Abstract
Background
Since years a discussion is held on the best approach to perform total hip replacement (THR). Risk of dislocation, abductor weakness and a possible difference in rehabilitation are mentioned. We performed this study to objectify that the use of the direct anterior approach (DAA) results in a faster rehabilitation after THR compared to the non-DAA (posterolateral and anterolateral) approach.
Methods
A single centre prospective cohort study was conducted. Pre- and 16-weeks postoperative completed PROMs like the VAS, PSC, GPE and HOOS were analyzed. A leg press and power test were performed. Functional capacity was determined by the TUG and the 6MWT.
Results
A total of 119 patients were included for analysis: 87 in the DAA group, 32 in the non-DAA group. There were no differences in general baseline characteristics. The length of stay was significant (p = .000) shorter in the DAA group. At 16 weeks, the DAA group showed a significant greater improvement with respect to the VAS and HOOS. Also significant differences for all strength, power and functional capacity parameters between the pre- and postoperative measurements were found. A subgroup analysis at 6-weeks postoperative showed significant improvements in the TUG (p = .009) and 6MWT (p = .009) in the DAA group, but not in the non-DAA group.
Conclusion
PROMs, strength, power and functional capacity tests show significant improvement in all approaches after THR. There seems to be a small advantage in favour of the DAA, in particular directly postoperative and the first postoperative weeks.
Keywords: Primary total hip replacement, Direct anterior approach, Posterolateral approach, Direct lateral approach, Anterolateral approach
1. Introduction
Total hip replacement (THR) is one of the most common orthopaedic interventions.1, 2 According to the Dutch registry, 28,026 primary THRs were performed in The Netherlands in 2014.3 The indication to perform a THR is most often osteoarthritis (87%).3 THR is a very successful intervention to decrease the amount of pain and to restore range of motion.2, 4 Since years a discussion is held on the best surgical approach to the hip joint.1, 5 The direct lateral approach (DLA) is losing popularity (20.2%)3 because often a Trendelenburg gait due to damage to the gluteus medius muscle exists after surgery.1, 6 The anterolateral approach (ALA) is currently used in 5.4% of THRs, but is losing popularity as well.3 Mostly used worldwide is the posterior or posterolateral approach (PLA). This approach does not damage the hip abductors.1, 5, 7 In The Netherlands, 61.9% of the primary THRs are placed using the PLA.3 Recently, the direct anterior approach (DAA) gains more popularity.8 In 2007, 0.1% of the THRs were placed using the DAA, increasing to 12.3% in 2014.3
The DAA is popular because of the low risk of dislocation. Soft-tissue tension is one of the factors which reduces the risk of dislocation. This tension is maintained with the anterior approach.9 In current literature dislocation after DAA was found in 0.0–1.5%.9 While PLA was found to have a risk of 1–5%, depending on capsule reconstruction.10, 11, 12 A 2% risk of dislocation was found by Sköldernberg et al. using ALA, while Tsai et al. reported no dislocations in 1077 patients.13, 14 In accordance, Sheth et al. reported significant less dislocations using the DAA or ALA compared to the PLA.15
In addition to the low risk of dislocation there are reports showing that the rehabilitation of THR using DAA is faster, because no damage is done to the tendons and muscles.4, 6 Abductor weakness and the risk of a Trendelenburg gait, is a complication which occurs regularly after DLA or ALA. Meneghini et al. showed that 6 weeks after THR with minimal invasive ALA, patients have a walking pattern revealing abductor weakness.16 Abductor weakness occurs in 4–20%.17 In contrast, the DAA is a so-called minimal invasive technique, using an interval between muscles.4 We performed this study to objectify that the use of the DAA results in a faster rehabilitation after THR compared to the other approaches.
2. Patients and methods
A single centre retrospective cohort study was conducted. In our hospital all patients scheduled for primary THR were asked to undergo measurements on a voluntary basis, performed by an independent physiotherapist (BLINDED) preoperative and 16-weeks postoperative. All patients who underwent primary THR in 2014 were included if the indication for THR was osteoarthritis, avascular necrosis, dysplasia or a rheumatological condition. Patients who underwent THR after an intracapsular fracture, failure of osteosynthesis or hemiarthroplasty were excluded. When patients underwent the preoperative measurement, but not the postoperative measurement they were excluded as well.
2.1. Approaches
Two out of five orthopaedic surgeons use the DAA (modified Smith-Peterson or Hueter approach), two others the PLA (Moore or Southern) and one a minimal invasive ALA (modified Watson-Jones).
