Abstract
Anti-bone resorptive drugs such as bisphosphonates, the anti-RANKL antibody (denosumab), or selective estrogen receptor modulators (SERMs) have been developed to treat osteoporosis. Mechanisms underlying activity of bisphosphonates or denosumab in this context are understood, while it is less clear how SERMs like tamoxifen, raloxifene, or bazedoxifene inhibit bone resorption. Recently, accumulation of hypoxia inducible factor 1 alpha (Hif1α) in osteoclasts was shown to be suppressed by estrogen in normal cells. In addition, osteoclast activation and decreased bone mass seen in estrogen-deficient conditions was found to require Hif1α. Here, we used western blot analysis of cultured osteoclast precursor cells to show that tamoxifen, raloxifene, or bazedoxifene all suppress Hif1α protein accumulation. The effects of each SERM on osteoclast differentiation differed in vitro. Our results suggest that interventions such as the SERMs evaluated here could be useful to inhibit Hif1α and osteoclast activity under estrogen-deficient conditions.
Introduction
Many developing countries show significantly increased numbers of aging individuals, resulting in a sharply increased number of osteoporosis patients and a parallel increase in the number of bone fragile fracture patients [1]. To prevent these conditions, several reagents have been developed such as either anti-bone resorptive or bone-forming drugs [2]. Among these, bisphosphonates, including alendronate and risedronate, the monoclonal antibody demosumab, and selective estrogen receptor modulators (SERMs) are anti-bone resorptive, while teriparatide is categorized as a bone-forming drug [2–4]. Mechanisms underlying bisphosphonate and denosumab activity are well-characterized [5]. For example, bisphosphonates are taken up by osteoclasts upon bone-resorption and inhibit the geranylgeranyl pathway, promoting osteoclast apoptosis [6]. By contrast, denosumab recognizes and inactivates the receptor activator of nuclear factor kappa B ligand (RANKL), blocking osteoclast differentiation and activation [7, 8].
Currently, several SERMs are being utilized clinically [3]. Tamoxifen is used as breast cancer treatment, and it inhibits osteoclast-driven bone resorption [9, 10]. The SERMs raloxifene and bazedoxifene also both reportedly inhibit bone resorptive activity in post-menopausal osteoporosis patients [3, 11–13] and have been used to prevent bone fragility fractures. Binding of SERMs to estrogen receptors (ERs) modulates the receptor’s conformation or ability to form a complex with co-regulators, which in turn, alters their transcriptional activity [14–19]. However, how SERMs inhibit bone resorption mechanistically remains unclear.
Analysis of post-menopausal development of osteoporosis indicates that ERα expressed in osteoclasts function to block osteoclast activation and bone loss [20–22]. Furthermore, our previous analysis of ovariectomized (OVX) mice indicated that hypoxia inducible factor 1 alpha (Hif1α) is required for osteoporosis development under an estrogen-deficient condition [23]. Specifically, Hif1α protein accumulation in osteoclasts was continuously suppressed by estrogen in pre-menopausal estrogen-sufficient conditions but accumulated in osteoclasts in estrogen-deficient conditions [23]. Moreover, treatment of OVX mice with a Hif1α-inhibitor completely abrogated estrogen deficiency-induced osteoclast activation and bone loss [23]. We have also shown that eldecalcitol, a vitamin D analogue and inhibitor of bone resorption in osteoporosis patients, functions as a Hif1α inhibitor [24]. Thus, Hif1α could serve as a therapeutic target to block osteoclast activation and bone loss under estrogen-deficient conditions.
Here, we define mechanisms underlying the anti-bone resorbing function of SERMs. To do so, we treated primary osteoclast precursor cells with SERMs in normal and estrogen-free conditions and evaluated osteoclastogenesis by multi-nuclear osteoclast formation and expression of osteoclastic genes such as Cathepsin K, nuclear factor of activated T cells 1 (NFATc1) and dendritic cell specific transmembrane protein (DC-STAMP). In addition, we assessed the effects of SERMs on Hif1α protein levels. We report that although the SERMs tamoxifen, raloxifene and bazedoxifene have varying effects on osteoclast differentiation, they all suppress Hif1α protein accumulation in osteoclasts grown under hypoxic and estrogen-free conditions. Thus, evaluation of Hif1α protein levels in osteoclasts grown under hypoxia in vitro may serve as a way to predict whether potential therapies will inhibit osteoclast bone-resorption activity in vivo.
Materials and Methods
Mice
Wild-type mice on a C57BL/6 background were purchased from Sankyo Labo Service (Tokyo, Japan). Animals were maintained under specific pathogen-free conditions and housed up to 5 mice per cage, and were kept in a 12 h light/dark cycle controlled rooms at the animal facility of the Keio University. Sterile distilled water and standard diet (CLEA Rodent Diet CE-2, Japan) was available ad libitum. Animal experiments were reviewed and approved by The Keio University Institutional Animal Care and Use Committee (Permit Number: 09092–14). Animal sacrifice was humanely performed by cervical dislocation for adult mice. This study was specifically approved by the Keio University animal care committee.
In vitro osteoclast formation
Bone marrow cells isolated from femurs and tibias were cultured for 72 h in α-MEM (Sigma-Aldrich Co.) containing 10% fetal bovine serum (FBS) (JRH Biosciences) and GlutaMax (Invitrogen Corp.) or phenol red-free media containing 10% charcoal-stripped FBS (Thermo Fisher Scientific K.K., Yokohama, Japan) supplemented with M-CSF (50 ng/mL, Kyowa Hakko Kirin Co.). After three days of culture, adherent cells were collected and cultured in 96-well plates (1 × 105 cells per well) in the presence or absence of M-CSF (50 ng/mL) and recombinant soluble RANKL (25 ng/mL, PeproTech Ltd.) with or without indicated concentrations of SERMs or estradiol (E2). The medium was replaced every 2 days. Hypoxic culture was performed at 5% O2/5% CO2 using an INVIVO2 hypoxia workstation (Ruskin Technology Ltd., Bridgend, UK) as previously described [23–26].
