Summary
Objective
The purpose of this study is to identify distinct body mass index (BMI) trajectories associated with weight classification, and to examine demographic characteristics and clusters of obesogenic behaviours in adolescents with these trajectories.
Methods
Data were extracted from the National Institute of Child Health and Human Development Study of Early Child Care and Youth Development (n = 1,006, Grades 5–8). The independent variables were physical activity (accelerometer and child report), sports participation, television/video watching time and recreational computer use. The dependent variable was raw BMI. Growth mixture modelling, mixture modelling and independent t‐test analyses were used.
Results
Two distinct BMI trajectories were identified – one with the mean BMI within the Overweight–Obese classification (≥85th percentile) and the other within the healthy weight classification (5th– 84th percentile). Two clusters of physical and sedentary behaviours were identified in adolescents with the Overweight–Obese BMI trajectory. These clusters differed in the type of sedentary behaviour (computer vs. television/video). Three clusters were identified in adolescents with the Healthy Weight BMI trajectory. These clusters differed in levels of physical activity and types of sedentary behaviour.
Conclusion
This study contributes to the understanding of multi‐dimensional obesogenic behavioural patterns and highlights the importance of understanding types of sedentary behaviour in adolescents.
Keywords: Adolescent obesity, obesogenic behaviours, wellness promotion
Introduction
The prevalence of obesity in youth in the United States, ages 12–19 years, is 20.5% 1 as measured by body mass index (BMI; kg/m2) at or above the 95th percentile based on gender and age specific growth charts 2
Physical activity and sedentary behaviour are known correlates of adolescent obesity and are important to consider in the development of obesity prevention intervention strategies. Participation in physical activity declines during adolescence 3. And, adolescents who are less physically active are at a higher risk for obesity 4, 5. Study results indicate that adolescents who engage in higher volumes of sedentary behaviour, such as screen time, are also at a higher risk for obesity 6, 7. The combined influence of low physical activity and high sedentary behaviour is associated with 1.7 to 3.1 higher odds of overweight and obesity in several studies based on national samples 5, 8.
Recent studies suggest, however, that an increase in physical activity may not be associated with a decrease in sedentary behaviour in adolescents 9, 10, 11. An adolescent with a high level of physical activity may or may not also have a low level of sedentary behaviour – and an adolescent with a low level physical activity may or may not have a high level of sedentary behaviour 12. Despite the elevated odds of obesity for those adolescents with high sedentary behaviour and low physical activity, the assumption that physical activity displaces sedentary behaviour has not been supported in the literature 9, 13, 14, 15, 16. Some studies using latent class analysis suggest that distinct clusters of physical activity and sedentary behaviour exist in many populations 9, 13, 17, 18, 19, 20, 21.
An understanding of the path of BMI, as a trajectory of adiposity accounting for fat increase and decrease over time, is more informative than descriptions of BMI at fixed ages or between fixed ages 22. Current longitudinal studies have examined the trajectory of BMI and the relationship with obesity related risk factors, such as cardiovascular disease 23 and physical activity 24. Longitudinal studies that identify distinct paths of BMI over time, and their association with obesogenic behavioural patterns are lacking. In addition, current literature is limited on the topic of how obesogenic behaviour patterns change over time 25.
This study addresses the need to shift the narrow focus on physical activity and sedentary behaviour as individual risk factors to a broader understanding of clusters of physical activity and sedentary behaviour patterns related to BMI trajectories. In this longitudinal study, the path of BMI from Grade 5 to Grade 8 is examined. And, for each of the distinct BMI trajectories identified, demographic characteristics and clusters of physical activity and sedentary behaviour patterns are examined. The clusters of behaviour are examined at Grade 5 in order to focus on the characteristics of early adolescent behaviours associated with trends in BMI through Grade 8. Ram and Grimm (2009) 26 note the benefit from this type of exploratory study that allows subpopulations to emerge from the data. In this study, groups are not formed based on pre‐determined criteria for BMI group membership at a fixed age (for example, those with BMI ≥ 85th percentile for age and sex) – rather, distinct BMI trajectories emerge from the data. Likewise, behaviours are not labelled based on pre‐determined criteria for group membership (for example, those who watch >2 hours of television/day) – rather, the behavioural clusters emerge from the data.
The purpose of this study is to identify distinct BMI trajectories in adolescents from Grade 5 through 8, to examine the demographic characteristics of adolescents with these trajectories and to determine their unique clusters of obesogenic behaviours.