2.2. Prosthesis
Cementless prosthesis of two different systems are used. The surgeons performing THR with the DAA use a hydroxyapatite coated stem (CORAIL Cementless, Depuy, Johnson & Johnson) with three different options: ‘standard’, ‘coxa vara’ and ‘high-offset. The acetabular component is a cementless, porous cup (Pinnacle® Duofix® HA Acetabular Shell Cementless, Depuy, Johnson & Johnson). A polyethylene or ceramic insert us used (28 mm–32 mm–36 mm). The other surgeons use a proximally coated stem (Symax Cementless, Stryker). A cementless hydroxapatite coated cup (Trident Cementless, Stryker) with a polyethylene insert (36 mm) is used.
2.3. Per- and postoperative policy
A 6-hour drain is used after DAA. In the other approaches a drain is used until the first morning after surgery when the patient is on any type of anticoagulants. All patients received the same standardized postoperative care. This consists of 24 h intravenous antibiotics, 6 weeks of antithrombotic prophylaxis (Dalteparin 5000 IE 1dd 1) and physical therapy as of the first day after surgery. Patients were allowed to bear weight as tolerated. Discharge criteria were normal X-rays, tolerable pain, an unremarkable wound and independent, save mobilization. All patients were advised to continue physical therapy in outward-clinic for at least 6 weeks postoperative.
2.4. Outcome
Pre- and postoperative completed Patient-Reported Outcome Measures (PROMs) were analyzed for every approach. With the Visual Analogue Scale (VAS) patients are asked to mark the average pain they felt in the involved hip during the previous week. The score ranges from ‘0’ (no pain at all) to ‘10’ (unbearable pain).We asked for the amount of complaints after 30 min of walking (Patient Specific Complaints, PSC), whereby ‘0’ means no problem at all to complete the activity and ‘10’ means impossible to complete the activity. The ‘Hip disability and Osteoarthritis Outcome Score’ (HOOS) was used to examine the opinion of the patients about their THR. The score will be expressed in a scale ranging from 0 to 100 whereby a low score indicates symptoms. The Global Perceived Effect (GPE) was used to measure the patient's opinion about the recovery on a 7-points scale. To determine strength and power in the involved leg, a leg press test and power test (concentric/eccentric) were performed. Functional capacity was determined by the ‘Timed-up-and-Go-Test’ (TUG) and the ‘6 minute walk-test’ (6MWT) both pre- and postoperative.
2.5. Statistical analysis
Data was analyzed using SPSS 22. Differences between pre- and postoperative parameters were compared by approach and between the anterior and non-anterior approach. A subgroup analysis was performed in patients who chose to rehabilitate with independent physiotherapy. This subgroup underwent an extra measuring moment at 6 weeks postoperative. Independent Sample t-tests and repeated-ANOVA tests were performed.
3. Results
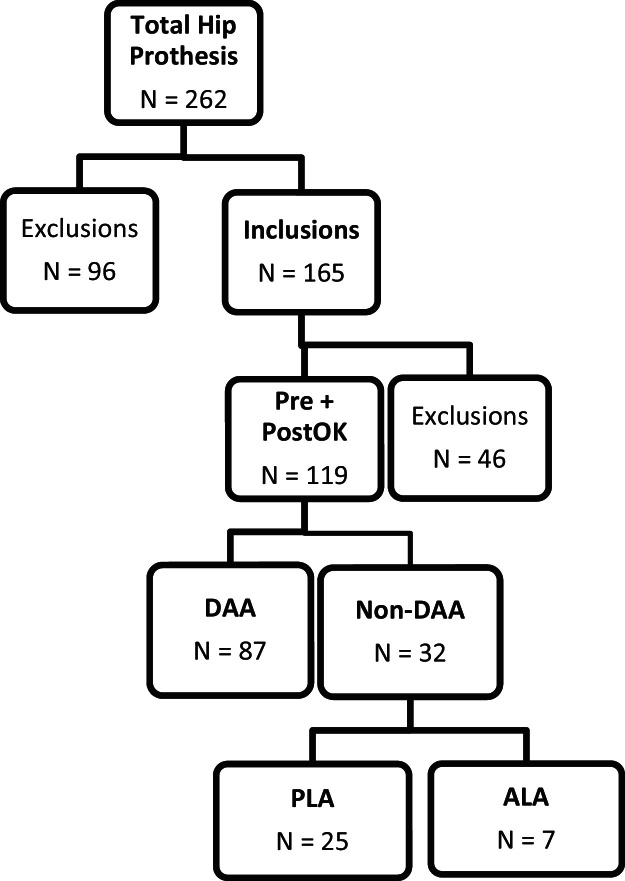
In 2014 a total of 262 hip replacements were performed in our hospital. Of these, 96 patients were excluded based on the exclusion criteria. A total of 166 patients performed the first measurement. Of these, 46 did not return for the second measurement and were excluded consequently. A total of 119 patients were included for analysis. Of these patients, 87 were operated with the DAA and 32 with a non-DAA of which 25 with the PLA and 7 with the ALA (Fig. 1).
Fig. 1.
Flowchart.
