Summary
Chronic liver damage is associated with unique changes in the hemostatic system. Patients with liver disease often exhibit a precariously rebalanced hemostatic system, easily tipped towards bleeding or thrombotic complications by otherwise benign stimuli. In addition, some clinical studies have shown that hemostatic system components contribute to the progression of liver disease. There is a strong basic science foundation for clinical studies with this particular focus. Chronic and acute liver disease can be modeled in rodents and large animals utilizing a variety of approaches that span chronic exposure to toxic xenobiotics, diet-induced obesity, and surgical intervention. Utilizing these experimental approaches, there is now strong evidence that in addition to perturbations in hemostasis caused by liver disease, elements of the hemostatic system have powerful effects on the progression of experimental liver toxicity and disease. In this review we cover the basis of animal models most often utilized to assess the impact of hemostatic system on liver disease, and highlight the role that coagulation proteases and their targets play in experimental liver toxicity and disease, emphasizing key similarities and differences between models. The need to characterize hemostatic changes in existing animal models and to develop novel animal models recapitulating the coagulopathy of chronic liver disease is highlighted. Finally, we emphasize the continued need to translate knowledge derived from highly applicable animal models to improve our understanding of the reciprocal interaction of liver disease and hemostatic system in patients.
Gaps in knowledge at the intersection of hemostasis and liver injury/disease
Activation of the hemostatic system is a virtually inescapable outcome of inflammatory cell activation and tissue injury in multiple diseases. Notably, this association is complex in the context of acute liver injury and chronic liver disease. As the primary site of synthesis of multiple coagulation factors, including anticoagulant proteins, the liver plays a central role in maintaining physiological hemostasis and preventing thrombosis. Thus, when hepatic dysfunction is present, as in acute liver injury (e.g., xenobiotic hepatotoxicity) or chronic liver disease (e.g., viral hepatitis, biliary disease, fatty liver disease), there may be local coagulation occurring in the liver, but also changes in hepatic expression of plasma proteins that are central to normal hemostasis. Although the hemostatic system retains balance in patients with severe liver disease, this balance is precarious, permitting otherwise innocuous stimuli to tip the scales toward either excessive bleeding or dangerous thrombotic events, such as portal vein thrombosis. This concept has been reviewed elsewhere in detail [1] and there is continued investment in identifying strategies to detect patients at risk of either bleeding or thrombotic complications caused by hepatic dysfunction.
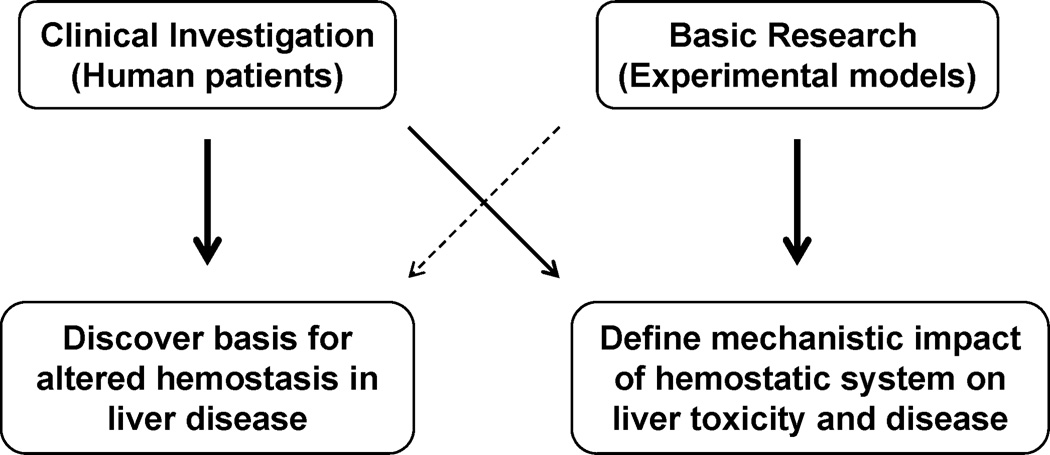
Numerous rodent models are commonly utilized to define mechanisms of acute and chronic liver injury (Table 1). There is the intrinsic, but not insurmountable challenge that rodent models do not always recapitulate the totality or severity of human disease. Nonetheless, animal models of acute and chronic liver injury retain high value as investigational tools to identify and define novel crosstalk between hemostasis and liver disease. Of importance, we find a relative dichotomy in experimental studies involving animals and clinical investigation in human subjects (Fig. 1). Substantial effort has been invested in defining changes in the hemostatic system that accompany acute and chronic liver damage in humans. However, matching systematic investigation is lacking in the majority of experimental animal models of these conditions (Fig. 1). Animal models offer an untapped opportunity to obtain information on the mechanism whereby liver disease affects the hemostatic system. This knowledge could lead to experimental platforms to assess interventions for the treatment of thrombosis or bleeding in human liver disease.
Table 1.
Experimental models and hemostatic changes in liver disease.
| Human disease | Model | Pathology (model) | Hemostatic changes (model) | Impact of hemostatic interventions | References |
|---|---|---|---|---|---|
| Acetaminophen overdose |
Acetaminophen hepatotoxicity in mice |
Centrilobular hepatic necrosis | TAT levels: ↑ | Low TF: ↓hepatotoxicity | [12–17] |
| PT/INR: ↑ | Thrombin inhibition (heparin/lepirudin): ↓ acute liver damage | ||||
| Hepatic fibrin(ogen) deposition: within areas of necrosis |
PAR-1 deficiency: ↓ liver damage | ||||
| PAI-1 in liver and plasma: ↑ | PAR-4 deficiency: ↓ liver damage, PAR-4 involvement is platelet- independent |
||||
| Thrombocytopenia | Complete fibrinogen deficiency: no change in serum ALT | ||||
| Enzymatic fibrinogen depletion: no effect on liver injury | |||||
| Plasminogen deficiency: ↓ hepatotoxicity | |||||
| Platelet depletion: ↓ hepatotoxicity | |||||
| PAI-1 deficiency: ↑ liver injury | |||||
| tPA administration: ↑ liver injury | |||||
| Liver cirrhosis (fibrosis) driven by different diseases (e.g., viral hepatitis, alcohol) |
Acute carbon tetrachloride hepatotoxicity |
Acute pericentral liver necrosis, lipid peroxidation and accumulation |
Hepatic fibrin(ogen) deposition within areas of necrosis |
Low molecular weight heparin/antithrombin: little protection against hepatotoxicity |
[19], [21], [23–24], [29–38] |
| Chronic carbon tetrachloride hepatotoxicity and bridging fibrosis |
Bridging hepatic fibrosis, cirrhosis, hepatocellular carcinoma |
Factor V Leiden: ↑ liver fibrosis | |||
| Complete fibrinogen deficiency: no change on gross pathology | |||||
| TAFI-deficiency: ↑ liver fibrosis, no effect on fibrin(ogen) deposition | |||||
| PAI-1 deficiency: ↑ liver fibrosis | |||||
| PAR-1 deficiency: ↓ liver fibrosis | |||||
| PAR-2 deficiency: ↓ liver fibrosis | |||||
| Bile duct obstruction | Common bile duct ligation in rodents |
Focal necrosis (bile infarcts), elevated bile acid levels and liver enzymes, fibrosis around proliferating bile ducts and fibrosis within bile infarcts |
Liver TF-driven thrombin generation: ↑ | Low TF: ↓coagulation | [30], [53–54], [58–61], [73–76], [78–81] |
| Hepatic fibrin(ogen) deposition within bile infarcts |
Liver-specific TF deletion: ↓ coagulation, no effect on liver injury or fibrosis |
||||
| Myeloid cell-specific TF deletion: no change in coagulation, no effect on liver injury or fibrosis |
|||||
| Monocyte TF expression: ↑ | Heterozygous antithrombin deficiency: ↑ liver injury | ||||
| Low molecular weight heparin: ↓ liver necrosis | |||||
| PAR-1 antagonists: ↓ liver damage | |||||
| PAI-1 deficiency: ↓ liver fibrosis | |||||
| Genetic thrombocytopenia: ↑ liver fibrosis | |||||
| PSC (cholangiofibrosis) |
Exposure to alpha- naphthylisothiocyanate |
Bile duct epithelial cell (BDEC) injury and hyperplasia, peribiliary fibrosis, cholestasis |
Thrombin generation: ↑ | Heterozygous TF deficiency: ↓ thrombin generation, ↓ peribiliary fibrosis, no change in liver enzymes |
[56], [70–72], [77], [99] |
| Hepatic fibrin(ogen) deposition: sinusoidal and peribiliary |
PAR-1 deficiency: ↓ fibrosis | ||||
| PAI-1 deficiency: ↑ fibrosis | |||||
| Complete fibrinogen deficiency: ↑ liver injury | |||||
| Tranexamic acid (antifibrinolytic): ↓ established fibrosis | |||||
| Mdr2−/− mice | Low dose aspirin: ↓ fibrosis | ||||
| Nonalcoholic fatty liver disease |
Western diet (various), methionine and choline- deficient (MCD) diet |
Steatosis, steatohepatitis, fibrosis |
TAT levels: ↑ | Hematopoietic cell TF deficiency: ↓ thrombin generation, ↓NAFLD pathology (hypercholesterolemic mice) |
[90–95] |
| Monocyte TF expression: ↑ | Thrombin inhibition (dabigatran): ↓ fatty liver, ↓ body weight gain |
||||
| Hepatic fibrin(ogen) deposition | Thrombin inhibition (argatroban): ↓inflammation, ↓stellate cell activation (hypercholesterolemic mice) |
||||
| PAR-1 deficiency: ↓fatty liver, ↓inflammation, no change in body weight gain |
|||||
| TF-PAR2 signaling inhibition: ↓ NAFLD pathology | |||||
Figure 1. Common themes in clinical and experimental studies of hemostasis and liver disease.
