Abstract
Food allergies and intolerances have increased during the last decades and regulatory authorities have taken different measures to prevent and manage consumers’ adverse reactions, including correct labelling of foods. Aim of this work was to search for soybean and lactose in meat products and meat preparations taken from retail in some provinces of Campania Region (Southern Italy) and to evaluate the food labels compliance with Regulation (EU) n.1169/2011. Soybean and lactose were searched using commercial kits in n. 58 samples of meat products produced in or distributed by 19 establishments, and in n. 55 samples of meat products and n. 8 of meat preparations produced in 21 plants. All samples were selected on the basis of the absence of any information on the labels about the presence of the two searched allergens, with the exception of n. 5 samples tested for lactose. Traces of soybean were detected in 50 out of the 58 examined samples, at concentrations up to 0.93 mg kg–1. Only two samples contained levels above the detection limit of 0.31 mg kg–1. Lactose levels ranging from 0.11 to 2.95 g/100 g, i.e. above the detection limit, were found in all the tested samples (n. 63). The results of the present research underline the need for careful controls and planning by operators as part of the self-control plans, and deserve attention from the competent authorities considering not only the consumers’ health but also the great attention media pay to regulations providing consumers with information on food.
Key words: Food allergy, Food intolerance, Soybeans, Lactose
Introduction
During the last decades food allergies (FA) and food intolerances (FI) have increased (Nwaru et al., 2014) especially in children (Vargas et al., 2011), even if estimates of their actual incidence and prevalence are uncertain. The gold standard of diagnosis – the double-blind placebo-controlled food challenge (DBPCFC) – has been utilised only in a few epidemiological studies to define FA and FI (Soares-Weiser et al., 2014). Most estimates are based on self-diagnosis or specific immunoglobulin E (IgE) or skin-prick test sensitisation to common food allergens, tests that are both known to overestimate the actual frequency of FA and FI (Nwaru et al., 2014).
People with FA and FI suffer symptoms that affect both their health and lifestyle (Cummings et al., 2010). Hence, there is considerable interest in reducing the exposure risk and informing consumers on the first signs of an allergic reaction (De Silva et al., 2014) so that they can treat themselves or seek qualified medical attention. Symptoms may be mild and limited to the oral cavity but also generalised and severe allergic reactions may occur, sometimes involving multiple organs and systems such as the skin and mucosal tissues and the gastrointestinal, respiratory and cardiovascular tracts (Versluis et al., 2015).
Regulatory authorities generally require measures to control FA and FI such as proper store and management of some foods and ingredients, control programmes and good manufacturing practices to minimise the chance of cross-contamination in the processing facilities. Some manufacturers have always used a precautionary labelling on a voluntary basis to alert consumers that some products might be subject to accidental contaminations. Appropriate labelling of foods containing substances or products causing allergies and intolerances is indeed essential to help people to prevent and manage food adverse reactions.
In the European Union (EU) labelling of all foods and ingredients causing allergies and intolerances is established by Regulation (EU) No 1169/2011 (European Commission, 2011). Annex II of this regulation contains a list of ingredients or other substances or products (such as processing aids) with a scientifically proven allergenic or intolerance effect, that must be indicated on the labels, when used in the production of foods and still present therein, to enable consumers, particularly those suffering from a food allergy or intolerance, to make informed choices which are safe for them.
Soybeans allergy is an exaggerated immune system response to soy proteins. Symptoms may include hives, itching, swelling, eczema, vomiting, diarrhea and nausea but also, in some cases, anaphylaxis, which is potentially life-threatening either by breathing difficulties and/or a sudden drop in blood pressure (Sicherer et al., 2000). Lactose intolerance is an adverse reaction that does not involve the immune system. Reactions can be immediate or delayed up to 20 h after ingestion. Symptoms of intolerance are sometimes vague and may include a combination of gastrointestinal problems, such as bloating and wind, diarrhea, nausea and indigestion, aggravation of eczema or asthma (Casellas et al., 2010; Järvelä et al., 2009; Jellema et al., 2010; Jouet et al., 1996). Soy and lactose are included in Annex II of Reg. 1169/2011 as follows: soybeans and products thereof [(except: fully refined soybean oil and fat; natural mixed tocopherols (E306), natural D-alpha tocopherol, natural D-alpha tocopherol acetate, and natural D-alpha tocopherol succinate from soybean sources; vegetable oils derived phytosterols and phytosterol esters from soybean sources; plant stanol ester produced from vegetable oil sterols from soybean sources)]; milk and products thereof (including lactose) (except: whey used for making alcoholic distillates including ethyl alcohol of agricultural origin; lactitol). Aim of this work was to search for soybean and lactose in pre-packed meat products and meat preparations and to evaluate the compliance of the food labels with the legislation in force.
