Abstract
Apixaban (factor Xa inhibitor) is a novel anticoagulant and may be beneficial during atrial fibrillation (AF) ablation for prevention of thromboembolic events. However, the adverse effects of periprocedural apixaban therapy have not been thoroughly evaluated. A meta-analysis was performed to evaluate the safety of apixaban for anticoagulation in AF ablation. We searched the online databases till October 2015 for studies comparing Apixaban with Vitamin K antagonists in atrial fibrillation patients undergoing catheter ablation. Primary outcome of our study was composite of thromboembolic event and bleeding (includes major and minor bleeding). A total of 1,057 atrial fibrillation patients in 3 studies undergoing catheter ablation were included in this analysis. Zero thromboembolic events were reported in the apixaban group and 1 in the VKA group with no statistical difference (OR 0.75; 95% CI 0.03-18.49). No major differences were observed for the primary outcome (OR 0.92; 95% CI 0.54-1.55), risk of overall bleeding (OR 0.94, 95% CI 0.55- 1.58), major bleeding (OR1.37; 95% CI 0.33-5.67), minor bleeding (OR 0.89; 95% CI 0.50-1.55), pericardial effusion (OR 0.50; 95% CI 0.18-1.38) and groin hematoma (OR 1.36; 95% CI 0.70-2.65). Uninterrupted apixaban administration in patients undergoing AF catheter ablation was non-inferior to VKA without increasing the risk of major and minor bleeding.
Keywords: Apixaban, Atrial Fibrillation Ablation, Anticoagulation, Complications
Introduction
Atrial fibrillation (AF) catheter ablation has been given a Class I recommendation (2012 AHA/ACC guidelines), for patients with symptomatic paroxysmal atrial fibrillation who are intolerant or refractory to at least one antiarrhythmic agent.[1] Traditionally, patients undergoing catheter ablation for AF had anticoagulation (Vitamin K antagonist [VKA] e.g. warfarin) discontinued 3 to 5 days prior to the procedure and were bridged with heparin or a low molecular weight heparin after the procedure until the patients were therapeutically anticoagulated with warfarin. However, there has been an increasing trend of the uninterrupted anticoagulation with VKA in patients undergoing AF ablation. In a recent meta-analysis, Nairooz et al[2] evaluated the role of uninterrupted VKA versus interrupted VKA with heparin bridging in AF ablation. They included 13 studies (1 randomized and 12 observational) with 17, 434 patients undergoing AF ablation, of which 7877 patients managed with uninterrupted approach and 9557 with interrupted approach. There was a significantly lower incidence of major bleeding (OR 0.72, 95% CI 0.54-0.95; p=0.02), minor bleeding (OR 0.33, 95% CI 0.21-0.52; p<0.0001), combined stroke and transient ischemic attack (OR 0.25, 95% CI 0.10-0.62; p=0.003) with uninterrupted VKA as opposed to an interrupted VKA and bridging heparin/enoxaparin strategy. Similarly, with advent of newer oral anticoagulant (NOAC’s)(especially dabigatran, rivaroxaban and apixaban, numerous studies have demonstrated thromboembolic safety profile in patients not only with non-valvular AF but also undergoing AF ablation with lower bleeding rates. In light of these findings, 3 studies have been conducted so far (1 retrospective and 2 prospective) assessing the safety and efficacy of uninterrupted apixaban in patients undergoing AF ablation as compared to VKA.[3-5] In view of these studies, we aim to perform a meta-analysis to assess for safety uninterrupted periprocedural apixaban in patients undergoing AF ablation.
