Abstract
Aims/Introduction
Besides the aging population in China, the following have become serious public health problems: increasing urban population, lifestyle changes and diabetes. We assessed the epidemiology of type 2 diabetes mellitus in China between 2000 and 2014, and analyzed time trends to better determine the prevalence status of diabetes in China and to provide a basis for prevention and decision‐making.
Materials and Methods
In our systematic review, we searched China National Knowledge Infrastructure, Chinese VIP Information, Wanfang and PubMed databases for studies on type 2 diabetes mellitus between 2000 and 2014 in China. Two investigators extracted the data and assessed the quality of the included literature independently. We excluded studies that did not use 1999 World Health Organization criteria for diabetes. We also excluded reviews and viewpoints, studies with insufficient data, studies that were not carried out in mainland China and studies on troops, community, schools or physical examination people. We used stata 12.0 to combine the prevalence of all studies, calculated the pooled prevalence and its 95% confidence interval, and analyzed the differences among men/women, urban/rural areas and year of study. We calculated the prevalence of seven geographic areas of China, respectively, and mapped the distribution in the whole country to estimate the pooled prevalence of each area.
Results
Our search returned 4,572 studies, 77 of which satisfied the inclusion criteria. The included studies had a total of 1,287,251 participants, in which 680,574 cases of type 2 diabetes mellitus were recorded. The overall prevalence (9.1%) has been increasing since the 1970s, and it increased rapidly with age. The prevalence of the 65–74 years group was as high as 14.1%. Meanwhile, the prevalence among men/women and urban/rural areas was significantly different. The prevalence was 9.9% for men and 11.6% for women, which were significantly higher than the average at the end of the last century and the beginning of this century. The prevalence rate in urban areas (11.4%) was significantly higher than that in rural areas and in urban‐rural fringe areas, and the prevalence in rural areas (8.2%) was slightly higher than that in urban‐rural fringe areas (7.5%). In addition, the prevalence in each geographic area were estimated and mapped, which showed a large imbalance in the map.
Conclusions
Our analysis suggested that type 2 diabetes mellitus is highly prevalent in China. These results underscore the urgent need for the government to vigorously strengthen the management of diabetes prevention and control.
Keywords: China, Prevalence, Type 2 diabetes mellitus
Introduction
Type 2 diabetes mellitus is a major global health problem causing significant morbidity and mortality1. The International Diabetes Federation has predicted that the number of individuals with diabetes will increase from 240 million in 2007 to 380 million in 2025, and will further increase to 439 million in 20302, 3.
The largest developing country, China, has experienced a high‐speed scientific, technological progress and socioeconomic development in the past two decades. The number of diabetic patients is estimated to increase from 20.8 million in 2000 to 42.3 million in 20304. It is reported that China has overtaken India, and has become the top country with the highest number of people with diabetes for 92.4 million adults affected5, 6.
Since the 1970s, many diabetes epidemiology studies have been carried out both nationwide5, 7, 8, 9 and at regional levels. The prevalence of diabetes was reported to be approximately 1% in the 1980 National Diabetes Survey among 159,900 participants aged 20 years or older7, 2.5% in the 1994 China National Diabetes Survey among 224,251 participants aged between 25 and 64 years8, and 2.6% in the 2002 Fourth National Nutritional Survey among 98,509 participants aged 18 years or older, of which 4.5% were in urban areas and 1.8% were in rural areas10. These studies have documented a marked increase in the prevalence of diabetes, which use uniform diagnostic criteria. However, nationally representative data of long‐term trends are lacking because of incomparability.
Although previous comprehensive reviews11, 12, 13 had reported the prevalence of diabetes in China, these studies only reported the prevalence of diabetes, not type 2 diabetes mellitus. One review14 reported the prevalence of type 2 diabetes mellitus; however, it focused on comparing the prevalence between mainland China, Hong Kong and Taiwan.
As a result, there is a need for a comprehensive review of trends of type 2 diabetes mellitus over the past 15 years. To better understand the prevalence of type 2 diabetes mellitus, we comprehensively summarized the prevalence trends of type 2 diabetes mellitus among inland residents from 2000 to 2014. First, we calculated the overall prevalence of type 2 diabetes mellitus, the pooled prevalence of different age periods, men/women, urban/rural areas and the different year of the studies, respectively. Second, we analyzed the differences of trends among men/women, urban/rural areas and the year of the studies. Third, we calculated the prevalence of seven geographic areas of China, respectively, and mapped the distribution in the whole country. We aimed to provide data that can be used to create a management decision. Our results can provide a basis for the rational allocation of health resources and health policy planning.
Materials and Methods
Search strategy
We searched the China National Knowledge Infrastructure (CNKI), Chinese VIP Information (VIP), Wanfang and PubMed databases. Searches, which were limited to studies published between 2000 and 2014, were carried out in parallel by LLY and JS. We used the following search terms: “type 2 diabetes”, “type 2 diabetes mellitus”, “epidemiology”, “prevalence”, “morbidity”, “China” and “Chinese”.
