Abstract
Threshold testing of cardiac rhythm devices is essential to monitoring the proper functioning of such devices (1). However, the currently method of applying multiple ECG leads to the patient is burdensome and time consuming (2). We are presenting a completely new way to perform cardiac rhythm device threshold testing using pulse oximetry.
Twenty patients, with varying cardiac rhythm devices and pacing modes, were enrolled and had their atrial and ventricular thresholds tested. A comparison was made between simultaneous threshold determinations via the standard EGM based method and the new pulse oximetry based method. 75% of the ventricular threshold tested and 58% of the atrial thresholds tested were the same with the two testing methods. The remainder of the tests (25% of ventricular threshold and 42% of the atrial threshold tests) varied by +0.25 V.
This study shows that pulse oximetry based testing is an accurate, reliable, and easy way to perform cardiac rhythm device threshold testing and may complement traditional methods to perform such tests in the future.
Keywords: Cardiac Rhythm, Oximetry, Plethysmography, Photoplethysmogram
Introduction
Monitoring of cardiac rhythm devices is key to preventing, identifying and solving problems with the devices.[1] A standard interrogation includes sensitivity, impedance, and threshold testing. While sensitivity and impedance testing are fairly quick and easy to do, threshold testing is fairly labor intensive and uncomfortable to the patient.[2]
Currently threshold testing procedures involve placing multiple ECG leads on the patient and using the interrogator to slowly lower the pacing Voltage outputs while monitoring when devices loses capture. This usually involves undressing the patient and applying ECG leads and electrodes to the patient. This is further complicated if the patient has applied lotion to the skin, or has a lot of hair, making the ECG signal much less accurate. New algorithms have allowed for simpler threshold testing, but the new interrogator based tests still require accurate interpretation of ECG and/or EGM interpretation.
We have discovered a new way of performing threshold testing for cardiac rhythm devices, which is based on pulse oximetry. This new process uses the principle of plethysmography, which is a process of determining changes in volume based on the physical relationship between pressure and volume. A photoplethysmogram, such as a pulse oximeter, is an optically obtained plethysmogram, and relies on an optical source to detect changes in volume of body fluids as a result of pressure waves.[3,4] Pulse oximeters emit light and are able to measure the change in light absorbance and reflection, and correlate it to the change in volume of blood within a pulse pressure wave.[3,4] This then creates a fairly accurate and reliable graph of the increase and decrease of blood volume in a specific body part, which is then indicative of the actual cardiac pulse in the body.
The new threshold testing protocol proposed here relies on pulse oximetry. A standard pulse oximeter, which is able to procedure a plethysmographic curve on a display, is placed on the digit of a patient. Once a clear plethysmographic curve is produced, standard technique of decreasing output voltage of the cardiac rhythm device is used to determine when the capture is lost. At the point of loss of capture, a cardiac pulse would not be produced, and a loss of the pulse pressure would result in a reduction or loss of the change in blood volume in the measured digit. This curve would then resume its normal volume change recording once a pulse is reestablished, which would be a result of either pacing at higher output voltage or the resumption of patient’s natural heart beat.
Methods
Twenty consecutive patients with cardiac rhythm devices (biventricular devices were excluded) were enrolled in the study from a busy cardiac rhythm device clinic in Brooklyn, NY. Standard informed consent protocols were followed with all of the enrolled patients.
A standard deluxe handheld pulse oximeter, Model CCI-300M, was used for the study. The pulse oximeter was placed on the index finger of all patients (patients would chose which arm they preferred). One patient was on hemodialysis, and had a AV graft on the right side, forcing us to use the left arm for the study analysis.
Once a good plethysmographic curve was established, the threshold testing would begin. Two board certified physicians were involved with the testing of each patient. One of the physicians was placed at the interrogator and was managing the threshold testing protocol using a standard algorithm (start at 2.0 V, and decrease the voltage by 0.25 V on every third beat). All threshold testing was done at 0.4 msec. This physician would state out loud every time the output was lowered and to what voltage. This physician would also record on a piece of paper (without announcing the value) the threshold result based on the ECG and EGM monitoring of the interrogator machine. The second physician was placed near the patient and had a clear view of the pulse oximeter plethysmographic output curve. The second physician did not have the ability to see the interrogator screen or any documentation by the first physician. The job of the second physician was to monitor the plethymosgraphic curve, and listen to the voltage readings by the first physician. Once the second physician saw that the pacing threshold was reached, the physician would record the threshold value for comparison.