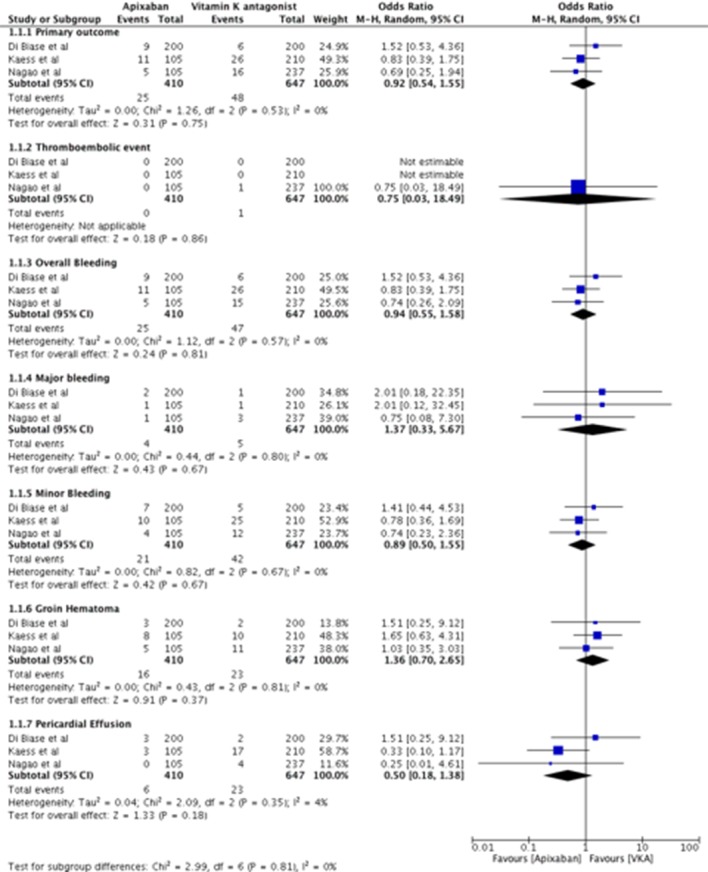
We searched PubMed, The Cochrane Library, EMBASE, EBSCO, Web of Science and CINAHL databases from the inception through October 15, 2015 comparing uninterrupted apixaban with uninterrupted VKA peri AF ablation. All endpoints were reported through the longest follow up available. The primary safety outcome in our study was a composite of thromboembolic event and overall bleeding. Individual outcomes assessed in our study were thromboembolic event, overall bleeding, major and minor bleeding, groin hematomas and pericardial effusion. Random effects model was followed to estimate the odds ratios (OR) and respective 95% confidence intervals (CI) using Cochrane Collaborative software, RevMan 5.3. Measure of heterogeneity between the studies was assessed using the chi square test and was considered significant if p values < 0.10 or I2 > 50%.
Three trials (2 prospective, 1 retrospective) with a total of 1,057 patients were included in the analysis, of those 410 on uninterrupted apixaban versus 647 uninterrupted VKA. Characteristics of included studies and periprocedural anticoagulation strategy are described in [table 1]. Zero thromboembolic events were reported in the apixaban group versus 1 in the VKA group with no statistical difference (OR 0.75; 95% CI 0.03-18.49). No statistical significant difference in the primary outcome (OR 0.92; 95% CI 0.54-1.55) was observed in our study. Consistently, no difference was observed in risk of overall bleeding (OR 0.94, 95% CI 0.55- 1.58), major bleeding (OR1.37; 95% CI 0.33-5.67), minor bleeding (OR 0.89; 95% CI 0.50-1.55), pericardial effusion (OR 0.50; 95% CI 0.18-1.38) and groin hematoma (OR 1.36; 95% CI 0.70-2.65) in the apixaban group as compared to VKA group ([figure 1]).
Table 1. Descriptive characteristics of included studies.
