Abstract
Objective:
Effects of time in moderate to vigorous physical activity (MVPA) and sitting (SIT) on bone were tested, hypothesizing that high MVPA would be positively associated with bone size and strength, offset effects of high SIT, and be mediated by lean mass.
Methods:
155 children (79 male, 58 pubertal), 6-20 years (10.2±3.5 yr) were measured by dual-energy x-ray absorptiometry (DXA) and peripheral quantitative computed tomography (pQCT). MVPA and SIT were measured by 7-day activity recall. Regression analyses tested effects of MVPA and SIT on bone. Mediation analysis was conducted to determine if lean mass mediated the effect of activity on bone.
Results:
In pubertal boys, SIT was negatively associated with tibial endosteal and periosteal circumference as well as bone strength (β= -0.19, -0.14, and -5.68, respectively; all p<0.05). Effects of SIT on bone circumferences and strength were mediated by lean mass. MVPA did not offset the effects of SIT. In pubertal girls, MVPA was positively associated with cortical thickness (β=0.01, p<0.05) and the association was not mediated by lean mass.
Conclusions:
Current health communications that encourage increased physical activity should include additional messaging to decrease time spent sitting, especially in pubertal boys.
Keywords: Sitting Time, MVPA, Bone, Lean Mass, Children
Introduction
Evidence from clinical trials suggests that high-impact weight bearing physical activity in children and adolescents increases osteogenic effects on bone[1]. Studies investigating the associations between moderate to vigorous physical activity (MVPA) and/or sedentary time on bone health in children are emerging. MVPA has been positively associated with increases in bone while sedentary time has shown negative effects[2-4]. Chastin et al.[5] reported physical activity measured by accelerometers and sport activity measured by questionnaire offset the detrimental effects on bone associated with increased television time in boys and increased time spent studying in girls.; In their analyses they adjusted for body mass index, but measures of lean mass were not considered. Gracia-Marco et al.[6] showed that increased internet time in boys was associated with low whole body bone mineral content (BMC) and this result remained significant when MVPA and lean mass were added to the model. In the same study, girls with increased study time had lower femoral neck BMC. Inclusion of lean mass in the analysis lessened the effect of study time on femoral neck BMC but adding MVPA did not change it further. A recent study using HR-pQCT[7] found no relationship between sedentary behavior in children 9-20 years of age and bone architecture, strength and volumetric bone mineral density (vBMD). This study did not include lean mass, but included muscle cross-sectional area in the regression analysis. A recent study focusing on the interrelations among BMC, height, and lean mass found lean mass to be a total mediator of the association between muscular fitness and bone health in children 8-11 years[8]. These previous studies indicate that measures of lean mass may be important in understanding the relationship between activity and bone.
Our aim was to add evidence to the existing understanding of the associations between the percent of time spent in MVPA and sitting (SIT) on both dual-energy x-ray absorptiometry (DXA) and peripheral quantitative computed tomography (pQCT) bone outcomes in children. To stress the importance of lean mass as a predictor of bone and to clarify the causal process of activity on bone due to lean mass, a mediation analysis was conducted. We hypothesized that high MVPA would be associated with larger bone size and higher bone strength and offset the detrimental bone effects of high SIT. We also hypothesized that the effects of MVPA and SIT on bone in children would be mediated by lean mass.
Materials and methods
This cross-sectional study included a convenience sample of 155 (79 male) healthy children 6-20 years of age (mean±SD 10.2±3.5 yrs) recruited from a rural community and surrounding area, a local rural elementary school, and via parents participating in other current studies at our institution. The study protocol was approved by the University Institutional Review Board and signed informed consent was obtained from all participants 18 years of age or older. Written informed consent signed by a parent and assent signed by the child were obtained from all participants under 18 years of age.