Methods
Subjects
Data were extracted from the National Institute of Child Health and Human Development Study of Early Child Care and Youth Development (NICHD SECCYD) for secondary analyses 27. Subjects were 1,006 adolescents, Grades 5–8. NICHD SECCYD is a comprehensive longitudinal study of children and the environments in which they develop. The goals of the NICHD SECCYD include researching the relationship of contextual factors that influence health during middle adolescence as well as the patterns of health and human development from infancy to middle adolescence. The instruments in the NICHD SECCYD use multiple methods including observations, interviews (parent, child, teachers), questionnaires and direct testing 27.
The NICHD SECCYD began in 1991 with a diverse sample of children at the age of 1 month and their families 28, 29. Phase III (2000 – 2004, through 6th grade) and Phase IV (2005 – 2007, through 9th grade) are utilized in this study. This study was exempt from IRB review because it uses a dataset that is de‐identified. NICHD SECCYD participants were recruited from hospitals in 10 US locations, and represent a diverse sample of children and their families with demographics consistent with the US population 28, 29. Missing values were estimated using maximum likelihood procedures.
Study variables
In this study, both BMI trajectories and obesogenic behavioural variables were analysed to find emergent trajectories and clusters. Table 1 includes the study variables, how that data were measured and the grade in which it was collected. The independent variables examined at Grade 5 were physical activity (moderate to vigorous physical activity direct measurement by accelerometer), parent report of number of sports participated in during the past year, child report of physical activity after school, child report of television and or video watching time after school, and child report of recreational computer use after school. The independent variables were selected as indicators of known correlates of adolescent obesity – physical activity and sedentary behaviour 3, 4, 5, 6, 7, 8. BMI was calculated using a programme from the Centers for Disease Control and Prevention from height and weight measured during laboratory visits at each grade level 27. The dependent variable was raw BMI at Grade 5, 6, 7 and 8. Raw BMI was determined to be the most appropriate outcome measure for obesity based on several studies that examined using raw versus BMI percentiles for longitudinal analysis 30, 31, 32.
Table 1.
Study variables
| Variable | Variable explanation | Grade |
|---|---|---|
| Physical Activity Monitor |
Computer Science and Applications, Inc. (CSA) single channel accelerometer worn by child for seven consecutive days during a typical school week. Average minutes/day of moderate to vigorous physical activity. Moderate (3 – 5.9 METs), Vigorous (6 – 8.9 METs), where: METs = 2.757 + (.0015 × count) + (−.08957 × age in years) + (−.000038 × count × age in years) |
5 |
| Parent Interviews of Child Physical Activity |
Mothers (or other parents/guardians) completed an interview to measure parental support for child physical activity. During the past year, did your child participate in any youth sports teams or clubs (including school or recreational teams)? Yes/No If yes, circle all sports that apply. Total # of sports teams or clubs the child participated in during the past year. |
5 |
| Physical Activity – Child Report |
After School Time Use Interview using a guided recall format to elicit information from the child about weekday afternoons. Scaled # of 15 min intervals/day of physical activity (school dismissal–6 pm) |
5 |
| Recreational PC/Video Game use – Child Report |
After School Time Use Interview using a guided recall format to elicit information from the child about weekday afternoons. Scaled # of 15 min intervals/day spent in recreational PC use or video games (school dismissal–6 pm) |
5 |
| TV/Video Watching – Child Report |
After School Time Use Interview using a guided recall format to elicit information from the child about weekday afternoons. Scaled # of 15 min intervals/day watching TV/Videos (school dismissal–6 pm) |
5 |
| BMI (raw) |
Body Mass Index weight (kilograms)/ height (metres)2 calculated using a programme from the Centers for Disease Control and Prevention from direct measurement of height and weight |
5, 6, 7, 8 |
Data analysis
Descriptive characteristics of the sample were calculated using frequencies and means ± standard deviation (SD). In the first analysis, growth mixture modelling analysis was used to determine distinct trajectories of raw BMI from Grade 5 to Grade 8. For the growth mixture analysis, the best fit was the model with the lower Akaike Information Criteria (AIC) and Bayesian Information Criteria (BIC), entropy closer to 1 and a significant P value for the Vuong–Lo–Mendell–Rubin Likelihood Ratio Test (LRT) and the Lo–Mendell–Rubin Adjusted LRT. These two tests were used to compare the fit of 1 vs. 2 and 2 vs. 3 distinct trajectories 33.
In the second analysis, a mixture modelling approach was used to determine the unique obesogenic behavioural clusters at Grade 5 of the adolescents with the distinct BMI trajectories. For the mixture modelling, the best fit was the model with the lower AIC and BIC, entropy closer to 1 and a significant P value for the Vuong–Lo–Mendell–Rubin LRT and Lo–Mendell–Rubin Adjusted LRT 33. These two tests were used to compare the fit of 1 vs. 2 and 2 vs. 3 behavioural clusters. All mixture modelling analysis was performed using MPlus 6.12 33.