Osteoclastogenesis was evaluated by tartrate resistance acid phosphatase (TRAP) staining, and TRAP-positive multi-nuclear cells containing more than three nuclei were scored as osteoclasts [27].
Quantitative PCR analysis
In three independent analyses, total RNAs were extracted from bone marrow cultures using an RNeasy kit (Qiagen, Venlo, Limburg, The Netherlands). Complementary DNA (cDNA) was prepared by using oligo (dT) primers and reverse transcriptase (Wako Pure Chemicals Industries). Quantitative PCR was performed using SYBR Premix ExTaq II reagent and a DICE Thermal cycler (Takara Bio Inc.), according to the manufacturer’s instructions. β-actin expression served as an internal control. Primers for realtime PCR were:
β-actin-forward: 5’-TGAGAGGGAAATCGTGCGTGAC-3’
β-actin-reverse: 5’-AAGAAGGAAGGCTGGAAAAGAG-3’
Cathepsin K-forward: 5’-ACGGAGGCATTGACTCTGAAGATG-3’
Cathepsin K -reverse: 5’-GGAAGCACCAACGAGAGGAGAAAT-3’
NFATc1-forward: 5’-CAAGTCTCACCACAGGGCTCACTA-3’
NFATc1-reverse: 5’-GCGTGAGAGGTTCATTCTCCAAGT-3’
DC-STAMP-forward: 5’-TCCTCCATGAACAAACAGTTCCAA-3’
DC-STAMP-reverse: 5’-AGACGTGGTTTAGGAATGCAGCTC-3’
Western blot analysis
Whole cell lysates were prepared from Raw264.7 cell cultures using RIPA buffer (1% Tween 20, 0.1% SDS, 150 mM NaCl, 10 mM Tris-HCl (pH 7.4), 0.25 mM phenylmethylsulfonylfluoride, 10 μg/mL aprotinin, 10 μg/mL leupeptin, 1 mM Na3VO4, 5 mM NaF (Sigma-Aldrich Co.)). Raw264.7 cells are murine leukemic cells transformed by Abelson murine leukemia virus infection [26] that have served as models of osteoclast progenitor cells [28]. Proteins were subjected to SDS-PAGE, transferred to a PVDF membrane (EMD Millipore Corp.), and detected using anti-Hif1α (#NB100-479, 1:1000 dilution; Novus Biologicals, Littleton, CO, USA), and anti-Vinculin (#9131, 1:1000 dilution; Sigma-Aldrich Co.), as previously described [23–25].
Replication of in vitro experiments
At least three independent experiments were performed for all in vitro experiments, and representative data are shown.
Statistical analyses
Statistical analyses were performed using the unpaired two-tailed Student’s t-test (*P<0.05; **P<0.01; ***P<0.005; NS, not significant, throughout the paper). All data are shown as means ± SD.
Results
Tamoxifen inhibits osteoclast differentiation
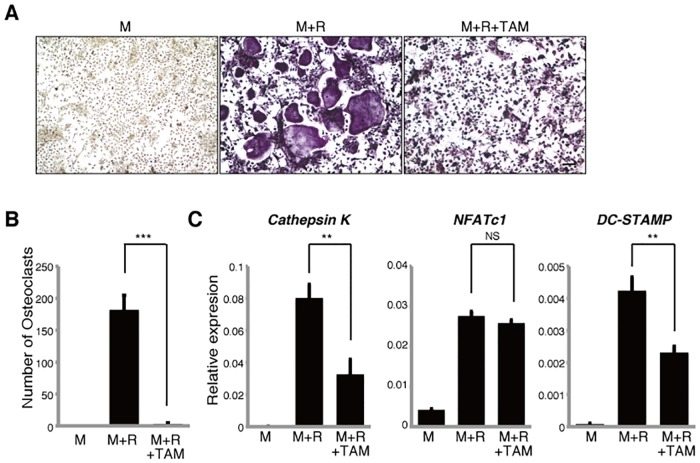
Tamoxifen reportedly inhibits osteoclast bone reorption [10]. To determine if tamoxifen can inhibit osteoclast differentiation in vitro, we isolated osteoclast progenitor cells from wild-type mice and cultured them in the presence of M-CSF and RANKL with or without tamoxifen. Osteoclastogenesis was evaluated by assessing formation of multi-nuclear TRAP-positive cells containing more than three nuclei and by expression levels of the osteoclast-related markers Cathepsin K, NFATc1 and DC-STAMP (Fig 1). Although mono-nuclear osteoclasts were formed in the presence of tamoxifen, tamoxifen treatment significantly inhibited multi-nuclear osteoclast formation induced by M-CSF and RANKL (Fig 1A and 1B) as well as Cathepsin K and DC-STAMP expression compared with untreated cells (Fig 1C), suggesting that tamoxifen inhibits osteoclast differentiation.
Fig 1. Tamoxifen inhibits osteoclast differentiation in vitro.