Materials and Methods
Soybean protein was searched in n. 58 samples of meat products (n. 6 würstel pork, n. 2 würstel pork/beef, n. 5 würstel chicken/turkey, n. 2 würstel chicken/cheese, n. 1 würstel chicken, n. 7 mortadella, n. 3 salami Hungarian type, n. 4 salami Milano, n. 2 salami Napoli, n. 3 cooked ham, n. 4 cooked shoulder ham, n. 1 smoked bacon, n. 1 bacon non smoked, n. 1 smoked bacon slice, n. 1 diced bacon non smoked, n. 1 diced smoked bacon, n. 1 stewed bacon, n. 3 lyoner with peppers, n. 1 lyoner classical, n. 1 cotechino, n. 2 hamburger cooked ham, n. 1 cooked meat in jelly, n. 1 meat pate, n. 1 luncheon meat, n. 1 cooked turkey breast, n. 1 roasted turkey, n. 1 cooked chicken breast, n. 1 cooked chicken in jelly) produced in or distributed by 19 establishments (A, B, C, D, E, F, G, H, I, J, K, L, M, N, O, P, Q, R, S).
Fifty-five samples of meat products and n. 8 of meat preparations (Table 1) produced in 21 plants (A, B, C, T, U, V, W, X, Y, Z, AA, AB, AB, AC, AD, AE, AF, AG, AH, AI, AJ, AK) were tested for lactose. Sampling for lactose was repeated 4 months later for products still present on the market.
Table 1.
Lactose levels (g/100 g) in fifty-five samples of meat products and eight of meat preparations.
| Sample | Type | First sampling | Second sampling | Sample | Type | First sampling | Second sampling |
|---|---|---|---|---|---|---|---|
| AA59 | Würstel (pork) | 0.22 | 0.77 | AE80 | Cotechino | 0.24 | |
| B60* | Würstel (pork) | 0.40 | 0.60 | AA81 | Burger (from cooked ham) | 2.90 | |
| AJ61 | Würstel (turkey/chicken) | 0.17 | 0.11 | AI82 | Burger (chicken) | 1.42 | |
| AD62 | Würstel (turkey/chicken) | 0.55 | A83 | Roast turkey | 0.43 | ||
| AJ63 | Würstel (chicken/turkey) | 0.55 | AD84 | Roast turkey drumstick | 0.51 | 0.87 | |
| AA64 | Würstel (chicken/turkey) | 0.56 | 0.92 | Y85 | Chicken with herbs | 1.36 | 0.66 |
| AA65 | Würstel (chicken) | 0.43 | 0.92 | AC86 | Chicken with herbs | 0.32 | 0.56 |
| AF66 | Mortadella | 2.95 | 0.78 | AK87 | Chicken fillet | 0.57 | |
| AB67 | Mortadella | 0.23 | 0.64 | AA88 | Valtellina Bresaola | 0.39 | 0.73 |
| AH68° | Mortadella | 0.27 | 0.56 | U92 | Halal kebab and white sauce | 1.28 | |
| C69 | Salami Milano | 0.27 | AB93 | Speck | 0.32 | ||
| X70 | Spicy salami Napoli | 0.34 | 0.60 | AH94 | Speck | 0.49 | 0.70 |
| A71 | Salami | 0.49 | X95 | Cured ham | 0.44 | 0.66 | |
| A72* | Salami | 0.36 | 0.71 | AK96 | Cous cous salad with chicken | 0.63 | 0.70 |
| AA73 | Cooked ham on toast | 0.42 | |||||
| AA74# | Diced cooked ham (high quality) | 0.39 | 0.80 | Z89§ | Fresh sausage (turkey and chicken) | 0.41 | |
| A75 | Cooked ham (high quality) | 0.45 | W90 | Fresh sausage (pork) | 0.24 | ||
| Y76 | Cooked ham (from shoulder) | 0.33 | V91 | Fresh sausage (veal) | 0.82 | ||
| A77 | Bacon (smoked) | 0.67 | T97 | Hamburger (beef) | 0.88 | 1.24 | |
| AG78 | Bacon (not smoked) | 0.39 | 0.59 | V98 | Hamburger (veal) | 0.39 | |
| AG79 | Bacon (lightly smoked) | 0.38 | 0.71 | V99 | Hamburger (beef) | 0.34 | 0.73 |
*Label reported the product to be lactose-free
°produced in a plant where milk is used
#it may contain milk and products thereof
§it may contain milk.