A large number of clinical studies have sought to discover the basis for altered hemostasis in liver disease (left). In contrast, very few studies have addressed changes in the hemostatic system that coincide with the development of experimental liver injury and disease in animal models (dashed arrow). Rather, studies in animal models have emphasized the mechanistic impact of the hemostatic system on liver toxicity and disease (right). Of importance, translation of these concepts is emerging in the form of clinical studies examining the impact of anticoagulants or antiplatelets on aspects of liver disease, particularly fibrosis (thin arrow). There is a need for additional studies examining hemostatic changes in experimental liver disease models and for continued clinical study defining the role of the hemostatic system in human liver injury and disease.
Whereas few studies have addressed how experimental liver injury and disease affect hemostasis, strong experimental evidence suggests that the blood coagulation cascade is also a powerful modifier of liver disease pathogenesis. Although intrinsically related to the question of how liver disease causes perturbed coagulation, it is the inverse question, of how coagulation can drive hepatic disease that has been the focus of the vast majority of animal models. As such, this is where we have focused this review. Here, we briefly review studies addressing coagulation activation and function in widely-utilized animal models of hepatic fibrosis and acute liver injury. For each our goal is to provide 1) working knowledge on the etiology/basis of the experimental pathology, 2) a current understanding of how procoagulant changes are elicited in each model, 3) and a review of evidence indicating how coagulation proteases, their targets, and other hemostatic factors can accelerate (or prevent) disease. Ultimately, we link these findings to observations in clinical studies assessing the effect of interventions on the hemostatic system, including coagulation proteases, on the progression of liver fibrosis, a penultimate and common feature of multiple chronic liver diseases.
Hemostatic system and acute liver failure in human patients
Acetaminophen (APAP) is widely considered as safe when taken at the recommended daily dose. However, APAP overdose remains the leading cause of acute liver failure (ALF) in the United States [2, 3]. Metabolism of APAP to the reactive metabolite N-acetyl-p-benzoquinone imine (NAPQI) causes centrilobular necrosis, which is exacerbated by engagement of multiple cellular and soluble mediators [4]. Strong evidence supports a consumptive coagulopathy in patients after APAP overdose, marked by thrombin generation and prolongation of the prothrombin time/international normalized ratio (PT/INR) [2, 5, 6], likely reflecting both consumption and failed coagulation factor synthesis by the injured liver [7, 8]. Notably, the prolonged INR and increased levels of tissue factor (TF)-positive microparticles are associated with poor outcome in ALF patients, but not necessarily with an increased bleeding risk [9]. Changes in the hemostatic system associated with ALF in humans have been reviewed in detail elsewhere [10].
Mouse model of APAP overdose
The classic model of APAP-induced liver injury involves intraperitoneal administration of APAP at a hepatotoxic dose (typically >250 mg/kg) and assessment of liver damage various times later. For the vast majority of studies, the dose selected produces marked hepatotoxicity that is followed by rapid liver repair and survival. Thus, interventions in this setting are often not performed with concurrent critical care (see advantages of large animal models below), although such studies may be of interest as failed liver repair and mortality are strictly connected to dose in this model [11]. Administration of a hepatotoxic dose of APAP to mice leads to rapid activation of coagulation cascade, marked by significant elevation of thrombin-antithrombin (TAT) levels as early as 2 hours after APAP administration, prolongation of the PT and increased fibrin deposition in areas of necrosis [12–15]. Thrombin generation, estimated by plasma TAT levels, is driven primarily by TF [12], and liver-specific TF deficiency largely prevents the early increase in TAT after APAP overdose [16]. Hepatic TF expression does not increase prior to thrombin generation after APAP overdose, implying that decryption of existing hepatocyte TF is central to coagulation after APAP overdose [16]. Many published studies indicate that TF-driven coagulation and thrombin activity are important for early APAP hepatotoxicity in mice. APAP hepatotoxicity is reduced in low TF mice, which express approximately 1% of normal TF levels [12]. Early APAP-induced liver injury (i.e., 6 hours after APAP administration) is significantly reduced by administration of either heparin or lepirudin [12, 14]. Notably, lepirudin was able to reduce liver damage when administered well after hepatic metabolism of APAP had completed [14]. The mechanism whereby thrombin exacerbates early APAP-induced liver injury appears to involve activation of protease activated receptors (PARs). Indeed, both PAR-1- and PAR-4-null mice develop less severe liver damage than their wild-type counterparts after administration of a hepatotoxic dose of APAP [12, 14]. The mechanism whereby PAR signaling enhances APAP hepatotoxicity is not completely understood, but it is interesting to note that involvement of PAR-4 appears independent of platelets.
Interestingly fibrinogen deficiency did not impact early APAP hepatotoxicity when compared to mice expressing 70% of normal fibrinogen levels [13]. Similar results were found when ancrod, which enzymatically depletes fibrinogen, was administered to wild-type mice [13]. This suggests that fibrin deposits are not a required element of the mechanism whereby APAP causes hepatotoxicity. Despite this, components of the fibrinolytic pathway appear pivotal for controlling early APAP hepatotoxicity. Plasminogen activator inhibitor-1 (PAI-1) expression in liver and plasma increases rapidly after APAP overdose in mice. Administration of recombinant tissue plasminogen activator (tPA) recapitulated the phenotype of PAI-1-deficient mice after APAP overdose leading to increased liver injury [13], and plasminogen deficiency significantly reduced APAP hepatotoxicity [13]. Collectively, these studies suggest a potentially fibrin-independent role of the plasminogen activator pathway in APAP hepatotoxicity. The precise mechanism whereby the plasminogen activators and plasmin drive APAP hepatotoxicity is not understood.
APAP overdose in mice and humans is associated with thrombocytopenia [14, 17]. In mice, the decrease in blood platelets is paralleled by platelet accumulation in the injured liver [14]. Importantly, prior depletion of platelets significantly reduced APAP hepatotoxicity in mice, suggesting their involvement in the pathogenesis. However, the exact mechanism whereby platelets accumulate and contribute to APAP hepatotoxicity is not understood.
Large animal models of coagulopathy of acute liver failure
Although the mouse model remains a robust and versatile experimental setting to investigate basic mechanisms of APAP hepatotoxicity and liver repair, there is a need to validate and expand upon large animal models more closely aligning to the human condition. At this juncture there remains a substantial opportunity to explore the coagulopathy of acute liver failure, and potentially intervention with anticoagulants, in models involving large animals, such as pigs. Indeed, the PT/INR is rapidly prolonged after APAP overdose in pigs, and this occurs alongside the predicted systemic consequences of ALF [18]. Here, clinical intervention very closely resembling the human condition can be applied alongside systematic sampling and assessment of changes in the hemostatic system. Routine use of models of this type is obviously costly and requires specialized facilities and engagement of veterinary expertise. However, such collaborations between human medicine, veterinary medicine, and toxicology may very well pave the way for studies examining the effect of anticoagulant intervention, identified using the mouse model, or other novel therapies after APAP overdose.
Hemostatic system and chronic liver injury/hepatic fibrosis
The majority of chronic liver injury and fibrosis models require administration of hepatotoxic chemicals. For example, hepatic fibrosis develops in rodents after chronic exposure to xenobiotics including carbon tetrachloride (CCl4), thioacetamide, alpha-naphthylisothiocyanate (ANIT), 3,5-diethoxycarbonyl-1,4-dihydrocollidine, or dimethyl- or diethyl-nitrosamine. The basis for each of these models has been reviewed elsewhere [19]. Hepatic fibrosis (i.e., excess deposition of collagen) is the typical pathology being explored, and often different models are pursued in tandem to identify pathways common to each experimental setting. However, like liver diseases of different etiologies (e.g., viral, metabolic, genetic, autoimmune), there are fundamental differences in the cellular mechanism whereby various toxicants damage the liver, and thus, large distinctions in the histological pattern of injury and fibrosis. Thus, it is perhaps not surprising that while there is a contribution of the hemostatic system in many models, the precise role of specific factors, including coagulation proteases, varies greatly between experimental settings. It is highly likely that liver damage will be associated with activation of the hemostatic system in nearly every experimental setting. Owing to space limitations, we have focused our review on models in which the greatest depth of investigation exists with respect to downstream mechanisms.