In the final analyses, independent t‐test analysis was used to determine which variables differed significantly between identified behavioural clusters. As appropriate, the Tukey's HSD post‐hoc test was used. The Levene's Test of Equal Variances was used when considering the significance of the results. The independent samples t‐test and frequencies were analysed using SPSS 34.
The sample size estimate needed for a 95% confidence level (5% margin of error) is 643 35. The sample size estimate for five predictor variables with a small effect size (0.02), and 0.8 power at alpha = 0.01 is 643 36. The sample size of 1006 for this study exceeds these estimates.
Results
Demographic characteristics
Table 2 describes demographic characteristics of the sample.
Table 2.
Demographic characteristics of the sample at Grade 5
| Characteristics | Percentage or mean (range) ± SD (n = 1006) |
|---|---|
| Gender (%) | |
| Girl | 50.7 |
| Boy | 49.3 |
| Race/ethnicity (%) | |
| American Indian. Eskimo, Aleutian | 0.3 |
| Asian or Pacific Islander | 1.2 |
| Black or Afro‐American | 12.6 |
| White | 81.1 |
| Other | 4.8 |
| Hispanic (%) | 6.0 |
| Non‐Hispanic | 94.0 |
| Mother Education (years of formal education) (%) | |
| 11 years or less | 8.1 |
| 12–16 years | 76.5 |
| 17 years or more | 15.5 |
| Income to Needs Ratio (income/poverty threshold) (mean ± SD) | 4.4 (0.1–27.8) ± 3.9 |
Distinct BMI trajectories
Growth mixture modelling analysis was used to identify distinct BMI trajectories from Grade 5 to Grade 8. The best fit from the growth mixture modelling analysis was for two distinct BMI trajectories (AIC = 14,253.5, BIC = 14,312.5, entropy = 0.896, Vuong–Lo–Mendell–Rubin Likelihood Ration Test P = 0.0059, and Lo–Mendell–Rubin Adjusted Likelihood Ration Test P = 0.0071; the P value for one more distinct trajectory was not significant).
Table 3 is the demographic characteristics and the mean BMI for Grade 5, Grade 6, Grade 7 and Grade 8 of the two distinct BMI trajectories. The mean BMI for the first distinct BMI trajectory is within the overweight–obese classification (≥85th percentile) based on gender and age specific growth charts 2 considering the average age at Grade 5, 6, 7 and 8. The mean BMI for the second distinct BMI trajectory is within the healthy weight classification (5th–84th percentile) based on gender and age specific growth charts 2 considering the average age for Grade 5, 6, 7 and 8. These trajectories will be referred to as the Overweight–Obese BMI trajectory and the Healthy Weight BMI trajectory, respectively.
Table 3.
Demographic and behavioural characteristics of adolescents with the two distinct BMI trajectories
| Characteristics | Percentage or mean (range, SD) | |
|---|---|---|
| Overweight–Obese BMI trajectory (n = 115) | Healthy weight BMI trajectory (n = 814) | |
| Gender % | ||
| Girl | 48 | 51.1 |
| Boy | 52 | 48.9 |
| Race/ethnicity % | ||
| American Indian. Eskimo, Aleutian | 0 | 0.3 |
| Asian or Pacific Islander | 0.8 | 1.2 |
| Black or Afro‐American | 19.5 | 11.7 |
| White | 71.5 | 82.4 |
| Other | 8.1 | 4.3 |
| Hispanic% | 92.7 | 94.2 |
| Non‐Hispanic | 7.3 | 5.8 |
| Mother's Education | 13.7, 7.0–18.0, 2.2 | 14.5, 7.0–21.0, 2.4 |
| Income‐to‐needs ratio | 2.7 (0.1 – 15.3, 2.2) | 4.69 (0.1 – 27.8, 4.0) |