Parents of elementary and middle school students assisted study staff in the completion of questionnaires used to collect demographic data, brief medical history, Tanner Stage, and activity patterns via in-person interview or by phone. High school students completed these questions without assistance from a parent. Parents of children under the age of 8 years were asked if their child showed any signs of pubertal changes. If parents thought their child was showing signs of pubertal change, then the parent was shown sketched line drawings of breast development for girls and pubic hair for boys[9] and the Tanner Stage was noted. If parents had not noted any signs of pubertal change, then the child was coded as Tanner Stage 1. Tanner Stage was self-assessed in children 8 years of age and older, assisted by study staff, using sketched line drawings of breast development for girls and pubic hair for boys[9]. Children were categorized as pre-pubertal if they were Tanner Stage 1 and pubertal if they were Tanner Stages 2-5. Activity was assessed using a modified Seven-Day Activity Recall (PAR)[10] that estimates the time spent sleeping, sitting, or in moderate to vigorous activities on weekdays and weekend days separately. The remaining time each day was assumed to be light activity. Average daily percent time spent in sitting (SIT) or moderate plus vigorous activity (MVPA) was calculated based on the estimates.
Total body lean mass (less bone, LM) and fat mass were assessed from whole body images obtained using DXA (Hologic, Inc.). Lumbar spine (spine), femoral neck (FN), and total hip bone area (BA) and BMC also were obtained using DXA. Images were analyzed for body composition, BA and BMC using Discovery Pediatric Software version 12.3 provided by the manufacturer. Coefficients of variation (CVs) at our institution based on triplicate scans from 15 children (mean age 12.1 years) ranged from 1.2 % for spine BMC to 5.0% for total body fat mass.
Bone strength measured as polar strength strain index (pSSI), cortical thickness (CrtThk), and periosteal and endosteal circumference (PeriC, EndoC) of the tibia were obtained using XCT2000 (Orthometrix Inc.). The right or left leg of the foot used to kick a ball was imaged. Tibia length was measured from the medial condyle to the medial malleolus of the tibia using a segmometer (Rosscraft). A scout view was obtained and a reference line placed at the distal end plate of the tibia or at the most distal portion of the growth plate when indicated. A slice image was obtained at 20% of the tibia length from the reference line using a speed of 30 mm/sec and voxel size of 0.40 mm and analyzed using manufacturer’s software version 6.00B. Analysis settings were: Contour mode 2, Peel mode 2 with a threshold of 400 mg/cm3 and Cort mode 1 and threshold of 710 mg/cm3 for cortical bone with a threshold of 280 mg/cm3 for pSSI. Our institution’s CVs at the 20% distal tibia site are 2.7% for cortical thickness, 0.5% for periosteal circumference, 1.4% for endosteal circumference and 4.9% for pSSI based on duplicate scans from 9 children (mean age=8 years).
Statistical analysis was completed using JMP software (version10, SAS Institute). Bone outcomes included spine, hip, and FN BA and BMC by DXA and CrtThk, PeriC, EndoC, and pSSI at the 20% distal tibia site by pQCT. Simple linear regression was used to obtain correlation coefficients for associations between activity (SIT and MVPA) and outcomes (bone measures and lean mass) in girls and boys separately by pubertal status. Regression models stratified by the two pubertal groups were used to test if associations of SIT and MVPA on bone outcomes remained significant when controlling for age, sex, weight and height for pQCT and DXA BA outcomes and adjusting for age, sex, weight, and bone area for DXA BMC outcomes. Regression models that showed activity as a significant predictor of bone were investigated to test if lean mass was the mediating factor of activity on bone by replacing weight with fat mass and then in a later step adding lean mass to the model. We used the conditions a variable must meet to be considered a mediator specified by Baron and Kenny[11]. Explicitly, we determined whether activity measures correlate with bone outcomes (step 1), whether activity measures correlate with lean mass (step 2), and whether lean mass correlated with bone outcomes (step 3; Figure 1). For mediation analysis, we obtained beta coefficients for activity measures from a base model controlling for age, sex, and fat mass for pre-pubertal and pubertal groups separately. Lean mass was then added to the base model to test for mediation effects. Marginal means for bone outcomes from the base model and the base model plus lean mass were noted for boys and girls. A p-value <0.05 indicated significant association. In addition, if the beta coefficient for activity changed by greater than 10% when lean mass was added to the regression equation, then model confounding[12] or in this context, mediation[13] was indicated.