All samples were collected at retail in some provinces of Campania Region (Southern Italy) and selected on the basis of the absence of any information on the labels about the presence of the two searched allergens, with the exception of n. 5 samples tested for lactose, as reported in Table 1.
The analyses were performed in the laboratory of the Food Hygiene Unit of the Department of Veterinary Medicine and Animal Production, University of Naples using the ELISA kit Ridascreen® Fast soybean (R-Biopharm, Darmstadt, Germany), a sandwich enzyme immunoassay for the quantitative analysis of native and processed soy proteins in food. The measurement is made photometrically. The absorption is proportional to the soy protein concentration in the sample.
The limit of detection is 0.31 mg kg–1 soy protein. The limit of quantification is 2.5 mg kg–1 soy protein. According to the producer’s indications there is a weak cross-reactivity of 0.0017% to legumes of the tribe Phaseoleae (various species of beans) and to legumes of the genus Vicia (0.0003%). There is no cross-reactivity to other legumes like peanut, lentil, pea, lupine as well as milk (casein, (β-lac-toglobulin) or egg proteins.
Soybean was determined according to the manufacturer’s instructions (www.r-bio-pharm.com). A spectrophotometer Sirio S Reader (Seac Radim Company, Calenzano, Italy) was used. Allergen concentration was calculated by use of a cubic spline function with the aid of the specific program Ridawin® software.
The UV-method kit lactose/D-galactose used for lactose is an enzymatic method (Boehringer Mannheim/R-Biopharm, Darmstadt, Germany). Lactose is hydrolysed to D-glucose and D-galactose at pH 6.6 in the presence of the enzyme β-galactosidase and water. D-galactose is oxidised at pH 8.6 by nicotinamide-adenine dinucleotide (NAD) to Dgalactonic acid in the presence of the enzyme β-galactose dehydrogenase. The amount of reduced NAD formed in reaction is stoichiometric to the amount of lactose, and D-galactose. The detection limit is 7 mg L–1.
Lactose was determined according to the manufacturer’s instructions (www.r-bio-pharm.com) using a spectrophotometer UV/Vis Jasco model V-530 (Jasco, Oklahoma City, OK, USA).
Results and Discussion
Soybean concentrations ranged from non-detectable levels up to 0.93 mg kg–1. Levels above the detection limit of 0.31 mg kg–1 were found only in two samples, one würstel from chicken and turkey (0.41 mg kg–1) and one cooked turkey breast (0.93 mg kg–1), produced in two different establishments.
Lactose levels ranged from 0.11 up to 2.95 g/100 g. The concentrations were lower than 1 g/100 g in n. 57 samples (90.47%) and lower than 2 g/100 g in n. 4 food items (6.35%). In the remaining two samples, one mortadella and one burger from cooked ham, levels of 2.95 and 2.90, respectively, were observed (Table 1, Figure 1).
Figure 1.