| BMI (average age in months, years) | 2.4 | 2.4 |
| Grade 5 (132 months, 11.04 years) | 29.5 (20.1 – 53.1, 4.2) | 18.7 (13.6 – 29.3, 2.9) |
| Grade 6 (143 months, 11.9 years) | 31.0 (25.8 – 49.8, 3.7) | 19.4 (11.6 – 28.2, 3.0) |
| Grade 7 (151 months, 12.6 years) | 32.2 (26.8 – 46.3, 3.8) | 19.9 (13.6 – 28.4, 3.0) |
| Grade 8 (163 months, 13.6 years) | 32.9 (22.7 – 51.4, 4.5) | 20.6 (13.5 – 33.8, 3.1) |
| Physical Activity: Monitor (average minutes/day of moderate to vigorous physical activity) | 109.4, 3.6 | 124.7, 1.5 |
| Physical Activity: Child Report (number of 15 min intervals/day of physical activity, school dismissal–6 pm) | 1.4, 0.2 | 1.9, 0.09 |
| Physical Activity: Parent Report of Sports Participation (number of 15 min intervals/day of physical activity, school dismissal–6 pm) | 1.5, 0.15 | 1.9, 0.06 |
| TV/Video watching Time (number of 15 min intervals/day watching TV/videos, school dismissal–6 pm) | 2.5, 0.2 | 1.9, 0.09 |
| PC Recreational Use (number of 15 min intervals/day in recreational PC use/video games, school dismissal–6 pm) | 1.3, 0.2 | 0.8, 0.06 |
A chi‐square test for BMI trajectory group differences (Table 4) showed that the prevalence of males and females did not differ. A higher prevalence of whites had Healthy Weight BMI trajectory than the Overweight–Obese BMI trajectory. A higher prevalence of Blacks or Afro‐Americans had the Overweight–Obese BMI trajectory than the Healthy Weight BMI trajectory; however, the prevalence of Hispanics did not differ. Mothers of adolescents with the Healthy Weight BMI trajectory had more education than those with the Overweight–Obese BMI trajectory. Results also showed a lower income‐to‐needs ratio in adolescents with the Overweight–Obese BMI trajectory than those with the Healthy Weight BMI trajectory.
Table 4.
Differences between adolescents with overweight–obese BMI trajectory and adolescents with healthy weight BMI trajectory
| Variable (Grade 5) | Test statistic | Significance |
|---|---|---|
| Gender | χ2 (1, n = 1,006) = .417 | P = 0.518 |
| Race: Blacks/Afro‐Americans | χ2 (1, n = 1,006) = 6.027 | P = 0.014* |
| Race: Hispanics | χ2 (1, n = 1,006) = .457 | P = 0.499 |
| Mothers Education | t(1004) = −3.415 | P = 0.001* |
| Income‐to‐needs ratio | t(957) = −5238 | P < 0.001* |
| Physical Activity: Monitor | t(818) = −3.564 | P < 0.001* |
| Physical Activity: Child Report | t(169) = −2.586 | P = 0.01* |
| Physical Activity: Parent Report of Sports Participation | t(844) = −2.600 | P = 0.009* |
| TV/Video watching Time | t(913) = 1.960 | P = 0.05 |
| PC Recreational Use | t(129) = 1.752 | P = 0.082 |
Significant at P < 0.05.
For three measures of physical activity (measured by accelerometer, child report and parent report of sports participation), adolescents with the Overweight–Obese BMI trajectory showed less physical activity than adolescents with the Healthy Weight BMI trajectory. For both measures of sedentary behaviour (child reported after school time television watching and using a computer for recreational use), adolescents with the Overweight–Obese BMI trajectory and the Healthy Weight BMI did not differ significantly. Figure 1 includes a summary of these differences.
Figure 1.
