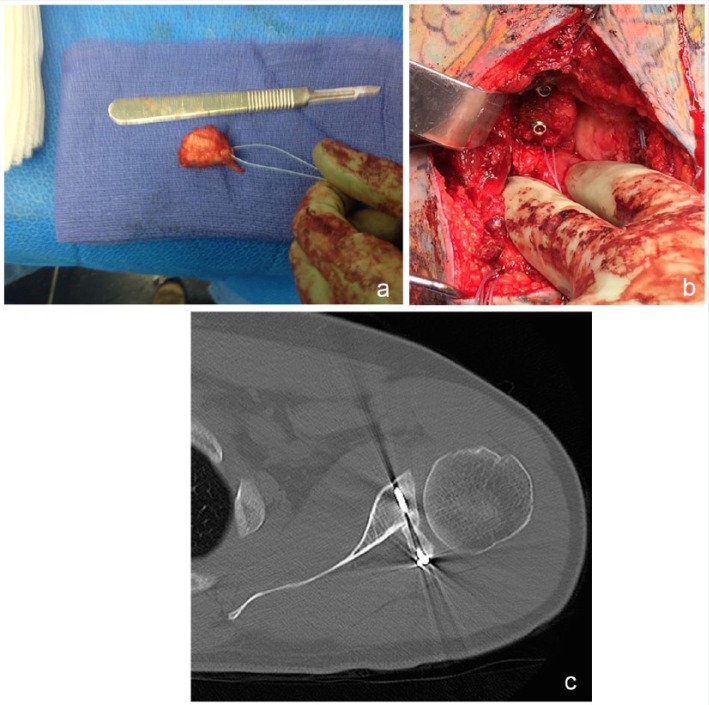
Posterior glenoid bone loss in the setting of posterior shoulder instability presents a rare and challenging situation for the surgeon. Similar to anterior bone loss, multiple techniques, both open and arthroscopic, can be used to treat posterior bone loss. This condition tends to be studied and reported far less than anterior bone loss, however. Numerous novel techniques have been reported to reconstruct the posterior glenoid, including iliac crest bone block, distal tibial allograft, glenoid allograft, pedunculated acromial graft, and distal clavicular autograft (Figure 6).1,15,34,38,40,42,43
Figure 6.
(a) Clinical view of distal clavicular autograft harvested and prepared on back table. (b) Posterior bone block augmentation completed through an open posterior incision. (c) Axial computed tomography image demonstrating osteochondral clavicle graft placement.
While promising clinical results have been reported with posterior bone block reconstruction techniques, the procedure is technically demanding, with complication rates up to 36%, including residual instability and development of osteoarthritis.27,38,39 Careful attention must be paid to positioning of the bone block posteriorly. A biomechanical study showed that a posterior bone block may overconstrain the posterior shoulder and not adequately address inferior instability compared with arthroscopic repair techniques.45
In rare circumstances, patients with increased glenoid retroversion may require correction with a posterior glenoid osteotomy. This is typically considered only in revision settings.17,46 Graichen et al16 reported good or excellent results in 81% of 32 patients undergoing posterior glenoid osteotomy, with the best results in patients with atraumatic instability. However, 25% of patients developed postoperative osteoarthritis, highlighting that this procedure should be only considered in select circumstances.16
Conclusion
Posterior shoulder instability represents about 10% of all shoulder instability, although posterior and combined labral repairs comprise up to 40% of operative repairs. Accurate diagnosis and prompt treatment may be difficult as patients may present with a spectrum of less obvious clinical complaints than anterior instability. Military patients constitute an at-risk population for this injury secondary to military-specific activity requirements, young age, and high activity demands. A detailed history, focused physical examination, and corroborating imaging findings will aid the clinician in obtaining the correct diagnosis. Arthroscopic posterior stabilization has demonstrated excellent clinical outcomes, high patient satisfaction, and low complication rates. Open techniques to address posterior glenoid bone loss or retroversion may be considered in select cases, typically in revision surgery.
Footnotes
The following authors declared potential conflicts of interest: John M. Tokish, MD, is a paid consultant for Arthrex and Depuy-Mitek and Brett D. Owens, MD, is a paid consultant for Mitek and MTF/Conmed.