For the China National Knowledge Infrastructure, see http://www.global.cnki.net. For Wanfang, see http://www.wanfangdata.com. For VIP, see http://en.cqvip.com.
Inclusion and exclusion criteria
The inclusion criteria were as follows: (i) the object of the study should be from mainland China, published in English or Chinese; (ii) the diagnosis criteria mentioned in the studies should be in accordance with 1999 World Health Organization criteria for diabetes15 . It was defined based on fasting capillary whole blood glucose level (≥6.1 mmol/L) or plasma glucose measurement (FPG ≥ 7.0 mmol/L and/or 2‐h postprandial blood glucose ≥11.1 mmol/L during an oral glucose tolerance test or previously diagnosed diabetes); (iii) the studies should be cross‐sectional or longitudinal, which report the prevalence of type 2 diabetes mellitus, or we can calculate the prevalence from the data provided; (iv) the population should be representative for a certain area's population (e.g., a province or city); and (v) the prevalence of type 2 diabetes mellitus should include previously known and new (undiagnosed) diabetes.
The exclusion criteria were as follows: (i) type 1 diabetes and gestational diabetes articles; (ii) studies representing a special population (e.g., troops, community, schools or physical examination people); (iii) studies involving a Chinese population, but were completed outside of mainland China; (iv) reviews, viewpoints or reports articles; (v) duplicates within and between the databases; and (vi) studies with insufficient data.
Data extraction
Two reviewers (Lili Yang, Jing Shao) read the trials, and extracted data independently according to search strategy and the inclusion/exclusion criteria. Data regarding author, title, age (including the number of cases of all age groups), study area (urban/rural), survey date, year of publication, total and sample size (number of men and women separately), diagnostic criteria and method were extracted. When the information was incomplete, we would try to contact the author to obtain the complete data. A third author (Yaoyao Bian) was consulted for the resolution of disagreements.
Quality of literature evaluation
For the evaluation of the searched studies, we used the literature quality assessment criteria proposed by Khambalia and Seen16 (Table 1).
Table 1.
Literature quality assessment criteria of literature proposed by Khambalia and Seen
| Quality score | Literature quality assessment criteria |
|---|---|
| 1 | Studies that included nationally representative data with large sample sizes (≥10,000) and that used random selection techniques |
| 2 | Studies that included large, randomly selected samples (≥1,000) from an entire state in the country |
| 3 | Studies that used random selection techniques within a specified number of sampling units (i.e., two towns and three clinics) |
| 4 | Studies that included large sample sizes (>1,000 persons), even though the samples were not randomly selected |
| 5 | Studies that included small sample sizes (<1,000 persons), even though the samples were not randomly selected |
The quality of studies was screened by sample size and whether random selection techniques were used.
Statistical analysis
We used stata 12.0 (StataCorp, College Station, TX, USA) to combine the prevalence of all studies, and calculate the pooled prevalence and its 95% confidence interval (CI). We carried out homogeneity tests for heterogeneity (size of test P > 0.1 and I 2 < 50%). If the aforementioned two conditions were satisfied, the combined test was shown as homogenous and we used a fixed effect model to carry out the meta‐analysis. When the combined tests were heterogeneous, the random effect model was used for analysis17. Subgroup analysis included age, men/women, urban/rural areas and the year of the study. We calculated the prevalence of seven geographic areas of China, respectively, and mapped the distribution in the whole country to estimate the pooled prevalence of each areas. GraphPad Prism 5 software (GraphPad Software, La Jolla, CA, USA) was used to draw the histogram and analyze the datum for investigating trends over time.
Results
Literature retrieval process and results
Our initial screening returned 3,450, 849, 193 and 80 results from the CNKI, VIP, Wanfang and PubMed, respectively. A total of 77 studies (Table S1) satisfied all the inclusion criteria (Figure 1). The main details of the studies are listed in Table S2.
Figure 1.
