Abstract
Resume In accordance with modern concepts, one of the leading roles in the development of paroxysmal atrial fibrillation and flutter, belongs - the restructuring of the myocardium, in second place - sick sinus syndrome and in third place - the presence of accessory pathways and hormonal disorders. The development of atrial fibrillation and flutter in the structural pathology, primarily begins with of drugs if it does not work, we have to carry out ablation. Providing proper, effective and important combination therapy - is the main challenge in cardiology.
Keywords: Atrial Fibrillation, tructural Heart Disease, S Electrical Instability Of The Heart
Introduction
Fibrillation and atrial flutter (AF) - one of the most common heart rhythm disturbance. In the population of their frequency is 1-2%. According to data presented in the recommendations of the European Society of Cardiology, about 6 million people in Europe suffer from AF, and in the next 50 years, their number at least double. AF can significantly reduce the quality of life of patients.[7] All this makes it necessary to find effective methods of treatment and prevention of cardiac electrical instability (CEI).
Antiarrhythmic drugs have limited efficacy in the treatment and prevention of AF and do not modify the structural substrate in AF. Currently, few controlled clinical studies on the choice of anti-arrhythmic drug, taking into account a variety of mechanisms and causes of AF. Therefore, modern algorithms for medical treatment of AF should include the combined use of anti-arrhythmic and anti-arrhythmic drugs, in order to address the complex causal interaction, forming a vicious circle and put increased difficulties in treating this rhythm disturbance over time.[2]
Promising reasons and mechanisms of AF can assume the existence of an antioxidant barrier, which can be damaged by structural heart disease. Under normal conditions, there is a distinction between the myocardium and the ectopic nodes located along the pathways of the heart. In the myocardium, intercellular fluid contains large amounts of Na+ ions and Cl-, especially during hypoxia and acidosis, i.e. there prevails acidic environment, and in ectopic sites and conductive paths heart predominant acidic environment. In order to prevent any oxidation of the proximal and middle conductive paths ectopic sites, there is the antioxidant barrier in the form of connective tissue adhesive coating. A distal Purkinje fibers, antioxidant barrier moves into T-cells, which differentiate B cells (Purkinje cells), and the myocardium itself. It is this antioxidant barrier, often damaged by structural heart disease, which leads to the development of atrial or ventricular fibrillation.[4]
Accordingly, if hypothetically assume that there is a damage of the antioxidant barrier, and treatment should be combined to work on all parts of AF: antiarimicheskoe, antioxidant and reparantnoe. Research in this area has not yet been carried out in the world, the very reason for the oxidation of ectopic sites at various anatomical levels of the heart, is an innovative, so references to the use of the described combination treatment of atrial fibrillation and flutter of the heart in the literature. Nevertheless, we refer to the use of some authors in the studies undertaken.
In this study, TA Zaynutdinova (2008.), It is noted that the beats I-III functional class Qudesan at course at a dose of 2 mg / kg / day in the complex therapy is the overall antiarrhythmic effect in 50% of children, causing half of them complete suppression of arrhythmias and improving the results of the basic treatment of 10%.[1]
In a study conducted Shubik Y. (1998.), Argues that solkoseril proved to be quite effective antiarrhythmic agent in the treatment of ventricular arrhythmias high grading B. Lown. effect which is realized by means of membrane and antihypoxic effect on cells including - myocardial cells.[5]
The aim of our study was to evaluate the efficacy and safety of antiarrhythmic action Qudesan and solcoseryl in patients with atrial flutter and atrial fibrillation.
Materials And Methods
The study met the requirements Helsenskoy diklaratsii. All patients provided written consent to participate in a clinical trial. The study protocol was approved by the Ethical Committee of the SEI HPE “Dagestan State Medical Academy” MoH.