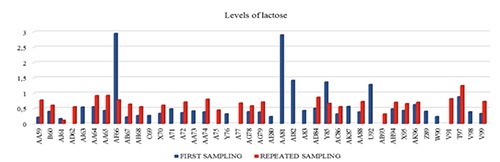
Lactose levels (g/100 g) in fifty-five samples of meat products and eight samples of meat preparations. AA59, AJ61, AJ63, AA65, würstel; AB67, mortadella; C69, salami Milano; A71, salami; AA73, A75, cooked ham; A77, AG79, bacon; AA81, burger; A83, roast turkey; Y85, AK87, chicken; U92, halal kebab; AH94, speck; AK96, cous cous salad; W90, fresh sausage (pork); T97, V99, hamburger.
On the whole, following the described screening method, most examined samples were suspected positive to the searched allergens.
Soybean traces were found in 50 out of 58 examined samples but no indication for soy was present in the labels of these products even if indications on the presence/absence of many other allergens, mainly gluten, milk and products thereof, mustard, celery, pistachio, were reported. Renčová and Tremlová (2009), using an indirect competitive ELISA method, searched soy proteins in 131 heat-processed meat product samples randomly purchased in the market chain of the Czech Republic and detected the allergen in 84% of the samples. Jankovica et al. (2015), using commercial ELISA kits, detected the presence of soybean in 29 out of 100 samples of different meat products (boiled sausages with different composition, fermented sausages, meat tins) taken from retail shops. No declaration concerning the allergen was reported in the labels of the samples examined in both researches.
Lactose levels above the detection limit were found in all the 63 samples tested for this substance even if indications concerning its presence were given only in the following five products (using different wordings): würstel from pork B60 and salami A72 reported lactose free; mortadella AH68 reported produced in a plant where milk is used; diced cooked ham of high quality AA74 reported it may contain milk and products thereof, and fresh sausage from turkey and chicken Z89 reported it may contain milk. Lactose was found in the four above mentioned meat products also at the second sampling and even at higher levels. This observation applies, however, to nearly all samples examined at the second control since higher (sometimes double) concentrations than those found at the first sampling were detected in 18 out of the 21 examined samples.
The different wordings used to indicate the presence of traces protect food business operators from disputes following the consumption of their products but rely on the choice of the allergic consumer, who becomes the only responsible for the assumption of the food. In this regard it is interesting the outcome of the EFSA scientific opinion on lactose thresholds in lactose intolerance and galactosaemia (EFSA, 2010). The document reports that, according to the systematic review by Wilt et al. (2010), most individuals diagnosed with lactose intolerance or lactose maldigestion can tolerate 12 g of lactose as a single dose, particularly if taken with food, with no or minor symptoms. Single doses of 24 g usually lead to appreciable symptoms. There is some evidence that many lactose maldigesters tolerate daily doses of 20 to 24 g of lactose if distributed throughout the day and consumed together with other nutrients. This notwithstanding, the Panel on Dietetic Products, Nutrition and Allergies concludes that a single threshold of lactose for all lactose intolerant subjects cannot be determined owing to the great variation in individual tolerances since symptoms of lactose intolerance have been described after intake of <6 g of lactose in some subjects. Some EU Member States have set at national level lactose thresholds for foodstuffs other than those intended for infants. Denmark, Estonia, Finland, Norway, Sweden, Germany, Slovenia, Hungary set levels ranging from 10 to 100 mg/100 g final product for the use of the term lactose-free, while levels of 1 g/100 g final product were established in Denmark, Estonia, Finland, Norway, Sweden, Ireland for the term low lactose (EFSA, 2010). According to these values most examined samples might be marked as low lactose, whereas for none of them the wording lactose-free might be used.
The presence of allergens in traces is not a rare result and might be due to different reasons, including contaminated raw materials, accidental cross-contamination, manufacturing facilities that, despite a routine cleaning, still contain traces of allergens from a previous processing cycle, use of processing aids, means of transport and promiscuous installations. In many cases it is possible, even if it is not always easy, to control cross-contamination. However, it must also be recognised that it is difficult to separate the production lines that involve the use of allergens from those ones that should be free. The ideal solution would require separated lines but this is not always possible, especially in small or medium food plants.