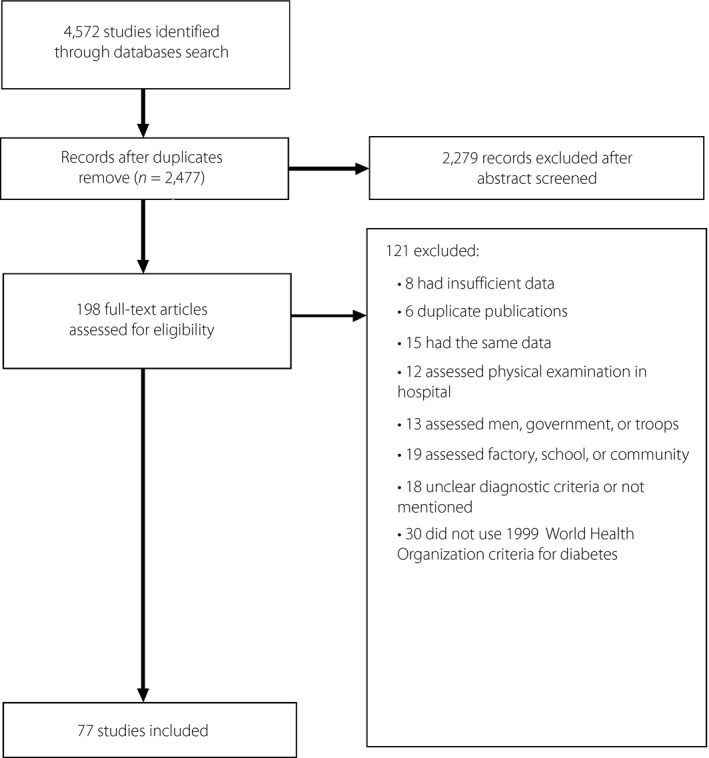
Diagram of study selection. After careful screening, a total of 77 studies were included to carry out the meta‐analysis.
We analyzed the quality of the 77 studies included as follows: three studies scored as 1, 21 studies scored as 2, 47 studies scored as 3 and the other six studies scored as 4. The total sample size of the study was 1,287,251 cases. The overall prevalence was 9.1% (95% CI 8.2–10.1%), and the heterogeneity was large (I 2 = 99.8%, P < 0.01). Among the 77 studies, the maximum sample size was 769,792 cases, whereas the minimum was 1,058 cases. Epidemiology investigation of location showed that the cases were from 20 provinces and autonomous regions, among which Zhejiang (8 cases); Shandong, Jiangsu, Shanghai (7 cases); Guangdong, Sichuan (6 cases) accounted for the top three proportions (Table S3).
Different age groups of type 2 diabetes mellitus prevalence
These data were from 77 studies that reported the prevalence for different age groups. Therefore, we adjusted the data for the purpose of comparability. For example, we pooled the 35–39 years and 40–44 years age groups into the 35–44 years group. The trend of 20–34 years to more than 75 years age groups was much more pronounced. The prevalence of type 2 diabetes mellitus increased rapidly with age (Figure 2). The prevalence rates were 0.9% (95% CI 0.6–1.2%) in the 20–34 years age group, 2.7% (95% CI 2.0–3.4%) in 35–44 years age group, 7.3% (95% CI 5.8–8.7%) in the 45–54 years age group, 11.0% (95% CI 9.0–13.0%) in the 55–64 years age group, 14.1% (95% CI 12.3–16.0%) in 65–74 years age group and 11.0% (95% CI 9.0–13.0%) in the more than 75 years age group. The highest incidence of age was observed in the 65–74 years age group (14.1%), followed by the 55–64 years and more than 75 years age groups (11.0%).
Figure 2.
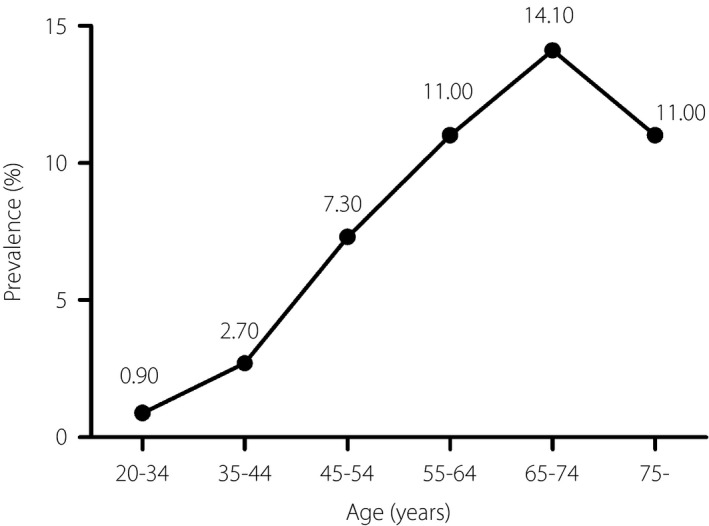
Meta‐analysis of the prevalence of different age groups. Data are point estimates of prevalence. Trends in prevalence of subgroup analysis by age.
Different periods of type 2 diabetes mellitus prevalence
According to the midpoints across time, we divided the 77 studies into three groups: 2000–2004, 2005–2009 and 2010–2014 for the purpose of comparability. We analyzed the type 2 diabetes mellitus prevalence in each group, and the pooled prevalence rates of the groups were as follows: 7.1% (95% CI 5.4–8.8%), 9.3% (95% CI 7.7–11.0%), and 10.1% (95% CI 8.4–11.7%) for 2000–2004, 2005–2009 and 2010–2014, respectively. Therefore, the type 2 diabetes mellitus prevalence trended over time (Figure 3).
Figure 3.