The study population counted slightly more women (53.8%). The mean age between the DAA and non-DAA group was comparable: 66.7 ± 10.4 years vs 67.9 ± 9.7 years. With respect to length, weight and BMI no (significant) differences were found. Most patients were ASA category II (63.0%), with a surgery indication being almost always osteoarthritis (97.5%). The Charnley Score showed mainly unilateral osteoarthritis (68.9%), but also patients with bilateral osteoarthritis (19.3%) and having a THR at the contralateral side (10.9%) are present. According to cup size, stem size and type of stem the groups cannot be compared due to the use of different prosthesis. All hip replacements were uncemented (Table 1).
Table 1.
Baseline characteristics.
| Approach |
p-value | ||
|---|---|---|---|
| DAA (n = 87) | Non-DAA (n = 32) | ||
| Gender | M39/F48 | M16/F16 | |
| Age in years | 66.7 ± 10.4 [31–87] | 67.9 ± 9.7 [52–89] | .576 |
| Length in cm | 170 ± 10 [148–194] | 171 ± 9 [152–193] | .613 |
| Weight in kg | 77.3 ± 13.8 [47–123] | 82.3 ± 15.2 [54–115] | .085 |
| BMI | 26.6 ± 3.7 [17.6–38.4] | 28.0 ± 4.5 [20.2–36.1] | .119 |
| In-hospital stay in days | 3.08 ± 1.41 [2–9] | 5.42 ± 5.25 [2–29] | .000* |
| ASA-classification | 1.75 ± 0.6 [1–3] | 1.88 ± 0.5 [1–3] | .240 |
| I | 29 (33.3%) | 6 (18.8%) | |
| II | 51 (58.6%) | 24 (75.0%) | |
| III | 7 (8.0%) | 2 (6.3%) | |
| IV | 0 | 0 | |
| Diagnosis | |||
| Osteoarthritis | 85 (97.7%) | 31 (96.9%) | |
| Dysplasia | 1 (1.1%) | 0 | |
| Rheumatoid arthritis | 1 (1.1%) | 0 | |
| Posttraumatic (late) | 0 | 1 (3.1%) | |
| Charnley score | |||
| A | 58 (66.7%) | 24 (75.0%) | |
| B1 | 18 (20.7%) | 5 (15.6%) | |
| B2 | 10 (11.5%) | 3 (9.4%) | |
| C | 1 (1.1%) | 0 | |
| Cup size | 51.8 ± 3.4 [44–64] | 52.3 ± 3.5 [46–60] | |
| Stem size | 11.3 ± 2.1 [8–16] | 6.1 ± 1.2 [4–8] | |
| KA | 54 (62.1%) | ||
| KLA | 28 (32.2%) | ||
| KHO | 5 (5.7) | ||
Significant difference at p < .050.
The length of stay was significant (p = .000) shorter in the anterior group compared to the non-anterior group: 3.08 ± 1.41 days [2–9] vs 5.42 ± 5.25 days [2–29], respectively. Also when complicated hospital stays were excluded a significant (p = .000) shorter stay was found for the DAA group compared with the non-DAA group: 2.89 ± .99 [2–7] vs 3.89 ± 1.16 [2–7], respectively. The mean number of days between the preoperative measurements and day of surgery was 23 ± 22 days, with a range of 1–113 days.
The PROMs are shown in Table 2b. The preoperative scores of the VAS, PSC and HOOS are not significant different between the groups. A significant improvement was noted for all PROMs in both groups. The difference between the pre- and postoperative scores of the VAS and HOOS is significant different between the groups. The DAA group shows a significant greater improvement compared to the non-DAA group. The patients opinion with respect to recovery and satisfaction (GPE) is not significant different between the groups (Table 2a).
Table 2b.
Strength, power and functional capacity tests.
| Approach |
p-value | ||
|---|---|---|---|
| DAA (n = 87) | Non-DAA (n = 32) | ||
| Leg press | |||
| T0 | 393.4 ± 286.2 | 332.3 ± 228.8 | .289 |
| Tend | 559.1 ± 260.6 | 552.8 ± 284.6 | .911 |
| Δ T0–tend | 165.7 ± 234.9 | 220.6 ± 220.1 | .513 |
| p-value | .000* | .000* | |
| Concentric power | |||
| T0 | 622.9 ± 401.9 | 591.4 ± 346.8 | .790 |
| Tend | 1088.3 ± 591.2 | 1200.6 ± 713.2 | .549 |
| Δ T0–tend | 465.3 ± 492.8 | 609.2 ± 649.2 | .060 |
| p-value | .000* | .004* | |
| Eccentric power | |||
| T0 | 616.4 ± 444.9 | 512.8 ± 340.3 | .438 |
| Tend | 1101.1 ± 660.2 | 1215.9 ± 791.9 | .593 |
| Δ T0–tend | 484.7 ± 519.9 | 703.2 ± 690.3 | .050* |
| p-value | .000* | .003* | |
| TUG | |||
| T0 | 9.6 ± 4.3 | 12.5 ± 6.6 | .031* |
| Tend | 7.4 ± 2.3 | 8.8 ± 3.2 | .030* |
| Δ T0–tend | 2.3 ± 3.1 | 3.7 ± 4.5 | .005* |
| p-value | .000* | .000* | |
| 6MWT | |||
| T0 | 356.8 ± 107.0 | 315.9 ± 136.7 | .112 |
| Tend | 437.2 ± 98.7 | 382.5 ± 133.6 | .025* |
| Δ T0–tend | 80.4 ± 60.8 | 66.6 ± 150.3 | .043* |
| p-value | .000* | .003* | |
Significant difference at p < .050.
