Highlights
-
•
Plantar midtarsal dislocations are uncommon injuries and can occur from a variety of mechanisms.
-
•
Initial management should consist of urgent reduction with appropriate wound care.
-
•
Definitive management may consist of operative or conservative treatment depending on the reduction stability.
-
•
A successful outcome can be obtained with conservative management as demonstrated by our case presentation.
Keywords: Midtarsal, Chopart, Transverse tarsal, Talonavicular, Cuneiform, Foot
Abstract
The midtarsal joint, also known as the Chopart or the transverse tarsal joint, is composed of the talonavicular and calcaneocuboid articulations.1 Midtarsal joint dislocations are rare injuries given the strong periarticular ligamentous support.2, 3 Medial, lateral, dorsal, and rarely plantar dislocations have been reported from multiple high-energy mechanisms.4, 5 We describe the case of a 24-year-old male who sustained talonavicular and calcaneocuboid plantar dislocations associated with a middle and lateral intercuneiform dislocation, open proximal 5th metatarsal fracture, 2nd–4th metatarsal base fractures, and lateral cuneiform fracture. The mechanism of injury, diagnosis, management, operative intervention, and follow up are discussed.
1. Introduction
The midtarsal joint, which consists of the talonavicular and calcaneocuboid articulations, are firmly stabilized by the plantar periarticular ligaments and requires significant force to disrupt.1 The talonavicular joint is stabilized by the superior medial and inferior aspects of the calcaneonavicular (spring) ligament.2, 3 The calcaneocuboid joint is supported inferiorly by the superficial and deep inferior calcaneocuboid ligaments and superiorly by the lateral limb of the bifurcate ligament.3 Dislocations of the midtarsal joint, although uncommon, have been reported from a variety of high-energy mechanisms including motor vehicle crashes and falls from height, and often have associated injuries in the polytrauma patient.5 An isolated dorsal midtarsal dislocation from a low-energy mechanism has also been reported.6 Although more energy is required to cause a dorsal midtarsal dislocation, it is the most often reported direction of dislocation given the frequent mechanism of a dorsally directed force to the forefoot.7 In contrast, plantar midtarsal dislocations are rare, accounting for only 7% of midtarsal dislocations.7 We describe the case of a 24-year-old male who sustained a plantar midtarsal dislocation associated with an intercuneiform dislocation, open proximal 5th metatarsal, and closed midfoot fractures from a blunt force trauma.
2. Case report
A 24-year-old man presented was transferred to a level 1 trauma center from an outside facility after his foot was caught under the hydraulic elevation bar of a construction excavator. The patient presented complaining of severe right foot pain, with no neurovascular deficits found at the time of initial evaluation. An 8 cm laceration with exposed bone was found over lateral aspect of the right foot, along with substantial swelling, dorsal prominence and early signs of dorsal skin necrosis. Radiographs (Fig. 1), CT scan (Fig. 2) and 3D reconstructions (Fig. 3) of the right foot revealed a plantar midtarsal dislocation, middle and lateral intercuneiform dislocation, proximal 2nd–5th metatarsal fractures, and a lateral cuneiform fracture. Two grams of cefazolin and a tetanus immunization were administered. The open 5th metatarsal fracture was irrigated with 2 l of sterile saline, and the right foot was placed into a short leg splint that was iced and elevated. The patient was then admitted to the orthopedic surgery service and taken to the operating room for emergent irrigation, debridement, midtarsal joint reduction, and placement of a negative pressure wound device. Post-operative radiographs (Fig. 4), CT scan (Fig. 5), and CT scan 3D reconstructions (Fig. 6) of the right foot demonstrated concentrically reduced talonavicular and calcaneocuboid joints as well as reduction of the middle and lateral intercuneiform dislocation. At the 2-week follow up visit, the talonavicular and calcaneocuboid joints maintained reduction (Fig. 7). The dorsal skin and lateral foot wound appeared to be healing uneventfully. Conservative treatment consisted of immobilization in a short leg cast for a total of 6 weeks with strict nonweightbearing. Radiographs at the 6-week follow up visit demonstrated interval healing of the metatarsal and cuneiform fractures and stable reduction of the midtarsal and intercuneiform dislocations (Fig. 8). The short leg cast was removed at the 6-week follow up visit. The patient was then transitioned to weight bearing as tolerated with a CAM walker boot. Weight bearing radiographs at the 12-week follow up visit demonstrated healed metatarsal and cuneiform fractures as well as continued maintenance of the talonavicular, calcaneocuboid, and intercuneiform joints (Fig. 9). On clinical examination, the lateral soft tissue injury overlying the proximal 5th metatarsal healed appropriately, and the patient was transitioned to regular shoe wear as full weight bearing. He reports painless ambulation and is able to perform all activities of daily living without hindrance.