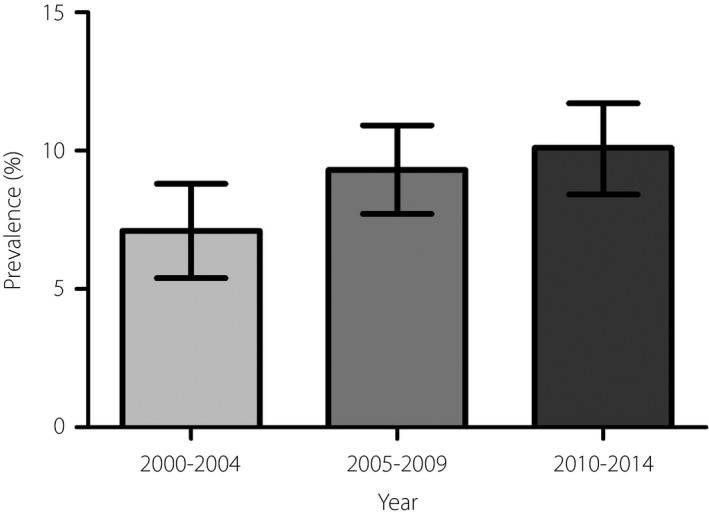
Meta‐analysis of the prevalence of different periods. Data are expressed as point estimates (95% confidence intervals) of prevalence. Trends in prevalence of subgroup analysis by different year group.
Different prevalence rates of type 2 diabetes mellitus among men and women
Of the 77 included studies, 70 studies reported the prevalence of type 2 diabetes mellitus among men and women. Meta‐analysis showed that the pooled prevalence rates were as follows: 9.9% (95% CI 8.8–11.0%) and 11.6% (95% CI 10.0–13.1%) for the men and women, respectively. The pooled prevalence was higher in women than in men. Figure 4 shows the men/women prevalence during the study year range 2000–2014. The prevalence rates of men were 6.9% (95% CI 5.4–8.5%) in 2000–2004, 9.8% (95% CI 7.9–11.7%) in 2005–2009 and 11.8% (95% CI 9.2–14.5%) in 2010–2014. Whereas, the prevalence rates of women were 6.6% (95% CI 4.3–8.8%) in 2000–2004, 13.6% (95% CI 9.8–17.3%) in 2005–2009 and 11.8% (95% CI 9.1–14.5%) in 2010–2014.
Figure 4.
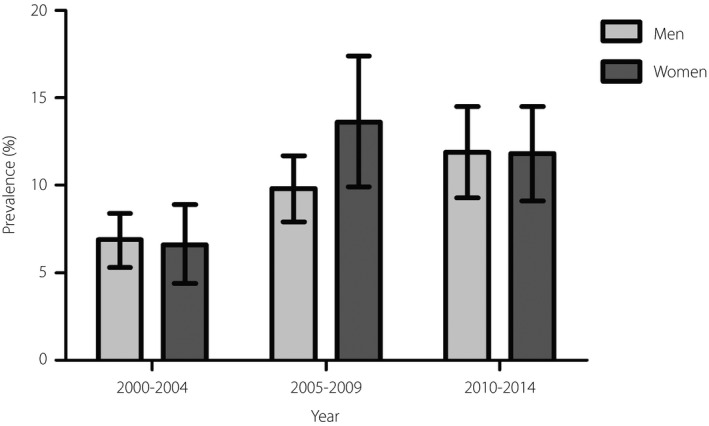
Men/women‐related type 2 diabetes mellitus prevalence during the study year 2000–2014. Data are expressed as point estimates (95% confidence intervals) of prevalence. Trends in prevalence of subgroup analysis by men/women and different year group.
Different age groups and periods of type 2 diabetes mellitus prevalence rates among men and women
We estimated the prevalence among three periods (2000–2004, 2005–2009, 2010–2014) and five age groups (20–34 years to 65–74 years) in both men and women. It increased with age and increased significantly. The rising trend of the prevalence of type 2 diabetes mellitus was different (Figure 5).
Figure 5.
