Abstract
The chronic obstructive pulmonary disease (COPD) Assessment Test (CAT), which was developed to measure the health status of patients with COPD, was applied to patients with interstitial lung disease, aiming to examine the CAT as a predictor of outcome. Over a follow-up period of more than one year, 101 consecutive patients with interstitial lung disease were evaluated by the CAT. The CAT scores of 40 in total were categorized into four subsets according to the severity. Patients with higher (more severe) scores exhibited lower forced vital capacity and lung diffusion capacity for carbon monoxide. The survival rate was significantly lower in patients with higher scores (log-rank test, P = 0.0002), and the hazard ratios for death of the higher scores and lower lung diffusion capacity for carbon monoxide were independently significant. These findings suggest that CAT can indicate the risk of mortality in patients with interstitial lung disease.
Keywords: quality of life, mortality, pulmonary function, home oxygen therapy
Introduction
Patients with interstitial lung disease have a wide range of diagnoses and prognoses, and some can live with their diagnosis and/or are responsive to treatments.1 For example, there is moderate evidence for the use of sildenafil and pulmonary rehabilitation to improve health-related quality of life in fibrotic interstitial lung disease. Health-related quality of life in patients with interstitial lung disease is mainly evaluated by the 36-item short-form questionnaire, Chronic Respiratory Questionnaire, or St George’s Respiratory Questionnaire (SGRQ).1 New evaluation tools have also been developed specifically to assess health-related quality of life for interstitial lung disease patients, such as the ATAQ-IPF (A Tool to Assess Quality of life in IPF; idiopathic pulmonary fibrosis) that is composed of 74 items2 and the King’s Brief Interstitial Lung Disease questionnaire with 15 items.3
Quality of life in interstitial lung disease patients has been correlated with the percent of predicted forced vital capacity (FVC), forced expiratory volume in the first second, lung diffusion capacity for carbon monoxide (DLCO), the level of dyspnea, and the distance walked and oxygen saturation during the 6-minute walk test (6MWT).4–6 Moreover, walking velocity, change in oxygen saturation with walking exercise, and percent of predicted DLCO have been associated with survival in idiopathic interstitial pneumonia.7,8
Recently, the COPD Assessment Test (CAT),9 which was originally developed to evaluate the health-related quality of life in patients with COPD, was also introduced to evaluate patients with interstitial lung disease, and it was reported that there was a very strong correlation between the CAT score and the SGRQ total score (r = 0.93) in those subjects.10 The CAT has only a short 8-item questionnaire for assessing health status, so it can be completed in about 2 minutes (See Appendix). The total score ranges from 0 to 40, with higher scores indicating a worse health status.11 However, the CAT has not been examined as a prognostic marker in interstitial lung disease; some patients with interstitial lung disease have a short disease trajectory and a similar prognosis to patients with lung cancer.1 The aim of this study was to apply this simple instrument to patients with interstitial lung disease and to verify the CAT as a predictor of outcome.
Methods
This study included 101 consecutive patients (53 females and 48 males, with an average age of 63.8 years) with interstitial lung disease defined by high-resolution computed tomography (Table 1).12 They were transferred to Kanazawa University Hospital, Japan, between January 2013 and July 2015 for routine evaluation or treatment. All patients were evaluated by the CAT on the day of their first visit and followed up for more than one year (median, 18 months). We performed a review of hospital records for the patient data. As this study was performed retrospectively, written informed consent for participation in the study was not obtained from patients, and subject records were anonymized prior to analysis. The use of patient records for the study was approved by the Human Ethics Committee of Kanazawa University. Kanazawa University, conforming to the provisions of the Declaration of Helsinki.
Table 1.
