Abstract
Background:
Between 2010 and 2012, the World Health Organization Division of Pacific Technical Support led a regional climate change and health vulnerability assessment and adaptation planning project, in collaboration with health sector partners, in 13 Pacific island countries—Cook Islands, Federated States of Micronesia, Fiji, Kiribati, Marshall Islands, Nauru, Niue, Palau, Samoa, Solomon Islands, Tonga, Tuvalu, and Vanuatu.
Objective:
We assessed the vulnerabilities of Pacific island countries to the health impacts of climate change and planned adaptation strategies to minimize such threats to health.
Methods:
This assessment involved a combination of quantitative and qualitative techniques. The former included descriptive epidemiology, time series analyses, Poisson regression, and spatial modeling of climate and climate-sensitive disease data, in the few instances where this was possible; the latter included wide stakeholder consultations, iterative consensus building, and expert opinion. Vulnerabilities were ranked using a “likelihood versus impact” matrix, and adaptation strategies were prioritized and planned accordingly.
Results:
The highest-priority climate-sensitive health risks in Pacific island countries included trauma from extreme weather events, heat-related illnesses, compromised safety and security of water and food, vector-borne diseases, zoonoses, respiratory illnesses, psychosocial ill-health, non-communicable diseases, population pressures, and health system deficiencies. Adaptation strategies relating to these climate change and health risks could be clustered according to categories common to many countries in the Pacific region.
Conclusion:
Pacific island countries are among the most vulnerable in the world to the health impacts of climate change. This vulnerability is a function of their unique geographic, demographic, and socioeconomic characteristics combined with their exposure to changing weather patterns associated with climate change, the health risks entailed, and the limited capacity of the countries to manage and adapt in the face of such risks.
Citation:
McIver L, Kim R, Woodward A, Hales S, Spickett J, Katscherian D, Hashizume M, Honda Y, Kim H, Iddings S, Naicker J, Bambrick H, McMichael AJ, Ebi KL. 2016. Health impacts of climate change in Pacific island countries: a regional assessment of vulnerabilities and adaptation priorities. Environ Health Perspect 124:1707–1714; http://dx.doi.org/10.1289/ehp.1509756
Introduction
Climate change is widely acknowledged to be one of the most serious global threats to future human population health and international development (Costello et al. 2009; Stephenson et al. 2013; Woodward et al. 2014). The Fifth Assessment Report (AR5) from the Intergovernmental Panel on Climate Change (IPCC) affirms that recent decades have seen warming air and ocean temperatures, altered precipitation patterns, rising sea levels, and changes in the frequency and intensity of some extreme events such as droughts, floods, and storms (IPCC 2014). The AR5 also asserts with greater confidence than reported in 2007 (Parry et al. 2007) that recent warming is largely attributable to human activity. Further, there is increasing certainty that these trends will continue or, in some cases, accelerate (IPCC 2014).
A changing climate has significant and diverse impacts on human health (McMichael and Lindgren 2011; Woodward et al. 2014). The pathways by which climate change affects health vary according to their modes of action and include primary or direct effects (e.g., injuries and deaths caused by extreme weather events such as cyclones), secondary or indirect effects (e.g., the increasing geographic range of, and population exposed to, vectors that spread disease), and tertiary, diffuse, and/or delayed effects (e.g., disruptions to health and social services) (Butler and Harley 2010; McMichael 2013).
Pacific island countries (PICs) are among those most vulnerable to the health impacts of a changing climate (Hanna and McIver 2014; Woodward et al. 2000). This vulnerability is a function of their exposure to changing weather patterns associated with climate change, the health risks entailed, and the limited capacity of these countries to manage and adapt in the face of such risks. The climate change phenomena occurring in the Pacific pose a suite of health hazards to the island communities across the region. A conceptualization of the pathways by which climate change will affect health in the Pacific and the major anticipated impacts throughout the region is shown in Figure 1.
Figure 1.
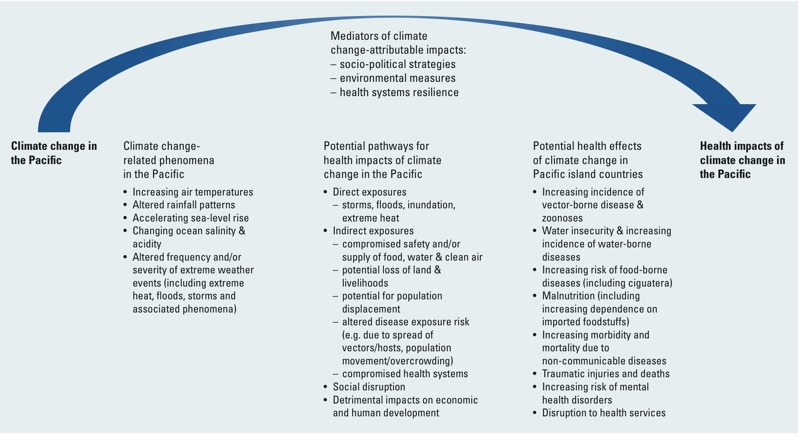
Climate change and health impact pathways relevant to Pacific island countries.
In PICs, this vulnerability reflects the unique geographic, demographic, and socioeconomic characteristics of small island developing states (SIDS) (Table 1), which, combined with their contemporary burden of ill-health and relatively low health systems capacity, give credence to the epithet “canaries in the coalmine” of climate change and health (Hanna and McIver 2014).
Table 1.