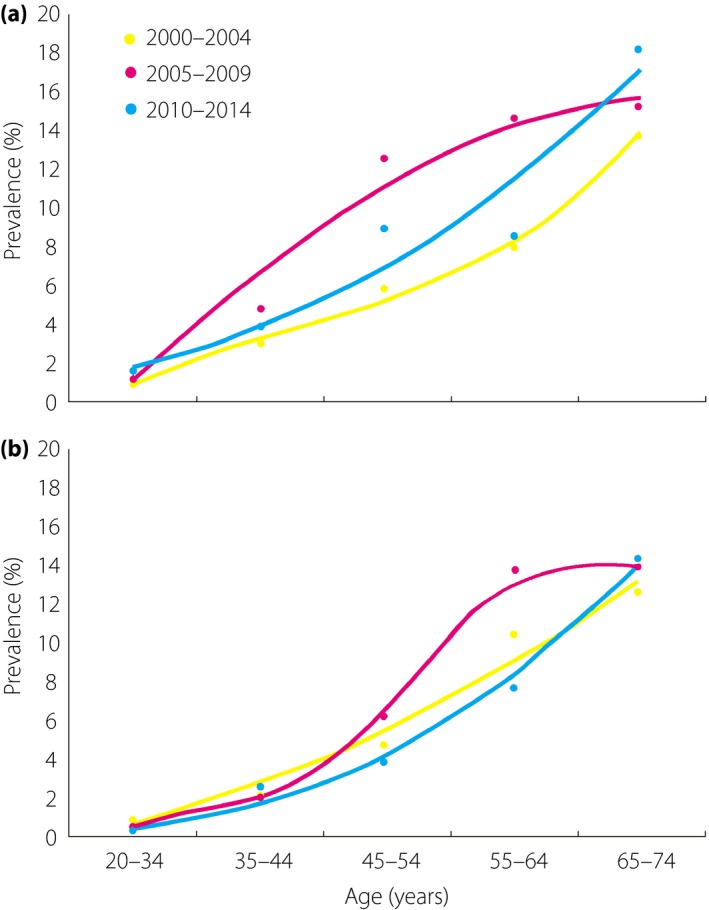
Prevalence of type 2 diabetes mellitus in (a) men and (b) women by different age groups and periods. Data are point estimates of prevalence. Trends in prevalence of subgroup analysis by age, male/female and different year group.
In 2000–2004, the prevalence rates of men were 0.9% (95% CI 0.3–1.5%) in the 20–34 years age group, 3.0% (95% CI 1.3–4.7%) in the 35–44 years age group, 5.7% (95% CI 2.6–8.8%) in the 45–54 years age group, 8.0% (95% CI 6.3–9.8%) in the 55–64 years age group and 13.9% (95% CI 12.4–15.4%) in the 65–74 years age group. In 2005–2009, the prevalence rates of men were 1.5% (95% CI 0.8–2.2%) in the 20–34 years age group, 4.7% (95% CI 0.8–8.6%) in the 35–44 years age group, 12.5% (95% CI 4.0–21.0%) in the 45–54 years age group, 14.4% (95% CI 11.1–17.6%) in the 55–64 years age group and 15.3% (95% CI 11.5–19.1%) in the 65–74 years age group. In 2010–2014, the prevalence rates of men were 1.6% (95% CI 0.2–3.0%) in the 20–34 years age group, 3.9% (95% CI 1.2–6.7%) in the 35–44 years age group, 9.1% (95% CI 2.5–15.7%) in the 45–54 years group, 8.5% (95% CI 2.6–14.3%) in the 55–64 years age group and 18.2% (95% CI 11.2–25.2%) in the 65–74 years age group.
Whereas in 2000–2004, the prevalence rates of women were 1.1% (95% CI 0.6–1.6%) in the 20–34 years age group, 2.7% (95% CI 1.2–4.1%) in the 35–44 years age group, 5.7% (95% CI 2.6–8.9%) in the 45–54 years group, 12.6% (95% CI 9.4–15.7%) in the 55–64 years age group and 15.2% (95% CI 11.5–19.0%) in the 65–74 years age group. In 2005–2009, the prevalence rates of women were 0.6% (95% CI 0.3–0.9%) in the 20–34 years age group, 2.5% (95% CI 1.3–3.6%) in the 35–44 years age group, 7.8% (95% CI 6.1–9.6%) in the 45–54 years age group, 16.7% (95% CI 12.7–20.7%) in the 55–64 years age group and 17.0% (95% CI 12.2–21.7%) in the 65–74 years age group. In 2010–2014, the prevalence rates of women were 0.5% (95% CI 0.1–0.9%) in the 20–34 years age group, 3.2% (95% CI 0.3–6.0%) in the 35–44 years age group, 4.8% (95% CI 1.4–8.2%) in the 45–54 years age group, 9.4% (95% CI 3.7–15.1%) in the 55–64 years age group and 17.4% (95% CI 8.5–26.4%) in the 65–74 years age group.
The general trend in men and women was that the prevalence in 2005–2009 was higher than both in 2000–2004 and in 2010–2014 at the age of 45–54 years and 55–64 years. The difference between men and women was inconsistent too. The prevalence rat of men was higher than that of women at the age of 35–54 years in 2005–2009.