Carbon tetrachloride hepatotoxicity and fibrosis
CCl4 is a hepatotoxic carcinogen that previously had wide-ranging applications including as a component of shampoo, a degreaser and solvent, and even as a treatment for helminth infections [20]. CCl4 is now more widely appreciated as a model hepatotoxicant capable of producing a range of pathologies in liver. Acute administration of CCl4 to rodents induces acute liver necrosis. Mechanisms of CCl4 hepatotoxicity have been described in detail elsewhere [20]. In brief, CCl4 is metabolized to a free radical form by cytochrome P450 enzymes in hepatic parenchymal cells (i.e., hepatocytes). This leads to hepatic parenchymal cell damage by multiple mechanisms, including disruption of intracellular calcium homeostasis and lipid peroxidation [21, 22]. The lesion produced by acute CCl4 administration is typified by necrosis of centrilobular hepatocytes, which undergo wound healing to restore normal hepatic architecture [19, 23]. Persistent hepatocellular injury elicited by chronic CCl4 administration to rodents, typically every 3–4 days, for several weeks, results in bridging hepatic fibrosis. Very prolonged exposure, particularly in rats, produces cirrhosis and even hepatocellular carcinoma [19, 24]. This model has been extensively utilized to decipher fundamental mechanisms of hepatic stellate cell activation and hepatic fibrosis.
The concept and role of the hemostatic system in CCl4 hepatotoxicity have been reinvigorated multiple times over the last half century, with even early reports noting thrombin-driven fibrin deposition in the injured liver [25, 26]. These studies and others were among the first to investigate the beneficial impact of heparin and antithrombin on hepatotoxicity [27, 28]. Additional studies more elegantly demonstrated deposition of fibrin within areas of centrilobular necrosis after both acute and chronic injury [29]. Collectively, these studies revealed a robust procoagulant response occurring after CCl4 administration and set the stage for later studies interested in hemostasis in the context of CCl4-induced fibrosis.
More in-depth experimentation has suggested that inhibition of coagulation with low molecular weight heparin or exogenous antithrombin affords little protection against acute CCl4 hepatotoxicity [30–32]. However, the protection afforded by anticoagulants is certainly toxin-specific, as thrombin inhibitors reduce acute liver damage elicited by dimethyl-nitrosamine [32] and APAP [12, 14], as mentioned previously. Although there is a lack of consistent evidence supporting a pathologic role for coagulation after acute CCl4 administration, strong experimental evidence indicates that thrombin activity enhances hepatic stellate cell activation and liver fibrosis driven by repeated administration of CCl4 [31]. It is very interesting that chronic CCl4-induced liver fibrosis is increased in procoagulant factor V-Leiden mice, presumably due to increased thrombin generating capacity, although an increase in thrombin activity was not directly demonstrated [33]. Collectively, these studies provide strong evidence in support of a profibrogenic effect of coagulation in experimental chronic CCl4-induced liver fibrosis.
One clear advantage of the mouse (and rat) models of fibrosis is the ability to delineate mechanisms whereby coagulation contributes to liver pathology. For CCl4-induced fibrosis, the majority of studies have considered pathways whereby coagulation factor Xa and thrombin could increase hepatic fibrosis. One obvious thrombin target that could exacerbate the fibrotic response is fibrin(ogen), as fibrin deposits are present in liver after both acute and chronic CCl4 administration [29, 34]. Similar to the role of fibrin(ogen) in thrombotic occlusion of large vessels, fibrin deposition is often assumed to contribute to liver pathology through hypoxic occlusion of liver blood vessels or by promoting inflammatory cell activation. However, the exact function of fibrin(ogen) in this model remains virtually unexplored. The only published study directly addressing the role of fibrin(ogen) in the CCl4 model is from Bezerra and colleagues, who reported no effect of complete fibrinogen deficiency on gross liver pathology after chronic CCl4 administration [35]. Several studies have examined the role of fibrinolysis after CCl4 administration. Plasmin(ogen) is essential for liver repair after chronic CCl4 administration, although elegant studies suggest the critical plasmin substrate is a non-fibrin matrix [35]. Thrombin-activatable fibrinolysis inhibitor (TAFI) deficiency increased CCl4-induced fibrosis, but TAFI deficiency had no effect on hepatic fibrin deposition [34]. PAI-1 deficiency, which would be anticipated to decrease hepatic fibrin deposition, increased CCl4-induced hepatic fibrosis [36], although the impact of PAI-1 deficiency on fibrin in this model is not clear. Altogether, the available literature is insufficient to support either beneficial or damaging effects of fibrin(ogen) after chronic CCl4 administration.
There is strong experimental evidence to suggest that thrombin exacerbates CCl4-induced liver fibrosis via activation of the PARs. PAR-1 or PAR-2 deficiency significantly reduced CCl4-induced liver fibrosis [37, 38], implying that signaling downstream of thrombin or factor Xa, respectively, could enhance fibrosis. This is consistent with cell culture studies demonstrating that thrombin signaling enhances the myofibroblast differentiation of hepatic stellate cells [39]. However, no published work has demonstrated that a direct thrombin activation of PAR-1 on stellate cells increases fibrosis in vivo. Such studies will likely be possible with the emergence of mice expressing a conditional PAR-1 allele and stellate cell-selective Cre mice [40]. Recent studies suggest that PAR-1 expressed by hematopoietic cells, particularly monocytes/macrophages, may also indirectly exacerbate CCl4-induced liver fibrosis [41]. Worth noting, the application of PAR-1-null mice for investigation of experimental fibrosis is complicated by the lack of PAR-1 expression on mouse platelets [42]. Thus, PAR-1-deficient mice provide a “clean” system to study how thrombin promotes hepatic fibrosis in the absence of an effect on thrombin-driven platelet activation. However, the impact of thrombin-mediated platelet activation is not addressed in these mice, which is certainly knowledge required to translate these results to humans, where PAR-1 is critical for platelet activation as well as having potentially independent profibrogenic function in liver. With many studies suggesting that platelets can drive liver pathology caused by common indications, such as viral infection [43] and steatohepatitis [44], it seems plausible that PAR-1 antagonists such as vorapaxar could have therapeutic utility.
It is worth noting that deficits in thrombin-mediated platelet activation are associated with increased liver injury/fibrosis in some settings, and platelet-derived mediators also have a well-appreciated role in liver repair. However, there are very few studies examining the effect of thrombocytopenia or highly selective platelet inhibitors on CCl4-induced liver fibrosis. Administration of aspirin or ibuprofen attenuated CCl4-induced liver fibrosis in rats, but neither drug is entirely platelet-specific, and each significantly attenuated hepatic lipid peroxidation and injury, the earliest steps in CCl4-induced liver fibrosis [45]. Clopidogrel administration had no effect on hepatic α-smooth muscle actin expression or collagen deposition in mice exposed chronically to CCl4 [46]. Unlike cholestatic liver injury (below), the impact of specific thrombocytopenia has not been evaluated in the CCl4 model. Interestingly experimental thrombocytosis and human platelet transfusion were found to reduce chronic CCl4-induced liver fibrosis in exposed mice [47, 48]. Overall, the precise role of platelets in CCl4-induced liver fibrosis has not been defined. This is in notable contrast to the setting of viral liver damage, where in both humans and experimental animals the inhibition of platelets appears to be associated with a reduction in liver fibrosis [43, 49, 50].
Models of bile duct injury and cholestasis
Although liver fibrosis models converge at exaggerated deposition of collagen, the stimuli for hepatic injury/disease that define the path to this outcome are varied. Whereas CCl4 is best recognized as a hepatocellular toxicant, other liver pathologies trigger disease and fibrosis through distinct cell types/pathways. Commonality is often sought, and found, in mechanisms of liver fibrosis across models. However, variation in mechanisms should be anticipated given differences in each experimental insult. This is the case for the role of hemostatic system in cholestatic liver injury. Cholestatic liver injury can be broadly defined as a condition in which bile flow through the liver is disrupted, often resulting in the release of components of the bile into the blood [51]. Bile acids produced by hepatocytes are ultimately transported into intrahepatic bile ducts lined by epithelial cells [52]. Components of bile, particularly bile acids, are particularly proinflammatory and can elicit inflammatory liver damage secondary to activation of multiple receptors [52, 53]. Insults to the liver that disrupt the intrahepatic bile flow trigger hepatic injury that can lead to fibrosis, often with a pattern distinct from CCl4. There are several models of this unique condition, not all of which readily produce hepatic fibrosis, including common bile duct ligation (BDL), ANIT exposure, Mdr2 deficiency, and autoimmunity in CD4-Tg dnTGFβRII mice [54–57]. We will focus our review on ANIT and BDL, as the vast majority of work on the hemostatic system has been done in these models.
Common bile duct ligation
Ligation of the common bile duct in the mouse or rat represents a model of acute obstructive cholestatic liver damage, best approximating obstruction of the common bile duct in humans by a gall-stone, tumor, etc. Increased biliary pressure results in rupture of intrahepatic bile ducts and spillage of bile into the hepatic parenchyma. The bile levels and composition of bile acids released into the serum have been carefully quantified in both humans and mice. Direct cytotoxic and proinflammatory effects of bile acids generate focal necrosis, formed in large part by the recruitment and activation of neutrophils [53, 58, 59]. Complete biliary obstruction in humans necessitates rapid surgical correction (i.e., removal of the stone or tumor). In rodents, however, BDL is frequently explored in long-term settings (~28 days) as a stimulus for liver fibrosis [54]. Hepatic necrosis and transaminase elevation persists with the fibrosis, often yielding two distinct areas of fibrosis, mainly around proliferating bile ducts and also within areas of hepatic necrosis [54, 60]. Several distinct mechanisms of fibrosis, including profibrogenic integrin expression by bile duct epithelial cells (BDECs), makes the pathway to fibrosis after BDL different from CCl4 [61].