Table 2a.
PROMs pre- and postoperative.
| Approach |
p-value | ||
|---|---|---|---|
| DAA (n = 87) | Non-DAA (n = 32) | ||
| VAS | |||
| T0 | 62.9 ± 19.9 | 65.5 ± 22.6 | .558 |
| Tend | 6.4 ± 15.6 | 15.8 ± 24.7 | .050* |
| Δ T0–tend | 56.6 ± 24.3 | 49.6 ± 31.6 | .049* |
| p-value | .000* | .000* | |
| PSK | |||
| T0 | 73.9 ± 30.5 | 77.0 ± 30.4 | .626 |
| Tend | 13.9 ± 28.6 | 25.0 ± 37.7 | .138 |
| Δ T0–tend | 59.9 ± 35.7 | 52.0 ± 46.7 | .294 |
| p-value | .000* | .000* | |
| HOOS | |||
| T0 | 41.3 ± 15.2 | 39.6 ± 17.2 | .620 |
| Tend | 86.9 ± 13.2 | 77.3 ± 20.9 | .023* |
| Δ T0–tend | 45.7 ± 18.9 | 37.7 ± 25.6 | .024* |
| p-value | .000* | .000* | |
| GPE – recovery | 6.3 ± 0.8 | 6.1 ± 0.9 | .163 |
| GPE – satisfaction | 6.4 ± 0.9 | 6.4 ± 0.7 | .883 |
Significant difference at P < .050.
In group analysis shows significant differences for all strength, power and functional capacity parameters between the pre- and postoperative measurements. The TUG shows a significant difference between the groups at the preoperative measurements in favour of the DAA group: 9.6 ± 4.3 vs 12.5 ± 6.6 s. The other strength, power test and 6MWT show no preoperative differences. But postoperatively the eccentric power shows a significant greater improvement in the non-DAA group (484.7 ± 519.9 vs 703.2 ± 690.3 Watt). The functional capacity tests show contradictory results. The non-DAA group shows a significant (p = .005) greater improvement in the TUG (2.3 ± 3.1 vs 3.7 ± 4.5 s). While the opposite was found for the 6MWT: 80.4 ± 60.8 vs 66.6 ± 150.3 m, in favour of the DAA group (p = .043) (Table 2b).
A subgroup analysis was performed in patients who chose to rehabilitate at an independent physiotherapist. This group consisted of 40 patients in the DAA group and 17 in the non-DAA group. With respect to age, length, weight, BMI, ASA-classification, Charnley score and the indication for surgery no significant differences were found. Analysis was performed in groups and between groups at an extra 6-week postoperative measurement moment. The PROMs showed significant improvements in both groups, but not between the groups (VAS, p = .701 (PSC, p = .942) (HOOS, p = .202)). The strength and power tests did not show significant difference in-group or between groups. There were significant improvements in the TUG (p = .009) and 6MWT (p = .009) in the DAA group. This in contrast to the non-DAA group: p = .078 and p = .498, respectively. No significant differences between the groups were found (Table 2c).
Table 2c.
Subgroup analysis 6 weeks postoperative (T2).