Different prevalence rates of type 2 diabetes mellitus in urban/rural areas
Meta‐analysis showed that the pooled prevalence rates were 11.4% (95% CI 9.5–13.3%), 8.2% (95% CI 6.3–10.0%), and 7.5% (95% CI 6.2–8.9%) for urban, rural and urban‐rural fringe areas, respectively. The prevalence rate in urban area was significantly higher than that in rural areas and in urban‐rural fringe areas, and the prevalence in rural areas was slightly higher than that in urban‐rural fringe areas. Figure 6 shows the prevalence in urban/rural areas during the study years 2000–2014. The prevalence rates in urban areas were 8.9% (95% CI 6.8–10.9%) in 2000–2004, 11.3% (95% CI 8.3–14.4%) in 2005–2009 and 13.6% (95% CI 10.2–17.0%) in 2010–2014; in rural areas were 6.1% (95% CI 0.1–12.9%) in 2000–2004, 8.3% (95% CI 5.5–11.2%) in 2005–2009 and 8.2% (95% CI 5.8–10.6%) in 2010–2014; and in urban‐rural fringe areas were 5.9% (95% CI 2.9–8.9%) in 2000–2004, 7.4% (95% CI 4.9–10%) in 2005–2009 and 9.2% (95% CI 6.2–12.1%) in 2010–2014.
Figure 6.
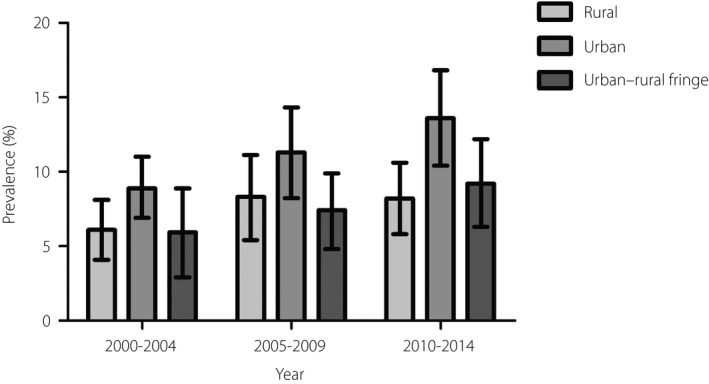
Prevalence in urban/rural areas during the study years 2000–2014. Data are expressed as point estimates (95% confidence intervals) of prevalence. Trends in prevalence of subgroup analysis by urban/rural and different year group.
Different prevalence rates of type 2 diabetes mellitus in geographic areas
A total of 77 included studies involved three national studies. The main details of the other 74 studies are listed in Table S2. Figure 7 shows the imbalance prevalence of type 2 diabetes mellitus in different geographic areas for the past 15 years; that is, Northeast China, North China, East China, South China, Central China, Northwest China and Southwest China, the pooled prevalence rates of type 2 diabetes mellitus were as follows: 22.1% (95% CI 8.0–3.6%), 11.5% (95% CI 9.6–13.3%), 8.1% (95% CI 6.8–9.4%), 8.4% (95% CI 5.1–11.8%), 8.4% (95% CI 9.7–8.3%), 6.4% (95% CI 4.8–7.9%) and 8.9% (95% CI 6.4–11.4%), respectively. Northeast China including Heilongjiang (30.6%) and Jilin (17.9%) had the highest prevalence of diabetes. Whereas in Northwest China the prevalence of type 2 diabetes mellitus was low, such as Ningxia (5.7%) and Xinjiang (6.8%).
Figure 7.
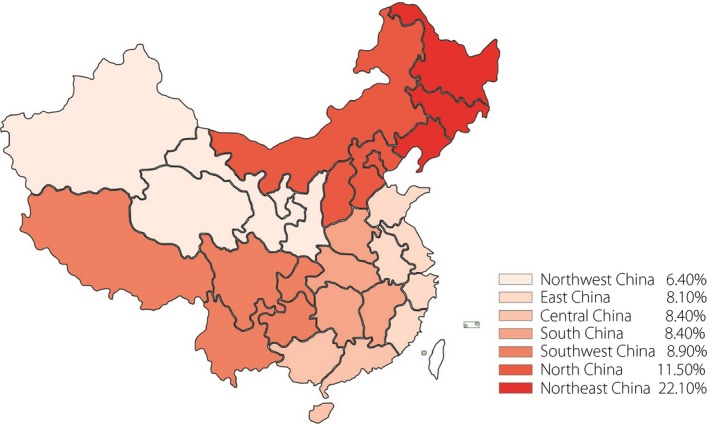
Prevalence of type 2 diabetes mellitus in geographic areas. Data are expressed as point estimates of prevalence. Trends in prevalence of subgroup analysis by geographic areas. The deeper the color, the higher the prevalence.
Discussion
The present meta‐analysis showed that the overall prevalence of type 2 diabetes mellitus was 9.1%, being nearly consistent with the study (9.7%)5. The stratified analysis showed that type 2 diabetes mellitus prevalence increased significantly, which was 7.1% in 2000–2004, 9.3% in 2005–2009 and 10.1% in 2010–2014. The data showed that the prevalence of type 2 diabetes mellitus has increased gradually in the past 15 years. We also found that the prevalence is increasing more quickly than other Asian countries (i.e., India, Pakistan, Indonesia)18, 19.