Alpha-naphthylisothiocyanate exposure
ANIT is a xenobiotic with a unique toxicological profile [62]. Hepatocytes in vivo detoxify ANIT through conjugation to glutathione, and this conjugate is transported into the bile by the canalicular transporter MRP2 [63]. However, for reasons that are not clear, this conjugate is unstable in bile [64]. Enterohepatic recirculation allows multiple rounds of ANIT metabolism, conjugation and biliary transport, resulting in a high concentration of ANIT in the bile, which can selectively injure BDECs [63, 65]. Biliary transport of ANIT by MRP2 is essential for hepatic parenchymal cell injury from ANIT [63]. Single, large doses of ANIT produce acute cholestatic liver injury in mice and rats, sharing pathological features and mechanistic similarity to BDL [66, 67]. As with CCl4, chronic exposure to ANIT also causes liver fibrosis, albeit with a different histological picture. Prolonged exposure (>2 weeks) of mice and rats to ANIT (via chow) recapitulates the pathological features of primary sclerosing cholangitis (PSC) characterized by portal lymphocytic inflammation, biliary hyperplasia and fibrosis of the bile ducts [56, 68, 69]. As in PSC, chronic ANIT-exposure is associated with elevations in serum bile acids and markers of biliary injury (e.g. alkaline phosphatase) with minimal to no change in markers of hepatocellular injury (i.e. alanine aminotransferase) [56, 69, 70]. Chronic ANIT exposure therefore serves as a unique model to define mechanisms of liver fibrosis caused directly by chronic BDEC cytotoxicity.
Cholestatic liver injury in mice is associated with activation of the coagulation cascade. BDECs, which line intrahepatic bile ducts, and hepatocytes, have each been shown to express TF [71]. BDL and ANIT models are associated with increased thrombin generation and deposition of fibrin in liver [56, 72]. In BDL, fibrin deposits are primarily within “bile infarcts,” a colloquial term for areas of bile-filled necrotic lesions present after BDL [73]. Deposition of fibrin in these lesions is also evident in ANIT-exposed mice [56], although these necrotic lesions are observed less frequently. Chronic ANIT exposure also causes sinusoidal and peribiliary fibrin deposition [56, 72]. The mechanism of coagulation cascade activation in these models is increasingly understood. Although monocytes express TF in patients with cholestasis, coagulation after BDL is driven by liver-associated TF, most likely expressed by hepatocytes or BDECs [74].
Deciphering the role of coagulation in the cholestatic liver injury models has revealed exciting dichotomy, and raises interesting questions on how the etiology of liver damage could impact downstream consequences of coagulation. For example, whereas coagulation was dramatically reduced in low TF mice and mice with liver-specific TF deficiency after BDL, hepatic injury and fibrosis were not affected [74]. The lack of effect of TF is intriguing in the context of other studies demonstrating that heterozygous antithrombin deficiency increases injury after BDL [30] and low molecular weight heparin reduces BDL-associated liver necrosis [75]. Interestingly, heterozygous TF deficiency attenuated thrombin generation and reduced peribiliary fibrosis in ANIT-exposed mice, without affecting serum liver enzyme levels [72]. Like CCl4-induced liver fibrosis, the mechanism whereby coagulation drives fibrosis most likely relates to PAR signaling. Indeed, PAR-1 deficiency significantly reduced liver fibrosis in ANIT-exposed mice [72]. Although there is no published evidence of BDL in PAR-1−/− mice, in unpublished preliminary studies we found that profibrogenic gene induction (e.g., COL1A1 and ACTA2) tended to decrease in PAR-1-deficient mice after 5 days of BDL (Luyendyk JP, Copple BL, unpublished results). Moreover, a PAR-1 antagonist attenuated BDL-associated liver damage in rats [76]. Collectively, and like CCl4-induced liver fibrosis, there is sufficient experimental evidence in support of a pathologic role of thrombin, through PAR-1 signaling, in liver fibrosis induced by cholestasis.
Despite the ANIT and BDL models causing chronic bile duct injury and similar peribiliary fibrosis, there is a dichotomy in the involvement of fibrinolytic pathways in the injury and fibrosis. Like chronic CCl4 administration, PAI-1 deficiency exacerbates ANIT-induced fibrosis in mice [77]. In striking contrast, PAI-1-deficient mice display a dramatic reduction in liver injury after BDL [73, 78]. Although PAI-1-deficient mice have a reduction in hepatic fibrin deposition after BDL, the role of fibrinogen in this model has not been examined. In light of work from Rautou et al. indicating that hepatocyte TF generates thrombin after BDL [74], it is likely that fibrin deposition is reduced in PAI-1-deficient mice simply as a function of reduced injury. Indeed, this is consistent with follow-up studies indicating that BDL-induced liver damage is tPA-driven, but neither PAI-1 nor tPA deficiency affects hepatic plasmin activity [79, 80]. Like the CCl4 model, the exact role of fibrin(ogen) and hepatic fibrin deposition after BDL remains unclear.
The only model of chronic liver injury and fibrosis where the precise role of fibrin(ogen) has been addressed is chronic ANIT exposure. Here, complete fibrinogen deficiency increased liver injury [70] and administration of the antifibrinolytic drug tranexamic acid significantly reduced established biliary fibrosis [77]. This suggests that PAI-1 deficiency could in fact increase fibrosis in this model by enabling a hyperfibrinolytic state [77]. The mechanism whereby fibrin(ogen) reduces hepatocellular injury elicited by chronic ANIT exposure involves the capacity of the molecule to engage platelets through the platelet integrin αIIBβ3. Mice expressing a mutant fibrinogen lacking this specific functional domain developed liver damage resembling mice completely lacking fibrinogen when exposed to chronic ANIT [56]. Collectively, the results suggest that under certain circumstances, fibrinogen may function to inhibit liver fibrosis or perhaps promote repair.
Studies with chronic ANIT exposure illustrated how one protective function of fibrin(ogen) in chronic cholestatic liver injury could be through activation of platelets. The exact role of platelets in chronic ANIT-mediated biliary fibrosis is not known. However, genetic thrombocytopenia significantly increased liver fibrosis in mice after BDL [81]. Interestingly, this finding was not linked to an increase in parenchymal cell necrosis. Rather, thrombocytopenia significantly reduced liver necrosis [81]. This is consistent with previous studies suggesting that platelets promote acute cholestatic liver injury. Collectively, these studies demonstrate a disconnect between biliary fibrosis and necrosis after BDL, and suggest diverse functions for platelets in acute and chronic cholestatic liver injury.
Non-alcoholic fatty liver disease and steatohepatitis
Non-alcoholic fatty liver disease (NAFLD) and its severe form non-alcoholic steatohepatitis (NASH) represent one of the most prevalent liver diseases in both adults and children in developed countries [82, 83]. This is a spectrum disorder, where simple steatosis (liver triglyceride accumulation) can transition to a hepatic inflammatory state and ultimately to liver fibrosis and cirrhosis. The primary risk factors for NAFLD, obesity and metabolic syndrome, are associated with a procoagulant state, and many studies have linked this procoagulant state to disturbances in coagulation factor expression by the liver [84–87]. Interestingly, biomarkers of coagulation often mark the progression of the disease to a more severe state, and prothrombotic risk factors are linked to more advanced disease in humans [85, 86]. Such studies suggest that changes in coagulation may not simply be a reflection of disease, but rather increased coagulation could play a central role in NAFLD pathogenesis. Indeed, this hypothesis is supported by direct mechanistic evidence derived experimentally in rodent models of diet-induced NAFLD and NASH.
Experimental settings of NAFLD/NASH include, but are not limited to, dietary interventions such as the high fat (HFD) and/or high carbohydrate diets in which liver pathology can be evaluated in the context of obesity and insulin resistance, and the methionine-choline deficient (MCD) diet, which rapidly produces liver histopathology resembling NASH and hepatic fibrosis [88, 89]. Like obese patients, monocyte TF expression increases in mice fed a HFD and this is associated with increased thrombin generation [90]. Interestingly, hematopoietic cell TF deficiency dramatically reduced thrombin generation and NAFLD pathology in hypercholesterolemic mice [90, 91], implying a key role for coagulation in the pathogenesis of fatty liver. Indeed, administration of the direct thrombin inhibitor dabigatran etexilate protected mice from HFD-induced fatty liver disease [92]. Moreover, therapeutic administration of argatroban to hypercholesterolemic mice with established fatty liver significantly reduced inflammation and stellate cell activation [93]. Like other models, the role of thrombin is likely mediated through PAR-1, as PAR-1-deficient mice exhibit near complete protection from HFD-induced fatty liver, despite gaining a similar amount of body weight [91]. Similarly, TF deficiency and PAR-1 deficiency reduced hepatic inflammation and injury in mice fed an MCD diet [94]. However, both TF deficiency and thrombin inhibition, along with TF-PAR-2 signaling, are each able to impact diet-induced obesity at large, implying that this pathway also plays a more global role in obesity [90, 95]. In summary, there is experimental evidence in multiple mouse models of NAFLD/NASH to suggest that coagulation can participate as an inducible modifier of fatty liver pathogenesis and perhaps ensuing fibrosis. Although exciting, it is important to note that translation of this concept to the clinic has not yet been realized.