| Name, year | Type of study | n, Study /Control | Anticoagulation protocol | Follow-up period | Thromboembolic complications, n (%) | Bleeding events, n(%) | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| AG | VG | p | AG | VG | p | |||||
| Di Biase et al, 2015 | Prospective multicenter registry | 400; 200/200 | Apixaban 2.5 mg or 5 mg two times a day according to creatinine clearance for up to 3 weeks pre-procedurally. Patients were instructed to take their apixaban dose the morning of the procedure without any discontinuation and to take next dose the same night of the procedure. | 30 days post-procedure | 0 | 0 | >0.99 | 9 (4.5%) | 6 (3%) | 0.43 |
| Nagao et al, 2014 | Retrospective case control study | 342; 105/237 | Anticoagulation was started 4 weeks before; apixaban was dosed into 2.5 mg or 5 mg two times a day based on creatinine clearance, age (2.5 mg BID for ≥ 80 yrs) and weight (2.5 mg for ≤ 60 kg). On the procedural day, the dose of apixaban was administered in the morning and in the night as usual days in the Apixaban group. | 3 months post-procedure | 0 | 1 (0.4%) | 0.51 | 5(5%) | 15 (6%) | 0.57 |
| Kaess et al, 2014 | Prospective case control study | 325; 105/210 | Anticoagulation atleast 4 weeks before the procedure; All patients received apixaban 2.5 mg in the morning of procedure followed by their usual dosage in the evening; 95% of patients in apixaban were on 5 mg BID and 5% on 2.5 BID | Till the time of discharge (2 days for majority of patients) | 0 | 0 | >0.99 | 11 (10.5%) | 26 (12.3%) | 0.71 |
Figure 1. Forest plot of primary outcome, thromboembolic events, overall bleeding events, groin hematoma, pericardial effusion in patients undergoing ablation of atrial fibrillation with uninterrupted apixaban compared to uninterrupted vitamin K antagonist.
This is the first meta-analysis of the currently available literature comparing uninterrupted apixaban to uninterrupted VKA in patients undergoing AF ablation. Among 1,047 patients who underwent AF ablation, we demonstrated that there was no difference in the primary outcome (i.e. composite of thromboembolic events and bleeding) in either group. Although non significant there were no thromboembolic events in the apixaban group as compared one event in the VKA group. Interestingly there was also no significant difference observed in the secondary endpoints of major bleeding, minor bleeding, pericardial effusion or groin hematoma in either strategy. Interestingly, the periprocedural activated clotting time in VKA group was significantly higher in all 3 studies: 258±26 versus 288±34, p<0.001;[5] 342.1±23.1 versus 363.1±26.5, p<0.001;[4] 275±54 versus 313±47, p<0.001,[3] apixaban and VKA groups respectively. However no difference in the bleeding events were observed in the both groups.
Based on our study, apixaban was the non-inferior to uninterrupted VKA in patients undergoing AF ablation. In a recent meta-analyses by Lu et al assessing the safety and efficacy of apixaban in patients undergoing atrial fibrillation ablation, apixaban was as effective as VKA (that corroborates with our study), but our study is essentially different from this meta-analyses as we only included trials in which apixaban was used in uninterrupted fashion, and excluded all trials where apixaban was either stopped a night before or started on postprocedure day 1 (as included in Lu et al meta-analysis).[6]
Also other NOAC agents that have been compared to VKA include dabigatran and rivaroxaban. There has been conflicting data with Steinberg et al[7] and Sardar et al[8] demonstrating an increase in neurologic complications with dabigatran compared to VKA. This is contrary to the meta-analysis conducted by Honhloser et al[9] and Providencia et al[10] who demonstrated no significant differences in the composite of neurologic and bleeding complications between the dabigatran and uninterrupted VKA groups. Rivaroxaban has even lesser data and no meta-analysis to compare the uninterrupted Rivaroxaban against uninterrupted VKA.
Given the lack of literature, a randomized controlled trial AFAXA (Apixaban During Atrial Fibrillation Catheter Ablation: Comparison to Vitamin K Antagonist Therapy; NCT02227550) will provide valuable information as the study compares fixed dose apixaban (5 mg two times a day) with uninterrupted VKA (goal INR 2.0-3.0) in AF ablation.[11] The primary outcome of the study is composite of allcause mortality, stroke (ischemic stroke, subarachnoid hemorrhage and hemorrhagic stroke), and major bleeding events with follow-up period of up to 4 months.