According to age groups among men and women, the prevalence rate at the age of 55–74 years was six‐ to sevenfold higher than that of 20–34 years. Age might be a major factor for diabetes. As China's population enters the 21st century, the Chinese government has faced the consequences of rapid population aging and needs to pay more attention to health services for the aging population.
In addition, the prevalence rates in men increased linearly in the past 15 years. The prevalence was 9.9% for men and 11.6% for women, and these rates were significantly higher than the average at the end of the last century and the beginning of this century. Some researchers have suggested a 26% increase in risk for men than women20. The increasing incidence has been attributed ecologically to an increasing prevalence of central obesity, total dietary intake, a shift in the ratio of refined vs unrefined carbohydrates and simple sugars, increased portion sizes, and decrease in energy expenditure21, 22. In 2005–2009, the prevalence was 13.6% in women and 9.8% in men, which is not similar to the results of the study reported by Yang et al.5. This might be due to a lack of exercise among women, and irrational dietary structure and irregular lifestyle. For example, consuming too much sugar‐sweetened beverages, such as soft drink and fruit juice, might increase the risk of developing hyperglycemia23. However, in 2000–2004 and 2010–2014, the prevalence rates were similar to the result of another study12.
China has experienced high‐speed socioeconomic development during the past two decades, which has resulted in rapid modernization and urbanization. Simultaneously, the prevalence rate differs in urban/rural areas. The prevalence rate in urban areas (13.6%) in 2010–2014 increased by 2.3% from the prevalence rate (11.3%) in 2005–2009, and these rates were significantly higher than those in the rural, urban‐rural fringe areas. This result is consistent with the findings of previous studies carried out among different populations and in different areas8, 9, 24, 25, 26 . Residents of urban areas were more sedentary and more exposed to high‐calorie foods than residents of rural areas27.
We also found that the prevalence in the whole country is imbalance in geographic areas from the map, and not directly related to the number of studies. The prevalence was as high as 30.6% in Heilongjiang and 17.9% in Jilin, whereas in some provinces the prevalence was as low as 3.6% in Yunnan and 5.7% in Ningxia. Zhejiang (8 cases) accounted for the top one proportion and its prevalence was 5.9%, which was much lower than Hunan (1 case) and its prevalence was 12.5%.
There were some important limitations in our review. First, although we selected studies carried out in nearly 20 provinces and autonomous regions, just three studies were carried out throughout the whole country. Our sample size was very small for China, which has a large population. Many studies did not provide prevalence data disaggregated by men/women and urban/rural location, which might cause sampling bias and publication bias. Second, an obviously imbalanced geographical variation existed, and the highest type 2 diabetes mellitus prevalence rate was recorded in Northeast China. These limitations caused difficulties during data analysis and result comparisons of the different studies because of inconsistencies in the age group. Third, in order to understand the relationship between prevalence and age, we categorized age groups for the purpose of comparability. For example, we pooled the 35–39 years and 40–44 years group into the 35–44 years group. In addition, the trend of the 20–34 years to more than 75 years age groups was much more pronounced. However, some studies did not categorize as such. It might cause publication bias.
To carry out an epidemiological survey of diabetes more scientifically in our country, we suggest that the relevant academic departments or agencies should formulate a unified method and age group.
In summary, the present results showed that diabetes is highly prevalent in China. Given its large population, China might bear a higher diabetes‐related burden than any other countries28. Carrying out publicity campaigns and diabetes prevention measures is considerably significant. The government should continue to boost diabetes awareness and promote healthy behavior among citizens. Health education and regular screening should also be carried out to increase the rates of diabetes identification.
Disclosure
The authors declare no conflict of interest.
Supporting information
Table S1 | The full list of studies included in the meta‐analysis.
Table S2 | Main details of the studies included in the meta‐analysis.
Table S3 | The description of geographic distributions in the subgroup analysis.
Acknowledgments
This study was supported by the National Natural Science Foundation (81271668), and the Ministry of Science and Technology Innovation Fund Projects (12C26213202418).