Demographic and clinical characteristics of the interstitial lung disease patients studied, subdivided according to CAT scores.
| TOTAL N = 101 |
LOW CAT ≤ 10 N = 35 |
MEDIUM CAT ≤ 20 N = 43 |
HIGH CAT ≤ 30 N = 21 |
VERY HIGH CAT > 30 N = 2 |
P | |
|---|---|---|---|---|---|---|
| Gender (f/m) | 53/48 | 23/12 | 19/24 | 10/11 | 1/1 | NS |
| Age (yrs) | 63.8 ± 12.6 | 60.3 ± 15.1 | 68.0 ± 9.9 | 61.0 ± 11.2 | 64.0 | 0.04 (L vs. M) |
| Height (cm) | 159 ± 9 | 160 ± 10 | 158 ± 8 | 160 ± 10 | 163 | NS |
| Weight (kg) | 57 ± 11 | 57 ± 11 | 56 ± 10 | 56 ± 14 | 70 | NS |
| Time since diagnosis (yrs) | 6.3 ± 7.2 | 7.4 ± 7.7 | 5.7 ± 5.4 | 6.4 ± 9.6 | 1.3 | NS |
| Home oxygen therapy (y/n) | 9/92 | 0/35 | 3/40 | 6/15 | 0/2 | NA |
| FVC (% pred) | 84.2 ± 24.6 | 97.6 ± 19.9 | 81.4 ± 23.5 | 66.7 ± 23.7 | 80.0 | <0.001 (L vs. H) 0.01 (L vs. M) |
| DLCO (% pred) | 48.1 ± 20.0 | 61.6 ± 17.1 | 42.5 ± 16.3 | 35.2 ± 21.9 | 39.4 | 0.0001 (L vs. H and M) |
Notes: Data are expressed as mean ± SD or absolute numbers. No SD is calculated in the group of CAT > 30 because the number of patients was only two.
Abbreviations: CAT, COPD Assessment Test; FVC, forced vital capacity; DLCO, lung diffusion capacity for carbon monoxide; L, low impact; M, medium impact; H, high impact; NS, not significant; NA, not available.
Thirty-six patients were diagnosed with idiopathic interstitial pneumonia, and the others were diagnosed with connective tissue disease-associated interstitial lung diseases. The percent of predicted FVC and DLCO were collected from the pulmonary function tests.
Statistical analysis
The CAT scores were categorized into low (CAT ≤ 10), medium (11 ≤ CAT ≤ 20), high (21 ≤ CAT ≤ 30), and very high (CAT > 30) impact according to the severity.13 Statistical analysis was performed using analysis of variance and Tukey’s honestly significant difference (HSD) test for multiple comparisons of values and the chi-squared test for comparison of frequencies classified by impacts evaluated by the CAT. Survival according to severity of the CAT score was illustrated via Kaplan–Meier curves. Cox regression analysis was used to examine mortality in terms of age, CAT score, percent of predicted FVC and DLCO, and home oxygen therapy. JMP 11 software (SAS Institute Inc.) was used for statistical analysis. P < 0.05 was considered significant.
Results
Gender, height, weight, and time since diagnosis were not different among subdivided patients according to CAT scores (Table 1). Patients with medium impact were older than patients with low impact. Nine patients used home oxygen therapy (up to 3 L/minute). Patients with higher CAT scores exhibited significantly lower percentages of predicted FVC and DLCO than those with lower CAT scores, a difference that was especially pronounced between patients with low and medium or high impact.
During the follow-up period, 12 patients died and at least 9 deaths from pulmonary insufficiency were put on record in our hospital. Mortality in patients with higher CAT scores was significantly higher than in patients with lower CAT scores (log-rank test, P = 0.0002; Fig. 1). In univariate models, the mortality hazard ratio of high CAT scores vs. low CAT scores was 5.11 (P = 0.04), and hazard ratio of very high CAT scores vs. low CAT scores and vs. medium CAT scores was 19.50 and 14.38 (P = 0.01 for both), respectively. The hazard ratios for FVC per 1% predicted and DLCO per 1% predicted were 0.97 and 0.94 (P = 0.02 for both; Table 2). Age and home oxygen therapy did not influence the hazard ratio. Relative hazards in multivariate models were also calculated for the same variables. The mortality hazard ratios of very high CAT scores vs. low, medium, and high CAT scores were 13.27, 35.95, and 428.51(P = 0.04, P = 0.005, and P = 0.001), respectively. The hazard ratio for DLCO per 1% predicted was 0.88 (P = 0.003).