Characteristics of Pacific island countries.
| Pacific island country | Geography | Demography | Economy | |||
|---|---|---|---|---|---|---|
| Land area (km2)a | Max elevation (m)b | Populationb | Population density (per km2) | Per capita GDPb,c | Main industries # (% GDP)b | |
| Cook Islands | 240 | 652 | 15,000 | 42 | 9,100 | T |
| Federated States of Micronesia | 700 | 791 | 112,000 | 158 | 2,200 | A, F |
| Fiji | 18,000 | 1,324 | 868,000 | 47 | 4,600 | T, A |
| Kiribati | 800 | 3, 81d | 101,000 | 135 | 6,200 | A, F, R |
| Marshall Islands | 200 | 10 | 64,000 | 342 | 2,500 | Aid (US) |
| Nauru | 20 | 71 | 10,000 | 480 | 5,000 | M |
| Niue | 260 | 68 | 1,000 | 5 | 8,400 | Aid (NZ) |
| Palau | 500 | 242 | 21,000 | 39 | 10,000 | T, A, F |
| Samoa | 2,900 | 1,857 | 184,000 | 63 | 6,000 | R, T, A, F |
| Solomon Islands | 28,000 | 2,335 | 552,000 | 18 | 3,300 | A, F, forestry |
| Tonga | 750 | 1,033 | 105,000 | 139 | 7,500 | A, F |
| Tuvalu | 300 | 5 | 10,000 | 476 | 3,400 | R, trusts, A |
| Vanuatu | 12,000 | 1,877 | 246,000 | 20 | 2,700 | A, F, T |
| Abbreviations: A, agriculture; F, fishing; M, mining; NZ, New Zealand; R, remittances; T, tourism; US, United States. All data are for 2011 unless otherwise stated. aUN Office of the High Representative for the Least Developed Countries, Landlocked Countries and Small Island Developing States (UN-OHRLLS 2015). bCentral Intelligence Agency (2012). cPer capita gross domestic product based on purchasing power parity. Estimates are for 2011 except for Marshall Islands (year 2008), Nauru (year 2005), Palau (year 2009), Tuvalu (year 2010), and Vanuatu (year 2009).dElevations for South Tarawa (the capital atoll of Kiribati) and Banaba (an outlying atoll), respectively. | ||||||
Recognizing the risks to health posed by climate change, the World Health Organization (WHO) Regional Offices for the Western Pacific and South-East Asia issued a joint Regional Framework for Action to Protect Human Health from the Effects of Climate Change in the Asia-Pacific Region (WHO 2007; Hanna and McIver 2014) This framework committed all countries in the region to increasing awareness of climate change and health, to strengthening the capacity of health systems to protect against climate-related health risks and reduce greenhouse gas emissions in the health sector, and to ensuring that health concerns were addressed in climate action in other sectors. Specific actions mandated in the framework included supporting formalized climate change and health vulnerability assessments and leading the health sector’s contribution to national adaptation planning processes in the region.
Subsequently, the health ministers of PICs strengthened their commitments to action on climate change at their biennial meeting in Madang, Papua New Guinea, in 2009. The Madang Commitment included further recommendations related to vulnerability assessments and adaptation planning, framing these within the Healthy Islands vision for health systems development in the Pacific (Galea et al. 2000; WHO 2009).
This paper describes the process and outcomes of climate change and health vulnerability assessments in 13 SIDS in the Pacific region: Cook Islands, Federated States of Micronesia, Fiji, Kiribati, Marshall Islands, Nauru, Niue, Palau, Samoa, Solomon Islands, Tonga, Tuvalu, and Vanuatu (see map in Figure 2).
Figure 2.
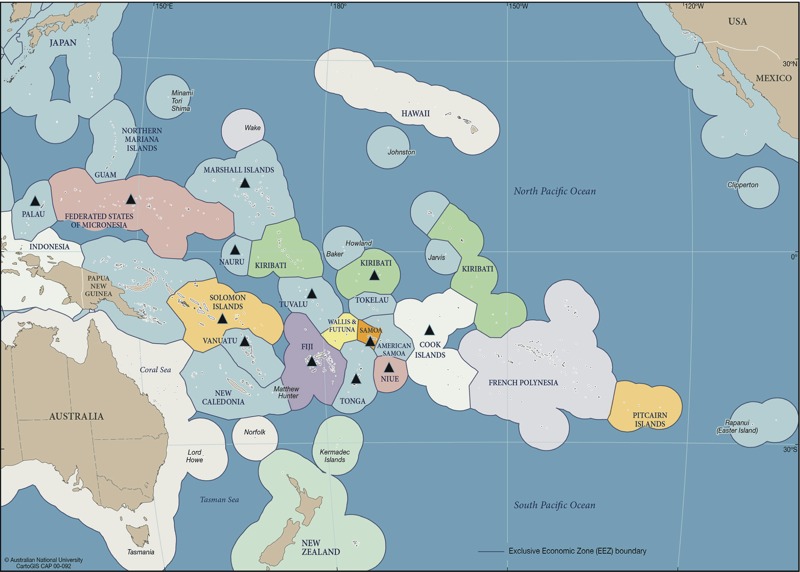
Countries involved in WHO-supported climate change and health project in the Pacific (2010–2013) [Source: adapted from CartoGIS (2016), College of Asia and Pacific, The Australian National University, under terms of ShareAlike 3.0 Australia (https://creativecommons.org/licenses/by-sa/3.0/au/legalcode). Some changes have been made to this figure: black triangles were added to indicate the project countries].
In this paper, we report how these assessments link with adaptation planning; we also highlight some of the unique challenges facing PICs in the context of climate change, and we summarize the corresponding recommendations arising from the regional project. This paper is aimed at a general scientific audience and is a synthesis of the key technical findings and policy implications of the forthcoming WHO report entitled, Human Health and Climate Change in Pacific Island Countries (McIver et al. 2015b).
Methods
Between 2010 and 2012, the WHO Division of Pacific Technical Support, with support from the Western Pacific Regional Office (WPRO) and funding from the governments of the Republic of Korea and Japan, led a regional climate change and health vulnerability and adaptation project involving 11 PICs: Cook Islands, Federated States of Micronesia (FSM), Kiribati, Marshall Islands, Nauru, Niue, Palau, Solomon Islands, Tonga, Tuvalu and Vanuatu. This project was implemented in three phases, with the 11 countries divided into three groups along broadly geographic lines and a team of expert climate change and health consultants guiding and assisting each group. These 11 countries form the majority of independent or autonomous states in the Pacific region, along with Fiji and Samoa, which carried out related projects (see below). Papua New Guinea has been involved in a separate climate change and health project, along with other countries in the Western Pacific region, and was not included; the French territories of New Caledonia, French Polynesia, and Wallis and Futuna were excluded for similar reasons.