Figure 1.
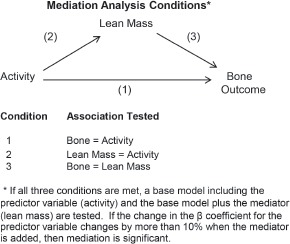
Summary of steps involved in mediation analysis.
Results
Participants included 155 children 6-20 years of age (58 pubertal, 79 boys). Covariates and outcome variables are given by pubertal status and sex in [Table 1]. In pre-pubertal children, boys were older, taller, weighed more, and had higher lean and lower percent body fat than girls. The bones of pre-pubertal boys were larger, had higher BMC, and were thicker which lead to higher bone strength than that of the girls. In pubertal children, boys had higher lean mass and lower percent body fat than girls. Endo C and Peri C were smaller in girls, but there was no difference in cortical bone thickness between pubertal girls and boys. Bone strength, and FN and Hip BA were higher in boys. SIT and MVPA were not different by sex in either pubertal group. MVPA was the only measure that was not different between pre-pubertal and pubertal children.
Table 1.
Covariate and outcome variables by sex and pubertal status.
| Pre-pubertal | Pubertal | |||
|---|---|---|---|---|
| Girls | Boys | Girls | Boys | |
| N | 41 | 56 | 35 | 23 |
| Mean Age (yr) | 7.9 ± 1.3 | 8.7 ± 1.5b | 13.1 ± 3.9 | 13.7 ± 3.4 |
| Weight (kg) | 28.0 ± 8.9 | 31.7 ± 7.7a | 50.6 ± 13.3 | 56.2 ± 20.5 |
| Height (cm) | 126 ± 9 | 134 ± 10b | 153 ± 15 | 158 ± 13 |
| Fat Mass (kg) | 7.5 ± 5.0 | 6.8 ± 3.7 | 14.1 ± 5.1 | 12.5 ± 9.7 |
| Body Fat (%) | 25 ± 7 | 21 ± 6b | 28 ± 7 | 21 ± 9b |
| Lean Mass (kg) | 20.0 ± 4.3 | 23.9 ± 4.7b | 35.3 ± 10.1 | 41.8 ± 13.5a |
| Endo C (mm) | 41 ± 6 | 42 ± 5 | 48 ± 6 | 52 ± 6b |
| Peri C (mm) | 54 ± 6 | 57 ± 5 | 65 ± 6 | 71 ± 7b |
| Crt Thk (mm) | 2.1 ± 0.3 | 2.4 ± 0.3b | 2.8 ± 0.5 | 2.9 ± 0.6 |
| pSSI (mm3) | 540 ± 157 | 636 ± 179b | 1056 ± 339 | 1288 ± 421a |
| Spine BA (cm2) | 35.4 ± 4.0 | 39.4 ± 5.1b | 49.0 ± 10.8 | 53.4 ± 10.0 |
| Spine BMC (g) | 20.8 ± 3.8 | 23.7 ± 4.8b | 43.5 ± 17.7 | 44.1 ± 17.8 |
| FN BA (cm2) | 3.6 ± 0.9 | 4.0 ± 0.6b | 4.5 ± 0.6 | 4.9 ± 0.6a |
| FN BMC (g) | 2.2 ± 0.7 | 2.8 ± 0.6b | 3.7 ± 1.0 | 4.1 ± 1.0 |
| Hip BA (cm2) | 18.7 ± 3.4 | 20.9 ± 4.0b | 28.3 ± 5.8 | 32.5 ± 6.7a |
| Hip BMC (g) | 12.3 ± 3.3 | 15.2 ± 4.0b | 25.5 ± 9.0 | 29.3 ± 10.5 |
| SIT (%) | 30.8 ± 5.4 | 30.6 ± 6.0 | 27.6 ± 9.4 | 24.5 ± 10.6 |
| MVPA (%) | 18.0 ± 7.0 | 18.3 ± 7.0 | 19.4 ± 10.5 | 21.1 ± 10.1 |
p<0.05
p<0.01 between girls and boys within pubertal status.