Osteoclast progenitors from wild-type mice were cultured with or without tamoxifen (TAM, 1μM) in the presence or absence of M-CSF 50ng/ml (M) and RANKL 25ng/ml (R). Osteoclast formation was evaluated by TRAP staining (A), by the number of multi-nuclear TRAP-positive cells (B) and by Cathepsin K, NFATc1, DC-STAMP expression as analyzed by realtime PCR (C). Data represent mean Cathepsin K, NFATc1 or DC-STAMP expression relative to β-actin ± SD (n = 3). Bar = 100 μm. **P<0.01; ***P<0.001; NS, not significant (unpaired two-tailed Student’s t-test). Representative data of at least three independent experiments are shown.
Other SERMs have varying effects on osteoclast differentiation
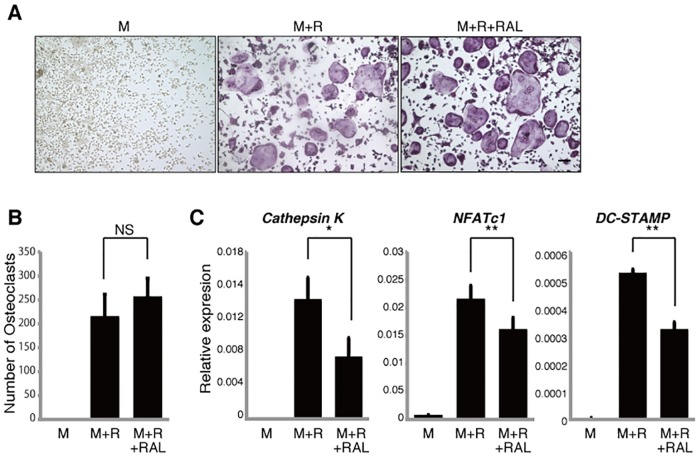
To determine whether other SERMs have effects comparable to tamoxifen, we first evaluated the effect of raloxifene on differentiation of cultured osteoclast progenitors. Unlike tamoxifen effects, formation of multi-nuclear TRAP-positive osteoclasts was not inhibited by raloxifene (Fig 2A and 2B). Raloxifene treatment did, however, inhibit expression of osteoclastic genes such as Cathepsin K, NFATc1 and DC-STAMP in osteoclasts (Fig 2C).
Fig 2. Raloxifene inhibits osteoclastic gene expression in vitro.
Osteoclast progenitors from wild-type mice were cultured with or without raloxifene (RAL, 1μM) in the presence or absence of M-CSF 50ng/ml (M) and RANKL 25ng/ml (R). Osteoclast formation was evaluated by TRAP staining (A), by the number of multi-nuclear TRAP-positive cells (B) and by Cathepsin K, NFATc1, DC-STAMP expression as analyzed by realtime PCR (C). Data represent mean Cathepsin K, NFATc1 or DC-STAMP expression relative to β-actin ± SD (n = 3). Bar = 100 μm. *P<0.05; **P<0.01; NS, not significant (unpaired two-tailed Student’s t-test). Representative data of at least three independent experiments are shown.
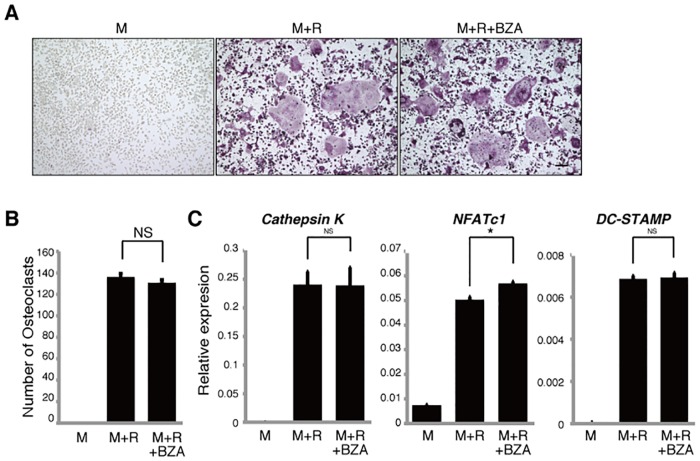
We then performed similar tests in osteoclast precursors using the SERM bazedoxifene and found that neither multi-nuclear TRAP-positive osteoclast formation nor osteoclastic gene expression was suppressed (Fig 3A–3C), although bazedoxifene has been shown to inhibit osteoclast bone resorption in post-menopausal osteoporosis patients [29, 30].
Fig 3. Bazedoxifene does not inhibit osteoclastogenesis in vitro.
Osteoclast progenitors from wild-type mice were cultured with or without bazedoxifene (BZA, 1μM) in the presence or absence of M-CSF 50ng/ml (M) and RANKL 25ng/ml (R). Osteoclast formation was evaluated by TRAP staining (A), by the number of multi-nuclear TRAP-positive cells (B) and by Cathepsin K, NFATc1, DC-STAMP expression as analyzed by realtime PCR (C). Data represent mean Cathepsin K, NFATc1 or DC-STAMP expression relative to β-actin ± SD (n = 3). Bar = 100 μm. *P<0.05; NS, not significant (unpaired two-tailed Student’s t-test). Representative data of at least three independent experiments are shown.