In the first phase, sub-regional inception meetings were held in Auckland, New Zealand (for the group that included Cook Islands, Kiribati, Niue, Tonga, and Tuvalu); Honiara, Solomon Islands (for Nauru, Solomon Islands, and Vanuatu); and Pohnpei, FSM (for FSM, Marshall Islands, and Palau). During these meetings, the science of climate change and health was reviewed, along with the relevant work previously conducted in each country, and plans were made for the in-country vulnerability assessment and adaptation planning phases of the project.
The second phase involved a mixed-methods approach to ascertain each country’s climate-sensitive health risks based on a combination of review and analysis of climate and health data, stakeholder consultations, and an assessment of the potential impacts of a changing climate across different aspects of society. Where possible, epidemiological analysis was performed on the available data for historical climate variables and climate-sensitive diseases (e.g., diarrheal disease, dengue fever, and leptospirosis). Performing these analyses was possible only in countries with adequate data (in terms of quality and quantity) and available technical support. The sophistication of the modeling undertaken ranged from simple reviews of disease burdens and weather patterns in Kiribati (McIver et al. 2014) to Poisson regression models in FSM (McIver et al. 2015a) and similar techniques, combined with spatial modeling, for multiple climate-sensitive diseases in Fiji (McIver et al. 2012). The results of these country-specific analyses have not been included in this paper, which instead provides a more general, regional overview.
In the final phase, each country’s climate change and health vulnerabilities were assessed using a “likelihood-versus-consequence” matrix. This tool was used to rank climate-sensitive health priorities, rationalize resources, and focus the activities of the health sector on the most urgent adaptation activities. Its use was based on precedents in Australia (Brown et al. 2014) and on growing evidence of its utility in this context in Pacific island countries such as Vanuatu (Spickett and Katscherian 2014; Spickett et al. 2013). In using this matrix, each climate-sensitive health risk was considered in terms of a) the likelihood of the burden of disease increasing with climate change (over a 20-year time-frame), b) a range of climate change projections (as localized as possible), and c) the impact of such an increased health burden occurring (considering the resilience or coping capacity of the community and health sector to manage such consequences).
Each Pacific island country differed in terms of its willingness and perceived capacity to manage its respective highest-priority climate-sensitive health risks. Some elected to include most or all of these hazards in their adaptation plans; others chose to concentrate on the few health impacts deemed to represent the greatest threat according to the abovementioned matrix. Thus, the climate-sensitive health risks presented in the “Results” below should be considered a synthesis of each country’s priorities rather than a true cross-country comparison of risks.
Following the prioritization of these climate change–related health vulnerabilities, relevant adaptation strategies were planned accordingly. Adaptation measures were categorized as follows: legislative and regulatory, public education and communication, surveillance and monitoring, ecosystem intervention, infrastructure development, technological and engineering responses, medical intervention, and research.
Each adaptation measure was prioritized for each PIC according to its local relevance, the current capacity of the health system, the inclusion of vulnerable groups, the manner in which adaptations could be implemented, and the identification of sectors that would be involved in the development and implementation of the adaptation strategies. The country teams—which were typically, but not exclusively, led by the Ministry of Health or its equivalent in collaboration with other government departments, civil society organizations and major private sector stakeholders—chose the factors that would be included and decided upon their relative weighting.
These vulnerabilities and the responses required from the health sector were incorporated into National Climate Change and Health Action Plans (NCCHAPs) or an equivalent thereof. At present, these domestic policy documents are in various stages of finalization and implementation across the Pacific island countries participating in this regional project.
The vulnerability assessment and adaptation planning process was slightly different for Samoa. An initial workshop on health aspects of vulnerability and adaptation to climate change was conducted in Apia in 2010 as part of a national project entitled, “Integrating Climate Change Risks in the Agriculture and Health Sectors in Samoa.” Building on this work, a climate change and health adaptation strategy and action plan was developed for Samoa in 2013.
The approach was different again for Fiji, which since 2010 has been participating in a global climate change and health adaptation pilot project led by WHO with support from the United Nations Development Programme (UNDP) and with funding from the Global Environment Facility (GEF; https://www.thegef.org/). In Fiji’s Piloting Climate Change Adaptation to Protect Human Health project, a small number of high-priority climate-sensitive diseases were selected as the focus for the vulnerability assessment, research, capacity-building, community education, and adaptation elements of the project (McIver et al. 2012).
The process outlined above broadly followed the guidelines laid out by WHO for vulnerability assessment and adaptation planning (Kovats et al. 2003; WHO 2013b). Table 2 compares the WHO theoretical framework with the actual steps implemented in the abovementioned PICs.
Table 2.
Steps involved in vulnerability assessment and adaptation planning process in Pacific island countries (PICs) and comparison with WHO framework [the latter adapated from Kovats et al. (2003)].
| WHO framework for vulnerability assessment and adaptation planning | Vulnerability assessment and adaptation planning process implemented in PICs |
|---|---|
| Determine scope of assessment |
|
| Describe current distribution and burden of climate-sensitive diseases |
|
| Identify and describe current strategies, policies and measures that reduce the burden of climate-sensitive diseases |
|
| Review the health implications of the potential impact of climate variability and change on other sectors |
|
| Estimate the future potential health impact using scenarios of future climate change, population growth and other factors and describe the uncertainty |
|
| Synthesize the results and draft a scientific assessment report |
|
| Identify additional adaptation policies and measures to reduce potential negative health effects, including procedures for evaluation after implementation |
|
| Source: adapted from WHO (2013a). Protecting Health from Climate Change: Vulnerability and Adaptation Assessment. http://www.who.int/globalchange/publications/vulnerability-adaptation/en/. | |
In each of the 13 PICs, efforts were made to include mechanisms for monitoring and evaluation and iterative information management—for example, the incorporation of updated data on climate and climate-sensitive diseases—into each NCCHAP (Ebi 2014).