Randomezirovannoe open prospective comparative study included 53 patients with new-onset paroxysmal AF or TA. Patients were treated in the cardiology department of the Republican Hospital №2 TSSEMP MOH RD (Makhachkala) in the period 2012-2013. Inpatient treatment lasted 7 days after discharge outpatient supervision and treatment continued - the total duration of the study was one month.
Criteria For Inclusion
hemodynamically stable episodes of AF with no more than 7 days;
informed consent to participate in the study;
age from 18 to 75 years.
Exclusion Criteria Were
Unstable Angina
a permanent form of atrial flutter or atrial fibrillation;
artificial pacemaker;
the inability of prospective study;
participation in any other study.
Criteria For Early Retirement From The Study
the emergence of side effects of drugs;
failure to continue to research and treatment;
non-compliance to medication.
On admission, patients were randomized by random numbers into two groups matched for sex and age, the level of blood pressure, body mass index. The ratio of male to female ratio was 44 (83.0%) and 9 (17.0%), respectively [Table 1].
Table 1. Baseline demographic and clinical and laboratory characteristic groups .
| ndicators | group 1 (n = 28) | group 2 (n = 25) |
| Men, n % | 67,9 | 74,4 |
| Average age | 57,8±7,3 | 56,5±7,0 |
| BMI: + 25–30 кг/м2, n (%) > 30 кг/м2, n (%) | 20 32 | 23 29 |
| Physical inactivity, n (%) | 47 | 51 |
| Smoking, n (%) | 32 | 26 |
| Leukocytes thousand. 1 ml. | 4,8±2,5 | 9,2±3,2 |
For all these measures groups were not significantly different from each other (p> 0.05).
Patients in both groups had a variety of related heart disease: coronary heart disease, hypertension, cardiomyopathy, myocarditis, atherosclerosis, etc. [Table 2].
Table 2. Characteristics of the groups on the main and additional diseases.
| Indicators | group 1 (n = 28) | group 2 (n = 25) |
| Duration of paroxysmal atrial tachycardia, days (M±m) | 3,7±0,6 | 4,1±2,9 |
| Duration of ischemic heart disease, years (M±m) | 4,2±1,5 | 3,7±1,3 |
| Myocardial infarction, n (%) | 38 | 29 |
| Myocarditis, n (%) | 2 | 0 |
| Cardiomyopathy, n (%) | 8 | 4 |
| Hypertension, n (%) | 33 | 37 |
| Diabetes mellitus type 2, n (%) | 12 | 9 |
| Hypercholesterolemia, n (%) | 42 | 40 |
| Ventricular premature beats, n (%) | 14 | 11 |
| Supraventricular arrhythmias, n (%) | 8 | 7 |
In the 1st group included (n = 28) patients undergoing therapy following:
1 Cordarone (Sanofi-Aventis / France) - 600 mg / day in the 1st day, the 2nd day to 400 mg / day., On the third and subsequent days, 200 mg / day., Within 7 days , followed by the transition to B-blocker - Concor (Merck / Germany) - 5 mg per day.
For all these measures groups were not significantly different from each other (p> 0.05).
2 From the moment of admission, administered one-time 4% sodium hydrogen carbonate - 200 ml / drip, with subsequent transition to kudesan Q10 (Akvion / Russia) - 10 drops (0.5 ml) 2 times a day with meals for 1 month. previously dissolved in a small amount of water.
3 Solkoseril (Solco Basel / Poland) - the drug was administered at 2 ml / drip (previously diluted in 250 ml 0.9% sodium chloride) for 5 days. 4 Dabigatran (prodaksa), Boehringer Ingelheim Pharma GmbH & Co. KG (Germany) - 150 mg, 1 time a day. The 2nd group included (n = 25) of patients.
1 Cordarone (Sanofi-Aventis / France) - 600 mg / day in the 1st day, the 2nd day to 400 mg / day., On the third and subsequent days, 200 mg / day., Within 7 days , followed by the transition to B-blocker - Concor (Merck / Germany) - 5 mg per day.