Summary, challenges and perspectives
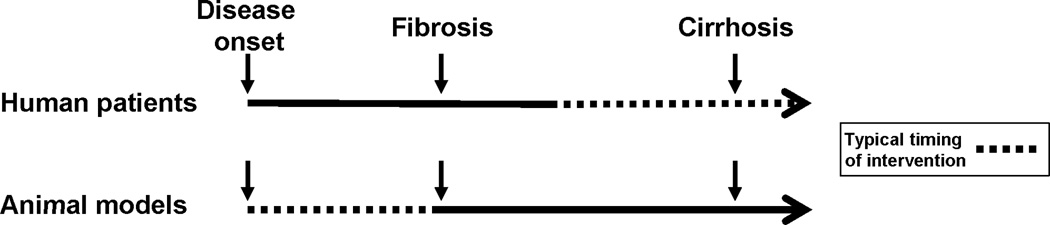
Hemostatic factors modifying liver disease
Our knowledge of how the hemostatic system can modify the pathogenesis of liver toxicity and disease is heavily weighted on studies using experimental animal models (Fig. 1), which while very informative, are not likely to achieve severity of disease observed clinically (Fig. 2). The emphasis has primarily been on mechanisms whereby thrombin and its targets modify the extent and progression of diverse liver pathologies. Clinical translation of these concepts is now emerging (Fig. 1), with several studies in patients identifying elements of the hemostatic system as a potential determinant of disease progression [96]. For example, the prothrombotic factor V-Leiden polymorphism increases the risk of fibrosis in patients with hepatitis C virus (HCV) [97], an observation consistent with the increased fibrosis observed in mice harboring the factor V-Leiden mutation after chronic CCl4 exposure [33]. One retrospective analysis suggested that antiplatelets, such as aspirin, can reduce the severity of hepatic fibrosis in patients with HCV [98], a result consistent with the reduction in fibrosis by low dose aspirin in mice [99]. One distinction here is that many interventions or analyses are done in patients with established liver disease (Fig. 2), although some ongoing studies, such as the WAFT-C trial, are examining the impact of warfarin in patients with mild liver disease. Building on strong evidence that anticoagulants reduce liver fibrosis in mouse models, it is conceivable that clinical use of anticoagulants such as warfarin and heparin, or new direct thrombin and Xa inhibitors, could reduce hepatic fibrosis. Although conceivable, the rationale is a balance of benefits and risks and this has been reviewed recently [100]. In summary, there is convincing evidence from animal models that components of the hemostatic system, particularly coagulation proteases, contribute to the pathogenesis of acute and chronic liver disease (Table 1). Moreover, despite some differences (Fig. 2), there is clinical evidence to support the basic research in this area. Additional studies exploring interventions targeting the hemostatic system in patients with various stages of disease, and refinement of animal models to test the impact of anticoagulants on established liver disease would each greatly benefit the field.
Figure 2. Distinct differences in clinical and basic research studies assessing anticoagulant intervention in liver fibrosis/cirrhosis.
Whereas the majority of anticoagulant trials in patients have been performed in patients with established liver disease/cirrhosis, few if any animal studies have addressed the impact of anticoagulants or genetic interventions on established liver fibrosis or severe cirrhosis. Rather, these studies address the role of hemostasis during the earliest phase of disease development. From a translational standpoint, it is important that this distinction be considered.
Liver disease modifying the hemostatic system
While there is considerable investment in clinical studies seeking to understand how hemostatic components modify liver disease, a larger volume of clinical research has been focused on the reciprocal relationship; that is, understanding how liver disease leads to complications like bleeding or thrombosis (Fig. 1). Very few studies have systematically assessed the hemostatic changes that accompany experimental acute liver injury and chronic liver disease in animal models (Fig. 1). The emergence of tools such as mice with liver-specific TF deficiency offers opportunity to define how the coagulation cascade is activated in experimental acute and chronic liver injury, which could potentially explain if and how pathologic intrahepatic coagulation occurs in humans with liver disease. Combined application of small and large animal models of APAP overdose, for example, is likely to yield valid insight into the nature of the consumptive coagulopathy occurring in patients with ALF. Defining the precise mechanism of coagulation cascade activation after liver injury does not fully address the entire scope of hemostatic changes occurring alongside liver pathology. Indeed, there is a need to fully characterize the hemostatic system in models of acute and chronic liver injury and based on this, refine existing or develop innovative experimental settings that recapitulate the precariously rebalanced hemostatic system observed in patients with severe liver disease. This will most likely be achieved through close collaboration between clinical investigators and basic scientists spanning the fields of hematology and hepatology.
Acknowledgments
Funding information
This work was supported by grants from the National Institutes of Health, National Institute of Environmental Health Sciences (NIEHS) [R01 ES017537] and National Institutes of Diabetes and Digestive and Kidney Diseases (NIDDK) [R01 DK105099]. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIEHS or NIDDK.
Footnotes
Author contributions
Wrote the initial draft of introductory and closing material, carbon tetrachloride and bile duct ligation section: J. P. Luyendyk, A. K. Kopec
Wrote the initial draft of the acetaminophen section: A. K. Kopec
Wrote the initial draft of the alpha-naphthylisothiocyanate section: N. Joshi.
Final and significant editorial contribution and approval of the version to be published: A. K. Kopec, N. Joshi, J. P. Luyendyk
Disclosure
A. K. Kopec, N. Joshi and J. P. Luyendyk report grants from National Institutes of Health, during the conduct of the study.
References
- 1.Lisman T, Caldwell SH, Burroughs AK, Northup PG, Senzolo M, Stravitz RT, Tripodi A, Trotter JF, Valla DC, Porte RJ Group CiLDS. Hemostasis and thrombosis in patients with liver disease: the ups and downs. J Hepatol. 2010;53:362–371. doi: 10.1016/j.jhep.2010.01.042. [DOI] [PubMed] [Google Scholar]
- 2.Larson AM, Polson J, Fontana RJ, Davern TJ, Lalani E, Hynan LS, Reisch JS, Schiødt FV, Ostapowicz G, Shakil AO, Lee WM Group ALFS. Acetaminophen-induced acute liver failure: results of a United States multicenter, prospective study. Hepatology. 2005;42:1364–1372. doi: 10.1002/hep.20948. [DOI] [PubMed] [Google Scholar]
- 3.Fontana RJ, Ellerbe C, Durkalski VE, Rangnekar A, Reddy RK, Stravitz T, McGuire B, Davern T, Reuben A, Liou I, Fix O, Ganger DR, Chung RT, Schilsky M, Han S, Hynan LS, Sanders C, Lee WM Group UALFS. Two-year outcomes in initial survivors with acute liver failure: results from a prospective, multicentre study. Liver Int. 2015;35:370–380. doi: 10.1111/liv.12632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jaeschke H, Bajt ML. Comprehensive Toxicology - Hepatic Toxicology 9.21 - Mechanisms of Acetaminophen Hepatotoxicity. 2010 [Google Scholar]
- 5.Harrison PM, O’Grady JG, Keays RT, Alexander GJ, Williams R. Serial prothrombin time as prognostic indicator in paracetamol induced fulminant hepatic failure. BMJ. 1990;1990;301:964–966. doi: 10.1136/bmj.301.6758.964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kerr R, Newsome P, Germain L, Thomson E, Dawson P, Stirling D, Ludlam CA. Effects of acute liver injury on blood coagulation. J Thromb Haemost. 2003;2003;1:754–759. doi: 10.1046/j.1538-7836.2003.00194.x. [DOI] [PubMed] [Google Scholar]
- 7.Gazzard BG, Henderson JM, Williams R. Early changes in coagulation following a paracetamol overdose and a controlled trial of fresh frozen plasma therapy. Gut. 1975;1975;16:617–620. doi: 10.1136/gut.16.8.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Payen C, Dachraoui A, Pulce C, Descotes J. Prothrombin time prolongation in paracetamol poisoning: a relevant marker of hepatic failure? Hum Exp Toxicol. 2003;22:617–621. doi: 10.1191/0960327103ht398oa. [DOI] [PubMed] [Google Scholar]