| Approach |
p-value | ||
|---|---|---|---|
| DAA (n = 40) | Non-DAA (n = 17) | ||
| VAS | |||
| T0 | 65.6 ± 18.9 | 68.5 ± 20.6 | .607 |
| T2 | 16.7 ± 18.5 | 16.0 ± 18.1 | .903 |
| ΔT0–T2 | 48.9 ± 25.0 | 51.4 ± 30.9 | .701 |
| p-value | .000* | .000* | |
| PSK | |||
| T0 | 74.8 ± 30.7 | 77.1 ± 29.1 | .792 |
| T2 | 43.9 ± 38.7 | 42.4 ± 39.7 | .911 |
| ΔT0–T2 | 27.4 ± 45.6 | 38.3 ± 45.5 | .942 |
| p-value | .001* | .002* | |
| HOOS | |||
| T0 | 38.1 ± 14.5 | 37.9 ± 14.1 | .959 |
| T2 | 77.5 ± 15.4 | 69.9 ± 17.9 | .178 |
| ΔT0–T2 | 36.5 ± 19.6 | 33.8 ± 22.9 | .202 |
| p-value | .000* | .000* | |
| Leg press | |||
| T0 | 362.7 ± 261.4 | 301.4 ± 221.5 | .402 |
| T2 | 440.9 ± 254.5 | 356.0 ± 248.8 | .329 |
| ΔT0–T2 | 54.7 ± 194.3 | 42.3 ± 235.7 | .273 |
| p-value | .105 | .456 | |
| Concentric power | |||
| T0 | 612.9 ± 480.5 | 519.1 ± 327.9 | .592 |
| T2 | 673.3 ± 469.3 | 437.6 ± 421.4 | .135 |
| ΔT0–T2 | 99.9 ± 355.1 | −121.6 ± 316.2 | .315 |
| p-value | .224 | .313 | |
| Eccentric power | |||
| T0 | 609.5 ± 518.2 | 494.8 ± 338.1 | .541 |
| T2 | 665.6 ± 555.4 | 412.9 ± 418.8 | .157 |
| ΔT0–T2 | 97.2 ± 385.6 | −121.0 ± 296.2 | .299 |
| p-value | .274 | .286 | |
| TUG | |||
| T0 | 10.1 ± 4.3 | 12.5 ± 6.3 | .100 |
| T2 | 8.7 ± 3.4 | 10.5 ± 3.9 | .132 |
| ΔT0–T2 | 1.6 ± 3.3 | 1.9 ± 4.4 | .077 |
| p-value | .009* | .078 | |
| 6MWT | |||
| T0 | 346.7 ± 107.1 | 326.1 ± 139.6 | .555 |
| T2 | 387.3 ± 104.8 | 333.1 ± 115.4 | .149 |
| ΔT0–T2 | 32.2 ± 68.9 | 12.5 ± 74.5 | .175 |
| p-value | .009* | .498 | |
Significant difference at p < .050.
4. Complications
Complications were registered until six months after 31-12-2014. The follow-up was 6–18 months. There were two early deep infections: one in the DAA group managed with debridement, prosthesis retention and systemic antibiotics and one in the non-DAA group managed with debridement, prosthesis retention with replacement of the femoral head, liner and systemic antibiotics. Also two superficial infections were seen, both treated with systemic antibiotics. All infections showed good response to the treatment, with retention of the prosthesis. Two hematomas were observed in the DAA group of which one was managed conservative and the other was managed operatively. One patient in the DAA group experienced pneumonia, hip dislocation and superficial wound infect (Table 3). The DAA group showed no significant (p = .075) more complications compared to the non-DAA group, although a trend exists. There were no significant differences in the occurrence of complications between the DAA and PLA (p = .160) or ALA and PLA (p = .605). Although there was a significant difference between the DAA and ALA (p = .001). However, only 7 patients were included in the ALA group.
Table 3.
Complications.
| DAA N = 10/87 (11.5%) |
Non-DAA N = 1/32 (0.03%) |
||
|---|---|---|---|
| PLA (N = 1/25 (4.0%)) |
ALA (N = 0/7) |
||
| Infect | |||
| Superficial | 2 (2.3%) | 0 | 0 |
| Deep | 1 (1.2%) | 1 (4.0%) | 0 |
| Dislocation | 1 (1.2%) | 0 | 0 |
| Haematoma | 2 (2.3%) | 0 | 0 |
| Fissure/fracture | 1 (1.2%) | 0 | 0 |
| Other | |||
| CVA | 1 (1.2%) | 0 | 0 |
| Pulmonary Embolism | 1 (1.2%) | 0 | 0 |
| Pneumonia | 1 (1.2%) | 0 | 0 |
5. Discussion
This study is one of the first in its kind, examining both subjective and objective parameters after THR in the anterior, posterolateral and anterolateral approach. Strength, power and functional capacity tests show significant improvement in all approaches after THR, making THR a very effective intervention.
The significant difference in hospital stay between the DAA and non-DAA can possibly be explained by a difference in (nursing) protocols. The nursing protocol for the non-DAA does not allow mobilization before the first day after the surgery, while mobilization in the DAA is allowed on the same day of surgery. This might have led to differences. Meneghini and Smits showed that it is possible to safely discharge patients the first day after surgery, independent of approach (two-incision, mini-posterior, mini-anterolateral).18, 19
This study showed no advantages of the DAA in strength and power outcome. The concentric power test showed no significant differences, but a trend in favour of the non-DAA was seen. Significant improvement in both groups was seen in eccentric power test after 16 weeks. This improvement was not seen at the 6 weeks measurement. It turns out that after 6 weeks, there is a decrease in power in the non-DAA group. However, in the subsequent 10 weeks a major improvement is observed. A significant difference between the groups at 6 weeks was not seen, but in contrast to the non-DAA group, we did observe improvement in the DAA group. This supports the hypothesis of less muscle damage with the DAA. Although not taken into account in this study, the idea exists that patients in the DAA group are able to walk without crutches earlier. Hereby, muscles are loaded and trained at an earlier stage. This hypothesis is supported by the score of the HOOS and the results of the power tests at the 6 weeks measurement moment. In a recently published, prospective cohort study with three parallel groups Winther et al. discovered that the decrease in power in the first week after surgery with the DAA or PLA is less compared to the DLA.20 An analysis by approach was not possible in this study due to the small number of patients operated with the ALA.