SERMs have varying effects on differentiation of osteoclasts cultured in estrogen-free conditions
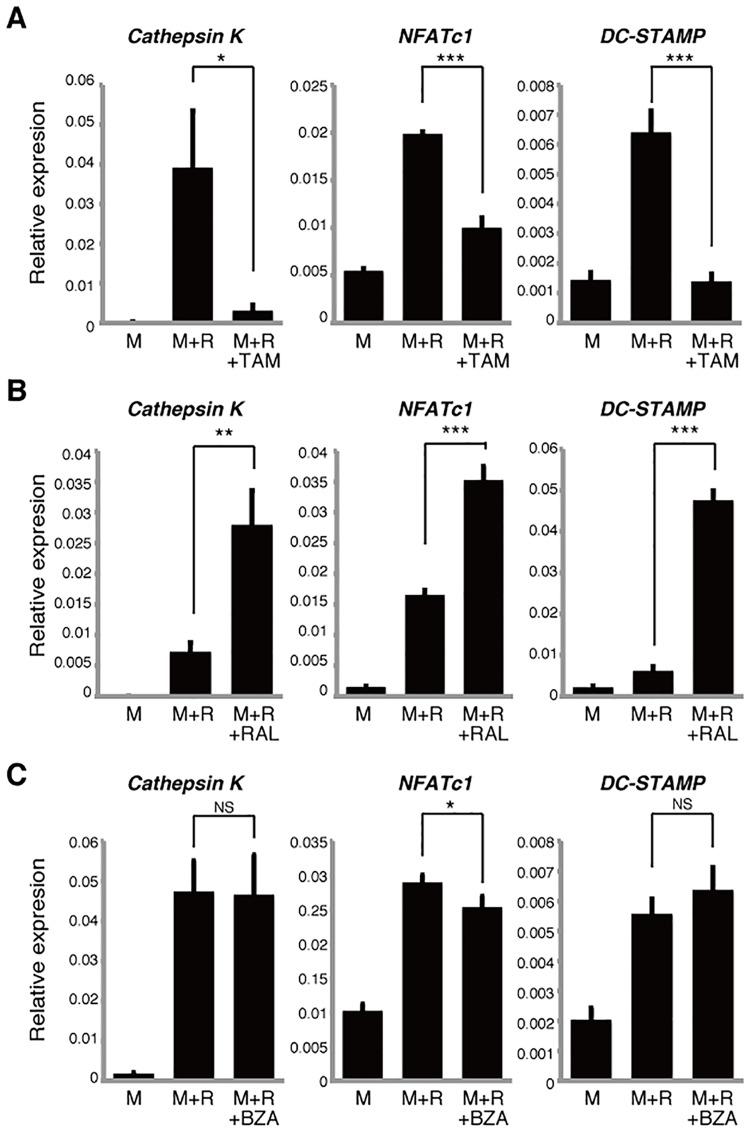
SERMs reportedly act via both ERα-dependent and -independent mechanisms [14, 16]. The presence of phenol red in culture media reportedly promotes estrogenic effects in several cell types; likewise, fetal bovine serum contains estrogen [23]. Thus to assess activity of tamoxifen, raloxifene or bazedoxifene in estrogen-free osteoclast culture conditions, we utilized phenol red-free media and estrogen-depleted serum (Fig 4). Since osteoclast formation promoted by M-CSF and RANKL is strongly inhibited in estrogen-free relative to normal culture conditions, we evaluated osteoclast differentiation based on osteoclastic gene expression rather than multi-nuclear TRAP-positive cell formation. Expression of Cathepsin K, NFATc1 and DC-STAMP was significantly inhibited by tamoxifen in estrogen-free conditions (Fig 4A), although NFATc1 expression was not significantly changed by tamoxifen treatment in normal culture conditions (Fig 1C). Raloxifene treatment significantly elevated Cathepsin K, NFATc1 and DC-STAMP expression in osteoclasts grown in estrogen-depleted conditions (Fig 4B), although all three genes had been significantly inhibited in normal culture by comparable treatment (Fig 2C). Moreover, NFATc1 expression was significantly inhibited by bazedoxifene in estrogen free-conditions (Fig 4C), although expression of NFATc1 is upregulated by comparable treatment in normal culture conditions (Fig 3C). Overall, despite these variations, the effects of SERMs on osteoclast differentiation in estrogen-free conditions differed from those seen in normal culture conditions.
Fig 4. SERM effects on osteoclastogenesis vary in estrogen-free culture conditions.
Osteoclast progenitors from wild-type mice were cultured with tamoxifen (TAM, 1μM) (A), raloxifene (RAL, 1μM) (B) or bazedoxifene (BZA, 1μM) (C) in the presence or absence of M-CSF 50ng/ml (M) and RANKL 25ng/ml (R) in phenol red-free medium. Cathepsin K, NFATc1 and DC-STAMP expression as analyzed by realtime PCR. Data represent mean Cathepsin K, NFATc1 or DC-STAMP expression relative to β-actin ± SD (n = 3). *P<0.05; **P<0.01; ***P<0.001; NS, not significant (unpaired two-tailed Student’s t-test). Representative data of at least three independent experiments are shown.
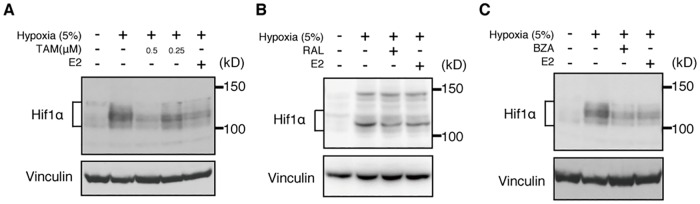
Hif1α protein levels in osteoclasts are suppressed by SERMs
Finally, given that Hif1α protein is reportedly a target of estrogen [23], we asked whether Hif1α protein levels in osteoclasts decrease following SERM treatment (Fig 5). To do so, we cultured Raw264.7 osteoclast progenitor cells in the presence of RANKL with or without SERMs in normoxic or hypoxic conditions, and evaluated Hif1α protein levels by western blots (Fig 5A–5C). We did not detect Hif1α protein in normoxic conditions, but Hif1α protein accumulated in hypoxic conditions, and that accumulation was suppressed by treatment with tamoxifen, raloxifene or bazedoxifene or by estrogen (E2) (Fig 5A–5C).