2 Dabigatran (prodaksa), Boehringer Ingelheim Pharma GmbH & Co. KG (Germany) - 150 mg, 1 time a day.
In addition to the results of clinical and laboratory studies (clinical analysis of blood and urine, total cholesterol), patients in both groups was carried out daily, three-time ECG examination. On the 2nd day, and a month later, all patients underwent ECG monitoring (CM ECG).
ECG study was conducted using a computer program of “Poly - spectrum” Neurosoft (Ivanovo). SM ECG Holter was performed using the computer program «DiaCard» CJSC “Medic” (Moscow).
Statistical Treatment Of Results Of Research
Statistical analysis of the results of research carried out using the software package STATISTICA 6.0 (StatSoft Inc, USA).
Analysis of normality studied traits analyzed using the Shapiro-Wilk test. Quantitative data are presented as mean values and standard deviations (M ± SD). Statistical significance of differences was assessed by Student t-test for dependent and independent samples, with uneven distribution using nonparametric Wilcoxon (x2). Statistical significance of differences or shear effect due to treatment was assessed at the level of p ≤ 0.05.
Results
According to the results of the ECG in the 1st study group, sinus rhythm was restored in 19 (67.8%) patients after 6 hours from the beginning of hospitalization and treatment. More in 5 (17.8%) of the patients heart rhythm was restored after 48 hours from the moment of admission to the hospital, and after 7 days of heart rhythm was restored in the remaining 4 (14.2%) patients, respectively, in all 28 patients. Statistically significant reduction from baseline (P <0.001).
According to the results (see ECG) - on the 2nd day of AF paroxysms were observed in 13 (46.4%) patients after 1 month none of the patients (P <0.05) [Table 3].
Table 3. Results SM ECG in the 1st study group (M±SD).
Note: The statistical significance of inter-group differences in the t-test for dependent data (r1-2- between the 1st and 2nd stages), n-number of patients with arrhythmia and u 2 before and after by Wilcoxon, step by step.
| Performance | After 48 h (1) | After 1 month (2) | Growth rate,% (48 h-1 month) |
| Number of episodes of painful ischemia | 3,42±2,68 | 0,71±1,61 | -79,2 Р1-2= 0,000009 |
| Number of episodes of silent ischemia | 4,80±3,45 | 0,90±2,05 | -81,2 Р1-2= 0,000001 |
| The average duration of episodes of paroxysmal AF or TA min | 18,53±3,85 | 0,00 | -100,0 Р1-2= 0,000004 |
| Ventricular premature beats, n | 11 | 11 | (1-2) (χ 2=16,0 р=0,00) |
| Supraventricular extrasystoles, n | 7 | 5 | (1-2) (χ 2=12,0 р=0,009) |
According to the results of the ECG in the 2nd - group, sinus rhythm was restored in 13 (48.0%) patients after 6 hours from the beginning of hospitalization and treatment. More in 7 (32.0%) patients of CP recovered after 48 hours of admission to the hospital. 7 days - AF was observed in 5 (20%) patients, respectively, heart rhythm they never recovered. Statistical reduction from baseline (P <0.001).
According to the results (see ECG) on the 2nd day, paroxysms of AF were observed in 15 (60.0%) patients, and 1 month in 7 (20.0%) patients (P <0.05) [Table 4].
Table 4. Results SM ECG 2nd study group (M±SD).