Results are Mean ± SD. Endo C – endosteal circumference; Peri C – periosteal circumference; Crt Thk – cortical thickness; pSSI – polar strength strain index; BA – bone area; BMC – bone mineral content; FN – femoral neck; SIT - % time spent sitting; MVPA – % time spent in moderate plus vigorous activity.
There was an association between activity and adjusted lean mass but only in pubertal children (Figure 2). SIT showed a negative association and MVPA a positive association when lean mass was adjusted for age, sex, height, and fat mass. These relationships were explored further in the mediation analysis. Correlation coefficients are given by pubertal status and sex for each variable according to the steps considered for mediation (Table 2). Considering the criteria for Step 1, there were no associations in pre-pubertal boys, but in pre-pubertal girls, SIT was positively associated with Peri C, pSSI, and spine and hip BMC. In pubertal boys, SIT was negatively associated with Endo C; Peri C; pSSI; spine, femoral neck, and total hip BA; and spine and hip BMC. In pubertal girls, MVPA was positively associated with Crt Thk; pSSI; spine and total hip BA; and spine, femoral neck, and total hip BMC. Considering the criteria for Step 2, SIT was positively associated with lean mass in pre-pubertal girls and showed a negative association in pubertal boys. MVPA was positively associated with lean mass in pubertal girls. Continuing to the criteria for Step 3, lean mass was positively correlated with bone outcomes indicated as significant in Step 1.
Figure 2.

Associations between activity and lean mass adjusted for age, sex, height, and fat mass. (a) Association between percent time spent sitting (SIT) and adjusted lean mass. Pre-pubertal = O solid line (p=NS). Pubertal=X dashed line (p<0.01). (b) Association between percent time spent in moderate plus vigorous activity (MVPA) and adjusted lean mass. Pre-pubertal=O solid line (p=NS). Pubertal=X dashed line (p<0.01).
Table 2.
Correlation coefficients for sit and mvpa for girls and boys by pubertal status.
| SIT | MVPA | Lean Mass | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-pubertal | Pubertal | Pre-pubertal | Pubertal | Pre-pubertal | Pubertal | |||||||
| Girls | Boys | Girls | Boys | Girls | Boys | Girls | Boys | Girls | Boys | Girls | Boys | |
| Step 1. Does activity correlate with bone outcomes? | Step 3. Does lean mass correlate with bone? | |||||||||||
| pQCT Outcome | ||||||||||||
| Endo C (mm) | 0.27 | -0.07 | - 0.27 | -0.44 | -0.12 | 0.05 | -0.01 | -0.17 | _ _a | _ _ a | _ _a | 0.52 |
| Peri C (mm) | 0.35 | -0.06 | - 0.29 | -0.54 | -0.20 | 0.19 | 0.27 | 0.01 | 0.89 | _ _ a | _ _a | 0.86 |
| Crt Thk (mm) | 0.27 | 0.02 | - 0.10 | -0.29 | -0.25 | -0.09 | 0.54 | 0.30 | _ _a | _ _ a | 0.82 | _ _a |
| pSSI (mm3) | 0.39 | -0.03 | -0.31 | -0.52 | -0.21 | -0.19 | 0.42 | 0.11 | 0.93 | _ _ a | 0.89 | 0.95 |
| DXA Outcome | ||||||||||||
| Spine BA (cm2) | 0.15 | -0.10 | -0.26 | -0.48 | -0.12 | -0.10 | 0.47 | 0.23 | _ _a | _ _ a | 0.94 | 0.93 |
| Spine BMC (g) | 0.35 | -0.01 | -0.26 | -0.48 | -0.17 | -0.07 | 0.49 | 0.14 | 0.77 | _ _ a | 0.93 | 0.91 |
| FN BA (cm2) | 0.15 | -0.16 | -0.28 | -0.45 | -0.3 | 0.00 | 0.25 | 0.18 | _ _a | _ _ a | _ _a | 0.82 |