We presume that the rehabilitation programme of patients in the DAA group is shorter than the non-DAA group programme. Patients in the DAA group complete there rehabilitation weeks prior of the final measurement moment at 16 weeks. By quitting strength exercises this might result in less improvement in strength compared to the non-DAA group. In addition, there are significant differences in power at T0 between the groups, in favour of the DAA group. The increase in strength is partially determined by the level of strength preoperative. A larger margin of profit exists when the starting point is lower. This seems the case in the non-DAA group.
In both the DAA and non-DAA group significant differences are found for improvement in PROMs, but no significant improvement was observed for the strength and power tests after 6 weeks. For the non-DAA group also no improvement was seen in functional capacity. This is in correspondence with patients in an early phase after hip replacement overestimating their functional capacity: the HOOS scores increase faster than the TUG, 6MWT and stair climbing improve. This is mainly based on experiencing less pain.21
We found a significant difference in improvement of functional capacity between both approaches for the TUG and 6MWT. Although, it is not fully clear which approach has improved best overall. There was already a significant difference in TUG in favour of the DAA preoperative. There is a physiologic limitation in walking speed. The walking speed in the DAA group is significantly higher at T0 compared to the non-DAA group. Therefore, the degree of improvement is less in the DAA compared to the non-DAA. A similar trend, but no significance, was found for the 6MWT. The longer duration of the 6MWT puts a bigger margin for improvement on this test. Because of this, the role of training is, beside the increase in power and decrease in pain, bigger in the 6MWT compared to the TUG.
As mentioned earlier, we believe that the physical therapy programme in the DAA group is finished earlier compared to the non-DAA group. The TUG test measures a combination of power (getting out of the chair) and walking speed. Because the DAA rehabilitation programme is finished earlier they probably receive less resistance training what might explain the smaller increase in strength and walking speed compared to the non-DAA group. In contrast, endurance is the most important parameter in 6MWT. It is likely that the DAA group is able to walk without crutches earlier what consequently results in a longer period of endurance training. Most of the time resistance training ends when the rehabilitation programme is finished, but endurance training (normal walking) continues. This might result in a significant better improvement in the 6MWT in favour of the DAA.
Although not significantly different, there seems to be a trend in the average weight and BMI which is higher in the non-anterior approach DAA group compared to the DAA group. This might affect the outcome on 6MWT. A subgroup analysis was performed with the hypothesis that differences between the groups would be seen in an earlier phase (6 weeks) after surgery, because of the minimal invasive character of the DAA. However, the subgroup analysis showed no significant difference between both approaches.
Rodriguez et al. showed that the maximum score in the ‘Functional Independence Measure (M-FIM)’ – consisting of an independent bed-chair transfer, walking and climbing the stairs – was reached significantly earlier in patients operated with the DAA patients compared to the PLA. However, the significant difference disappeared after two weeks. Also the walking speed at discharge, measured with the TUG test, was significantly higher in the DAA. This difference was still significant after two weeks, but disappeared at 6 weeks.4 In a retrospective cohort study, Poehling-Monaghan et al. found no significant difference in recovery for daily activities after 2 days, 2 weeks and 2 months between the DAA and the mini-PLA. In addition, there was no difference in maximum walking distance and climbing stairs between both approaches during the hospital stay.5 Reininga et al. also did not found any significant differences in walking gait between a conventional PLA and a computer-navigated minimal invasive DAA.22 In contrast, Mayr et al. found a significant improvement in walking gait and walking speed after 12 weeks for the minimal invasive DAA compared to the ALA.23 Barret et al. performed a RCT and also discovered a significant improvement in walking and stair climbing after 6 weeks for the DAA. It needs to be mentioned that a restriction for patients operated with the PLA to prevent dislocation of the hip was used. This restriction was not imposed on the DAA.24 This is also one of the limitations of this study. These restrictions might cause fear of movement in the PLA, what might result in better results in the DAA. No restrictions were given in the study of Poehling-Monaghan et al. and it is not clear if there were any dislocations during this study. Therefore it is not clear if it is safe to train without restrictions.5 The risk of dislocation generally is low and restrictions are associated with slower recovery in daily activities.25 This is supported in a meta-analysis by van der Weegen et al. who used six studies. They concluded that restrictions are not effective in any approach after THR.26
Pre- and postoperative tests were conducted by an independent physical therapist. Patients were allowed to choose their own physical therapist. Limitation of this study is the lack of contact between the hospital and the physical therapists with respect to a standardized post hip replacement therapy programme. It is likely that differences in physical therapy programmes have occurred. The retrospective character of this study is also a limitation. There was no randomization what might cause a bias. This bias can be undone because every surgeon is using his own approach in which they trust. There were several patients who came from a different region to the hospital because of the positive stories about the DAA. It is possible these people are more motivated during rehabilitation. The effect size of the ALA group is limited because only seven patients were included in the ALA group. Future studies should focus on randomized controlled trials between the different approaches in primary hip arthroplasty. We performed a post hoc power analysis. A randomized-controlled trial should have a sample size of 945 patients per arm, taking a 10% drop-out into account (n = 859 per arm), based on a two-tailed test, probability of error α = 0.05, desired power of 0.80 and effect-size r of 0.135.