References
- 1. Barbier O, Ollat D, Marchaland JP, Versier G. Iliac bone-block autograft for posterior shoulder instability. Orthop Traumatol Surg Res. 2009;95:100-107. [DOI] [PubMed] [Google Scholar]
- 2. Bottoni CR, Franks BR, Moore JH, DeBerardino TM, Taylor DC, Arciero RA. Operative stabilization of posterior shoulder instability. Am J Sports Med. 2005;33:996-1002. [DOI] [PubMed] [Google Scholar]
- 3. Bradley JP, Baker CL, 3rd, Kline AJ, Armfield DR, Chhabra A. Arthroscopic capsulolabral reconstruction for posterior instability of the shoulder: a prospective study of 100 shoulders. Am J Sports Med. 2006;34:1061-1071. [DOI] [PubMed] [Google Scholar]
- 4. Bradley JP, McClincy MP, Arner JW, Tejwani SG. Arthroscopic capsulolabral reconstruction for posterior instability of the shoulder: a prospective study of 200 shoulders. Am J Sports Med. 2013;41:2005-2014. [DOI] [PubMed] [Google Scholar]
- 5. Cameron KL, Duffey ML, DeBerardino TM, Stoneman PD, Jones CJ, Owens BD. Association of generalized joint hypermobility with a history of glenohumeral joint instability. J Athl Train. 2010;45:253-258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Campbell SE, Dewitt RM, Cameron KL, Thompson AK, Owens BD. Posterior chondrolabral cleft: clinical significance and associations with shoulder instability. HSS J. 2014;10:208-212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Chalmers PN, Hammond J, Juhan T, Romeo AA. Revision posterior shoulder stabilization. J Shoulder Elbow Surg. 2013;22:1209-1220. [DOI] [PubMed] [Google Scholar]
- 8. Chang ES, Greco NJ, McClincy MP, Bradley JP. Posterior shoulder instability in overhead athletes. Orthop Clin North Am. 2016;47:179-187. [DOI] [PubMed] [Google Scholar]
- 9. Cho JH, Chung NS, Song HK, Lee DH. Recurrent posterior shoulder instability after rifle shooting. Orthopedics. 2012;35:e1677-e1679. [DOI] [PubMed] [Google Scholar]
- 10. DeLong JM, Bradley JP. Posterior shoulder instability in the athletic population: variations in assessment, clinical outcomes, and return to sport. World J Orthop. 2015;6:927-934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. DeLong JM, Jiang K, Bradley JP. Posterior instability of the shoulder: a systematic review and meta-analysis of clinical outcomes. Am J Sports Med. 2015;43:1805-1817. [DOI] [PubMed] [Google Scholar]
- 12. Dickens JF, Kilcoyne KG, Haniuk E, Owens BD. Combined lesions of the glenoid labrum. Phys Sportsmed. 2012;40:102-108. [DOI] [PubMed] [Google Scholar]
- 13. Diklic ID, Ganic ZD, Blagojevic ZD, Nho SJ, Romeo AA. Treatment of locked chronic posterior dislocation of the shoulder by reconstruction of the defect in the humeral head with an allograft. J Bone Joint Surg Br. 2010;92:71-76. [DOI] [PubMed] [Google Scholar]
- 14. Finkelstein JA, Waddell JP, O’Driscoll SW, Vincent G. Acute posterior fracture dislocations of the shoulder treated with the Neer modification of the McLaughlin procedure. J Orthop Trauma. 1995;9:190-193. [PubMed] [Google Scholar]
- 15. Gupta AK, Chalmers PN, Klosterman E, Harris JD, Provencher MT, Romeo AA. Arthroscopic distal tibial allograft augmentation for posterior shoulder instability with glenoid bone loss. Arthrosc Tech. 2013;2:e405-e411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Graichen H, Koydl P, Zichner L. Effectiveness of glenoid osteotomy in atraumatic posterior instability of the shoulder associated with excessive retroversion and flatness of the glenoid. Int Orthop. 1999;23:95-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Graichen H, Koydl P, Zichner L. Value of glenoid osteotomy in treatment of posterior shoulder instability [in German]. Z Orthop Ihre Grenzgeb. 1998;136:238-242. [DOI] [PubMed] [Google Scholar]