- 9.Stravitz RT, Bowling R, Bradford RL, Key NS, Glover S, Thacker LR Gabriel DA. Role of procoagulant microparticles in mediating complications and outcome of acute liver injury/acute liver failure. Hepatology. 2013;58:304–313. doi: 10.1002/hep.26307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lisman T, Stravitz RT. Rebalanced Hemostasis in Patients with Acute Liver Failure. Semin Thromb Hemost. 2015;41:468–473. doi: 10.1055/s-0035-1550430. [DOI] [PubMed] [Google Scholar]
- 11.Bhushan B, Walesky C, Manley M, Gallagher T, Borude P, Edwards G, Monga SP, Apte U. Pro-regenerative signaling after acetaminophen-induced acute liver injury in mice identified using a novel incremental dose model. Am J Pathol. 2014;184:3013–3025. doi: 10.1016/j.ajpath.2014.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ganey PE, Luyendyk JP, Newport SW, Eagle TM, Maddox JF, Mackman N, Roth RA. Role of the coagulation system in acetaminophen-induced hepatotoxicity in mice. Hepatology. 2007;46:1177–1186. doi: 10.1002/hep.21779. [DOI] [PubMed] [Google Scholar]
- 13.Sullivan BP, Kassel KM, Jone A, Flick MJ, Luyendyk JP. Fibrin(ogen)-independent role of plasminogen activators in acetaminophen-induced liver injury. Am J Pathol. 2012;180:2321–2329. doi: 10.1016/j.ajpath.2012.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Miyakawa K, Joshi N, Sullivan BP, Albee R, Brandenberger C, Jaeschke H, McGill MR, Scott MA, Ganey PE, Luyendyk JP, Roth RA. Platelets protease-activated receptor-4 contribute to acetaminophen-induced liver injury in mice. Blood. doi: 10.1182/blood-2014-09-598656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hughes RD, Gove CD, Williams R. Protective effects of propylene glycol, a solvent used pharmaceutically, against paracetamol-induced liver injury in mice. Biochem Pharmacol. 1991;1991;42:710–713. doi: 10.1016/0006-2952(91)90339-7. [DOI] [PubMed] [Google Scholar]
- 16.Sullivan BP, Kopec AK, Joshi N, Cline H, Brown JA, Bishop SC, Kassel KM, Rockwell C, Mackman N, Luyendyk JP. Hepatocyte tissue factor activates the coagulation cascade in mice. Blood. 2013;121:1868–1874. doi: 10.1182/blood-2012-09-455436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fischereder M, Jaffe JP. Thrombocytopenia following acute acetaminophen overdose. Am J Hematol. 1994;1994;45:258–259. doi: 10.1002/ajh.2830450313. [DOI] [PubMed] [Google Scholar]
- 18.Lee KC, Palacios Jimenez C, Alibhai H, Chang YM, Leckie PJ, Baker LA, Stanzani GL, Priestnall S, Mookerjee RP, Jalan R, Davies NA. A reproducible, clinically relevant, intensively managed, pig model of acute liver failure for testing of therapies aimed to prolong survival. Liver Int. 2013;33:544–551. doi: 10.1111/liv.12042. [DOI] [PubMed] [Google Scholar]
- 19.Martínez AK, Maroni L, Marzioni M, Ahmed ST, Milad M, Ray D, Alpini G, Glaser SS. Mouse models of liver fibrosis mimic human liver fibrosis of different etiologies. Curr Pathobiol Rep. 2014;2:143–153. doi: 10.1007/s40139-014-0050-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fujimoto J, Iimuro Y. Comprehensive Toxicology - Hepatic Toxicology 9.20 - Carbon Tetrachloride-Induced Hepatotoxicity. 2010 [Google Scholar]
- 21.Recknagel RO, Glende EA, Dolak JA, Waller RL. Mechanisms of carbon tetrachloride toxicity. Pharmacol Ther. 1989;1989;43:139–154. doi: 10.1016/0163-7258(89)90050-8. [DOI] [PubMed] [Google Scholar]
- 22.Castro GD, Díaz Gómez MI, Castro JA. Biotransformation of carbon tetrachloride and lipid peroxidation promotion by liver nuclear preparations from different animal species. Cancer Lett. 1990;1990;53:9–15. doi: 10.1016/0304-3835(90)90004-h. [DOI] [PubMed] [Google Scholar]
- 23.Bruckner JV, MacKenzie WF, Muralidhara S, Luthra R, Kyle GM, Acosta D. Oral toxicity of carbon tetrachloride: acute, subacute, and subchronic studies in rats. Fundam Appl Toxicol. 1986;1986;6:16–34. doi: 10.1016/0272-0590(86)90260-5. [DOI] [PubMed] [Google Scholar]
- 24.Domenicali M, Caraceni P, Giannone F, Baldassarre M, Lucchetti G, Quarta C, Patti C, Catani L, Nanni C, Lemoli RM, Bernardi M. A novel model of CCl4-induced cirrhosis with ascites in the mouse. J Hepatol. 2009;51:991–999. doi: 10.1016/j.jhep.2009.09.008. [DOI] [PubMed] [Google Scholar]
- 25.Rake MO, Flute PT, Pannell G, Shilkin KB, Williams R. Experimental hepatic necrosis: studies on coagulation abnormalities, plasma clearance, and organ distribution of 125I–labelled fibrinogen. Gut. 1973;1973;14:574–580. doi: 10.1136/gut.14.7.574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rice CE, Boulanger RP, Plummer PJ. Parallel studies of complement, coagulation. IVEffect of carbon tetrachloride. Can J Med Sci. 1951;1951;29:48–58. doi: 10.1139/cjms51-006. [DOI] [PubMed] [Google Scholar]
- 27.Ronneberger H. Influence of antithrombin III on carbon tetrachloride intoxication of rabbits. Arch Toxicol Suppl. 1985;1985;8:156–159. doi: 10.1007/978-3-642-69928-3_23. [DOI] [PubMed] [Google Scholar]
- 28.Rake MO, Flute PT, Shilkin KB, Williams R. Intravascular coagulation in acute hepatic necrosis: clinical and experimental studies into the deposition of microthrombi and the effect of treatment. Gut. 1971;1971;12:868–869. [PubMed] [Google Scholar]
- 29.Neubauer K, Knittel T, Armbrust T, Ramadori G. Accumulation and cellular localization of fibrinogen/fibrin during short-term and long-term rat liver injury. Gastroenterology. 1995;1995;108:1124–1135. doi: 10.1016/0016-5085(95)90211-2. [DOI] [PubMed] [Google Scholar]
- 30.Guerrero JA, Teruel R, Martínez C, Arcas I, Martínez-Martínez I, de la Morena-Barrio ME, Vicente V, Corral J. Protective role of antithrombin in mouse models of liver injury. J Hepatol. 2012;57:980–986. doi: 10.1016/j.jhep.2012.06.023. [DOI] [PubMed] [Google Scholar]
- 31.Abe W, Ikejima K, Lang T, Okumura K, Enomoto N, Kitamura T, Takei Y, Sato N. Low molecular weight heparin prevents hepatic fibrogenesis caused by carbon tetrachloride in the rat. J Hepatol. 2007;46:286–294. doi: 10.1016/j.jhep.2006.08.023. [DOI] [PubMed] [Google Scholar]
- 32.Fujiwara K, Ogata I, Ohta Y, Hirata K, Oka Y, Yamada S, Sato Y, Masaki N, Oka H. Intravascular coagulation in acute liver failure in rats and its treatment with antithrombin III. Gut. 1988;1988;29:1103–1108. doi: 10.1136/gut.29.8.1103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Anstee QM, Goldin RD, Wright M, Martinelli A, Cox R, Thursz MR. Coagulation status modulates murine hepatic fibrogenesis: implications for the development of novel therapies. J Thromb Haemost. 2008;6:1336–1343. doi: 10.1111/j.1538-7836.2008.03015.x. [DOI] [PubMed] [Google Scholar]
- 34.Hugenholtz GC, Meijers JC, Adelmeijer J, Porte RJ, Lisman T. TAFI deficiency promotes liver damage in murine models of liver failure through defective down-regulation of hepatic inflammation. Thromb Haemost. 2013;109:948–955. doi: 10.1160/TH12-12-0930. [DOI] [PubMed] [Google Scholar]
- 35.Pohl JF, Melin-Aldana H, Sabla G, Degen JL, Bezerra JA. Plasminogen deficiency leads to impaired lobular reorganization and matrix accumulation after chronic liver injury. Am J Pathol. 2001;159:2179–2186. doi: 10.1016/S0002-9440(10)63069-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.von Montfort C, Beier JI, Kaiser JP, Guo L, Joshi-Barve S, Pritchard MT, States JC, Arteel GE. PAI-1 plays a protective role in CCl4-induced hepatic fibrosis in mice: role of hepatocyte division. Am J Physiol Gastrointest Liver Physiol. 2010;298:G657–G666. doi: 10.1152/ajpgi.00107.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rullier A, Gillibert-Duplantier J, Costet P, Cubel G, Haurie V, Petibois C, Taras D, Dugot-Senant N, Deleris G, Bioulac-Sage P, Rosenbaum J. Protease-activated receptor 1 knockout reduces experimentally induced liver fibrosis. Am J Physiol Gastrointest Liver Physiol. 2008;294:G226–G235. doi: 10.1152/ajpgi.00444.2007. [DOI] [PubMed] [Google Scholar]
- 38.Knight V, Tchongue J, Lourensz D, Tipping P, Sievert W. Protease-activated receptor 2 promotes experimental liver fibrosis in mice and activates human hepatic stellate cells. Hepatology. 2012;55:879–887. doi: 10.1002/hep.24784. [DOI] [PubMed] [Google Scholar]