Results
Table 3 summarizes the climate-sensitive health risks prioritized in each country’s vulnerability assessment. These risks are subdivided into three categories: direct, indirect, and diffuse effects, in accordance with the international nomenclature (McMichael and Lindgren 2011). Examples of direct effects include the traumatic injuries and deaths that occur during hydro-meteorological disasters and the detrimental physiological consequences of heatwaves. Indirect effects occur through disruption of ecological systems; examples include increased pathogen loads in food and water in hotter and/or more humid conditions and altered geographic ranges and biting habits of mosquitoes that spread diseases such as malaria and dengue fever. Diffuse effects are related to societal dysfunction, key examples of which are disrupted health services, population displacement, and potential conflict over climate-related resources (Kjellstrom and McMichael 2013).
Table 3.
Highest priority climate-sensitive health risks in individual Pacific island countries (with each country’s highest priorities indicated by “x”).
| Climate-sensitive health risk | Country | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cook Islands | FSM | Fiji | Kiribati | Marshall Islands | Nauru | Niue | Palau | Samoa | Solomon Islands | Tonga | Tuvalu | Vanuatu | |
| Direct effects | |||||||||||||
| Health impacts of extreme weather eventsa | x | x | x | x | x | x | x | x | x | x | x | ||
| Heat-related illnessb | x | x | x | x | x | ||||||||
| Indirect effects | |||||||||||||
| Water security & safety (including water-borne diseases)c | x | x | x | x | x | x | x | x | x | x | x | x | x |
| Food security & safety (including malnutrition & food-borne diseases)d | x | x | x | x | x | x | x | x | x | x | x | x | |
| Vector-borne diseasese | x | x | x | x | x | x | x | x | x | x | x | x | x |
| Zoonosesf | x | x | x | ||||||||||
| Respiratory illnessg | x | x | x | x | x | x | x | x | x | ||||
| Disorders of the eyes, ears, skin, and other body systemsh | x | x | x | x | x | x | |||||||
| Diffuse effects | |||||||||||||
| Disorders of mental/psycho-social healthi | x | x | x | x | x | x | x | x | |||||
| Non-communicable diseases (NCDs)j | x | x | x | x | x | x | x | x | x | x | |||
| Health system deficienciesk | x | x | |||||||||||
| Population pressuresl | x | ||||||||||||
| FSM, Federated States of Micronesia. A number of climate-sensitive health risks may be considered to cut across categories: for example, there may be direct mental health consequences of extreme weather events; NCDs may be affected indirectly through disruption of food supplies, or more diffusely through socio-political strategies related to climate change, industry, and trade; health systems problems may be directly affected by extreme weather events as well as via the broader impact of climate change on development. aThis was typically taken to mean traumatic injuries and deaths, but may also be understood to include the psychosocial impacts of extreme events. bIncluding occupational exposure to hotter working conditions. cThis category encompasses water-borne infections causing diarrheal illness, as well as typhoid fever, and also includes problems such as sea-level rise-induced salination of potable water supplies. dIncluding food insecurity, food-borne diseases causing diarrheal illness, and ciguatera (“fish poisoning”). eIncluding, but not limited to, dengue fever and malaria; noting that these two diseases occur in some, but not all, PICs (of those countries listed, malaria is currently limited to Solomon Islands and Vanuatu). fThe primary zoonosis of concern in most PICs is leptospirosis. gIncluding infections, obstructive airways disease (e.g., asthma), and the pulmonary effects of heat and air pollution. hThis category includes a range of health problems, from skin infections and cataracts to sexually transmitted infections that were of concern in various PICs in the context of climate change. iIncludes the unspecified detrimental effects of social disruption (e.g., loss of life, land, or livelihoods) because of climate change–related phenomena; this category may include, inter alia, depression, anxiety, and posttraumatic stress disorder. jIn this context, NCDs refer primarily to circulatory diseases (e.g., cardiovascular disease, cerebrovascular diseases, hypertension) as well as to diabetes; in some PICs, this was also taken to include cancers and mental health disorders. kIncluding compromised access to health services, damage to health infrastructure, and additional strains on scarce resources (e.g., for climate-sensitive disease surveillance). lIncludes the possibility of climate change–induced resettlement and the effects of climate change–induced sea-level rise in exacerbating overcrowding. | |||||||||||||
This list was not intended to be comprehensive, to describe every conceivable risk to health that can be attributed to climate change; only those risks regarded by the country teams as being most important at the present time are included in this summary table. This table is also not intended to serve as a tool for comparison because although all countries used a similar process of prioritizing climate change and health vulnerabilities, each country differed in terms of the number of these hazards it felt appropriate to address in its respective adaptation plans. Thus, the absence of an entry in a row for a particular country in Table 3 should not necessarily be interpreted to mean that the country did not perceive that specific climate-sensitive health risk to be a problem; rather, this health risk was not among the most immediate priorities for that country at that time.
Table 3 displays some common themes in terms of climate-sensitive health risks across the Pacific. Climate change–attributable impacts on extreme weather events and diseases related to food, water, and vectors are prominent concerns throughout the region. Specific diseases such as dengue fever, malaria, diarrheal illness, leptospirosis, typhoid fever, respiratory infections, obstructive airways disease, and malnutrition are generally considered to be highly climate-sensitive (Woodward et al. 2014). There is thus a clear and relatively urgent need for these and other hazards (such as the health effects of heat and extreme weather events) to be considered in the context of climate change in the Pacific and to be anticipated accordingly (Haines et al. 2014).