| FN BMC (g) | 0.30 | -0.14 | -0.25 | -0.40 | -0.14 | 0.05 | 0.47 | 0.19 | _ _a | _ _ a | 0.93 | _ _a |
| Hip BA (cm2) | 0.30 | -0.13 | -0.29 | -0.60 | -0.8 | -0.11 | 0.45 | 0.19 | _ _a | _ _ a | 0.92 | 0.91 |
| Hip BMC (g) | 0.38 | -0.15 | -0.32 | -0.53 | -0.15 | -0.05 | 0.55 | 0.18 | 0.87 | _ _ a | 0.96 | 0.94 |
| Step 2. Does activity correlate with lean mass? | ||||||||||||
| Lean Mass (kg) | 0.40 | _ _a | _ _a | -0.43 | _ _a | _ _a | 0.49 | _ _a | ||||
Not tested – no significance with previous criteria
Bolded results are significant at p<0.05
SIT - % time spent sitting; MVPA - % time spent in moderate plus vigorous activity; Endo C – endosteal circumference; Peri C – periosteal circumference; Crt Thk – cortical thickness; pSSI – polar strength strain index; BA – bone area; BMC – bone mineral content; FN – femoral neck.
Mediation analysis was conducted in cases that met all 3 criteria stated previously. The base model used for mediation controlled for age, sex, and fat mass. Effects of SIT on bone in pre-pubertal girls and on DXA bone measures in pubertal boys did not remain significant in the base model and further mediation analysis was not completed for these groups (data not shown). Likewise, effects of MVPA on DXA bone measures in pubertal girls did not remain significant in the base model and mediation analysis was not conducted for DXA bone measures. Results of mediation analysis for pubertal girls and boys on pQCT bone outcomes are shown in [Table 3]. The effect of SIT on bone became insignificant when lean mass was included in the model, with the beta coefficient for SIT changing by 25-45%, which indicates lean mass mediates the effect of SIT on EndoC, PeriC, and pSSI. However, lean mass did not mediate the effect of MVPA on Crt Thk. Due to the higher amount of lean mass in boys and lower amount in girls, marginal means were decreased for boys and increased for girls when lean mass was added to the base models (Table 3). Additional analysis was completed to test whether or not MVPA offset the negative effects of SIT on bone. MVPA was not significant when added to the base model and did not offset the negative association between SIT and Endo C, Peri C, or pSSI in pubertal boys (data not shown).
Table 3.
Mediating effect of lean mass on beta coefficients for activity and marginal means for bone outcomes in pubertal girls and boys.
| β Coefficient [95% CI] | Marginal Means | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Base Model1 | Base+ Lean Mass | Change (%) | Base Model | Base + Lean Mass | Change (%) | ||||
| Girls | Boys | Girls | Boys | Girls | Boys | ||||
| SIT | |||||||||
| Endo C | -0.20 [-0.37, -0.03] | -0.15 [-0.31, 0.01] | 25 | 48.2 ±0.9 | 52.0 ±1.1 | 49.4 ± 0.9 | 50.2 ± 1.2 | +2.5 | -3.5 |
| Peri C | -0.17 [-0.32, -0.02] | -0.10 [-0.22, 0.02] | 41 | 65.5 ± 0.8 | 70.3 ± 1.0 | 67.0 ± 0.7 | 68.0 ±0.9 | +2.3 | -3.3 |
| pSSI | -7.1 [-13.4. -0.8] | -3.9 [-8.6, 0.8] | 45 | 1067 ± 34 | 1273 ± 42 | 1139 ± 27 | 1162 ± 35 | +6.7 | -8.7 |
| MVPA | |||||||||
| Crt Thk | 0.01 [0.00, 0.01] | 0.01 [0.00, 0.02] | 0 | 2.8 ±0.1 | 2.8 ± 0.1 | 2.8 ± 0.1 | 2.8 ± 0.1 | 0 | 0 |
Base Model was adjusted for age, sex, and fat mass. Bolded results are significant at p<0.05.