Fig 5. Hif1α protein accumulation is suppressed by SERMs.
Western blot analysis of Raw264.7 cells cultured in hypoxic conditions with or without tamoxifen (TAM, 0.5μM, 0.25μM) (A), raloxifene (RAL, 1μM) (B), or bazedoxifene (BZA, 1μM) (C) or estradiol (E2, 1μM). Vinculin expression serves as an internal control. In all panels, –(minus) symbols in the hypoxia row indicate normoxic conditions. Representative data of at least three independent experiments are shown.
Discussion
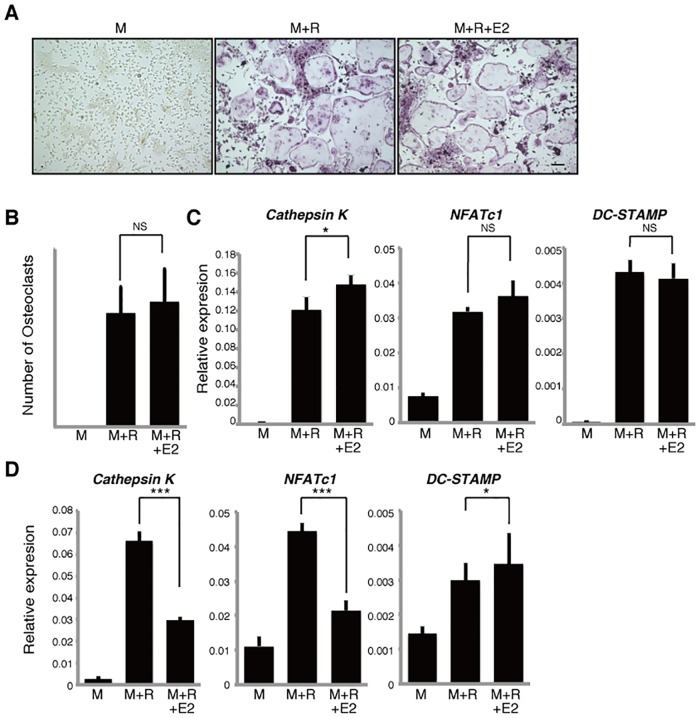
Prevention of bone fragility fractures and control of osteoporosis are global health issues in developed countries. To date, most reagents used to prevent bone fragility fractures in osteoporosis patients are anti-bone resorptive (among them SERMs), although a few activate bone formation. Mechanisms underlying SERM activity in this context remain unclear. Under sex hormone-depleted conditions, Hif1α was demonstrated to be a therapeutic target in conditions of post-menopausal [23] and male [25] osteoporosis. SERM treatment also inhibits osteoclast bone resorption in post-menopausal osteoporosis patients [9, 11, 13, 31]. To date, there has been no definitive mechanistic explanation for why SERMs act as anti-bone resorptive agents. Our finding that SERM treatment blocks Hif1α accumulation provides a possible explanation for this outcome. Our observations also imply that the fact that the effects of any drugs on osteoclast differentiation in vitro is not sufficient to suggest that that drug would have anti-bone resorptive effects in vivo or in patients, as the three drugs tested here had different effects on in vitro osteoclastogenesis, although all of the SERMs tested were reportedly acting as inhibitors of osteoclast bone resorption [3, 4, 9, 11, 13], but all blocked Hif1α accumulation in osteoclasts. More studies are required to determine whether tamoxifen alters activities other than Hif1α protein suppression in osteoclasts. Moreover, the effects of SERMs on osteoclastic gene expression differed in normal and estrogen-free conditions, an outcome that we cannot yet explain. However, in normal conditions, following addition of estradiol to cultures of osteoclast precursors, we found that only Cathepsin K, but not NFATc1 and DC-STAMP, expression was upregulated in osteoclasts and multi-nuclear osteoclast formation was not accelerated (Fig 6A–6C). By contrast, in estrogen-free conditions Cathepsin K and NFATc1 expression was significantly inhibited by estradiol (Fig 6D). Thus, none of the SERMs tested here recapitulate the effects of estradiol in vitro in terms of osteoclastic gene expression. Since estradiol reportedly suppresses Hif1α protein accumulation in osteoclasts grown in hypoxic, estrogen-free conditions [23], suppression of Hif1α protein in osteoclasts is an activity shared by both SERMs and estradiol in vitro.
Fig 6. Effects of estradiol on osteoclastogenesis in normal and estrogen-free conditions.
Osteoclast progenitors from wild-type mice were cultured with or without estradiol (E2, 1μM) in the presence or absence of M-CSF 50ng/ml (M) and RANKL 25ng/ml (R). Osteoclast formation was evaluated by TRAP staining (A), by the number of multi-nuclear TRAP-positive cells (B) and by Cathepsin K, NFATc1, DC-STAMP expression as analyzed by realtime PCR in normal (C) or estrogen-free (D) medium. Data represent mean Cathepsin K, NFATc1 or DC-STAMP expression relative to β-actin ± SD (n = 3). Bar = 100 μm. *P<0.05; ***P<0.001; NS, not significant (unpaired two-tailed Student’s t-test). Representative data of at least three independent experiments are shown.