Note: The statistical significance of inter-group differences in the t-test for dependent data (r1-2- between the 1st and 2nd stages), n-number of patients with arrhythmia and u 2 before and after by Wilcoxon, step by step.
| Performance | After 48 h (1) | Within 1 month (2) | Growth rate,% (48 h-1 month) |
| Number of episodes of painful ischemia | 3,38±2,95 | 0,86±1,62 | -74,5 Р1-2= 0,0003 |
| Number of episodes of silent ischemia | 4,52±3,37 | 1,00±1,94 | -77,8 Р1-2= 0,0002 |
| The average duration of episodes of paroxysmal AF or TA min | 15,36±4,22 | 3,17±2,25 | -78,1 Р1-2= 0,0003 |
| Ventricular premature beats, n | 14 | 10 | (1-2) (χ 2=20,9 р=0,00) |
| Supraventricular extrasystoles, n | 8 | 4 | (1-2) (χ 2=8,9 р=0,038) |
Discussion
The study revealed significant differences in the dynamics of the electrocardiogram and daily ECG monitoring in the two groups.
In group 1, with the appointment of a comprehensive treatment of a statistically significant reduction in the number of patients with paroxysmal AF, six hours after admission to the hospital with n = 19 of 28 Much of this effect is due to the appointment of Cordarone with sodium bicarbonate. In the following 48 hours of complex treatment kordaronom, kudesanom and solkoserilom, sinus rhythm was restored in 5 patients, and after 7 days, the remaining four (P <0.001). Further comprehensive antioxidant treatment on an outpatient basis, a control examination CM ECG one month showed that relapse paroxysm AF are not revealed in the examined patients of group 1 (P <0.05).
According to the results (see ECG) - the second day of paroxysms of AF in group 1 were observed in 13 (46.4%) patients, and 1 month later episodes of paroxysmal absent in all patients (P <0.05). ([Fig. one]).
Figure 1.
In group 2, the subjects with the main purpose of Cordarone without antioxidant therapy and reparant, just decreased the number of patients with paroxysmal AF (P <0.001). After 6 hours, the sinus rhythm was restored in 13 of the 25 patients from the start of admission and early treatment, and even at n = 7 for 48 hours. In 4 patients, paroxysmal atrial fibrillation and atrial flutter 1 turned into a permanent form (P> 0.05).
According to the results (see ECG) on the 2nd day, paroxysms of AF were observed in 15 (60.0%) patients, and 1 month in 7 (20.0%) patients (P <0.05). [Figure 1].
Thus, it can be noted that a comprehensive treatment kordaronom, sodium hydrogen carbonate and kudesanom contributed to the creation of anesthesia and antioxidant protection for ectopic sites, and solkoseril restored antioxidant barrier along the pathways of the atria. This has led to excellent results in group 1 had completely disappeared paroxysms of AF, and in the 2nd group of five patients with atrial fibrillation and moved into a permanent form, and still remained in seven episodes of paroxysmal. As we can see, the use as a basic drug Cordarone only, not as effective. Probably, it leads only to a temporary anesthetic stabilization of ectopic foci, followed by the inclusion of compensatory abilities of the body to restore the antioxidant barrier. But the ability of the organism are not unlimited, especially in the age of patients, and for this you need to carry out a comprehensive treatment with the additional use reparants and antioxidant drugs.
In both groups, there was no side effects from the therapy, all patients comply with their assigned mode of treatment failures and drop-outs were not. In the chapter “Introduction”, we described the cause of atrial fibrillation, and heart, and in the discussion of the topic, we want to offer you the mechanism of their development. If you can analyze these mechanisms, then you will understand that we are not trying to go to the section of the existing scientific data, we are only their orderable.