However, there are some climate-related health risks that are of concern in the Pacific to an extent not documented elsewhere in the world: notably, noncommunicable diseases (NCDs), disorders of mental/psychosocial health, and ciguatera (Mannava et al. 2015; WHO 2013c). The potential for climate change to amplify the drivers of NCD risk in the Pacific is considered in more detail below.
In addition, there are other important aspects of health vulnerability in the region that are unique to, or at least uniquely highly prioritized in, a small number of PICs. These aspects include high fertility rates and overcrowding in atoll nations such as Kiribati which, combined with limited land area, low elevation, and the threat posed by rising seas, may lead to forced relocation, which brings with it a particular suite of health complications (McMichael et al. 2012; Berry et al. 2010).
Women and children are expected to experience a disproportionate burden of climate change and health impacts in the Pacific (Lawler 2011) and elsewhere, particularly in the developing world (IPCC 2014).
With respect to adaptation, a number of strategies have been proposed and are being implemented across the Pacific region. Although some adaptation measures are country-specific (for example, developing legislation around cultural practices such as kava-drinking to protect against water-borne diseases, or experimenting with drought- and salt-resistant taro and cassava crops), the majority may be grouped under broad categories aligned with the abovementioned vulnerabilities. These measures include
Ensuring that health and safety considerations are incorporated into adaptation activities across sectors (“Health in All Policies” approach)
Improving the safety and security of food and water
Improving sanitation and hygiene facilities
Increased resourcing for health emergency risk management
Climate-proofing key health and safety infrastructure
Enhanced surveillance targeting climate-sensitive diseases and their risk sources
Applied environmental epidemiological research focusing on climate-sensitive diseases
New and improved communication pathways between the health sector, meteorology services and other stakeholders, including trialing and evaluating climate-based early warning systems.
Discussion
The climate change and health vulnerability assessment and adaptation planning project in the Pacific is similar in some respects to the corresponding work being carried out in other regions (Brooks and Adger 2003; Confalonieri et al. 2009; Wolf et al. 2014). However, there are some significant differences in terms of the process, findings, and implications that distinguish climate change and health issues in PICs from those in other countries of the world.
In terms of process, the precise methods by which the assessments were performed and adaptations planned varied from country to country. These included highly focused, largely quantitative assessments in the Marshall Islands and FSM, as distinct from a more deliberative, qualitative process employed in Nauru, Solomon Islands, and Vanuatu, where a modified environmental health impact assessment approach was employed (Spickett and Katscherian 2014; Spickett et al. 2013). In Kiribati, a mixed-methods, “middle way” approach proved effective in combining a review and analysis of the available data with a pragmatic process of inter-agency collaboration and stakeholder engagement, which has contributed to Kiribati’s NCCHAP being among the first to undergo government ratification and implementation (McIver et al. 2014).
With respect to outcomes, the issue of NCDs, in particular, was of unprecedented prominence in the Pacific in the face of climate change. With PICs already experiencing the highest rates of NCDs in the world (Mannava et al. 2015), the potential for climate change to act as an additional driver of NCD risk is considerable and of significant concern.
Although the literature on climate change and NCDs is relatively scant and has hitherto focused primarily on the implications of heat for individuals with preexisting NCDs (Friel et al. 2011; Kjellstrom and McMichael 2013; Kovats and Hajat 2008; Shubair et al. 2013), in the Pacific region, there is a very real concern that climate change may act as an additional risk factor for NCDs. It is likely that the Pacific region is—or will be—the first to experience the consequences of the interaction between climate change phenomena and other factors driving the burden of NCDs, such as physical inactivity, food insecurity, and poor nutrition. The schema in Figure 3, developed in consultation with the climate change and health team in Nauru (a tiny Pacific island country with one of the highest burdens of NCDs in the world), summarizes these interactions as they are perceived in a number of countries across the region.
Figure 3.
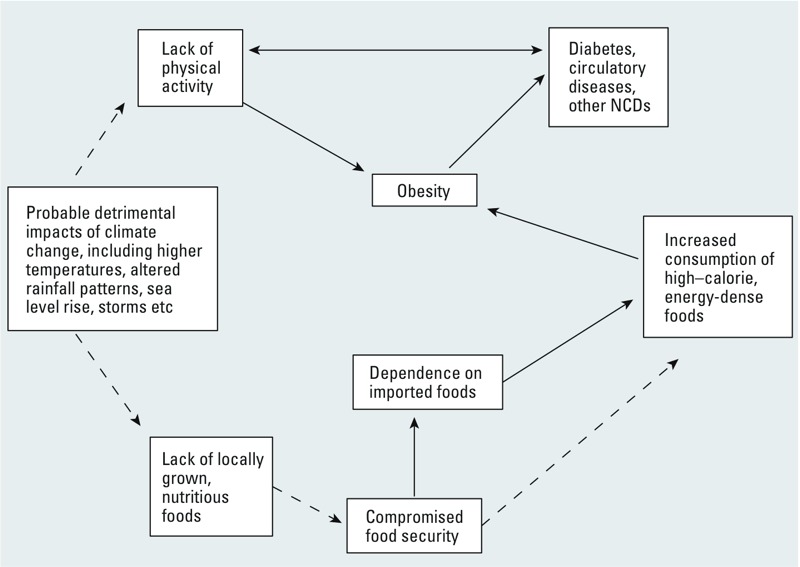
Conceptual model summarizing the pathways between climate change and NCDs (broken arrows represent hypothetical links).
It must also be acknowledged that PICs are very likely to be among the first communities to be forced to relocate because of anthropogenic climate change (Campbell 2014). There is some evidence that this forced migration—both internal and external—is already taking place (Birk and Rasmussen 2014; Locke 2009), and the physical and psychosocial health consequences of this phenomenon must not be underestimated (Butler et al. 2014; Reuveny 2007).