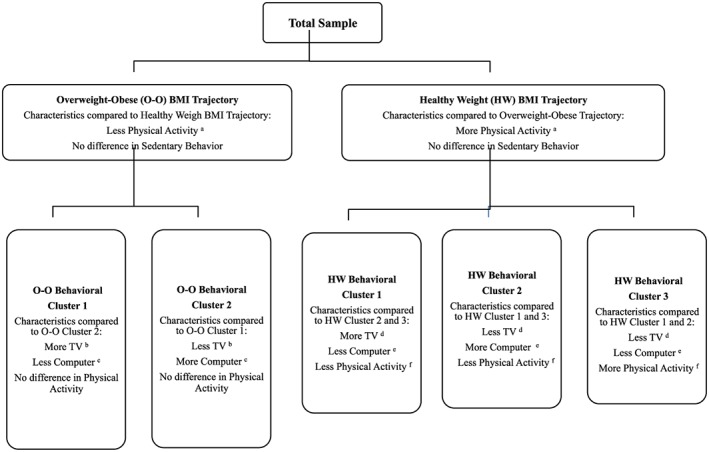
Characteristics of the behavioural clusters of adolescents with an Overweight–Obese BMI trajectory and Healthy Weight BMI trajectory. Notes:a mean of 109.41 min/day of moderate to vigorous physical activity (O–O Trajectory) compared to 124.69 min (HW Trajectory) (significant difference); mean of 1.38 15 min intervals of activity after school (O–O Trajectory) compared to 1.95 15 min intervals (HW Trajectory) (significant difference); and mean of 1.49 sports teams (O‐O Trajectory) compared to 1.92 sports teams (HW Trajectory) (significant difference), bmean of 2.62 15 min intervals of TV watching after school (O–O Cluster 1) compared to 0.34 15 min intervals (O–O Cluster 2), cmean of 0.68 15 min intervals of computer use after school (O–O Cluster 1) compared to 8.95 15 min intervals (O–O Cluster 2), dmean of 2.41 15 min intervals of TV watching after school (HW Cluster 1) compared to 0.84 15 min intervals (HW Cluster 3) (HW Cluster 1 is significantly different from HW Cluster 2 and 3, but HW Cluster 2 and 3 are not significantly different from each other), emean of 5.86 15 min intervals of computer use after school (HW Cluster 2) compared to 0.20 15 min intervals (HW Cluster 3) (HW Cluster 2 is significantly different from HW Cluster 1 and 3, but HW Cluster 1 and 3 are not significantly different from each other), fmean of 121.91 min/day of moderate to vigorous physical activity (HW Cluster 1) compared to 133.23 min/day (HW Cluster 3) (significant); mean of 0.65 15 min intervals of physical activity after school (HW Cluster 1) compared to 0.80 15 min intervals (HW Cluster 2) compared to 6.35 15 min intervals (HW Cluster 3) (HW Cluster 3 is significantly different from HW Cluster 1 and 2, but HW Cluster 1 and 2 are not significantly different from each other).
Behavioural clusters: adolescents with the Overweight–Obese BMI trajectory
Mixture modelling analysis was used to identify clusters of behaviour within adolescents with the Overweight–Obese BMI trajectory. The best fit from the mixture modelling analysis was for two behavioural clusters (AIC = 2860.1, BIC = 2905.1, entrophy = 0.970, Vuong–Lo–Mendell–Rubin Likelihood Ration Test P < 0.001 and Lo–Mendell–Rubin Adjusted Likelihood Ration Test P < 0.00; the P value for one more behavioural cluster was not significant).
An independent samples t‐test for group differences showed that Behavioural Cluster 1 in adolescents with the Overweight–Obese BMI trajectory spent more time watching television (M = 2.61, SE = 0.256) than Behaviour Cluster 2 (M = 0.34, SE = 0.229). This difference was significant t(32) = 6.618, P = 0.002. An independent samples t‐test for group differences showed that Behavioural Cluster 1 in adolescents with the Overweight–Obese BMI trajectory spent less time using a computer for recreational use (M = 0.681, SE = 0.121) than Behavioural Cluster 2 (M = 8.94, SE = 0.697). This difference was significant t(7.4) = −11.68, P < 0.001. Behavioural Cluster 1 and 2 in adolescents with the Overweight–Obese BMI trajectory did not differ significantly in monitored, child reported or parent reported physical activity. At Grade 5, 6, 7 and 8 the mean BMIs for Behavioural Clusters 1 and 2 also did not differ significantly. Figure 1 includes a summary of these behavioural clusters and a profile of the means of specific obesogenic behaviours.
Behavioural clusters: adolescents with the healthy weight BMI trajectory
Mixture modelling analysis was also used to identify clusters of behaviour for adolescents with the Healthy Weight BMI trajectory. The best fit from the mixture modelling analysis was for three behavioural clusters (AIC = 20,075.7, BIC = 20,180.7, entrophy = 0.871, Vuong–Lo–Mendell–Rubin Likelihood Ration Test P < 0.001 and Lo–Mendell–Rubin Adjusted Likelihood Ration Test P < 0.001; the P value for one more behavioural cluster was not significant).
The three behavioural clusters in adolescents with the Healthy Weight BMI trajectory differed significantly in their physical activity measured by accelerometer and child report. The three behavioural clusters did not differ in physical activity as measured by sports participation. According to Tukey's HSD post‐hoc test, Behavioural Cluster 1 was less physically active than Behavioural Cluster 3 (mean difference = −11.32, SE = 3.80, P = 0.008), Behavioural Cluster 1 was less physically active than Behavioural Cluster 3 as measured by child report (mean difference = −5.47, SE = 0.115, P < 0.001) and Behaviour Cluster 2 was less physically active than Behavioural Cluster 3 as measured by child report (mean difference = −5.56, SE = 0.185, P < 0.001).