Fig. 1.

Injury radiographs of the right foot demonstrating plantar dislocations of the talonavicular and calcaneocuboid joints, middle and lateral intercuneiform dislocation, and proximal 2nd–5th metatarsal and lateral cuneiform fractures on lateral (A), oblique (B), and anteroposterior (C) views.
Fig. 2.
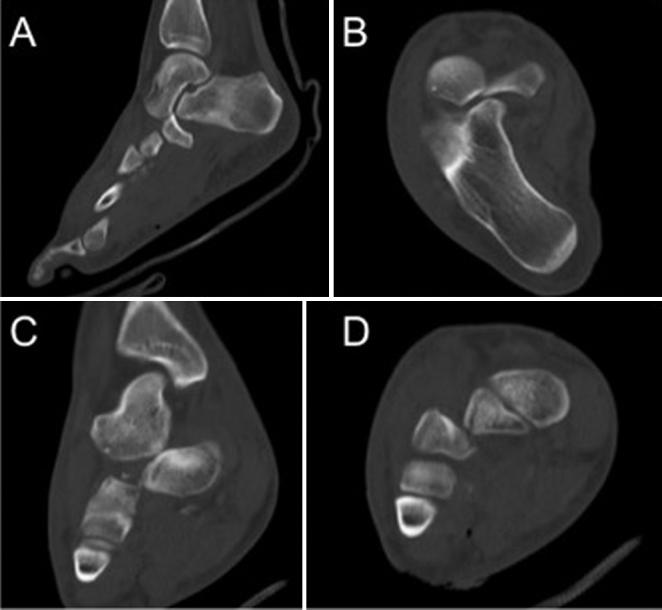
CT scan of the right foot demonstrating plantar talonavicular and calcaneocuboid dislocations on sagittal (A), axial (B), and coronal (C) views. Associated intercuneiform dislocation on coronal (D) view.
Fig. 3.

Pre-operative 3D CT reconstructions of the right foot demonstrating plantar dislocations of the talonavicular and calcaneocuboid joints, and intercuneiform dislocation on sagittal (A), coronal (B), and axial (C) views.
Fig. 4.

Post-operative radiographs of the right foot demonstrating concentrically reduced talonavicular, calcaneocuboid, and intercuneiform joints on oblique (A), anteroposterior (B), and lateral (C) views.
Fig. 5.
Post-operative CT scan of the right foot demonstrating concentrically reduced talonavicular, calcaneocuboid, and intercuneiform joints on sagittal (A), axial (B), and coronal (C) views.
Fig. 6.

Post-operative CT scan 3D reconstructions of the right foot demonstrating concentrically reduced talonavicular, calcaneocuboid, and intercuneiform joints on sagittal (A), coronal (B), and axial (C) views.
Fig. 7.

Two-week follow up radiographs of the right foot demonstrating maintained concentric reduction of the talonavicular, calcaneocuboid, and intercuneiform joints on lateral (A), oblique (B), and anteroposterior (C) views.
Fig. 8.
Six-week follow up radiographs of the right foot demonstrating interval metatarsal and cuneiform fracture healing, and maintained concentric reduction of the talonavicular, calcaneocuboid, and intercuneiform joints on lateral (A), oblique (B), and anteroposterior (C) views.
Fig. 9.

12-week follow up weight bearing radiographs demonstrating healed 2nd through 5th metatarsal fractures with maintained concentric reduction of the talonavicular, calcaneocuboid, and intercuneiform joints on lateral (A), oblique (B), and anteroposterior (C) views.