One of the major limitations of the current meta-analysis includes reliance on retrospective and prospective and lack on any randomized controlled trials. In the trial by Kaess et al,[5] irrespective of the patient’s home apixaban dose or renal function, a fixed dose of 2.5 mg was administered to apixaban group, which could potentially result in decreased bleeding events. Despite, heterogeneity in trials design, study protocols, and baseline characteristics of study population, the test of heterogeneity was non significant.
Conclusions
In this meta-analysis of patients undergoing AF ablation, apixaban was safe and non-inferior to uninterrupted VKA without any increase the risk of thromboembolic event, major and minor bleeding. Although the results from randomized controlled trials are pending, our study demonstrates that safety and efficacy of apixaban in comparison to uninterrupted VKA, and hence supports its use in AF ablation.
Disclosures
None.
References
- 1.Calkins Hugh, Kuck Karl Heinz, Cappato Riccardo, Brugada Josep, Camm A John, Chen Shih-Ann, Crijns Harry J G, Damiano Ralph J, Davies D Wyn, DiMarco John, Edgerton James, Ellenbogen Kenneth, Ezekowitz Michael D, Haines David E, Haissaguerre Michel, Hindricks Gerhard, Iesaka Yoshito, Jackman Warren, Jalife José, Jais Pierre, Kalman Jonathan, Keane David, Kim Young-Hoon, Kirchhof Paulus, Klein George, Kottkamp Hans, Kumagai Koichiro, Lindsay Bruce D, Mansour Moussa, Marchlinski Francis E, McCarthy Patrick M, Mont J Lluis, Morady Fred, Nademanee Koonlawee, Nakagawa Hiroshi, Natale Andrea, Nattel Stanley, Packer Douglas L, Pappone Carlo, Prystowsky Eric, Raviele Antonio, Reddy Vivek, Ruskin Jeremy N, Shemin Richard J, Tsao Hsuan-Ming, Wilber David. 2012 HRS/EHRA/ECAS expert consensus statement on catheter and surgical ablation of atrial fibrillation: recommendations for patient selection, procedural techniques, patient management and follow-up, definitions, endpoints, and research trial design: a report of the Heart Rhythm Society (HRS) Task Force on Catheter and Surgical Ablation of Atrial Fibrillation. Developed in partnership with the European Heart Rhythm Association (EHRA), a registered branch of the European Society of Cardiology (ESC) and the European Cardiac Arrhythmia Society (ECAS); and in collaboration with the American College of Cardiology (ACC), American Heart Association (AHA), the Asia Pacific Heart Rhythm Society (APHRS), and the Society of Thoracic Surgeons (STS). Endorsed by the governing bodies of the American College of Cardiology Foundation, the American Heart Association, the European Cardiac Arrhythmia Society, the European Heart Rhythm Association, the Society of Thoracic Surgeons, the Asia Pacific Heart Rhythm Society, and the Heart Rhythm Society. Heart Rhythm. 2012 Apr;9 (4):632–696.e21. doi: 10.1016/j.hrthm.2011.12.016. [DOI] [PubMed] [Google Scholar]
- 2.Nairooz Ramez, Sardar Partha, Payne Jason, Aronow Wilbert S, Paydak Hakan. Meta-analysis of major bleeding with uninterrupted warfarin compared to interrupted warfarin and heparin bridging in ablation of atrial fibrillation. Int. J. Cardiol. 2015;187 ():426–9. doi: 10.1016/j.ijcard.2015.03.376. [DOI] [PubMed] [Google Scholar]