- 18. Hawkins RJ, Koppert G, Johnston G. Recurrent posterior instability (subluxation) of the shoulder. J Bone Joint Surg Am. 1984;66:169-174. [PubMed] [Google Scholar]
- 19. Hawkins RJ, Krishnan SG, Karas SG, Noonan TJ, Horan MP. Electrothermal arthroscopic shoulder capsulorrhaphy: a minimum 2-year follow-up. Am J Sports Med. 2007;35:1484-1488. [DOI] [PubMed] [Google Scholar]
- 20. Kang RW, Mahony GT, Harris TC, Dines JS. Posterior instability caused by batter’s shoulder. Clin Sports Med. 2013;32:797-802. [DOI] [PubMed] [Google Scholar]
- 21. Kim SH, Ha KI, Park JH, et al. Arthroscopic posterior labral repair and capsular shift for traumatic unidirectional recurrent posterior subluxation of the shoulder. J Bone Joint Surg Am. 2003;85-A:1479-1487. [DOI] [PubMed] [Google Scholar]
- 22. Kim SH, Park JS, Jeong WK, Shin SK. The Kim test: a novel test for posteroinferior labral lesion of the shoulder—a comparison to the jerk test. Am J Sports Med. 2005;33:1188-1192. [DOI] [PubMed] [Google Scholar]
- 23. Leivadiotou D, Ahrens P. Arthroscopic treatment of posterior shoulder instability: a systematic review. Arthroscopy. 2015;31:555-560. [DOI] [PubMed] [Google Scholar]
- 24. Lenart BA, Sherman SL, Mall NA, Gochanour E, Twigg SL, Nicholson GP. Arthroscopic repair for posterior shoulder instability. Arthroscopy. 2012;28:1337-1343. [DOI] [PubMed] [Google Scholar]
- 25. McClincy MP, Arner JW, Bradley JP. Posterior shoulder instability in throwing athletes: a case-matched comparison of throwers and non-throwers. Arthroscopy. 2015;31:1041-1051. [DOI] [PubMed] [Google Scholar]
- 26. McIntyre LF, Caspari RB, Savoie FH., 3rd The arthroscopic treatment of posterior shoulder instability: two-year results of a multiple suture technique. Arthroscopy. 1997;13:426-432. [DOI] [PubMed] [Google Scholar]
- 27. Meuffels DE, Schuit H, van Biezen FC, Reijman M, Verhaar JA. The posterior bone block procedure in posterior shoulder instability: a long-term follow-up study. J Bone Joint Surg Br. 2010;92:651-655. [DOI] [PubMed] [Google Scholar]
- 28. Miniaci A, McBirnie J. Thermal capsular shrinkage for treatment of multidirectional instability of the shoulder. J Bone Joint Surg Am. 2003;85-A:2283-2287. [DOI] [PubMed] [Google Scholar]
- 29. Owens BD, Campbell SE, Cameron KL. Risk factors for posterior shoulder instability in young athletes. Am J Sports Med. 2013;41:2645-2649. [DOI] [PubMed] [Google Scholar]
- 30. Owens BD, Duffey ML, Deberardino TM, Cameron KL. Physical examination findings in young athletes correlate with history of shoulder instability. Orthopedics. 2011;34:460. [DOI] [PubMed] [Google Scholar]
- 31. Owens BD, Duffey ML, Nelson BJ, DeBerardino TM, Taylor DC, Mountcastle SB. The incidence and characteristics of shoulder instability at the United States Military Academy. Am J Sports Med. 2007;35:1168-1173. [DOI] [PubMed] [Google Scholar]
- 32. Owens BD, Tucker CJ, Zacchilli M. Surgical management of posterior shoulder instability. Curr Orthop Pract. 2011;22:474-482. [Google Scholar]
- 33. Pennington WT, Sytsma MA, Gibbons DJ, et al. Arthroscopic posterior labral repair in athletes: outcome analysis at 2-year follow-up. Arthroscopy. 2010;26:1162-1171. [DOI] [PubMed] [Google Scholar]