PICs face substantial challenges in implementing plans for adaptation. They include the scarce resources available to health sectors that are typically already under significant strain. Shortfalls in data, information systems, human resources, technical capacity, infrastructure, and finance are the rule, rather than the exception, in the Pacific region.
In light of the stark realities described above, many of the adaptation strategies recommended over the course of this climate change and health project were explicitly considered in terms of their overall utility, applicability, and feasibility in the context of profoundly underresourced health systems. Thus, the theoretical requirement for “additionality” mentioned in the international climate change and health literature with respect to adaptation (Füssel 2007) was considered significantly less important for health systems support in the Pacific than pragmatic, realistic measures that would both improve health care and build health systems resilience to climate change. Examples of these measures include improving water, sanitation, and hygiene systems and scaling up vector control. Such interventions have clear, broad, and long-term benefits, climate change notwithstanding, but they may not be possible for small, developing countries to implement without the avenues for resources and technical support afforded by adaptation.
There may, however, be some modest advantages for PICs in adapting to climate change. Principal among these advantages is the clear consensus about the need for action: debate about the science and implications of climate change is redundant in these countries, which are already experiencing its impacts. In addition, the small size of most PICs, where populations range from approximately 10,000 in Nauru and Tuvalu to < 1,000,000 in Fiji (Table 1), and the close-knit nature of such small, isolated communities, enables a relatively high degree of collaboration on adaptation between sectors, which has the potential for increased agility in decision making. There is some indication, however faint, that it may yet prove somewhat easier to achieve coherence in climate change and health governance in relatively cohesive Pacific island communities with shared traditional values than in other countries at varying levels of development but with looser or weaker social capital (Adger 2001; Bowen et al. 2013; Woodward et al. 2000).
There are clear limits to the effectiveness of adaptation, some of which will be tested even if, as is hoped, effective climate change mitigation policy is soon agreed upon and implemented at the global scale. Perhaps the clearest example is that of sea level rise, which threatens the very existence of low-lying island communities, posing an existential threat to the atoll nations of Kiribati, Marshall Islands, and Tuvalu (see Table 1).
One of the most promising areas of potential benefit, from both an economic and a social perspective, lies in co-benefits—the health gains anticipated from action on climate change mitigation—which are most pertinent in relation to NCDs (Ganten et al. 2010). Well-chosen disease-prevention strategies, such as decreased fossil fuel use, increased active transport (e.g., walking and cycling), and greater consumption of fresh, local foods instead of imported products, have obvious health benefits and will help reduce the pressure on the world’s climate.
It is impossible to address vulnerability and adaptation to climate change in the Pacific without pointing out the gross inequities and injustice that are involved. Pacific island countries have made infinitesimal contributions to the planetary problem of anthropogenic climate change, yet they will be among those who suffer most from its consequences. Industrialized countries have a clear responsibility to both scale up mitigation efforts to arrest climate change and to provide the necessary financial, technical, and in-kind support to developing countries to strengthen their coping capacity via adaptation in the meantime.
Finally, recognizing that PICs are among many countries in the world battling climate change as one of a number of significant impediments to social, economic, and health development, WHO is in the process of providing detailed guidance, in the form of frameworks, to assist member states in scaling up essential public health packages for health adaptation and building climate-resilient health systems (Neira 2014).
Conclusion
Pacific island countries are among the most vulnerable societies in the world to the health impacts of a changing climate.
Managing these health risks will require frequent revisions of adapation plans to take into account post-implementation reviews; new knowledge and understanding of climate change and health processes, pathways, and risks; and changes in relevant aspects of Pacific societies such as institutional structures, economic development, technology, and demographics.
This paper, and the corresponding WHO report released in early 2016, represent the first comprehensive synthesis of the current state of knowledge of health and climate change in the Pacific islands. This is but the first, important step in a long journey, for which PICs will require substantial and ongoing support.
Acknowledgments
This paper is the result of a collaborative project between the World Health Organization Division of Pacific Technical Support and the ministries and departments of health in 13 Pacific island countries. Although it is not possible to mention all of the project’s collaborators, we give special thanks to Y. Underhill-Sem, M. Pretrick, S. Davies, T. Tibwe, R. Edwards, M. Nosa, V. Nosa, M. Sengebau, V. Faasili, B. Patterson, J. Hilly, M. Ofanoa, M. Ake, N. Ituaso-Conway, T. Percival, B. Phillips, S. Laban, P. Rarua, and the late G. Waidubu. We also add a special acknowledgement to our co-author, colleague, and friend, A.J.M.—a pioneer and leader in the field of global public health—who passed away during the preparation of this final manuscript.
Footnotes
The work conducted throughout the course of this project was made possible by funding from the governments of the Republic of Korea and Japan.
The authors declare they have no actual or potential competing financial interests.