3. Discussion
The midtarsal joint is composed of the talonavicular and calcaneocuboid joints.1 Main and Jowett classified a series of 71 midtarsal joint injuries according to the direction of the deforming force and the subsequent displacement: medial forces, longitudinal forces, lateral forces, plantar forces, and crush injuries.4 Only one case of an isolated midtarsal dislocation was reported in this series.4 Kenwright and Taylor reported 58 injuries to the talus and peritalar joints.8 In their series, two of the 10 midtarsal dislocations were reported as plantar, although it is unclear if any fractures were associated.8 A review of the current literature revealed only one case report of an isolated plantar midtarsal dislocation.9 Intercuneiform dislocations have been reported in association with Lisfranc injuries.10, 11 To the best of our knowledge, this is the first report of a plantar midtarsal dislocation associated with an intercuneiform dislocation.
Midtarsal dislocations are uncommon injuries given the support conferred to the talonavicular and calcaneocuboid joints by the robust periarticular ligaments.12 The bifurcate ligament, calcaneonavicular ligament, and inferior calcaneocuboid ligament provide strong structural support to the midtarsal joints and are key structures of the foot arch.2, 3 Due to the force needed to disrupt these ligaments, tarsal dislocations are often associated with fractures and rarely occur in isolation.13
Wilson et al. reported that hindfoot injuries and midfoot injuries account for approximately 24% and 16% respectively of all foot and ankle injuries sustained as a consequence of motor vehicle accidents.14 In a series by Main and Jowett, a delayed diagnosis occurred in 41% of midtarsal joint injuries.4 During the evaluation of a patient with lower extremity trauma, physicians must maintain a high index of suspicion for these injuries.4 Following initial evaluation, plain radiographs of the injured extremity should be obtained.15 A CT scan is often needed to further characterize associated fractures.13 Small avulsion fractures may represent significant joint instability and dislocations that have spontaneously reduced prior to imaging.13 Midtarsal dislocations should be promptly reduced, either under conscious sedation or general anesthesia in the operating room, to avoid sequelae of prolonged dislocation, including avascular necrosis and osteoarthritis.15, 16 Surgical intervention and stabilization of the midtarsal joints may be avoided with urgent stable reduction and immobilization.15 Recent studies have demonstrated that operative intervention to maintain talonavicular joint reduction can improve outcomes, particularly in cases of unstable reduction.5, 17, 18
4. Conclusion
Hindfoot and midfoot injuries have been reported to account for approximately 24% and 16% respectively of all foot and ankle injuries as a result of motor vehicle accidents.14 Given this high rate of injury associated with trauma patients and potentially debilitating consequences, physicians must remain vigilant.14 Following diagnosis with plain radiographs or CT scan, the joints should be promptly reduced and any open wounds irrigated and dressed.15, 16 Those dislocations that are unable to be reduced in the emergency department with conscious sedation must be urgently reduced in the operating room.15 Operative stabilization of midtarsal dislocations post reduction may be indicated depending on the stability of the reduction.15 As demonstrated in our case, a successful outcome can be obtained with conservative management.
Conflicts of interest
The authors have none to declare.