Figure 1.
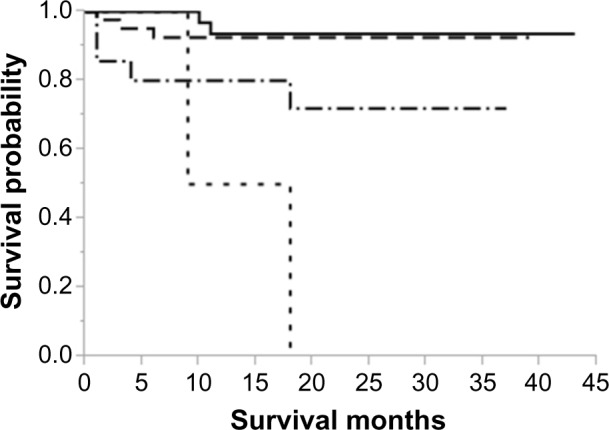
Kaplan–Meier survival curves according to severity of CAT score. Solid line: CAT score ≤10; dash line: 11–20; dash and dotted line: 21–30; dotted line: >30. Survival curves were compared with the log-rank statistic, P = 0.0002.
Table 2.
Cox regression analysis of survival-related parameters.
| VARIABLES | UNIVARIATE | MULTIVARIATE | ||
|---|---|---|---|---|
| RELATIVE HAZARD (95% CI) | P | RELATIVE HAZARD (95% CI) | P | |
| Age | 1.03 (0.99–1.09) | NS | 1.07 (0.98–1.22) | NS |
| CAT categories | ||||
| Medium/Low | 1.36 (0.22–10.30) | NS | 0.37 (0.04–8.41) | NS |
| High/Low | 5.11 (1.10–35.75) | 0.04 | 0.03 (0.00–2.28) | NS |
| High/Medium | 3.77 (0.92–18.40) | NS | 0.08 (0.00–1.96) | NS |
| Very high/Low | 19.50 (2.33–162.95) | 0.01 | 13.27 (1.20–305.53) | 0.04 |
| Very high/Medium | 14.38 (1.89–87.01) | 0.01 | 35.95 (3.40–593.63) | 0.005 |
| Very high/High | 3.81 (0.54–17.76) | NS | 428.51 (9.21–130916.4) | 0.001 |
| Home oxygen therapy (y/n) | 2.35 (0.36–8.94) | NS | 15.97 (0.31–964.31) | NS |
| FVC (% pred) | 0.97 (0.94–0.996) | 0.02 | 0.996 (0.94–1.05) | NS |
| DLCO (% pred) | 0.94 (0.87–0.99) | 0.02 | 0.88 (0.78–0.96) | 0.003 |
Abbreviations: CI, confidence interval; CAT, COPD Assessment Test; FVC, forced vital capacity; DLCO, lung diffusion capacity for carbon monoxide; NS, not significant.
Discussion
Our data demonstrate a relationship between higher CAT scores and lower pulmonary function and that higher CAT scores indicate a higher hazard of dying during follow-up of 18 months. Moreover, severely deteriorated quality of life was an independent factor from impaired DLCO in terms of mortality. Previous studies have demonstrated the relationship between quality of life and pulmonary functions such as FVC and DLCO or results of the 6MWT in interstitial lung disease,3–6 and our results supported the validity of the CAT. However, no study has referred to the relationship between the CAT and outcomes in those patients. The CAT, comprising only eight items and able to be completed in short time,11 appears to be useful as a prognostic marker for interstitial lung disease.