For ventricular threshold testing, all tests were done in VVI mode at a rate of 90 bpm. For atrial threshold testing, tests were done either in AAI mode (if possible based on the state of patient’s conduction system) or DDD mode at 90 bpm. If the patient’s native heart rate was noted to be above 85 bpm, the testing was performed at 10 bpm higher than the patient’s native heart rate.
If the loss of capture (atrial or ventricular) occurred at >1.5 V, the threshold testing would be repeated starting at 4V. If the loss of capture occurred at >3.5 V, that patient was excluded from this study.
For every patient, the threshold results of the two physicians were analyzed and compared. For clinical purposes, the result obtained by the ECG/EGM method was used for cardiac rhythm device management and adjustment.
Results
All together, twenty patients were selected consecutively for this study. Out of the twenty selected, all twenty agreed to participate in the study.
Out of the twenty patients, five were set in VVI mode and pacemaker dependent, three were set in VVI mode and were not pacemaker dependent, five were set in DDD mode and were pacemaker dependent (either atrial, ventricular, or both) and seven were set in DDD mode and were not pacemaker dependent. No patient had a resting heart rate above 85 bpm. There were no patients who had generators at ERI or EOL.
All threshold tests were performed only once. There were twenty ventricular threshold tests performed and twelve atrial threshold tests performed.
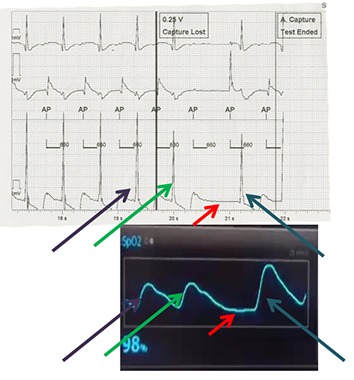
[Figure 1] shows the EGM (above) and pulse oximetry (below) based displays while conducting atrial threshold testing. This was recorded simultaneously in a patient who was atrial pacing dependent, but did not have AV block. As such, atrial threshold testing was performed in AAI mode. Arrows of the same color represent the corresponding beats in the two sets of displays. Purple arrows represent the beat prior to the threshold setting beat. The green arrows represent the beat that is the threshold beat. The red arrows represent a failure to capture beat, and the blue arrows represent the resumption of normal atrial pacing in this patient. Nicely illustrated here in the pulse oximetry curve is the concept that a beat after a pause produces a stronger contraction than prior beats (the blue arrow beat has a much higher amplitude than purple and green arrow beats).
Figure 1. Simultaneous EGM (top) and pulse oximetry (bottom) displays during atrial threshold testing in AAI format. Purple and green arrows represent captured beats during threshold testing, red arrows show the missed capture beat, and the blue arrows shows the beat after resumption of normal pacing.
Out of the twelve atrial threshold tests performed, seven (58%) had the same threshold results between the two physicians involved in the tests. The other 42% had differences of no more than 0.25 V.
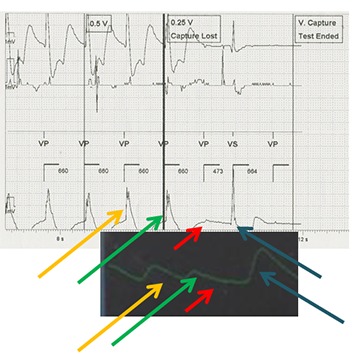
[Figure 2] shows the EGM and pulse oximetry based displays in ventricular threshold testing. This was conducted in a patient who was not pacemaker dependent, in VVI format. These were recorded simultaneously. Yellow and green arrow beats are prior to the missed capture beats, with the green arrow representing the threshold setting beat. The red arrow represents the missed capture beat, and the blue arrow representing the patient’s native beat after threshold has been reached. As in [Figure 1], the amplitude of the post pause beat is higher than the pre-pause beats. However, in this case the post pause beat is a patient’s native beat, and not a paced beat.