- 3.Nagao Tomoyuki, Inden Yasuya, Shimano Masayuki, Fujita Masaya, Yanagisawa Satoshi, Kato Hiroyuki, Ishikawa Shinji, Miyoshi Aya, Okumura Satoshi, Ohguchi Shiou, Yamamoto Toshihiko, Yoshida Naoki, Hirai Makoto, Murohara Toyoaki. Efficacy and safety of apixaban in the patients undergoing the ablation of atrial fibrillation. Pacing Clin Electrophysiol. 2015 Feb;38 (2):155–63. doi: 10.1111/pace.12553. [DOI] [PubMed] [Google Scholar]
- 4.Di Biase Luigi, Lakkireddy Dhanujaya, Trivedi Chintan, Deneke Thomas, Martinek Martin, Mohanty Sanghamitra, Mohanty Prasant, Prakash Sameer, Bai Rong, Reddy Madhu, Gianni Carola, Horton Rodney, Bailey Shane, Sigmund Elisabeth, Derndorfer Michael, Schade Anja, Mueller Patrick, Szoelloes Atilla, Sanchez Javier, Al-Ahmad Amin, Hranitzky Patrick, Gallinghouse G Joseph, Hongo Richard H, Beheiry Salwa, Pürerfellner Helmut, Burkhardt J David, Natale Andrea. Feasibility and safety of uninterrupted periprocedural apixaban administration in patients undergoing radiofrequency catheter ablation for atrial fibrillation: Results from a multicenter study. Heart Rhythm. 2015 Jun;12 (6):1162–8. doi: 10.1016/j.hrthm.2015.02.028. [DOI] [PubMed] [Google Scholar]
- 5.Kaess Bernhard M, Ammar Sonia, Reents Tilko, Dillier Roger, Lennerz Carsten, Semmler Verena, Grebmer Christian, Bourier Felix, Buiatti Alessandra, Kolb Christof, Deisenhofer Isabel, Hessling Gabriele. Comparison of safety of left atrial catheter ablation procedures for atrial arrhythmias under continuous anticoagulation with apixaban versus phenprocoumon. Am. J. Cardiol. 2015 Jan 1;115 (1):47–51. doi: 10.1016/j.amjcard.2014.10.005. [DOI] [PubMed] [Google Scholar]
- 6.Lu Dasheng, Liu Qian, Wang Kai, Zhang Q I, Shan Qi-Jun. Meta-Analysis of Efficacy and Safety of Apixaban in Patients Undergoing Catheter Ablation for Atrial Fibrillation. Pacing Clin Electrophysiol. 2016 Jan;39 (1):54–9. doi: 10.1111/pace.12771. [DOI] [PubMed] [Google Scholar]
- 7.Steinberg Benjamin A, Hasselblad Vic, Atwater Brett D, Bahnson Tristram D, Washam Jeffrey B, Alexander John H, Daubert James P, Piccini Jonathan P. Dabigatran for periprocedural anticoagulation following radiofrequency ablation for atrial fibrillation: a meta-analysis of observational studies. J Interv Card Electrophysiol. 2013 Sep;37 (3):213–21. doi: 10.1007/s10840-013-9813-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sardar Partha, Nairooz Ramez, Chatterjee Saurav, Wetterslev Jørn, Ghosh Joydeep, Aronow Wilbert S. Meta-analysis of risk of stroke or transient ischemic attack with dabigatran for atrial fibrillation ablation. Am. J. Cardiol. 2014 Apr 1;113 (7):1173–7. doi: 10.1016/j.amjcard.2013.12.027. [DOI] [PubMed] [Google Scholar]
- 9.Hohnloser Stefan H, Camm A John. Safety and efficacy of dabigatran etexilate during catheter ablation of atrial fibrillation: a meta-analysis of the literature. Europace. 2013 Oct;15 (10):1407–11. doi: 10.1093/europace/eut241. [DOI] [PubMed] [Google Scholar]
- 10.Providência Rui, Albenque Jean-Paul, Combes Stephane, Bouzeman Abdeslam, Casteigt Benjamin, Combes Nicolas, Narayanan Kumar, Marijon Eloi, Boveda Serge. Safety and efficacy of dabigatran versus warfarin in patients undergoing catheter ablation of atrial fibrillation: a systematic review and meta-analysis. Heart. 2014 Feb;100 (4):324–35. doi: 10.1136/heartjnl-2013-304386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Di Biase Luigi, Natale Andrea. Apixaban is dear to me, but dearer still is warfarin. Pacing Clin Electrophysiol. 2015 Feb;38 (2):153–4. doi: 10.1111/pace.12570. [DOI] [PubMed] [Google Scholar]