In this study, we found a significant independent relationship between the percent of predicted DLCO and survival, demonstrated by relative hazards in multivariate models. A conflicting study reported that the percent of predicted FVC and DLCO did not directly affect the hazard ratio for death in idiopathic interstitial pneumonia,8 whereas in patients with systemic sclerosis, systolic pulmonary artery pressure and DLCO (cutoff value: 64%) were found to be independently associated with the risk of death.14,15 In this study, 9 of 12 deaths were of patients with idiopathic interstitial pneumonia, while the others were patients with systemic sclerosis or mixed connective tissue disease, who showed percent of predicted DLCO values lower than 64%. Therefore, it is suggested that percent of predicted DLCO should be considered one of the factors for predicting survival in widely classified interstitial lung disease.
The status of oxygen therapy in this study did not show a significant effect on survival, although oxygen therapy may be beneficial for maintaining oxygen saturation. However, the lack of association between home oxygen therapy and survival cannot be generalized because of the low number of subjects (nine patients). Generally, long-term oxygen therapy is known to improve survival without affecting quality of life in patients with COPD.16 Previously, deterioration in quality of life in interstitial lung disease compared with COPD was reported,17,18 and it was thought to be due to differences in the dyspnea mechanism or in the rate of disease progression. For example, forced expiratory volume in the first second was associated with health status in COPD,19 whereas FVC and DLCO also showed significant correlations with quality of life in interstitial lung disease.20
There were some limitations to this study. First, medications or complications were not taken into account, although different clinical approaches and survival rates were suggested depending on lung biopsy findings or underlying diseases associated with interstitial lung disease.21,22 Second, the study was retrospectively performed at a single facility. We cannot deny the possibility of an unexpected bias among the present patients, even though we analyzed consecutive patients who visited our facility. Further multicenter studies will be needed to assess longitudinal changes regarding health status.
Conclusion
This work has demonstrated that it is possible to relate CAT scores to mortality in patients with interstitial lung disease, similar to lung perfusion disturbance. Considering that the CAT needs no special equipment to evaluate the health status of patients, the CAT may have a potential for use in everyday clinical practice regarding mortality hazard for patients with interstitial lung disease.
Appendix
The COPD Assessment Test (CAT)
For each item below, place a mark (√) in the box that best describes your experience.
| Example: I am very happy | 0 | √1 | 2 | 3 | 4 | 5 | I am very sad |
| SCORE | ||||||||
|---|---|---|---|---|---|---|---|---|
| I never cough | 0 | 1 | 2 | 3 | 4 | 5 | I cough all the time | |
| I have no phlegm (mucus) in my chest at all | 0 | 1 | 2 | 3 | 4 | 5 | My chest is completely full of phlegm (mucus) | |
| My chest does not feel tight at all | 0 | 1 | 2 | 3 | 4 | 5 | My chest feels very tight | |
| When I walk up a hill or one flight of stairs I am not breathless | 0 | 1 | 2 | 3 | 4 | 5 | When I walk up a hill or one flight of stairs I am very breathless | |
| I am not limited doing any activities at home | 0 | 1 | 2 | 3 | 4 | 5 | I am very limited doing activities at home | |
| I am confident leaving my home despite my lung condition | 0 | 1 | 2 | 3 | 4 | 5 | I am not at all confident leaving my home because of my lung condition | |
| I sleep soundly | 0 | 1 | 2 | 3 | 4 | 5 | I don’t sleep soundly because of my lung condition | |
| I have lots of energy | 0 | 1 | 2 | 3 | 4 | 5 | I have no energy at all | |
| SCORE | ||||||||
This questionnaire was developed by Jones et al.9
Footnotes
ACADEMIC EDITOR: Hussein D. Foda, Editor in Chief
PEER REVIEW: Six peer reviewers contributed to the peer review report. Reviewers’ reports totaled 1043 words, excluding any confidential comments to the academic editor.