The three behavioural patterns in adolescents with the Healthy Weight BMI trajectory also differed significantly in their sedentary behaviours as measured by time watching television and time using a computer for recreation. According to Tukey's HSD post‐hoc test, Behavioural Cluster 1 spent more time watching television than Behavioural Cluster 2 and Behavioural Cluster 3 as measured by child report (mean difference = 1.244, SE = 0.311, P < 0.001; mean difference = 1.581, SE = 0.214, P < 0.001), Behavioural Cluster 1 spent less time using a computer for recreation than Behavioural Cluster 2 as measured by child report (mean difference = −5.474, SE = 0.115, P < 0.001) and Behavioural Cluster 2 spent more time using a computer for recreation than Behavioural Cluster 3 as measured by child report (mean difference = −5.474, SE = 0.115, P < 0.001). Figure 1 includes a summary of these behavioural clusters.
Discussion
In the exploratory analysis used in this study, participants were not assigned to a group based on pre‐determined criteria. Group membership is determined by the distinct BMI trajectories and behavioural patterns that emerge from the data. The results show two distinct BMI trajectories – one with a higher mean BMI (Overweight–Obese BMI trajectory) and the other with a lower mean BMI (Healthy Weight BMI trajectory).
Adolescents in the BMI trajectory group with a mean BMI classified as Overweight–Obese were less physically active than those in the BMI trajectory group with a mean BMI classified as healthy weight. This finding is expected and consistent with the literature 4, 5, 8, 19.
Adolescents with an Overweight–Obese BMI trajectory and adolescents with a Healthy Weight BMI trajectory, however, did not differ in the time spent in sedentary screen time behaviour. Current studies indicate that adolescents with more sedentary behaviour are at a greater risk for obesity 4, 7, 19, 37, 38. The results of this study do not contradict sedentary behaviour as a risk factor, given that this study's aim was not to identify risk factors, but to identify characteristics of the subpopulations. Nonetheless, the lack of a significant difference in sedentary screen time behaviour between the group with higher mean BMI and the group with lower mean BMI is unexpected.
The emergence of obesogenic behavioural patterns within the distinct BMI trajectories begins to fill the gap in the literature. In adolescents with a BMI trajectory with a higher mean BMI, two distinct behavioural clusters were found. In one behaviour cluster, adolescents spent more sedentary time on the computer for recreational use than watching television/videos. In the other behavioural cluster, adolescents spent more sedentary time watching television/videos than on the computer. The importance of understanding types of sedentary behaviour and their potential contribution to obesity risk has been supported by several recent studies 39, 40. The behavioural clusters did not differ in the level of physical activity as measured by direct monitor, parent report of sports participation or child report.
Adolescents with a BMI trajectory with a lower mean BMI showed three distinct behavioural clusters. Overall, one of the behavioural clusters was more physically active with less sedentary screen time behaviour as compared to the others. And, two of the clusters were less physically active with more sedentary screen time behaviour as compared to the third. These behavioural clusters indicate the importance of considering physical activity and sedentary behaviour as independent targets for obesity prevention 13, 17, 18, 20, 21.
This study has several limitations. Although the study sample is diverse and shares demographic characteristics of the 1990 population, the sample is not nationally representative 28. Physical activity is reported by the child for the period after school on a weekday, and may not be representative of evening or weekend physical activity levels. The direct monitoring with the accelerometer would not capture activity during contact or water sports 27. Sample size limitations did not allow for analysis of groups stratified according to demographic characteristics. This study focuses on the behavioural clusters in early adolescence (Grade 5). The stability of these behaviour clusters over time is not well understood 24.
Conclusion
High levels of physical activity may not necessarily be associated with less sedentary behaviour in the behaviour patterns of early adolescents. In addition, different types of sedentary behaviour such as TV watching and use of electronic devices may distinguish behavioural patterns. When providing wellness education to early adolescents, it should not be assumed that those with high physical activity are also less sedentary. Wellness education related to sedentary behaviour should target screen time spent with electronic devices as well as TV/video watching.
The understanding of unique obesogenic behavioural patterns from a diverse population of children and families can inform the development of wellness promotion strategies. This exploratory study suggests that guidelines for physical activity and simple screening questions for health promotion with a narrow focus on levels of physical activity may be less than adequate given a growing understanding of multi‐dimensional obesogenic behavioural patterns. And, this study also highlights the importance of understanding types of sedentary behaviour in early adolescents as a component of wellness promotion. This contribution to better understanding of the characteristics of the target audience can be the groundwork for more meaningful messaging and engagement in wellness initiatives for early adolescents.
Funding
There was no funding support for this project.
Disclosure
No authors have any conflict of interest to disclose.