The possibility that, due to cross-contamination, small amounts of allergenic substances may be transferred to foods that should be allergenic-free is cause of concern not only for consumers but also for food business operators. When a minimum tolerable value of a specific allergen is not specified, even if measures are in place to control contamination, it is difficult for a manufacturer to decide whether to declare the presence of traces. The request of fixing minimum tolerance thresholds is therefore strongly supported by the producers. Still, the solution of the problem is complex because it involves different skills and two conflicting requirements need to be solved: the request of the producers, especially those who cannot ensure zero contamination mainly for structural reasons, and the opinion of the scientific community, which supports that, having allergic consumers a different sensitivity to the allergens, it is not possible to define a minimum level below which the food can be considered as safe.
The problem of the cross-contamination is complicated by the risk of cross-reactivity with different allergens. In peanut-allergic patients a clinically relevant sensitisation to other legumes such as soybean, lupine, lentil, or pea occurs. In a group of 39 peanut-sensitised patients, 82,55, and 87% of patients were also sensitised to lupine, pea, and soybean, respectively, whereas, based on DBPCFC, 29-35% had symptoms to these beans (Barre et al., 2008). In a recent study, Klemans et al. (2013) showed that 60% of soy-allergic patients had a concomitant peanut allergy. The peanut allergic group often showed specific IgE to soy extract, soy 2S and Gly m 8 albumins and soy Gly m 5 and Gly m 6 cupins. Barre et al. (2007) built models of vicilin-like allergens from peanut (Ara h 1), walnut (Jug r 2), hazelnut (Cor a 11), and cashew nut (Ana o 1) using the x-ray coordinates of soybean Gly m 5 to illustrate the structural similarity of these allergens. In addition, their study included one experiment with a pool of a number of sera from peanut-allergic patients, which indicated IgE reactivity to the three allergens Jug r 2, Cor a 11 and Ana o 1, as well as to the soybean allergen Gly m 5. For this reason, currently the only solution for food business operators is a careful application of self-monitoring plans to verify if they can guarantee the absence of traces.
Conclusions
In conclusion, the results of the present research underline the need for careful controls and planning by operators as part of the self-control plans. It also highlights the need of attention on the part of the competent authorities, considering not only the consumers’ health but also the great attention the media pay to the topic. In fact, in order to make easier and safer food choices for people suffering from food allergies and intolerances it is mandatory to indicate the presence of products or substances causing allergy and intolerance not only on the label of prepackaged products, as previously required, but also for non-pre-packaged foods sold at retail or administered at any level, including all forms of public distribution and restoration, such as catering, restaurants and canteens, to reduce the risk for allergic people whenever having a meal outside their home.
References
- Barre A, Jacquet G, Sordet C, Culerrier R, Rouge P, 2007. Homology modelling and conformational analysis of IgE-binding epitopes of Ara h 3 and other legumin allergens with a cupin fold from tree nuts. Mol Immunol 44:3243-55. [DOI] [PubMed] [Google Scholar]
- Barre A, Sordet C, Culerrier R, Rance F, Didier A, Rouge P, 2008. Vicilin allergens of peanut and tree nuts (walnut, hazelnut and cashew nut) share structurally related IgE-binding epitopes. Mol Immunol 45:1231-40. [DOI] [PubMed] [Google Scholar]
- Casellas F, Aparici A, Casaus M, Rodriguez P, Malagelada JR, 2010. Subjective perception of lactose intolerance does not always indicate lactose malabsorption. Clin Gastroenterol Hepatol 8:581-6. [DOI] [PubMed] [Google Scholar]