- 39.Gaça MD, Zhou X, Benyon RC. Regulation of hepatic stellate cell proliferation and collagen synthesis by proteinase-activated receptors. J Hepatol. 2002;2002;36:362–369. doi: 10.1016/s0168-8278(01)00285-9. [DOI] [PubMed] [Google Scholar]
- 40.Mederacke I, Hsu CC, Troeger JS, Huebener P, Mu X, Dapito DH, Pradere JP, Schwabe RF. Fate tracing reveals hepatic stellate cells as dominant contributors to liver fibrosis independent of its aetiology. Nat Commun. 2013;2013;4:2823. doi: 10.1038/ncomms3823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kallis YN, Scotton CJ, Mackinnon AC, Goldin RD, Wright NA, Iredale JP, Chambers RC, Forbes SJ. Proteinase activated receptor 1 mediated fibrosis in a mouse model of liver injury: a role for bone marrow derived macrophages. PLoS One. 2014;9:e86241. doi: 10.1371/journal.pone.0086241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Connolly AJ, Ishihara H, Kahn ML, Farese RV, Coughlin SR. Role of the thrombin receptor in development and evidence for a second receptor. Nature. 1996;381:516–519. doi: 10.1038/381516a0. [DOI] [PubMed] [Google Scholar]
- 43.Lang PA, Contaldo C, Georgiev P, El-Badry AM, Recher M, Kurrer M, Cervantes-Barragan L, Ludewig B, Calzascia T, Bolinger B, Merkler D, Odermatt B, Bader M, Graf R, Clavien PA, Hegazy AN, Löhning M, Harris NL, Ohashi PS, Hengartner H, Zinkernagel RM, Lang KS. Aggravation of viral hepatitis by platelet-derived serotonin. Nat Med. 2008;14:756–761. doi: 10.1038/nm1780. [DOI] [PubMed] [Google Scholar]
- 44.Nocito A, Dahm F, Jochum W, Jang JH, Georgiev P, Bader M, Renner EL, Clavien PA. Serotonin mediates oxidative stress and mitochondrial toxicity in a murine model of nonalcoholic steatohepatitis. Gastroenterology. 2007;133:608–618. doi: 10.1053/j.gastro.2007.05.019. [DOI] [PubMed] [Google Scholar]
- 45.Chávez E, Castro-Sánchez L, Shibayama M, Tsutsumi V, Pérez Salazar E, Moreno MG, Muriel P. Effects of acetyl salycilic acid and ibuprofen in chronic liver damage induced by CCl4. J Appl Toxicol. 2012;32:51–59. doi: 10.1002/jat.1638. [DOI] [PubMed] [Google Scholar]
- 46.Saito S, Hata K, Iwaisako K, Yanagida A, Takeiri M, Tanaka H, Kageyama S, Hirao H, Ikeda K, Asagiri M, Uemoto S. Cilostazol attenuates hepatic stellate cell activation and protects mice against carbon tetrachloride-induced liver fibrosis. Hepatol Res. 2014;44:460–473. doi: 10.1111/hepr.12140. [DOI] [PubMed] [Google Scholar]
- 47.Watanabe M, Murata S, Hashimoto I, Nakano Y, Ikeda O, Aoyagi Y, Matsuo R, Fukunaga K, Yasue H, Ohkohchi N. Platelets contribute to the reduction of liver fibrosis in mice. J Gastroenterol Hepatol. 2009;24:78–89. doi: 10.1111/j.1440-1746.2008.05497.x. [DOI] [PubMed] [Google Scholar]
- 48.Takahashi K, Murata S, Fukunaga K, Ohkohchi N. Human platelets inhibit liver fibrosis in severe combined immunodeficiency mice. World J Gastroenterol. 2013;19:5250–5260. doi: 10.3748/wjg.v19.i32.5250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sitia G, Iannacone M, Guidotti LG. Anti-platelet therapy in the prevention of hepatitis B virus-associated hepatocellular carcinoma. J Hepatol. 2013;59:1135–1138. doi: 10.1016/j.jhep.2013.05.040. [DOI] [PubMed] [Google Scholar]
- 50.Sitia G, Aiolfi R, Di Lucia P, Mainetti M, Fiocchi A, Mingozzi F, Esposito A, Ruggeri ZM, Chisari FV, Iannacone M, Guidotti LG. Antiplatelet therapy prevents hepatocellular carcinoma and improves survival in a mouse model of chronic hepatitis B. Proc Natl Acad Sci U S A. 2012;109:E2165–E2172. doi: 10.1073/pnas.1209182109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Woolbright BL, Jaeschke H. Novel insight into mechanisms of cholestatic liver injury. World J Gastroenterol. 2012;18:4985–4993. doi: 10.3748/wjg.v18.i36.4985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Chiang JY. Bile acid metabolism and signaling. Compr Physiol. 2013;2013;3:1191–1212. doi: 10.1002/cphy.c120023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Allen K, Jaeschke H, Copple BL. Bile acids induce inflammatory genes in hepatocytes: a novel mechanism of inflammation during obstructive cholestasis. Am J Pathol. 2011;178:175–186. doi: 10.1016/j.ajpath.2010.11.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Tag CG, Sauer-Lehnen S, Weiskirchen S, Borkham-Kamphorst E, Tolba RH, Tacke F, Weiskirchen R. Bile duct ligation in mice: induction of inflammatory liver injury, fibrosis by obstructive cholestasis. J. Vis. Exp. 2015 doi: 10.3791/52438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Popov Y, Patsenker E, Fickert P, Trauner M, Schuppan D. Mdr2 (Abcb4)−/− mice spontaneously develop severe biliary fibrosis via massive dysregulation of pro- and antifibrogenic genes. J Hepatol. 2005;43:1045–1054. doi: 10.1016/j.jhep.2005.06.025. [DOI] [PubMed] [Google Scholar]
- 56.Joshi N, Kopec AK, O’Brien KM, Towery KL, Cline-Fedewa H, Williams KJ, Copple BL, Flick MJ, Luyendyk JP. Coagulation-driven platelet activation reduces cholestatic liver injury and fibrosis in mice. J Thromb Haemost. 2015;13:57–71. doi: 10.1111/jth.12770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Oertelt S, Lian ZX, Cheng CM, Chuang YH, Padgett KA, He XS, Ridgway WM, Ansari AA, Coppel RL, Li MO, Flavell RA, Kronenberg M, Mackay IR, Gershwin ME. Anti-mitochondrial antibodies and primary biliary cirrhosis in TGF-beta receptor II dominant-negative mice. J Immunol. 2006;2006;177:1655–1660. doi: 10.4049/jimmunol.177.3.1655. [DOI] [PubMed] [Google Scholar]
- 58.Woolbright BL, Dorko K, Antoine DJ, Clarke JI, Gholami P, Li F, Kumer SC, Schmitt TM, Forster J, Fan F, Jenkins RE, Park BK, Hagenbuch B, Olyaee M, Jaeschke H. Bile acid-induced necrosis in primary human hepatocytes and in patients with obstructive cholestasis. Toxicol Appl Pharmacol. 2015;283:168–177. doi: 10.1016/j.taap.2015.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Gujral JS, Liu J, Farhood A, Hinson JA, Jaeschke H. Functional importance of ICAM-1 in the mechanism of neutrophil-induced liver injury in bile duct-ligated mice. Am J Physiol Gastrointest Liver Physiol. 2004;286:G499–G507. doi: 10.1152/ajpgi.00318.2003. [DOI] [PubMed] [Google Scholar]
- 60.Moon JO, Welch TP, Gonzalez FJ, Copple BL. Reduced liver fibrosis in hypoxia-inducible factor-1alpha-deficient mice. Am J Physiol Gastrointest Liver Physiol. 2009;296:G582–G592. doi: 10.1152/ajpgi.90368.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Popov Y, Patsenker E, Stickel F, Zaks J, Bhaskar KR, Niedobitek G, Kolb A, Friess H, Schuppan D. Integrin alphavbeta6 is a marker of the progression of biliary and portal liver fibrosis and a novel target for antifibrotic therapies. J Hepatol. 2008;48:453–464. doi: 10.1016/j.jhep.2007.11.021. [DOI] [PubMed] [Google Scholar]
- 62.Plaa GL, Priestly BG. Intrahepatic cholestasis induced by drugs and chemicals. Pharmacol Rev. 1976;1976;28:207–273. [PubMed] [Google Scholar]
- 63.Dietrich CG, Ottenhoff R, de Waart DR, Oude Elferink RP. Role of MRP2 and GSH in intrahepatic cycling of toxins. Toxicology. 2001;2001;167:73–81. doi: 10.1016/s0300-483x(01)00459-0. [DOI] [PubMed] [Google Scholar]
- 64.Orsler DJ, Ahmed-Choudhury J, Chipman JK, Hammond T, Coleman R. ANIT-induced disruption of biliary function in rat hepatocyte couplets. Toxicol Sci. 1999;1999;47:203–210. doi: 10.1093/toxsci/47.2.203. [DOI] [PubMed] [Google Scholar]
- 65.Jean PA, Bailie MB, Roth RA. 1-naphthylisothiocyanate-induced elevation of biliary glutathione. Biochem Pharmacol. 1995;1995;49:197–202. doi: 10.1016/0006-2952(94)00469-2. [DOI] [PubMed] [Google Scholar]
- 66.Dahm LJ, Schultze AE, Roth RA. An antibody to neutrophils attenuates alpha-naphthylisothiocyanate-induced liver injury. J Pharmacol Exp Ther. 1991;1991;256:412–420. [PubMed] [Google Scholar]
- 67.Kodali P, Wu P, Lahiji PA, Brown EJ, Maher JJ. ANIT toxicity toward mouse hepatocytes in vivo is mediated primarily by neutrophils via CD18. Am J Physiol Gastrointest Liver Physiol. 2006;291:G355–G363. doi: 10.1152/ajpgi.00458.2005. [DOI] [PubMed] [Google Scholar]
- 68.Hirschfield GM, Karlsen TH, Lindor KD, Adams DH. Primary sclerosing cholangitis. Lancet. 2013;382:1587–1599. doi: 10.1016/S0140-6736(13)60096-3. [DOI] [PubMed] [Google Scholar]