Discussion
In general, our results do not support the hypothesis of an association between MVPA and larger, stronger bones or that MVPA offsets the detrimental bone effects of high SIT. Our results, however, do support the hypothesis that lean mass mediates the adverse effect of SIT on bone.
Previous studies have observed the influence of different levels of physical activity on lean mass and bone but results are not consistent. Two studies had results that are in contrast to our findings. Kennedy et al. observed MVPA to be positively associated with lean mass index (lean mass/height[2]), hip BMC, and spine bone area in low birth weight children at 6.7 years of age[3]. Vaitkevicuite et al. found increased MVPA to be associated with increased femoral neck aBMD in pubertal boys and this association remained significant when lean mass was added to the model[4]. Our population was not representative of children with low birth weight and we did not find associations between activity and femoral neck BMC adjusted for BA in pre-pubertal or pubertal children. It is possible that the broad range of Tanner stages we used to define pubertal children could explain our differing results.
In our study, MVPA did not offset the detrimental effects of high SIT. Similar to our findings, MVPA did not offset the detrimental effects of greater internet use on whole body BMC in boys reported by Gracia-Marco[6] or greater TV and screen time on hip BMC in boys observed by Chastin[5]. However, Chastin found that when sport and vigorous activity, but not MVPA, were considered, the unfavorable effects of higher TV and screen time on hip BMC were eliminated. Another study in adolescents showed participation in extracurricular activities offset lower whole body BMC associated with ≥3 hours of TV/day[14]. Unfortunately, vigorous physical activity estimated via recall is limited[15] and we did not collect information on sports participation. It is possible measures of extracurricular and sport activity may have offset the negative associations between SIT and bone we observed in this population.
A unique finding in our study was the association between higher SIT and lower endosteal and periosteal circumference along with lower bone strength as measured by pQCT at the tibia of pubertal boys. A recent study by Gabel et al. found no associations between sedentary behavior and HR-pQCT bone outcomes[7] while controlling for cross-sectional muscle area. In our study, lean mass was found to mediate the associations between SIT and tibia bone measures similar to the findings by Torres-Costoso et al.[8] who reported that lean mass mediated the influence of muscle fitness on bone in children. The mediation analysis results by Torres-Costoso, along with our findings, emphasize the importance of lean mass on bone size and strength. The negative relationship between sitting time and lean mass in pubertal boys leads to a practical application; encouraging less sitting time may be an effective method to increase lean mass thereby leading to improved bone health in children, especially in pubertal boys.
There are limitations to this study. The validity of the study is limited by the cross-sectional design and convenience sample. The mediation analysis, taken from data at one time point, cannot deduce if higher amounts of sitting affect lean mass, or if individuals with lower amounts of lean mass sit more. The lack of association between MVPA and bone or lean mass was not expected. Activity was not objectively collected with accelerometers but instead via a subjective seven-day activity recall. It is possible that time spent sitting is easier for parents and participants to recall and more consistent throughout the year than time spent in moderate or vigorous activity. This may explain why we found associations with SIT but not with MVPA. Even with these limitations, our findings add evidence to the current understanding of relationships between activity and bone measures in children. In particular, the inclusion of pQCT bone measures, the focus on sitting time, and the additional analysis of lean mass as a mediator adds to the existing knowledge base.
Pubertal boys who spent more time sitting had smaller endosteal and periosteal circumferences and lower bone strength in the tibia. These effects were not offset by MVPA but were mediated by lean mass. It may prove beneficial for future studies to collect activity data objectively via accelerometer to distinguish between moderate and vigorous activity levels, and via questionnaire to test effects of estimated sedentary behavior or sport participation. Measures of lean mass are essential in understanding causal relationships between activity and bone. Methods that decrease sedentary behaviors are as vital as previous approaches attempting to increase lean mass and bone via increased moderate to vigorous physical activity. Therefore, in addition to the current public health messaging aimed at increasing moderate plus vigorous activity, encouraging less sitting time may be effective to improve pediatric bone health.