- Cummings AJ, Knibb RC, King RM, Lucas JS, 2010. The psychosocial impact of food allergy and food hypersensitivity in children, adolescents and their families: a review. Allergy 65:933-45. [DOI] [PubMed] [Google Scholar]
- De Silva D, Geromi M, Halken S, Host A, Panesar SS, Muraro A, Werfel K, Hoffmann-Sommergruber T, Roberts G, Cardona V, Dubois AEJ, Poulsen LK, Van Ree R, Vlieg-Boerstra B, Agache I, Grimshaw K, O’Mahony L, Venter C, Arshad SH, Sheikh A, 2014. Primary prevention of food allergy in children and adults: systematic review. Allergy 69:581-9. [DOI] [PubMed] [Google Scholar]
- EFSA, 2010. Scientific opinion on lactose thresholds in lactose intolerance and galactosaemia. EFSA J 8:1777. [Google Scholar]
- European Commission, 2011. Regulation of the European Parliament and of the Council of 25 October 2011. On the provision of food information to consumers, amending Regulations (EC) No 1924/2006 and (EC) No 1925/2006 of the European Parliament and of the Council, and repealing Commission Directive 87/250/EEC, Council Directive 90/496/EEC, Commission Directive 1999/10/EC, Directive 2000/13/EC of the European Parliament and of the Council, Commission Directives 2002/67/EC and 2008/5/EC and Commission Regulation (EC) No 608/2004, Norm 1169/2011/EU. In: Official Journal, L 304/18, 22.11.2011. [Google Scholar]
- Jankovica V, Matekalo-Sveraka V, Lakicevica B, Spirica D, Petronijevica R, 2015. Soybean and gluten in meat products: consumer protection strategy. Procedia Food Sci 5:121-4. [Google Scholar]
- Järvelä I, Torniainen S, Kolho KL, 2009. Molecular genetics of human lactase deficiencies. Ann Med 41:568-75. [DOI] [PubMed] [Google Scholar]
- Jellema P, Schellevis FG, van der Windt DA, Kneepkens CM, van der Horst HE, 2010. Lactose malabsorption and intolerance: a systematic review on the diagnostic value of gastrointestinal symptoms and self-reported milk intolerance. Q J Med 103:555-72. [DOI] [PubMed] [Google Scholar]
- Jouet P, Sabaté JM, Flourié B, Bouhnik Y, Coffin B, Francihisseur C, Rambaud JC, 1996. Lactose intolerance: role of the colon and of changes in motor activity in the occurrence of symptoms. Gastroenterology 110:335-42. [Google Scholar]
- Klemans RJ, Knol EF, Michelsen-Huisman A, Pasmans SG, de Kruijf-Broekman W, Bruijnzeel-Koomen CA, 2013. Components in soy allergy diagnostics: Gly m 2S albumin has the best diagnostic value in adults. Allergy 68:1396-402. [DOI] [PubMed] [Google Scholar]
- Nwaru BI, Hickstein L, Panesar SS, Muraro A, Werfel T, Cardona V, Dubois AEJ, Halken S, Hoffmann-Sommergruber K, Poulsen LK, Roberts G, Van Ree R, Vlieg-Boerstra BJ, Sheikh A, 2014. The epidemiology of food allergy in Europe: a systematic review and meta-analysis. Allergy 69:62-75. [DOI] [PubMed] [Google Scholar]
- Renčová E, Tremlová B, 2009. ELISA for detection of soya proteins in meat products. Acta Vet Brno 78:667-71. [Google Scholar]
- Sicherer SH, Sampson HA, Burks AW, 2000. Peanut and soy allergy: a clinical and therapeutic dilemma. Allergy 55:515-21. [DOI] [PubMed] [Google Scholar]
- Soares-Weiser K, Takwoingi Y, Panesar SS, Muraro A, Werfel T, Hoffmann-Sommergruber K, Roberts G, Halken S, Poulsen L, Van Ree R, Vlieg-Boerstra BJ, Sheikh A, 2014. The diagnosis of food allergy systematic review and meta-analysis. Allergy 69:76-86. [DOI] [PubMed] [Google Scholar]
- Vargas PA, Sicherer SH, Christie L, Keaveny M, Noone S, Watkins D, Carlisle SK, Jones SM, 2011. Developing a food allergy curriculum for parents. Pediatr Allergy Immu 22:575-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Versluis A, Knulst AC, Kruizinga AG, Michelsen A, Houben GF, Baumert JL, van Os-Medendorp H, 2015. Frequency, severity and causes of unexpected allergic reactions to food: a systematic literature review. Clin Exp Allergy 45:347-67. [DOI] [PubMed] [Google Scholar]
- Wilt TJ, Shaukat A, Shamliyan T, Taylor BC, MacDonald R, Tacklind J, Rutks I, Schwarzenberg SJ, Kane RL, Levitt M, 2010. Lactose intolerance and health. Agency for Healthcare Research and Quality ed., Rockville, MD, USA. [PMC free article] [PubMed] [Google Scholar]