References
- 1.Klaue K. Chopart fractures. Injury. 2004;35(suppl 2):SB64–SB70. doi: 10.1016/j.injury.2004.07.013. [DOI] [PubMed] [Google Scholar]
- 2.Taniguchi A., Tanaka Y., Takakura Y., Kadono K., Maeda M., Yamamoto H. Anatomy of the spring ligament. J Bone Joint Surg Am. 2003;85-A(11):2174–2178. doi: 10.2106/00004623-200311000-00018. [DOI] [PubMed] [Google Scholar]
- 3.Melão L., Canella C., Weber M., Negrão P., Trudell D., Resnick D. Ligaments of the transverse tarsal joint complex: MRI-anatomic correlation in cadavers. AJR Am J Roentgenol. 2009;193(3):662–671. doi: 10.2214/AJR.08.2084. [DOI] [PubMed] [Google Scholar]
- 4.Main B.J., Jowett R.L. Injuries of the midtarsal joint. J Bone Joint Surg Br. 1975;57(1):89–97. [PubMed] [Google Scholar]
- 5.van Dorp K.B., de Vries M.R., van der Elst M., Schepers T. Chopart joint injury: a study of outcome and morbidity. J Foot Ankle Surg. 2010;49(6):541–545. doi: 10.1053/j.jfas.2010.08.005. [DOI] [PubMed] [Google Scholar]
- 6.Harris A.P., Johnson J., Waryasz G.R. Isolated dorsal dislocations of the talonavicular and calcaneocuboid articulations (Chopart joints) from a low-energy mechanism. Am J Emerg Med. 2016;34(8):1733.e1–1733.e4. doi: 10.1016/j.ajem.2015.12.054. [DOI] [PubMed] [Google Scholar]
- 7.Miller C.M., Winter W.G., Bucknell A.L., Jonassen E.A. Injuries to the midtarsal joint and lesser tarsal bones. J Am Acad Orthop Surg. 1998;6(4):249–258. doi: 10.5435/00124635-199807000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Kenwright J., Taylor R.G. Major injuries of the talus. J Bone Joint Surg Br. 1970;52(1):36–48. [PubMed] [Google Scholar]
- 9.Ruthman J.C., Meyn N.P. Isolated plantar midtarsal dislocation. Am J Emerg Med. 1988;6(6):599–601. doi: 10.1016/0735-6757(88)90100-3. [DOI] [PubMed] [Google Scholar]
- 10.Cain P.R., Seligson D. Lisfranc's fracture-dislocation with intercuneiform dislocation: presentation of two cases and a plan for treatment. Foot Ankle. 1981;2(3):156–160. doi: 10.1177/107110078100200307. [DOI] [PubMed] [Google Scholar]
- 11.Hung J.L.P., Chan S.C.F. Intercuneiform and Lisfranc fracture-dislocation due to seizure: a case report. J Foot Ankle Surg. 2016;55(2):314–316. doi: 10.1053/j.jfas.2014.09.039. [DOI] [PubMed] [Google Scholar]
- 12.Puthezhath K., Veluthedath R., Kumaran C.M., Patinharayil G. Acute isolated dorsal midtarsal (Chopart's) dislocation: a case report. J Foot Ankle Surg. 2009;48(4):462–465. doi: 10.1053/j.jfas.2009.01.016. [DOI] [PubMed] [Google Scholar]
- 13.Schmitt J.W., Werner C.M.L., Ossendorf C., Wanner G.A., Simmen H.-P. Avulsion fracture of the dorsal talonavicular ligament: a subtle radiographic sign of possible Chopart joint dislocation. Foot Ankle Int. 2011;32(7):722–726. doi: 10.3113/FAI.2011.0722. [DOI] [PubMed] [Google Scholar]
- 14.Wilson L.S., Mizel M.S., Michelson J.D. Foot and ankle injuries in motor vehicle accidents. Foot Ankle Int. 2001;22(8):649–652. doi: 10.1177/107110070102200806. [DOI] [PubMed] [Google Scholar]
- 15.Klaue K. Treatment of Chopart fracture-dislocations. Eur J Trauma Emerg Surg. 2010;36(3):191–195. doi: 10.1007/s00068-010-1047-0. [DOI] [PubMed] [Google Scholar]
- 16.Swords M.P., Schramski M., Switzer K., Nemec S. Chopart fractures and dislocations. Foot Ankle Clin. 2008;13(4):679–693. doi: 10.1016/j.fcl.2008.08.004. [DOI] [PubMed] [Google Scholar]
- 17.Richter M., Thermann H., Huefner T., Schmidt U., Goesling T., Krettek C. Chopart joint fracture-dislocation: initial open reduction provides better outcome than closed reduction. Foot Ankle Int. 2004;25(5):340–348. doi: 10.1177/107110070402500512. [DOI] [PubMed] [Google Scholar]
- 18.Richter M., Wippermann B., Krettek C., Schratt H.E., Hufner T., Therman H. Fractures and fracture dislocations of the midfoot: occurrence, causes and long-term results. Foot Ankle Int. 2001;22(5):392–398. doi: 10.1177/107110070102200506. [DOI] [PubMed] [Google Scholar]