Nesbit, K. C. , Low, J. A. , and Sisson, S. B. (2016) Adolescent BMI trajectories with clusters of physical activity and sedentary behaviour: an exploratory analysis. Obesity Science & Practice, 2: 115–122. doi: 10.1002/osp4.36.
References
- 1. Ogden CL, Carroll MD, Fryar CD, Flegal, KM . Prevalence of Obesity Among Adults and Youth: United States, 2011–2014. NCHS Data Brief, no. 2019. Hyattsville, MD: National Center for Health Statistics; 2015. [PubMed] [Google Scholar]
- 2. Kuczmarski R, Flegal K. Criteria for definition of overweight in transition: background and recommendations for the United States. Am J Clin Nutr. 2000; 72: 1074–81. [DOI] [PubMed] [Google Scholar]
- 3. Kahn J, Juang B, Gillman M. Patterns and determinants of physical activity in US adolescents. J Adolesc Health. 2008; 42: 369–77. [DOI] [PubMed] [Google Scholar]
- 4. Nesbit K, Kolobe T, Sisson S, Ghement I. A model of environmental correlates of adolescent obesity in the United States. J Adolesc Health. 2014; 55: 394–401. [DOI] [PubMed] [Google Scholar]
- 5. Eisenmann JC, Bartee RT, Smith DT, Welk GJ, Fu Q. Combined influence of physical activity and television viewing on the risk of overweight in US youth. Int J Obes (Lond). 2008; 32: 613–8. [DOI] [PubMed] [Google Scholar]
- 6. Boone JE, Gordon‐Larsen P, Adair LS, Popkin BM. Screen time and physical activity during adolescence: longitudinal effects of obesity in young adulthood. Int J Behav Nutr Phys Act. 2007; 4: 26–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Mitchell JA, Rodriguez D, Schmitz KH, Audrain‐McGovern J. Greater screen time is associated with adolescent obesity: a longitudinal study of the BMI distribution from Ages 14 to 18. Obesity. 2013; 21: 572–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Sisson SB, Broyles ST, Baker BL, Katzmarzyk PT. Screen time, physical activity, and overweight in U.S. youth: national survey of children's health 2003. J Adolesc Health. 2010; 47: 309–11. [DOI] [PubMed] [Google Scholar]
- 9. Marshall S, Biddle S, Sallis J, McKenzie T, Conway T. Clustering of sedentary behaviors and physical activity among youth: a cross‐national study. Ped Exer Sci. 2002; 14: 401–17. [Google Scholar]
- 10. Melkevik O, Torsheim T, Iannotti RJ, Wold B. Is spending time in screen‐based sedentary behaviors associated with less physical activity: a cross national investigation. Int J Behav Nutr Phys Act. 2010; 7: 46–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. te Velde SJ, De Bourdeaudhuij I, Thorsdottir I, Rasmussen M, Hagstromer M, Klepp KI, et al. Patterns in sedentary and exercise behaviors and associations with overweight in 9–14‐year‐old boys and girls—a cross‐sectional study. BMC Public Health. 2007; 7: 16–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Pate RR, O'Neill JR, Lobelo F. The evolving definition of “sedentary”. Exerc Sport Sci Rev. 2008; 36: 173–8. [DOI] [PubMed] [Google Scholar]
- 13. Boone‐Heinonen J, Gordon‐Larsen P, Adair LS. Obesogenic clusters: multidimensional adolescent obesity‐related behaviors in the U.S. Ann Behav Med. 2008; 36: 217–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Burton NW, Khan A, Brown WJ, Turrell G. The association between sedentary leisure and physical activity in middle‐aged adults. Br J Sports Med. 2012; 46: 747–52. [DOI] [PubMed] [Google Scholar]
- 15. Melkevik O, Torsheim T, Rasmussen M. Patterns of screen‐based sedentary behavior and physical activity and associations with overweight among Norwegian adolescents: a latent profile approach. Norsk Epidemiologi. 2010; 20: 109–17. [Google Scholar]
- 16. Owen N, Leslie E, Salmon J, Fotheringham M. Environmental determinants of physical activity and sedentary behavior. Exerc Sport Sci Rev. 2000; 28: 153–8. [PubMed] [Google Scholar]
- 17. Beets M, Foley J. Comparison of 3 different analytic approaches for determining risk‐related active and sedentary behavioral patterns in adolescents. J Phys Act Health. 2010; 7: 381–92. [DOI] [PubMed] [Google Scholar]