Since post-menopausal, estrogen-deficient conditions promote osteoclast activation leading to bone loss, estrogen administration is considered a means to reverse these conditions. Indeed, hormone replacement therapy (HRT) increases bone mass in post-menopausal osteoporosis patients, although treatment can have adverse effects [32]. Other agents such as bisphosphonates and denosumab can block osteoclastic bone resorption in osteoporosis patients, but these, too, can have adverse effects such as osteonecrosis of the jaws (ONJ) and severely suppressed bone turnover (SSBT) [33–35]. Comparable adverse effects have not been reported in patients treated with SERMs [3, 31]. However, SERMs have been found to be less effective in inhibiting osteoclastic bone resorption than bisphosphonates [4, 36]. This observation may support the idea that SERMs are Hif1α inhibitors, since treatment of normal mice with Hif1α inhibitors does not block physiological osteoclast activity in estrogen- or testosterone-sufficient conditions [23, 25]. In contrast, administration of bisphosphonates or an anti-RANKL antibody to comparable, hormone-sufficient mice strongly inhibits physiological osteoclast activity, increasing bone mass [37].
Unlike individuals treated with bisphosphonates or denosumab, patients treated with HRT and SERMs can exhibit thrombosis development in deep veins [38–40], although the cause of these complications remains unclear. ERα is reportedly required to suppress Hif1α protein in osteoclasts [23], while SERMs are thought to act via ERα-dependent or independent mechanism [14–16]. Hif1α has also been considered a therapeutic target in some malignancies [41]. Tamoxifen and raloxifene are effective in inhibiting tumor burden in some breast cancers, while HRT promotes tumor development [42]. Further studies are needed to clarify molecular mechanisms underlying thrombosis and tumor development by HRT and SERMs.
Estrogen also inhibits osteoclast activation indirectly via osteoblasts [43–45]. Moreover, osteoclast-specific ERα conditional knockout (ERα cKO) mice exhibit reduced bone mass relative to controls, and OVX does not decrease bone mass in ERα cKO mice [20], suggesting that ERα expressed in osteoclasts plays a crucial role in regulating bone mass.
We previously demonstrated that Hif1α could be a therapeutic target in osteoporosis [23], leading us to test the effects of candidate anti-bone resorptive agents on Hif1α protein suppression in osteoclasts in vitro. Eldecalcitol, which is used to inhibit bone resorption in osteoporosis patients [46], lowers Hif1α protein levels in osteoclasts [24], comparable to our observation following SERM treatment. To date, anti-osteoporosis agents have been tested in animal models such as OVX mice in vivo, but this system does not allow efficient testing of numerous candidate agents due to costs and time frame of testing. Screening in vitro for Hif1α protein suppression in osteoclasts could substitute for animal models and reduce expenses and time required to evaluate anti-bone resorbing agents.
Conclusions
SERMs act as inhibitors of Hif1α, a therapeutic target of post-menopausal osteoporosis, in osteoclasts under an estrogen-deficient condition. Testing inhibitory effects on Hif1α protein in osteoclasts in vitro is useful to screen candidate anti-bone resorptive agents before animal models.
Acknowledgments
We thank Prof. M. Suematsu and Dr. Y.A. Minamishima for technical support of hypoxic cultures.
Data Availability
All relevant data are within the paper.
Funding Statement
This study was funded by Grant-in-aid for Scientific Research in Japan and a grant from Japan Agency for Medical Research and Development. This study was also funded in part by a research grant from Chugai Scientific foundation, Pfizer Japan Inc. and Eli Lilly Scientific foundation. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Riggs BL, Melton LJ 3rd. The worldwide problem of osteoporosis: insights afforded by epidemiology. Bone. 1995;17(5 Suppl):505S–11S. . [DOI] [PubMed] [Google Scholar]
- 2.Delmas PD. Treatment of postmenopausal osteoporosis. Lancet. 2002;359(9322):2018–26. 10.1016/S0140-6736(02)08827-X . [DOI] [PubMed] [Google Scholar]
- 3.Pinkerton JV, Thomas S. Use of SERMs for treatment in postmenopausal women. J Steroid Biochem Mol Biol. 2014;142:142–54. 10.1016/j.jsbmb.2013.12.011 . [DOI] [PubMed] [Google Scholar]
- 4.Maeda SS, Lazaretti-Castro M. An overview on the treatment of postmenopausal osteoporosis. Arq Bras Endocrinol Metabol. 2014;58(2):162–71. . [DOI] [PubMed] [Google Scholar]
- 5.Mazziotti G, Bilezikian J, Canalis E, Cocchi D, Giustina A. New understanding and treatments for osteoporosis. Endocrine. 2012;41(1):58–69. 10.1007/s12020-011-9570-2 . [DOI] [PubMed] [Google Scholar]
- 6.Li B, Ling Chau JF, Wang X, Leong WF. Bisphosphonates, specific inhibitors of osteoclast function and a class of drugs for osteoporosis therapy. J Cell Biochem. 2011;112(5):1229–42. 10.1002/jcb.23049 . [DOI] [PubMed] [Google Scholar]