6. Conclusion
This study is one of the first to examine both subjective as objective parameters in primary total hip replacement. THR is, independent of approach, a very effective intervention. This study shows no major differences in subjective or objective outcome between the anterior approach and non-anterior (posterolateral/anterolateral) approach. There seems to be a small advantage in favour of the DAA, in particular directly postoperative and the first postoperative weeks. Surgeons are advised to use the approach they are experienced and confident with. Future studies should focus on randomized controlled trials.
Ethics
Authorship of the paper: All authors state they had a significant contribution and approve the manuscript.
Originality and plagiarism: All authors state that they have written entirely original work.
Data access and retention: Raw data is accessible.
Multiple, redundant or concurrent publication: All authors state that the manuscript has not been published before.
Conflicts of interest
The authors have none to declare.
References
- 1.Edmunds C.T., Boscainos P.J. Effect of surgical approach for total hip replacement on hip function using Harris Hip scores and Trendelenburg's test. A retrospective analysis. Surgeon. 2011;9(3):124–129. doi: 10.1016/j.surge.2010.08.014. [DOI] [PubMed] [Google Scholar]
- 2.Husby V.S., Helgerud J., Bjørgen S., Husby O.S., Benum P., Hoff J. Early maximal strength training is an efficient treatment for patients operated with total hip arthroplasty. Arch Phys Med Rehabil. 2009;90(10):1658–1667. doi: 10.1016/j.apmr.2009.04.018. [DOI] [PubMed] [Google Scholar]
- 3.Nederlandse Orthopaedische Vereniging . Jaarrapportage uit de Landelijke Registratie Orthopedische Implantaten 2014. 2014. LROI-Rapportage 2014, Orthopedische Implantaten in Beeld. [Google Scholar]
- 4.Rodriguez J.A., Deshmukh A.J., Rathod P.A. Does the direct anterior approach in THA offer faster rehabilitation and comparable safety to the posterior approach. Clin Orthop Relat Res. 2014;472:455–463. doi: 10.1007/s11999-013-3231-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Poehling-Monaghan K.L., Kamath A.F., Taunton M.J., Pagnano M.W. Direct anterior versus miniposterior THA with the same advanced perioperative protocols: surprising early clinical results. Clin Orthop Relat Res. 2015;473:623–631. doi: 10.1007/s11999-014-3827-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Spaans A.J., van den Hout J.A., Bolder S.B. High complication rate in the early experience of minimally invasive total hip arthroplasty by the direct anterior approach. Acta Orthop. 2012;83(4):342–346. doi: 10.3109/17453674.2012.711701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chechik O., Khashan M., Lador R., Salai M., Amar E. Surgical approach and prosthesis fixation in hip arthroplasty world wide. Arch Orthop Trauma Surg. 2013;133(11):1595–1600. doi: 10.1007/s00402-013-1828-0. [DOI] [PubMed] [Google Scholar]
- 8.Matta J.M., Shahrdar C., Ferguson T. Single-incision anterior approach for total hip arthroplasty on an orthopaedic table. Clin Orthop Relat Res. 2005;441:115–124. doi: 10.1097/01.blo.0000194309.70518.cb. [DOI] [PubMed] [Google Scholar]
- 9.Tsukada S., Wakui M. Lower dislocation rate following total hip arthroplasty via direct anterior approach than via posterior approach: five-year-average follow-up results. Open Orthop J. 2015;9:157–162. doi: 10.2174/1874325001509010157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Petis S., Howard J.L., Lanting B.L., Vasarhelyi E.M. Surgical approach in primary total hip arthroplasty: anatomy, technique and clinical outcomes. Can J Surg. 2015;58(2):128–139. doi: 10.1503/cjs.007214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Browne J.A., Pagnano M.W. Surgical technique: a simple soft-tissue-only repair of the capsule and external rotators in posterior-approach THA. Clin Orthop Relat Res. 2010;470:511–515. doi: 10.1007/s11999-011-2113-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kwon M.S., Kuskowski M., Mulhall K.J., Macaulay W., Brown T.E., Saleh K.J. Does surgical approach affect total hip arthroplasty dislocation rates? Clin Orthop Relat Res. 2006;447:34–38. doi: 10.1097/01.blo.0000218746.84494.df. [DOI] [PubMed] [Google Scholar]