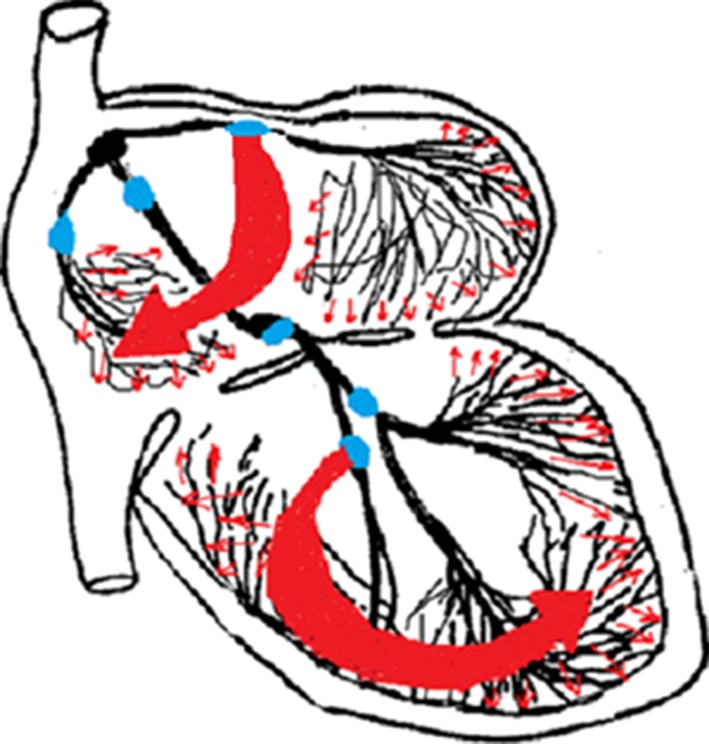
One may wonder why the proposed mechanism of atrial right? The fact that the most powerful source of ectopic supraventricular paroxysmal tachycardia and atrial flutter is in the atria (atrial fibrillation does not count, it is due to multiple ectopic), but ECG is observed different picture, why? Because supraventricular paroxysmal tachycardia electrical impulses to overcome obstacles, passing through many small pathways and ectopic sites in the atria, and then he goes to the myocardium is not as powerful impetus, as in macro - re-entry. A atrial flutter on the myocardium smoothly sees powerful wave electric pulse (macro - re-entry), connective tissue damage through the insulation shell [Figure 1].
Figure 2: The figure of the heart can be seen, the formation of a powerful wave of macro - re-entry at damage to the connective tissue adhesive coating pathways in heart atria and ventricles (large red arrow). The simultaneous excitation of the myocardium through Purkinje fibers (small red arrows). Blue dots indicate the likely fault locations connective insulation shell with structural heart disease, as well as, the approximate anatomical location of the proximal ectopic sites in the atria and the ventricles, which are able to run as paroxysmal tachycardia, and flutter.
This mechanism can be compared with the syndrome WPW, only in this case, a large part of the wave of electrical excitation (wave macro - re-entry), vomited through the damaged connective insulation shell covers less passed through the pathways of the heart, and the F-wave flutter - a delta wave pre-excitation infarction.
Oxidation and irritation of the proximal ectopic focus in damage connective insulation shell with free discharge of electricity in the atrial myocardium, contributes to a more rapid reduction in the power voltage in the pathways and ectopic foci. This shortens the refractory period, which leads to higher frequency rate during atrial flutter, paroxysmal supraventricular than tachycardia. Accordingly, in the interruption of atrial fibrillation and restoring sinus rhythm, the ECG will be celebrated only broad P wave (more than 0.13 sec.). Moreover, F delta wave macro - re-entry will be present, but it will merge with P tooth and become invisible due to the fact that the source of rhythm shift to the sinus node and the electricity goes in three ways: Wenckebach, Bachman and Toreli.
In the book written by Genco of the existence of two theories of flutter, increased ectopic activity or development of a powerful wave (macro - re-entry).[3] This study and the described mechanism does not refute any of the theories, and combines them into a single mechanism of flutter.
Fibrillation, most often damaged connective insulating sheaths distal portions of the conductive paths of the heart (atrial or ventricular branch) or multiple damage transition of T cells. This leads to the oxidation of not one but several less powerful ectopic foci and the development of atrial fibrillation with the mechanism of micro - re-entry.
In the assumed cause of AF, it is clear that the damage antioxidant barriers pathways of the heart and along these ectopic sites, leading to a rapid oxidation process with the development of AF. The longer the oxidation process continues, the greater will be deposited calcium salts around ectopic sites to form calcific capsules, respectively, such oxidation will never recover sinus rhythm of the heart, without cauterization of ectopic foci (ablation).