- 7.Kostenuik PJ, Nguyen HQ, McCabe J, Warmington KS, Kurahara C, Sun N, et al. Denosumab, a fully human monoclonal antibody to RANKL, inhibits bone resorption and increases BMD in knock-in mice that express chimeric (murine/human) RANKL. J Bone Miner Res. 2009;24(2):182–95. 10.1359/jbmr.081112 . [DOI] [PubMed] [Google Scholar]
- 8.Cummings SR, San Martin J, McClung MR, Siris ES, Eastell R, Reid IR, et al. Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N Engl J Med. 2009;361(8):756–65. 10.1056/NEJMoa0809493 . [DOI] [PubMed] [Google Scholar]
- 9.Powles TJ, Hickish T, Kanis JA, Tidy A, Ashley S. Effect of tamoxifen on bone mineral density measured by dual-energy x-ray absorptiometry in healthy premenopausal and postmenopausal women. J Clin Oncol. 1996;14(1):78–84. . [DOI] [PubMed] [Google Scholar]
- 10.Love RR, Mazess RB, Barden HS, Epstein S, Newcomb PA, Jordan VC, et al. Effects of tamoxifen on bone mineral density in postmenopausal women with breast cancer. N Engl J Med. 1992;326(13):852–6. 10.1056/NEJM199203263261302 . [DOI] [PubMed] [Google Scholar]
- 11.Ettinger B, Black DM, Mitlak BH, Knickerbocker RK, Nickelsen T, Genant HK, et al. Reduction of vertebral fracture risk in postmenopausal women with osteoporosis treated with raloxifene: results from a 3-year randomized clinical trial. Multiple Outcomes of Raloxifene Evaluation (MORE) Investigators. JAMA. 1999;282(7):637–45. . [DOI] [PubMed] [Google Scholar]
- 12.Ronkin S, Northington R, Baracat E, Nunes MG, Archer DF, Constantine G, et al. Endometrial effects of bazedoxifene acetate, a novel selective estrogen receptor modulator, in postmenopausal women. Obstet Gynecol. 2005;105(6):1397–404. 10.1097/01.AOG.0000163253.27610.b9 . [DOI] [PubMed] [Google Scholar]
- 13.Silverman SL, Christiansen C, Genant HK, Vukicevic S, Zanchetta JR, de Villiers TJ, et al. Efficacy of bazedoxifene in reducing new vertebral fracture risk in postmenopausal women with osteoporosis: results from a 3-year, randomized, placebo-, and active-controlled clinical trial. J Bone Miner Res. 2008;23(12):1923–34. 10.1359/jbmr.080710 . [DOI] [PubMed] [Google Scholar]
- 14.Zhang X, Jeyakumar M, Petukhov S, Bagchi MK. A nuclear receptor corepressor modulates transcriptional activity of antagonist-occupied steroid hormone receptor. Mol Endocrinol. 1998;12(4):513–24. 10.1210/mend.12.4.0089 . [DOI] [PubMed] [Google Scholar]
- 15.Couse JF, Korach KS. Estrogen receptor null mice: what have we learned and where will they lead us? Endocr Rev. 1999;20(3):358–417. 10.1210/edrv.20.3.0370 . [DOI] [PubMed] [Google Scholar]
- 16.Shang Y, Brown M. Molecular determinants for the tissue specificity of SERMs. Science. 2002;295(5564):2465–8. 10.1126/science.1068537 . [DOI] [PubMed] [Google Scholar]
- 17.Tsai MJ, O'Malley BW. Molecular mechanisms of action of steroid/thyroid receptor superfamily members. Annu Rev Biochem. 1994;63:451–86. 10.1146/annurev.bi.63.070194.002315 . [DOI] [PubMed] [Google Scholar]
- 18.Riggs BL, Hartmann LC. Selective estrogen-receptor modulators—mechanisms of action and application to clinical practice. N Engl J Med. 2003;348(7):618–29. 10.1056/NEJMra022219 . [DOI] [PubMed] [Google Scholar]
- 19.Martinkovich S, Shah D, Planey SL, Arnott JA. Selective estrogen receptor modulators: tissue specificity and clinical utility. Clin Interv Aging. 2014;9:1437–52. 10.2147/CIA.S66690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nakamura T, Imai Y, Matsumoto T, Sato S, Takeuchi K, Igarashi K, et al. Estrogen prevents bone loss via estrogen receptor alpha and induction of Fas ligand in osteoclasts. Cell. 2007;130(5):811–23. 10.1016/j.cell.2007.07.025 . [DOI] [PubMed] [Google Scholar]
- 21.Martin-Millan M, Almeida M, Ambrogini E, Han L, Zhao H, Weinstein RS, et al. The estrogen receptor-alpha in osteoclasts mediates the protective effects of estrogens on cancellous but not cortical bone. Mol Endocrinol. 2010;24(2):323–34. 10.1210/me.2009-0354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vanderschueren D, Laurent MR, Claessens F, Gielen E, Lagerquist MK, Vandenput L, et al. Sex steroid actions in male bone. Endocr Rev. 2014;35(6):906–60. 10.1210/er.2014-1024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Miyauchi Y, Sato Y, Kobayashi T, Yoshida S, Mori T, Kanagawa H, et al. HIF1alpha is required for osteoclast activation by estrogen deficiency in postmenopausal osteoporosis. Proc Natl Acad Sci U S A. 2013;110(41):16568–73. 10.1073/pnas.1308755110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sato Y, Miyauchi Y, Yoshida S, Morita M, Kobayashi T, Kanagawa H, et al. The vitamin D analogue ED71 but Not 1,25(OH)2D3 targets HIF1alpha protein in osteoclasts. PLoS One. 2014;9(11):e111845 10.1371/journal.pone.0111845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tando T, Sato Y, Miyamoto K, Morita M, Kobayashi T, Funayama A, et al. Hif1alpha is required for osteoclast activation and bone loss in male osteoporosis. Biochem Biophys Res Commun. 2016;470(2):391–6. 10.1016/j.bbrc.2016.01.033 . [DOI] [PubMed] [Google Scholar]