- 13.Sköldenberg O., Ekman A., Salemyr M., Bodén H. Reduced dislocation rate after hip arthroplasty for femoral neck fractures when changing from posterolateral to anterolateral approach. Acta Orthop. 2010;81(5):583–587. doi: 10.3109/17453674.2010.519170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tsai S.W., Chen C.F., Wu P.K., Chen T.H., Liu C.L., Chen W.M. Modified anterolateral approach in minimally invasive total hip arthroplasty. Hip Int. 2015;25(3):245–250. doi: 10.5301/hipint.5000218. [DOI] [PubMed] [Google Scholar]
- 15.Sheth D., Cafri G., Inacio M.C., Paxton E.W., Namba R.S. Anterior and anterolateral approaches for THA are associated with lower dislocation risk without higher revision risk. Clin Orthop Relat Res. 2015;473(11):3401–3408. doi: 10.1007/s11999-015-4230-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Meneghini R.M., Smits S.A., Swinford R.R., Bahamonde R.E. A randomized, prospective study of 3 minimally invasive surgical approaches in total hip arthroplasty: comprehensive gait analysis. J Arthroplasty. 2008;23(6 Suppl. 1):68–73. doi: 10.1016/j.arth.2008.05.014. [DOI] [PubMed] [Google Scholar]
- 17.Masonis J.L., Bourne R.B. Surgical approach, abductor function, and total hip arthroplasty dislocation. Clin Orthop Relat Res. 2002;(405):46–53. doi: 10.1097/00003086-200212000-00006. [DOI] [PubMed] [Google Scholar]
- 18.Meneghini R.M., Smits S.A. Early discharge and recovery with three minimally invasive total hip arthroplasty approaches: a preliminary study. Clin Orthop Relat Res. 2009;467(6):1431–1437. doi: 10.1007/s11999-009-0729-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Berger R.A., Jacobs J.J., Meneghini R.M., Della Valle C., Paprosky W., Rosenberg A.G. Rapid rehabilitation and recovery with minimally invasive total hip arthroplasty. Clin Orthop Relat Res. 2004;429:239–247. doi: 10.1097/01.blo.0000150127.80647.80. [DOI] [PubMed] [Google Scholar]
- 20.Winther S.B., Husby V.S., Foss O.A. Muscular strength after total hip arthroplasty – a prospective comparison of 3 surgical approaches. Acta Orthopaedica. 2016;87(1):22–28. doi: 10.3109/17453674.2015.1068032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dayton M.R., Judd D.L., Hogan C.A., Stevens-Lapsley J.E. Performance-based versus self-reported outcomes using the hip disability and osteoarthritis outcome score after total hip arthroplasty. Am J Phys Med Rehabil. 2016;95(2):132–138. doi: 10.1097/PHM.0000000000000357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reininga I.H., Stevens M., Wagenmakers R. Comparison of gait in patients following a computer-navigated minimally invasive anterior approach and a conventional posterolateral approach for total hip arthroplasty: a randomized controlled trial. J Orthop Res. 2013;31(2):288–294. doi: 10.1002/jor.22210. [DOI] [PubMed] [Google Scholar]
- 23.Mayr E., Nogler M., Benedetti M.G., Kessler O., Reinthaler A., Krismer M. A prospective randomized assessment of earlier functional recovery in THA patients treated by minimally invasive direct anterior approach: a gait analysis study. Clin Biomech. 2009;24(10):812–818. doi: 10.1016/j.clinbiomech.2009.07.010. [DOI] [PubMed] [Google Scholar]
- 24.Barrett W.P., Turner S.E., Leopold J.P. Prospective randomized study of direct anterior vs postero-lateral approach for total hip arthroplasty. J Arthroplasty. 2013;28(9):1634–1638. doi: 10.1016/j.arth.2013.01.034. [DOI] [PubMed] [Google Scholar]
- 25.Barnsley L., Barnsley L., Page R. Are hip precautions necessary post total hip arthroplasty? A systematic review. Geriatr Orthop Surg Rehabil. 2015;6(3):230–235. doi: 10.1177/2151458515584640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.van der Weegen W., Kornuijt A., Das D. Do lifestyle restrictions and precautions prevent dislocation after total hip arthroplasty? A systematic review and meta-analysis of the literature. Clin Rehabil. 2016;30(4):329–339. doi: 10.1177/0269215515579421. [DOI] [PubMed] [Google Scholar]