J Diabetes Investig 2016; 7: 845–852
References
- 1. King H, Rewers M. Global estimates for prevalence of diabetes mellitus and impaired glucose tolerance in adults. WHO Ad Hoc Diabetes Reporting Group. Diabetes Care 1993; 16: 157–177. [DOI] [PubMed] [Google Scholar]
- 2. Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract 2010; 87: 4–14. [DOI] [PubMed] [Google Scholar]
- 3. International Diabetes Federation . Diabetes Atlas, 3rd edn International Diabetes Federation, Brussels, 2006. [Google Scholar]
- 4. Boutayeb A, Boutayeb S. The burden of non‐communicable diseases in developing countries. Int J Equity Health 2005; 4: 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Yang W, Lu J, Weng J, et al Prevalence of diabetes among men and women in China. N Engl J Med 2010; 362: 1090–1101. [DOI] [PubMed] [Google Scholar]
- 6. Guariguata L, Whiting DR, Hambleton I, et al Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res Clin Pract 2014; 103: 137–149. [DOI] [PubMed] [Google Scholar]
- 7. National Diabetes Research Group . Diabetes mellitus survey of 300,000 in fourteen provinces and cities of China. Chin Med J 1981; 20: 678–681. [Google Scholar]
- 8. Pan XR, Yang WY, Li GW, et al Prevalence of diabetes and its risk factors in China, 1994. Diabetes Care 1997; 20: 1664–1669. [DOI] [PubMed] [Google Scholar]
- 9. Gu D, Reynolds K, Duan X, et al Prevalence of diabetes and impaired fasting glucose in the Chinese adult population: International Collaborative Study of Cardiovascular Disease in Asia(InterASIA). Diabetologia 2003; 46: 1190–1198. [DOI] [PubMed] [Google Scholar]
- 10. Ministry of Public Health . Nutrition and Health status Among Chinese: Result from the Fourth China Nutrition and Health Survey. Ministry of Public Health, Beijing, 2004. [Google Scholar]
- 11. Zuo H, Shi Z, Hussain A. Prevalence, trends and risk factors for the diabetes epidemic in China: a systematic review and meta‐analysis. Diabetes Res Clin Pract 2014; 104: 63–72. [DOI] [PubMed] [Google Scholar]
- 12. Li MZ, Su L, Liang BY, et al Trends in prevalence, awareness, treatment, and control of diabetes mellitus in mainland China from 1979 to 2012. Int J Endocrinol 2013; 2013: 753150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Li H, Oldenburg B, Chamberlain C, et al Diabetes prevalence and determinants in adults in China mainland from 2000 to 2010: a systematic review. Diabetes Res Clin Pract 2012; 98: 226–235. [DOI] [PubMed] [Google Scholar]
- 14. Wong KC, Wang Z. Prevalence of type 2 diabetes mellitus of Chinese populations in Mainland China, Hong Kong, and Taiwan. Diabetes Res Clin Pract 2006; 73: 126–134. [DOI] [PubMed] [Google Scholar]
- 15. Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med 1998; 15: 539–553. [DOI] [PubMed] [Google Scholar]
- 16. Khambalia AZ, Seen LS. Trends in overweight and obese adults in Malaysia (1996‐2009): a systematic review. Obes Rev 2010; 11: 403–412. [DOI] [PubMed] [Google Scholar]
- 17. Grant A, Cody D, Glazener C. Cochrane Incontinence Group. Cochrane Library.
- 18. International Diabetes Federation . IDF Diabetes Atlas, 4th edn International Diabetes Federation, Brussels, 2009. [Google Scholar]
- 19. International Diabetes Federation . IDF Diabetes Atlas, 1st edn International Diabetes Federation, Brussels, 2000. [Google Scholar]
- 20. Chinese Diabetes Society . Guidelines for the prevention and treatment of type 2 diabetes in China (2013). Chin Diabetes World 2014; 8: 298–311. [Google Scholar]
- 21. Imperatore G, Boyle JP, Thompson TJ, et al Projections of type 1 and type 2 diabetes burden in the U.S. population aged <20 years through 2050: dynamic modeling of incidence, mortality, and population growth. Diabetes Care 2012; 35: 2515–2520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Popkin BM, Nielsen SJ. The sweetening of the world's diet. Obes Res 2003; 11: 1325–1332. [DOI] [PubMed] [Google Scholar]
- 23. Schulze MB, Manson JE, Ludwig DS, et al Sugar‐sweetened beverages, weight gain, and incidence of type 2 diabetes in young and middle‐aged women. JAMA 2004; 292: 927–934. [DOI] [PubMed] [Google Scholar]
- 24. Qiao Q, Hu G, Tuomilehto J, et al Age‐ and sex‐specific prevalence of diabetes and impaired glucose regulation in 11 Asian cohorts. Diabetes Care 2003; 26: 1770–1780. [DOI] [PubMed] [Google Scholar]
- 25. Xiang HD, Wu W, Liu CQ, et al An epidemiological study on DM 1995‐1996, in China. Chin J Diabetes 1998; 6: 131–133. [Google Scholar]
- 26. Diabetes Research Cooperation Group of National . A survey of diabetes prevalence in middle‐aged and elderly Chinese from 12 areas of China. Chin J Endocrinol Metab 2002; 18: 280–284. [Google Scholar]
- 27. Wang Y, Mi J, Shan XY, et al Is China facing an obesity epidemic and the consequences? The trends in obesity and chronic disease in China. Int J Obes (Lond) 2007; 31: 177–188. [DOI] [PubMed] [Google Scholar]
- 28. Wild S, Roglic G, Green A, et al Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care 2004; 27: 1047–1053. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1 | The full list of studies included in the meta‐analysis.
Table S2 | Main details of the studies included in the meta‐analysis.
Table S3 | The description of geographic distributions in the subgroup analysis.