- 26.Raschke WC, Baird S, Ralph P, Nakoinz I. Functional macrophage cell lines transformed by Abelson leukemia virus. Cell. 1978;15(1):261–7. . [DOI] [PubMed] [Google Scholar]
- 27.Piper K, Boyde A, Jones SJ. The relationship between the number of nuclei of an osteoclast and its resorptive capability in vitro. Anat Embryol (Berl). 1992;186(4):291–9. . [DOI] [PubMed] [Google Scholar]
- 28.Collin-Osdoby P, Yu X, Zheng H, Osdoby P. RANKL-mediated osteoclast formation from murine RAW 264.7 cells. Methods Mol Med. 2003;80:153–66. 10.1385/1-59259-366-6:153 . [DOI] [PubMed] [Google Scholar]
- 29.Miller CP, Collini MD, Tran BD, Harris HA, Kharode YP, Marzolf JT, et al. Design, synthesis, and preclinical characterization of novel, highly selective indole estrogens. J Med Chem. 2001;44(11):1654–7. . [DOI] [PubMed] [Google Scholar]
- 30.Lello S, Brandi ML, Minisola G, Minisola S, Genazzani AR. Bazedoxifene: literature data and clinical evidence. Clin Cases Miner Bone Metab. 2011;8(3):29–32. [PMC free article] [PubMed] [Google Scholar]
- 31.Diez-Perez A. Selective estrogen receptor modulators (SERMS). Arq Bras Endocrinol Metabol. 2006;50(4):720–34. . [DOI] [PubMed] [Google Scholar]
- 32.Christiansen C, Christensen MS, Transbol I. Bone mass in postmenopausal women after withdrawal of oestrogen/gestagen replacement therapy. Lancet. 1981;1(8218):459–61. . [DOI] [PubMed] [Google Scholar]
- 33.Whyte MP, McAlister WH, Novack DV, Clements KL, Schoenecker PL, Wenkert D. Bisphosphonate-induced osteopetrosis: novel bone modeling defects, metaphyseal osteopenia, and osteosclerosis fractures after drug exposure ceases. J Bone Miner Res. 2008;23(10):1698–707. 10.1359/jbmr.080511 . [DOI] [PubMed] [Google Scholar]
- 34.Gedmintas L, Solomon DH, Kim SC. Bisphosphonates and risk of subtrochanteric, femoral shaft, and atypical femur fracture: a systematic review and meta-analysis. J Bone Miner Res. 2013;28(8):1729–37. 10.1002/jbmr.1893 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Edwards BJ, Bunta AD, Lane J, Odvina C, Rao DS, Raisch DW, et al. Bisphosphonates and nonhealing femoral fractures: analysis of the FDA Adverse Event Reporting System (FAERS) and international safety efforts: a systematic review from the Research on Adverse Drug Events And Reports (RADAR) project. J Bone Joint Surg Am. 2013;95(4):297–307. 10.2106/JBJS.K.01181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Luckey M, Kagan R, Greenspan S, Bone H, Kiel RD, Simon J, et al. Once-weekly alendronate 70 mg and raloxifene 60 mg daily in the treatment of postmenopausal osteoporosis. Menopause. 2004;11(4):405–15. . [DOI] [PubMed] [Google Scholar]
- 37.Miyamoto K, Yoshida S, Kawasumi M, Hashimoto K, Kimura T, Sato Y, et al. Osteoclasts are dispensable for hematopoietic stem cell maintenance and mobilization. J Exp Med. 2011;208(11):2175–81. 10.1084/jem.20101890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Deroo BJ, Korach KS. Estrogen receptors and human disease. J Clin Invest. 2006;116(3):561–70. 10.1172/JCI27987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Martino S, Disch D, Dowsett SA, Keech CA, Mershon JL. Safety assessment of raloxifene over eight years in a clinical trial setting. Curr Med Res Opin. 2005;21(9):1441–52. 10.1185/030079905X61839 . [DOI] [PubMed] [Google Scholar]
- 40.Layton D, Clarke A, Wilton LV, Shakir SA. Safety profile of raloxifene as used in general practice in England: results of a prescription-event monitoring study. Osteoporos Int. 2005;16(5):490–500. 10.1007/s00198-004-1710-6 . [DOI] [PubMed] [Google Scholar]
- 41.Ryan HE, Poloni M, McNulty W, Elson D, Gassmann M, Arbeit JM, et al. Hypoxia-inducible factor-1alpha is a positive factor in solid tumor growth. Cancer Res. 2000;60(15):4010–5. . [PubMed] [Google Scholar]
- 42.Li F, Dou J, Wei L, Li S, Liu J. The selective estrogen receptor modulators in breast cancer prevention. Cancer Chemother Pharmacol. 2016;77(5):895–903. 10.1007/s00280-016-2959-0 . [DOI] [PubMed] [Google Scholar]
- 43.Maatta JA, Buki KG, Gu G, Alanne MH, Vaaraniemi J, Liljenback H, et al. Inactivation of estrogen receptor alpha in bone-forming cells induces bone loss in female mice. FASEB J. 2013;27(2):478–88. 10.1096/fj.12-213587 . [DOI] [PubMed] [Google Scholar]
- 44.Almeida M, Iyer S, Martin-Millan M, Bartell SM, Han L, Ambrogini E, et al. Estrogen receptor-alpha signaling in osteoblast progenitors stimulates cortical bone accrual. J Clin Invest. 2013;123(1):394–404. 10.1172/JCI65910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Melville KM, Kelly NH, Khan SA, Schimenti JC, Ross FP, Main RP, et al. Female mice lacking estrogen receptor-alpha in osteoblasts have compromised bone mass and strength. J Bone Miner Res. 2014;29(2):370–9. 10.1002/jbmr.2082 . [DOI] [PubMed] [Google Scholar]
- 46.Matsumoto T, Ito M, Hayashi Y, Hirota T, Tanigawara Y, Sone T, et al. A new active vitamin D3 analog, eldecalcitol, prevents the risk of osteoporotic fractures—a randomized, active comparator, double-blind study. Bone. 2011;49(4):605–12. 10.1016/j.bone.2011.07.011 . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the paper.