FUNDING: Authors disclose no external funding sources.
COMPETING INTERESTS: Authors disclose no potential conflicts of interest.
Paper subject to independent expert blind peer review. All editorial decisions made by independent academic editor. Upon submission manuscript was subject to anti-plagiarism scanning. Prior to publication all authors have given signed confirmation of agreement to article publication and compliance with all applicable ethical and legal requirements, including the accuracy of author and contributor information, disclosure of competing interests and funding sources, compliance with ethical requirements relating to human and animal study participants, and compliance with any copyright requirements of third parties. This journal is a member of the Committee on Publication Ethics (COPE).
Author Contributions
Contributed to the design of the study and data collection, performed statistical analysis, and drafted the manuscript: FS. Participated in the design of the study and data collection: TN. Contributed to the conception, data acquisition, and approval of the manuscript: NM. All the authors reviewed and approved the final manuscript.
REFERENCES
- 1.Bajwah S, Ross JR, Peacock JL, et al. Interventions to improve symptoms and quality of life of patients with fibrotic interstitial lung disease: a systematic review of the literature. Thorax. 2013;68:867–79. doi: 10.1136/thoraxjnl-2012-202040. [DOI] [PubMed] [Google Scholar]
- 2.Swigris JJ, Wilson SR, Green KE, Sprunger DB, Brown KK, Wamboldt FS. Development of the ATAQ-IPF: a tool to assess quality of life in IPF. Health Qual Life Outcomes. 2010;8:77. doi: 10.1186/1477-7525-8-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Patel AS, Siegert RJ, Brignall K, et al. The development and validation of the King’s Brief Interstitial Lung Disease (K-BILD) health status questionnaire. Thorax. 2012;67:804–10. doi: 10.1136/thoraxjnl-2012-201581. [DOI] [PubMed] [Google Scholar]
- 4.Martinez TY, Pereira CAC, dos Santos ML, Ciconelli RM, Guimaraes SM, Martinez JAB. Evaluation of the Short-Form 36-item questionnaire to measure health-related quality of life in patients with idiopathic pulmonary fibrosis. Chest. 2000;117:1627–32. doi: 10.1378/chest.117.6.1627. [DOI] [PubMed] [Google Scholar]
- 5.Manali ED, Lyberopoulos P, Triantafillidou C, et al. MRC chronic Dyspnea Scale: relationships with cardiopulmonary exercise testing and 6-minute walk test in idiopathic pulmonary fibrosis patients: a prospective study. BMC Pulm Med. 2010;10:32. doi: 10.1186/1471-2466-10-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.du Bois RM, Weycker D, Albera C, et al. Six-minute-walk test in idiopathic pulmonary fibrosis: test validation and minimal clinically important difference. Am J Respir Crit Care Med. 2011;183:1231–7. doi: 10.1164/rccm.201007-1179OC. [DOI] [PubMed] [Google Scholar]
- 7.Hallstrand TS, Boitano LJ, Johnson WC, Spada CA, Hayes JG, Raghu G. The timed walk test as a measure of severity and survival in idiopathic pulmonary fibrosis. Eur Respir J. 2005;25:96–103. doi: 10.1183/09031936.04.00137203. [DOI] [PubMed] [Google Scholar]
- 8.Lama VN, Flaherty KR, Toews GB, et al. Prognostic value of desaturation during a 6-minute walk test in idiopathic interstitial pneumonia. Am J Respir Crit Care Med. 2003;168:1084–90. doi: 10.1164/rccm.200302-219OC. [DOI] [PubMed] [Google Scholar]
- 9.Jones PW, Harding G, Berry P, Wiklund I, Chen W-H, Leidy NK. Development and first validation of the COPD Assessment Test. Eur Respir J. 2009;34:648–54. doi: 10.1183/09031936.00102509. [DOI] [PubMed] [Google Scholar]