Analysis of the literature indicates that in many studies, structural and pathological condition of the heart is the source of a life-threatening arrhythmias:
is a prerequisite for the emergence of life-threatening arrhythmias is the presence of structural heart disease, which leads to the formation of an unstable substrate under the influence of various functional factors. As these structural changes that underpin the development of LTA can be: marked hypertrophy, dilatation, aneurysm, heart, necrotic and sclerotic processes myocardial inflammation with swelling of the myocardial tissue, etc. These changes, according to many researchers, are anatomic substrate with different mechanisms of occurrence of LTA.[6]
for the appearance of LTA requires a combination of several factors predisposing to CEI: the presence of a substrate (structural heart disease), the modulation of the autonomic nervous system dysfunction and triggering factors LTA. Morphological substrate that creates inhomogeneity impulse conduction after a myocardial infarction, is the border with necrotic tissue infarction zone formed of intertwined islands of viable myocardial fibers and connective tissue. At this point, the path of the pulse is lengthened due to the fact that the connective tissue islets become barriers to excitation wavelength, and the speed is slowed down as a result of violation of a parallel orientation of the muscle fibers. Thus, the area of myocardium with delayed ventricular depolarization may represent the anatomical and physiological substrate for re-entry - the main mechanism of LTA.[8]
Conclusions
The study showed that the complex pharmacological effect on the causes of atrial fibrillation and flutter of the heart, leading to a more significant effect than just an anti-arrhythmic. This effect is achieved due to the impact on all parts of structural heart disease in the development of atrial fibrillation and flutter. Integrated use of Cordarone with antioxidant drugs - sodium bicarbonate and kudesan (Q10), as well as reparants - solkoseril, just contributes to the stabilization of electrical processes of the heart.
Disclosures
None.
References
- 1.Zajnutdinov TA. An experimental and clinical study of antiarrhythmic activity Qudesan. Scientific library of dissertations and abstracts. Saransk. http://www.dissercat.com/content/eksperimentalno-klinicheskoeissledovanie- protivoaritmicheskoi-aktivnosti-kudesana#ixzz31xmL1QXS. 2008;13:128–0. [Google Scholar]
- 2.Kakuchaya TT, Kochladze NG. Nearitmicheskie drugs in the treatment of atrial fibrillation. Annals arrhythmology. 2005;0:32–39. [Google Scholar]
- 3.Orlov VN. Guidelines for electrocardiography. 4th sr. izd.-M .: Medical Information Agency. 2004;0:528–0. [Google Scholar]
- 4.Habchabov RG. Single cause and mechanism of electrical instability pathways for all structural and pathological heart disease. Journal of scientific publications and postgraduate doctors. 2012;0:48–55. [Google Scholar]
- 5.Shubik YV, Tatar BA. Correction of tissue metabolism solkoseril treating ventricular arrhythmias high grading B. Lown. Herald arrhythmology. 1998;0:74–76. [Google Scholar]
- 6.Buxton A E, Kirk M M, Michaud G F. Current approaches to evaluation and management of patients with ventricular arrhythmias. Med Health R I. 2001 Feb;84 (2):58–62. [PubMed] [Google Scholar]
- 7.Dulli Douglas A, Stanko Heather, Levine Ross L. Atrial fibrillation is associated with severe acute ischemic stroke. Neuroepidemiology. 2003 Mar 12;22 (2):118–23. doi: 10.1159/000068743. [DOI] [PubMed] [Google Scholar]
- 8.El-Sherif N, Smith R A, Evans K. Canine ventricular arrhythmias in the late myocardial infarction period. 8. Epicardial mapping of reentrant circuits. Circ. Res. 1981 Jul;49 (1):255–65. doi: 10.1161/01.res.49.1.255. [DOI] [PubMed] [Google Scholar]