Footnotes
Edited by: F. Rauch
References
- 1.Hind K, Burrows M. Weight-bearing exercise and bone mineral accrual in children and adolescents: A review of controlled trials. Bone. 2007;40:14–27. doi: 10.1016/j.bone.2006.07.006. [DOI] [PubMed] [Google Scholar]
- 2.Ivuskans A, Maeestu J, Juerimaee T, et al. Sedentary time has a negative influence on bone mineral parameters in peripubertal boys: a 1-year prospective study. J Bone Miner Metab. 2015;33:85–92. doi: 10.1007/s00774-013-0556-4. [DOI] [PubMed] [Google Scholar]
- 3.Kennedy K, Shepherd S, Williams JE, Ahmed SF, Wells JC, Fewtrell M. Activity, body composition and bone health in children. Arch Dis Child. 2013;98:204–7. doi: 10.1136/archdischild-2012-302823. [DOI] [PubMed] [Google Scholar]
- 4.Vaitkeviciute D, Laett E, Maeestu J, et al. Physical Activity and Bone Mineral Accrual in Boys with Different Body Mass Parameters during Puberty: A Longitudinal Study. PLOS One. 2014:9. doi: 10.1371/journal.pone.0107759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chastin SFM, Mandrichenko O, Skelton DA. The frequency of osteogenic activities and the pattern of intermittence between periods of physical activity and sedentary behaviour affects bone mineral content: the cross-sectional NHANES study. Bmc Public Health. 2014:14. doi: 10.1186/1471-2458-14-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gracia-Marco L, Rey-Lopez JP, Santaliestra-Pasias AM, et al. Sedentary behaviours and its association with bone mass in adolescents: the HELENA cross-sectional study. BMC Public Health. 2012:12. doi: 10.1186/1471-2458-12-971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gabel L, McKay HA, Nettlefold L, Race D, Macdonald HM. Bone architecture and strength in the growing skeleton: the role of sedentary time. Med Sci Sports Exer. 2015;47:363–72. doi: 10.1249/MSS.0000000000000418. [DOI] [PubMed] [Google Scholar]
- 8.Torres-Costoso A, Gracia-Marco L, Sanchez-Lopez M, et al. Lean mass as a total mediator of the influence of muscular fitness on bone health in schoolchildren: a mediation analysis. J Sport Sci. 2015;33:817–30. doi: 10.1080/02640414.2014.964750. [DOI] [PubMed] [Google Scholar]
- 9.Morris N, Udry J. Validation of a self-administered instrument to assess stage of adolescent development. J Youth Adolesc. 1980;9:271–81. doi: 10.1007/BF02088471. [DOI] [PubMed] [Google Scholar]
- 10.Paffenbarger JRS, Blair SN, Lee IM, Hyde RT. Measurement of physical activity to assess health effects in free-living populations. Med Sci Sports Exerc. 1993;25:60–70. doi: 10.1249/00005768-199301000-00010. [DOI] [PubMed] [Google Scholar]
- 11.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–82. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 12.Greenland S. Modeling and variable selectionin epidemiological analysis. Am J Public Health. 1989;79:340–9. doi: 10.2105/ajph.79.3.340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.MacKinnon DP, Krull JL, Lockwood CM. Equivalence of the mediation, confounding and suppression effect. Prev Sci. 2000;1:173–81. doi: 10.1023/a:1026595011371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vicente-Rodríguez G, Ortega FB, Rey-López JP, et al. Extracurricular physical activity participation modifies the association between high TV watching and low bone mass. Bone. 2009;45:925–30. doi: 10.1016/j.bone.2009.07.084. [DOI] [PubMed] [Google Scholar]
- 15.Manios Y, Androutsos O, Moschonis G, et al. Criterion validity of the Physical Activity Questionnaire for Schoolchildren (PAQ-S) in assessing physical activity levels: the Healthy Growth Study. J Sport Med Phys Fit. 2013;53:502–8. [PubMed] [Google Scholar]