- 34. Petrera M, Veillette CJ, Taylor DW, Park SS, Theodoropoulos JS. Use of fresh osteochondral glenoid allograft to treat posteroinferior bone loss in chronic posterior shoulder instability. Am J Orthop (Belle Mead NJ). 2013;42:78-82. [PubMed] [Google Scholar]
- 35. Provencher MT, Bell SJ, Menzel KA, Mologne TS. Arthroscopic treatment of posterior shoulder instability: results in 33 patients. Am J Sports Med. 2005;33:1463-1471. [DOI] [PubMed] [Google Scholar]
- 36. Provencher MT, LeClere LE, King S, et al. Posterior instability of the shoulder: diagnosis and management. Am J Sports Med. 2011;39:874-886. [DOI] [PubMed] [Google Scholar]
- 37. Ryu RK, Dunbar WH, 5th, Kuhn JE, McFarland EG, Chronopoulos E, Kim TK. Comprehensive evaluation and treatment of the shoulder in the throwing athlete. Arthroscopy. 2002;18(suppl 2):70-89. [DOI] [PubMed] [Google Scholar]
- 38. Schwartz DG, Goebel S, Piper K, Kordasiewicz B, Boyle S, Lafosse L. Arthroscopic posterior bone block augmentation in posterior shoulder instability. J Shoulder Elbow Surg. 2013;22:1092-1101. [DOI] [PubMed] [Google Scholar]
- 39. Servien E, Walch G, Cortes ZE, Edwards TB, O’Connor DP. Posterior bone block procedure for posterior shoulder instability. Knee Surg Sports Traumatol Arthrosc. 2007;15:1130-1136. [DOI] [PubMed] [Google Scholar]
- 40. Sirveaux F, Leroux J, Roche O, Gosselin O, De Gasperi M, Molé D. Surgical treatment of posterior instability of the shoulder joint using an iliac bone block or an acromial pediculated bone block: outcome in eighteen patients [in French]. Rev Chir Orthop Reparatrice Appar Mot. 2004;90:411-419. [DOI] [PubMed] [Google Scholar]
- 41. Song DJ, Cook JB, Krul KP, et al. High frequency of posterior and combined shoulder instability in young active patients. J Shoulder Elbow Surg. 2015;24:186-190. [DOI] [PubMed] [Google Scholar]
- 42. Struck M, Wellmann M, Becher C, Pastor MF, Smith T. Results of an open posterior bone block procedure for recurrent posterior shoulder instability after a short- and long-time follow-up. Knee Surg Sports Traumatol Arthrosc. 2016;24:618-624. [DOI] [PubMed] [Google Scholar]
- 43. Tokish JM, Fitzpatrick K, Cook JB, Mallon WJ. Arthroscopic distal clavicular autograft for treating shoulder instability with glenoid bone loss. Arthrosc Tech. 2014;3:e475-e481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Wanich T, Dines J, Dines D, Gambardella RA, Yocum LA. ‘Batter’s shoulder’: can athletes return to play at the same level after operative treatment? Clin Orthop Relat Res. 2012;470:1565-1570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Wellmann M, Bobrowitsch E, Khan N, et al. Biomechanical effectiveness of an arthroscopic posterior Bankart repair versus an open bone block procedure for posterior shoulder instability. Am J Sports Med. 2011;39:796-803. [DOI] [PubMed] [Google Scholar]
- 46. Wirth MA, Seltzer DG, Rockwood CA., Jr. Recurrent posterior glenohumeral dislocation associated with increased retroversion of the glenoid. A case report. Clin Orthop Relat Res. 1994;(308):98-101. [PubMed] [Google Scholar]
- 47. Wooten C, Klika B, Schleck CD, Harmsen WS, Sperling JW, Cofield RH. Anatomic shoulder arthroplasty as treatment for locked posterior dislocation of the shoulder. J Bone Joint Surg Am. 2014;96:e19. [DOI] [PubMed] [Google Scholar]
- 48. Wooten CJ, Krych AJ, Schleck CD, Hudgens JL, May JH, Dahm DL. Arthroscopic capsulolabral reconstruction for posterior shoulder instability in patients 18 years old or younger. J Pediatr Orthop. 2015;35:462-466. [DOI] [PubMed] [Google Scholar]