- 10.Nagata K, Tomii K, Otsuka K, et al. Evaluation of the chronic obstructive pulmonary disease assessment test for measurement of health-related quality of life in patients with interstitial lung disease. Respirology. 2012;17:506–12. doi: 10.1111/j.1440-1843.2012.02131.x. [DOI] [PubMed] [Google Scholar]
- 11.Ringbaek T, Martinez G, Lange P. A comparison of the assessment of quality of life with CAT, CCQ, and SGRQ in COPD patients participating in pulmonary rehabilitation. COPD. 2012;9:12–5. doi: 10.3109/15412555.2011.630248. [DOI] [PubMed] [Google Scholar]
- 12.Woodhead F, Wells AU, Desai SR. Pulmonary complications of connective tissue diseases. Clin Chest Med. 2008;29:149–64. doi: 10.1016/j.ccm.2007.11.009. [DOI] [PubMed] [Google Scholar]
- 13.Jones PW, Tabberer M, Chen WH. Creating scenarios of the impact of COPD and their relationship to COPD assessment test (CAT™) scores. BMC Pulm Med. 2011;11:42. doi: 10.1186/1471-2466-11-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hachulla E, Clerson P, Airo P, et al. Value of systolic pulmonary arterial pressure as a prognostic factor of death in the systemic sclerosis EUSTAR population. Rheumatology. 2015;54:1262–9. doi: 10.1093/rheumatology/keu450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nihtyanova SI, Schreiber BE, Ong VH, et al. Prediction of pulmonary complications and long-term survival in systemic sclerosis. Arthritis Rheum. 2014;66:1625–35. doi: 10.1002/art.38390. [DOI] [PubMed] [Google Scholar]
- 16.Okubadejo AA, Paul EA, Jones PW, Wedzicha JA. Dose long-term oxygen therapy affect quality of life in patients with chronic obstructive pulmonary disease and severe hypoxaemia? Eur Respir J. 1996;9:2335–9. doi: 10.1183/09031936.96.09112335. [DOI] [PubMed] [Google Scholar]
- 17.Berry CE, Drummond MB, Han MK, et al. Relationship between lung function impairment and health-related quality of life in COPD and interstitial lung disease. Chest. 2012;142:704–11. doi: 10.1378/chest.11-1332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kozu R, Senjyu H, Jenkins SC, Mukae H, Sakamoto N, Kohno S. Differences in response to pulmonary rehabilitation in idiopathic pulmonary fibrosis and chronic obstructive pulmonary disease. Respiration. 2011;81:196–205. doi: 10.1159/000315475. [DOI] [PubMed] [Google Scholar]
- 19.Westwood M, Bourbeau J, Jones PW, Cerulli A, Capkun-Niggli G, Worthy G. Relationship between FEV1 change and patient-reported outcomes in randomized trials of inhaled bronchodilators for stable COPD: a systematic review. Respir Res. 2011;12:40. doi: 10.1186/1465-9921-12-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chang JA, Curtis JR, Patrick DL, Raghu G. Assessment of health-related quality of life in patients with interstitial lung disease. Chest. 1999;116:1175–82. doi: 10.1378/chest.116.5.1175. [DOI] [PubMed] [Google Scholar]
- 21.Travis WD, Matsui K, Moss J, Ferrans VJ. Idiopathic nonspecific interstitial pneumonia: prognostic significance of cellular and fibrosing patterns: survival comparison with usual interstitial pneumonia and desquamative interstitial pneumonia. Am J Surg Pathol. 2000;24:19–33. doi: 10.1097/00000478-200001000-00003. [DOI] [PubMed] [Google Scholar]
- 22.de Lauretis A, Veeraraghavan S, Renzoni E. Review series: aspects of interstitial lung disease: connective tissue disease-associated interstitial lung disease: how does it differ from IPF? How should the clinical approach differ? Chron Respir Dis. 2011;8:53–82. doi: 10.1177/1479972310393758. [DOI] [PubMed] [Google Scholar]