References
- Adger WN. Norwich, UK: University of East Anglia; 2001. Social Capital and Climate Change. Tyndall Centre for Climate Change Research, Working Paper 8. http://www.tyndall.ac.uk/sites/default/files/wp8.pdf [accessed 25 November 2015] [Google Scholar]
- Berry HL, Bowen K, Kjellstrom T. 2010. Climate change and mental health: a causal pathways framework. Int J Public Health 55 123 132, doi: 10.1007/s00038-009-0112-0 [DOI] [PubMed] [Google Scholar]
- Birk T, Rasmussen K. 2014. Migration from atolls as climate change adaptation: current practices, barriers and options in Solomon Islands. Nat Resour Forum 38 1 13, doi: 10.1111/1477-8947.12038 [DOI] [Google Scholar]
- Bowen K, Ebi K, Friel S, McMichael A. 2013. A multi-layered governance framework for incorporating social science insights into adapting to the health impacts of climate change. Glob Health Action 6 21820, doi: 10.3402/gha.v6i0.21820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks N, Adger WN. Norwich, UK: University of East Anglia; 2003. Country Level Risk Measures of Climate-Related Natural Disasters and Implications for Adaptation to Climate Change. Tyndall Centre for Climate Change Research, Working Paper 26. http://tyndall.ac.uk/sites/default/files/wp26.pdf [accessed 25 November 2015] [Google Scholar]
- Brown H, Spickett J, Katscherian D. 2014. A health impact assessment framework for assessing vulnerability and adaptation planning for climate change. Int J Environ Res Public Health 11 12896 914, doi: 10.3390/ijerph111212896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler CD, Bowles DC, McIver L, Page L. In: Climate Change and Global Health (Butler CD, ed) Wallingford, UK: CABI; 2014. Mental health, cognition and the challenge of climate change. pp. 251–259. [Google Scholar]
- Butler CD, Harley D. 2010. Primary, secondary and tertiary effects of eco-climatic change: the medical response. Postgrad Med J 86 230 234, doi: 10.1136/pgmj.2009.082727 [DOI] [PubMed] [Google Scholar]
- Campbell JR. 2014. Climate-change migration in the Pacific. Contemp Pac 26 1 28, doi: 10.1353/cp.2014.0023 [DOI] [Google Scholar]
- CartoGIS, College of Asia and Pacific, The Australian National University. Pacific EEZ Zones. 2016 http://asiapacific.anu.edu.au/mapsonline/base-maps/pacific-eez-zones [accessed 25 November 2015]
- Central Intelligence Agency. CIA World Factbook 2012. 2012 https://www.cia.gov/library/publications/the-world-factbook/ [accessed 25 November 2015]
- Confalonieri UEC, Marinho DP, Rodriguez RE. 2009. Public health vulnerability to climate change in Brazil. Clim Res 40 175 186, doi: 10.3354/cr00808 [DOI] [Google Scholar]
- Costello A, Abbas M, Allen A, Ball S, Bell S, Bellamy R, et al. 2009. Managing the health effects of climate change: Lancet and University College London Institute for Global Health Commission. Lancet 373 1693 1733, doi: 10.1016/S0140-6736(09)60935-1 [DOI] [PubMed] [Google Scholar]
- Ebi KL 2014. National and global monitoring and surveillance systems for the health risks of global change. In: Global Environmental Change (Freedman B, ed) NewYork: Springer; 649 655, doi: 10.1007/978-94-007-5784-4 [DOI] [Google Scholar]
- Friel S, Bowen K, Campbell-Lendrum D, Frumkin H, McMichael AJ, Rasanathan K. 2011. Climate change, noncommunicable diseases, and development: the relationships and common policy opportunities. Annu Rev Public Health 32 133 147, doi: 10.1146/annurev-publhealth-071910-140612 [DOI] [PubMed] [Google Scholar]
- Füssel HM. 2007. Adaptation planning for climate change: concepts, assessment approaches, and key lessons. Sustain Sci 2 265 275, doi: 10.1007/s11625-007-0032-y [DOI] [Google Scholar]
- Galea G, Powis B, Tamplin SA. Healthy islands in the Western Pacific—international settings development. Health Promot Int. 2000;15:169–178. [Google Scholar]
- Ganten D, Haines A, Souhami R. 2010. Health co-benefits of policies to tackle climate change. Lancet 376 1802 1804, doi: 10.1016/S0140-6736(10)62139-3 [DOI] [PubMed] [Google Scholar]
- Haines A, Ebi KL, Smith KR, Woodward A. 2014. Health risks of climate change: act now or pay later. Lancet 384 1073 1075, doi: 10.1016/S0140-6736(14)61659-7 [DOI] [PubMed] [Google Scholar]
- Hanna EG, McIver L. In: Climate Change and Global Health (Butler C, ed) Wallingford, UK: CABI; 2014. Small island states – canaries in the coal mine of climate change and health. pp. 181–192. [Google Scholar]
- IPCC (Intergovernmental Panel on Climate Change) Volume I: Global and Sectoral Aspects. Contribution of Working Group II to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change (Field CB, Barros VR, Dokken DJ, Mach KJ, Mastrandrea MD, Bilir TE, et al., eds.). New York:Cambridge University Press; 2014. Climate Change 2014: Impacts, Adaptation, And Vulnerability. http://ipcc-wg2.gov/AR5/images/uploads/WGIIAR5-PartA_FINAL.pdf [accessed 25 November 2015] [Google Scholar]
- Kjellstrom T, McMichael AJ. 2013. Climate change threats to population health and well-being: the imperative of protective solutions that will last. Glob Health Action 6 20816, doi: 10.3402/gha.v6i0.20816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovats S, Ebi KL, Menne B. Copenhagen, Denmark: World Health Organization; 2003. Methods of assessing human health vulnerability and public health adaptation to climate change. http://www.euro.who.int/__data/assets/pdf_file/0009/91098/E81923.pdf [accessed 25 November 2015] [Google Scholar]
- Kovats RS, Hajat S. 2008. Heat stress and public health: a critical review. Annu Rev Public Health 29 41 55, doi: 10.1146/annurev.publhealth.29.020907.090843 [DOI] [PubMed] [Google Scholar]
- Lawler J. Bangkok, Thailand: UNICEF East Asia and Pacific Regional Office; 2011. Children’s Vulnerability to Climate Change and Disaster Impacts in East Asia and the Pacific. http://www.unicef.org/environment/files/Climate_Change_Regional_Report_14_Nov_final.pdf [accessed 25 November 2015] [Google Scholar]