Figure 2. Simultaneous EGM (top) and pulse oximetry (bottom) displays during ventricular threshold testing in VVI format. Yellow and green arrows represent captured beats during threshold testing, red arrows show the missed capture beat, and the blue arrows shows the resumption of native beating.
Out of the twenty ventricular threshold tests, fifteen (75%) had the same threshold as recorded by the two physicians involved in the tests. The other 25% of the tests had a difference of 0.25 V between the two recorded thresholds. There were no difference above 0.25 V in any of the performed ventricular threshold tests.
Figure 3 shows the pulse oximetry recording in a single patient who is not pacemaker dependent. The patient’s native heart rate was 70 bpm. On the left side of the figure (green arrow) there is a beat recorded while the patient is being paced at VVI 75 bpm (pacing is doen at 2 V @0.4 msec, which is higher than the patient’s ventricular threshold of 0.75 V @0.4 msec). On the right side of the figure (red arrow) there is a patient’s native beat recorded. The amplitude of the patient’s native beat is much higher than the patient’s ventricular paced beat. Although this amplitude difference can be caused by the higher pulse during pacing, we set the difference in heart rate as small as possible between native and paced beats, and believe that it should not account for such a large difference in amplitude between the two beats.
Discussion
The use of pulse oximetry is a reliable and accurate method to determine the atrial and ventricular thresholds of cardiac rhythm devices. In this study, we have shown as proof of concept the successful determination of atrial and ventricular thresholds using pulxe oximetry.
The use of EGM/ECG based algorithms to determine thresholds is complicated, labor intensive, and patient effort intensive, which is not ideal for routine cardiac rhythm device maintenance testing. Pulse oximetry is much less labor intensive and involves almost no discomfort to the patient. The patient just notices that the pulse oximeter has been applied to his/her finger during the test. There is no need for undressing, application of ecg leads, or shaving of hair.
We did observe, as expected, a higher incongruence rate with atrial threshold testing than ventricular threshold testing: 42% vs. 25% error rate respectively. We believe this to be acceptable as there was no deviation between the methods of testing by more than 0.25V in any of the cases, which is unlikely to be clinically significant. Atrial threshold testing was expected to be more difficult and less congruent since EGM and pulse oximetry based threshold testing rely heavily on the display of the effects of ventricular contraction, and it becomes necessary to account for differences in atrio-ventricular conduction. Furthermore, atrial threshold testing in patients who are pacemaker dependent may not be feasible with our method, or be technically very challenging, since it would be based on detection of subtle differences in the waveform shape, related to loss of atrial contribution to the cardiac output.
Our exploratory study suggests that pulse oximetry may be a safe, accurate, and reliable guide for the performance of threshold testing in cardiac rhythm devices. Further research needs to be performed to clarify the benefits and pitfalls of this new technique. However, with its promise of much less patient discomfort and much less labor intensive threshold testing, pulse oximetry may become a useful, alternative method of conducting cardiac rhythm device threshold testing.
Disclosures
None.
References
- 1.Schoenfeld Mark H. Contemporary pacemaker and defibrillator device therapy: challenges confronting the general cardiologist. Circulation. 2007 Feb 6;115 (5):638–53. doi: 10.1161/CIRCULATIONAHA.106.618587. [DOI] [PubMed] [Google Scholar]
- 2.Senges-Becker Julia C, Klostermann Martina, Becker Ruediger, Bauer Alexander, Siegler Karl E, Katus Hugo A, Schoels Wolfgang. What is the "optimal" follow-up schedule for ICD patients? Europace. 2005 Jul;7 (4):319–26. doi: 10.1016/j.eupc.2005.02.117. [DOI] [PubMed] [Google Scholar]
- 3.Shamir M, Eidelman L A, Floman Y, Kaplan L, Pizov R. Pulse oximetry plethysmographic waveform during changes in blood volume. Br J Anaesth. 1999 Feb;82 (2):178–81. doi: 10.1093/bja/82.2.178. [DOI] [PubMed] [Google Scholar]
- 4.Sinex JE. Pulse oximetry: Principles and limitations. Am J. Emerg Med . 1999;1:59–66. doi: 10.1016/s0735-6757(99)90019-0. [DOI] [PubMed] [Google Scholar]