- 18. Jago R, Fox KR, Page AS, Brockman R, Thompson JL. Physical activity and sedentary behaviour typologies of 10–11 year olds. Int J Behav Nutr Phys Act. 2010; 7: 59–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Liu J, Kim J, Colabianchi N, Ortaglia A, Pate R. Co‐varying patterns of physical activity and sedentary behaviors and their long‐term maintenance among adolescents. J Phys Act Health. 2010; 7: 465–74. [DOI] [PubMed] [Google Scholar]
- 20. Patnode C, Lytle L, Erickson D, Sirand J, CBarr‐Anderson D, Story M. Physical activity and sedentary activity patterns among children and adolescents a latent class analysis approach. J Phys Act Health. 2011; 8: 457–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Zabinski M, Norman G, Sallis J, Calfas K. Patterns of sedentary behavior among adolescents. Health Psychol. 2007; 26: 113–20. [DOI] [PubMed] [Google Scholar]
- 22. Wen X, Kleinman K, Gillman MW, Rifas‐Shiman SL, Taveras EM. Childhood body mass index trajectories: modeling, characterizing, pairwise correlations and socio‐demographic predictors of trajectory characteristics. BMC Med Res Methodol. 2012; 12: 38–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Attard SM, Herring AH, Howard AG, Gordon‐Larsen P. Longitudinal trajectories of BMI and cardiovascular disease risk: the national longitudinal study of adolescent health. Obesity. 2013; 21: 2180–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Monda K, Popkin B. Cluster analysis methods help to clarify the activity – BMI relationship of Chinese youth. Obes Res. 2005; 13: 1042–61. [DOI] [PubMed] [Google Scholar]
- 25. Leech RM, McNaughton SA, Timperio A. The clustering of diet, physical activity, sedentary behavior in children and adolescents: a review. Int J Behav Nutr Phys Act. 2014; 11: 4–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ram N, Grimm K. Growth mixture modeling: a method for identifying differences in longitudinal change among unobserved groups. Int J Behav Dev. 2009; 33: 565–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. National Institute of Child Health and Human Development Study of Early Child Care and Youth Development. 2012. Accessed July 15, 2013.
- 28. Bradley R, McRitchie S, Houts R, Nader P, O'Brien BC. Parenting and the decline of physical activity from age 9 to 15. Int J Behav Nutr Phys Act. 2011; 8: 33–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. United States Census Bureau . 1990 US Census. 1990.
- 30. Berkey CS, Colditz GA. Adiposity in adolescents: change in actual BMI works better than change in BMI z score for longitudinal studies. Ann Epidemiol. 2007; 17: 44–50. [DOI] [PubMed] [Google Scholar]
- 31. Cole TJ, Faith MS, Pietrobelli A, Heo M. What is the best measure of adiposity change in growing children: BMI, BMI %, BMI z‐score or BMI centile? Eur J Clin Nutr. 2005; 59: 419–25. [DOI] [PubMed] [Google Scholar]
- 32. Must A, Anderson SE. Body mass index in children and adolescents: considerations for population‐based applications. Int J Obes. 2006; 30: 590–4. [DOI] [PubMed] [Google Scholar]
- 33. Muthen, Muthen . MPLUS. 6.11 ed. Los Angeles, CA, 2011.
- 34. IBM . SPSS Statistics. 21 ed: IBM Corporation; 2012.
- 35. Raosoft I. Sample Size Calculator. http://www.raosoft.com/samplesize.html. Accessed November 3, 2014.
- 36. DanielSoper.com. Statistics calculators. http://www.danielsoper.com/statcalc/. Accessed November 3, 2014.
- 37. Sisson SB, Camhi SM, Church TS, Martin CK, Tudor‐Locke C, Bouchard C, et al. Leisure time sedentary behavior, occupational/domestic physical activity, and metabolic syndrome in U.S. men and women. Metab Syndr Relat Disord. 2009; 7: 529–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Sisson SB, Church TS, Martin CK, Tudor‐Locke C, Smith SR, Bouchard C, et al. Profiles of sedentary behavior in children and adolescents: the US National Health and Nutrition Examination Survey, 2001–2006. Int J Pediatr Obes. 2009; 4: 353–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Rhodes RE, Mark RS, Temmel CP. Adult sedentary behavior: a systematic review. Am J Prev Med. 2012; 42: e3–28. [DOI] [PubMed] [Google Scholar]
- 40. Sisson SB, Broyles ST, Baker BL, Katzmarzyk PT. Television, reading and computer time: correlates of school‐day leisure‐time sedentary behavior and relationship with overweight in children in the U.S. J Phys Act Health. 2011; 8(Suppl 2): S188–S97. [PubMed] [Google Scholar]