- Locke JT. 2009. Climate change-induced migration in the Pacific Region: sudden crisis and long-term developments. Geogr J 175 171 180, doi: 10.1111/j.1475-4959.2008.00317.x [DOI] [Google Scholar]
- Mannava P, Abdullah A, James C, Dodd R, Annear PL. 2015. Health systems and noncommunicable diseases in the Asia-Pacific region: a review of the published literature. Asia Pac J Public Health 27 NP1 19, doi: 10.1177/1010539513500336 [DOI] [PubMed] [Google Scholar]
- McIver L, Hashizume M, Kim H, Honda Y, Pretrick M, Iddings S, et al. 2015a. Assessment of climate-sensitive infectious diseases in the Federated States of Micronesia. Trop Med Health 43 29 40, doi: 10.2149/tmh.2014-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McIver L, Kim R, Hales S, Honda Y, Spickett J, Woodward A, et al. Manila, Philippines: WHO Western Pacific Regional Office; 2015b. Human Health and Climate Change in Pacific Island Countries. http://iris.wpro.who.int/bitstream/handle/10665.1/12399/9789290617303_eng.pdf [accessed 9 March 2016] [Google Scholar]
- McIver L, Naicker J, Hales S, Singh S, Dawainavesi A. Climate change & health in Fiji: environmental epidemiology of infectious diseases & potential for climate-based early warning systems. Fiji J Pub Health. 2012;1:7–13. [Google Scholar]
- McIver L, Woodward A, Davies S, Tibwe T, Iddings S. 2014. Assessment of the health impacts of climate change in Kiribati. Int J Environ Res Public Health 11 5224 5240, doi: 10.3390/ijerph110505224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMichael AJ. 2013. Globalization, climate change, and human health. N Engl J Med 368 1335 1343, doi: 10.1056/NEJMra1109341 [DOI] [PubMed] [Google Scholar]
- McMichael AJ, Lindgren E. 2011. Climate change: present and future risks to health, and necessary responses. J Intern Med 270 401 413, doi: 10.1111/j.1365-2796.2011.02415.x [DOI] [PubMed] [Google Scholar]
- McMichael C, Barnett J, McMichael AJ. 2012. An ill wind? Climate change, migration, and health. Environ Health Perspect 120 646 654, doi: 10.1289/ehp.1104375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neira M. 2014. The 2014 WHO conference on health and climate. Bull World Health Organ 92 546, doi: 10.2471/BLT.14.143891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parry ML, Canziani OF, Palutikof JP, van der Linden PJ, Hanson CE, eds. Cambridge, UK: Cambridge University Press; 2007. Climate Change 2007: Impacts, Adaptation and Vulnerability. Working Group II Contribution to the Fourth Assessment Report of the Intergovernmental Panel on Climate Change, 2007. http://www.ipcc.ch/pdf/assessment-report/ar4/wg2/ar4_wg2_full_report.pdf [accessed 25 November 2015] [Google Scholar]
- Reuveny R. 2007. Climate change-induced migration and violent conflict. Polit Geogr 26 656 673, doi: 10.1016/j.polgeo.2007.05.001 [DOI] [Google Scholar]
- Shubair MM, Haider M, Bassa M. Climate change and type 2 diabetes. J Endocrinol Diabetes Mellit. 2013;1:22–26. [Google Scholar]
- Spickett JT, Katscherian D. 2014. Health impacts of climate change in the Solomon Islands: an assessment and adaptation action plan. Glob J Health Sci 6 261 273, doi: 10.5539/gjhs.v6n5p261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spickett JT, Katscherian D, McIver L. 2013. Health impacts of climate change in Vanuatu: an assessment and adaptation action plan. Glob J Health Sci 5 42 53, doi: 10.5539/gjhs.v5n3p42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephenson J, Crane SF, Levy C, Maslin M. 2013. Population, development, and climate change: links and effects on human health. Lancet 382 1665 1673, doi: 10.1016/S0140-6736(13)61460-9 [DOI] [PubMed] [Google Scholar]
- UN-OHRLLS (United Nations Office of the High Representative for the Least Developed Countries, Landlocked Countries and Small Island Developing States) UN-OHRLLS Homepage. 2015 http://unohrlls.org/ [accessed 25 November 2015]
- Wolf T, Martinez GS, Cheong HK, Williams E, Menne B. 2014. Protecting health from climate change in the WHO European Region. Int J Environ Res Public Health 11 6265 6280, doi: 10.3390/ijerph110606265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woodward A, Hales S, Litidamu N, Phillips D, Martin J. Protecting human health in a changing world: the role of social and economic development. Bull World Health Organ. 2000;78:1148–1155. [PMC free article] [PubMed] [Google Scholar]
- Woodward A, Smith K, Campbell-Lendrum D, Chadee D, Honda Y, Liu Q, et al. Climate change and health: on the latest IPCC report. Lancet. 2014;383:1185–1189. doi: 10.1016/S0140-6736(14)60576-6. [DOI] [PubMed] [Google Scholar]
- (WHO) World Health Organization. Regional Framework for Action to Protect Human Health from Effects of Climate Change in the Asia-Pacific Region. 2007 http://www.wpro.who.int/entity/environmental_health/documents/docs/AsiaPacificRegionalActionPlanonCCHFinalApr2008.pdf?ua=1 [accessed 25 November 2015]
- WHO. Geneva: WHO and the Secretariat of the Pacific Community; 2009. Madang Commitment. http://www.wpro.who.int/southpacific/pic_meeting/reports/madang_commitment_2009.pdf [accessed 25 November 2015] [Google Scholar]
- WHO. Geneva: WHO; 2013a. Protecting health from climate change: vulnerability and adaptation assessment. http://www.who.int/globalchange/publications/vulnerability-adaptation/en/ [accessed 26 September 2016] [Google Scholar]
- WHO. Geneva: WHO; 2013b. WHO Guidance to Protect Health from Climate Change through Health Adaptation Planning (Villalobos Prats E, Ebi K, eds). http://www.who.int/globalchange/publications/guidance-health-adaptation-planning/en/ [accessed 25 November 2015] [Google Scholar]
- WHO. Manila, Philippines: WHO Western Pacific Region; 2013c. WHO Multi-Country Cooperation Strategy for the Pacific (2013–2017). http://www.wpro.who.int/southpacific/who_pacific_mccs.pdf [accessed 25 November 2015] [Google Scholar]