- 69.Golbar HM, Izawa T, Ichikawa C, Tanaka M, Juniantito V, Sawamoto O, Kuwamura M, Yamate J. Slowly progressive cholangiofibrosis induced in rats by α-naphthylisothiocyanate (ANIT), with particular references to characteristics of macrophages and myofibroblasts. Exp Toxicol Pathol. 2013;65:825–835. doi: 10.1016/j.etp.2012.12.001. [DOI] [PubMed] [Google Scholar]
- 70.Luyendyk JP, Kassel KM, Allen K, Guo GL, Li G, Cantor GH, Copple BL. Fibrinogen deficiency increases liver injury and early growth response-1 (Egr-1) expression in a model of chronic xenobiotic-induced cholestasis. Am J Pathol. 2011;178:1117–1125. doi: 10.1016/j.ajpath.2010.11.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Luyendyk JP, Cantor GH, Kirchhofer D, Mackman N, Copple BL, Wang R. Tissue factor-dependent coagulation contributes to alpha-naphthylisothiocyanate-induced cholestatic liver injury in mice. Am J Physiol Gastrointest Liver Physiol. 2009;296:G840–G849. doi: 10.1152/ajpgi.90639.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Sullivan BP, Weinreb PH, Violette SM, Luyendyk JP. The coagulation system contributes to alphaVbeta6 integrin expression and liver fibrosis induced by cholestasis. Am J Pathol. 2010;177:2837–2849. doi: 10.2353/ajpath.2010.100425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Wang H, Vohra BP, Zhang Y, Heuckeroth RO. Transcriptional profiling after bile duct ligation identifies PAI-1 as a contributor to cholestatic injury in mice. Hepatology. 2005;42:1099–1108. doi: 10.1002/hep.20903. [DOI] [PubMed] [Google Scholar]
- 74.Rautou PE, Tatsumi K, Antoniak S, Owens AP, Sparkenbaugh E, Holle LA, Wolberg AS, Kopec AK, Pawlinski R, Luyendyk JP, Mackman N. Hepatocyte Tissue Factor Contributes to the Hypercoagulable State in a Mouse Model of Chronic Liver Injury. J Hepatol. doi: 10.1016/j.jhep.2015.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Abdel-Salam OM, Baiuomy AR, Ameen A, Hassan NS. A study of unfractionated and low molecular weight heparins in a model of cholestatic liver injury in the rat. Pharmacol Res. 2005;51:59–67. doi: 10.1016/j.phrs.2004.04.009. [DOI] [PubMed] [Google Scholar]
- 76.Fiorucci S, Antonelli E, Distrutti E, Severino B, Fiorentina R, Baldoni M, Caliendo G, Santagada V, Morelli A, Cirino G. PAR1 antagonism protects against experimental liver fibrosis. Role of proteinase receptors in stellate cell activation. Hepatology. 2004;39:365–375. doi: 10.1002/hep.20054. [DOI] [PubMed] [Google Scholar]
- 77.Joshi N, Kopec AK, Towery K, Williams KJ, Luyendyk JP. The antifibrinolytic drug tranexamic acid reduces liver injury and fibrosis in a mouse model of chronic bile duct injury. J Pharmacol Exp Ther. 2014;349:383–392. doi: 10.1124/jpet.113.210880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bergheim I, Guo L, Davis MA, Duveau I, Arteel GE. Critical role of plasminogen activator inhibitor-1 in cholestatic liver injury and fibrosis. J Pharmacol Exp Ther. 2006;316:592–600. doi: 10.1124/jpet.105.095042. [DOI] [PubMed] [Google Scholar]
- 79.Wang H, Zhang Y, Heuckeroth RO. Tissue-type plasminogen activator deficiency exacerbates cholestatic liver injury in mice. Hepatology. 2007;45:1527–1537. doi: 10.1002/hep.21613. [DOI] [PubMed] [Google Scholar]
- 80.Wang H, Zhang Y, Heuckeroth RO. PAI-1 deficiency reduces liver fibrosis after bile duct ligation in mice through activation of tPA. FEBS Lett. 2007;581:3098–3104. doi: 10.1016/j.febslet.2007.05.049. [DOI] [PubMed] [Google Scholar]
- 81.Kodama T, Takehara T, Hikita H, Shimizu S, Li W, Miyagi T, Hosui A, Tatsumi T, Ishida H, Tadokoro S, Ido A, Tsubouchi H, Hayashi N. Thrombocytopenia exacerbates cholestasis-induced liver fibrosis in mice. Gastroenterology. 2010;138:2487–2498. doi: 10.1053/j.gastro.2010.02.054. 98.e1-7. [DOI] [PubMed] [Google Scholar]
- 82.Lazo M, Hernaez R, Eberhardt MS, Bonekamp S, Kamel I, Guallar E, Koteish A, Brancati FL, Clark JM. Prevalence of nonalcoholic fatty liver disease in the United States: the Third National Health and Nutrition Examination Survey, 1988-1994. Am J Epidemiol. 2013;178:38–45. doi: 10.1093/aje/kws448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Welsh JA, Karpen S, Vos MB. Increasing prevalence of nonalcoholic fatty liver disease among United States adolescents, 1988-1994 to 2007-2010. J Pediatr. 2013;162:496–500. doi: 10.1016/j.jpeds.2012.08.043. e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Tripodi A, Fracanzani AL, Primignani M, Chantarangkul V, Clerici M, Mannucci PM, Peyvandi F, Bertelli C, Valenti L, Fargion S. Procoagulant imbalance in patients with non-alcoholic fatty liver disease. J Hepatol. 2014;61:148–154. doi: 10.1016/j.jhep.2014.03.013. [DOI] [PubMed] [Google Scholar]
- 85.Verrijken A, Francque S, Mertens I, Prawitt J, Caron S, Hubens G, Van Marck E, Staels B, Michielsen P, Van Gaal L. Prothrombotic factors in histologically proven nonalcoholic fatty liver disease and nonalcoholic steatohepatitis. Hepatology. 2014;59:121–129. doi: 10.1002/hep.26510. [DOI] [PubMed] [Google Scholar]
- 86.Bell LN, Theodorakis JL, Vuppalanchi R, Saxena R, Bemis KG, Wang M, Chalasani N. Serum proteomics and biomarker discovery across the spectrum of nonalcoholic fatty liver disease. Hepatology. 2010;51:111–120. doi: 10.1002/hep.23271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Northup PG, Argo CK, Shah N, Caldwell SH. Hypercoagulation and thrombophilia in nonalcoholic fatty liver disease: mechanisms, human evidence, therapeutic implications, and preventive implications. Semin Liver Dis. 2012;32:39–48. doi: 10.1055/s-0032-1306425. [DOI] [PubMed] [Google Scholar]
- 88.Takahashi Y, Soejima Y, Fukusato T. Animal models of nonalcoholic fatty liver disease/nonalcoholic steatohepatitis. World J Gastroenterol. 2012;18:2300–2308. doi: 10.3748/wjg.v18.i19.2300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Kohli R, Kirby M, Xanthakos SA, Softic S, Feldstein AE, Saxena V, Tang PH, Miles L, Miles MV, Balistreri WF, Woods SC, Seeley RJ. High-fructose, medium chain trans fat diet induces liver fibrosis and elevates plasma coenzyme Q9 in a novel murine model of obesity and nonalcoholic steatohepatitis. Hepatology. 2010;52:934–944. doi: 10.1002/hep.23797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Owens AP, Passam FH, Antoniak S, Marshall SM, McDaniel AL, Rudel L, Williams JC, Hubbard BK, Dutton JA, Wang J, Tobias PS, Curtiss LK, Daugherty A, Kirchhofer D, Luyendyk JP, Moriarty PM, Nagarajan S, Furie BC, Furie B, Johns DG, Temel RE, Mackman N. Monocyte tissue factor-dependent activation of coagulation in hypercholesterolemic mice and monkeys is inhibited by simvastatin. J Clin Invest. 2012;122:558–568. doi: 10.1172/JCI58969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Kassel KM, Owens AP, Rockwell CE, Sullivan BP, Wang R, Tawfik O, Li G, Guo GL, Mackman N, Luyendyk JP. Protease-activated receptor 1 and hematopoietic cell tissue factor are required for hepatic steatosis in mice fed a Western diet. Am J Pathol. 2011;179:2278–2289. doi: 10.1016/j.ajpath.2011.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Kopec AK, Joshi N, Towery KL, Kassel KM, Sullivan BP, Flick MJ, Luyendyk JP. Thrombin inhibition with dabigatran protects against high-fat diet-induced fatty liver disease in mice. J Pharmacol Exp Ther. 2014;351:288–297. doi: 10.1124/jpet.114.218545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Kassel KM, Sullivan BP, Cui W, Copple BL, Luyendyk JP. Therapeutic administration of the direct thrombin inhibitor argatroban reduces hepatic inflammation in mice with established fatty liver disease. Am J Pathol. 2012;181:1287–1295. doi: 10.1016/j.ajpath.2012.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Luyendyk JP, Sullivan BP, Guo GL, Wang R. Tissue factor-deficiency and protease activated receptor-1-deficiency reduce inflammation elicited by diet-induced steatohepatitis in mice. Am J Pathol. 2010;176:177–186. doi: 10.2353/ajpath.2010.090672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Badeanlou L, Furlan-Freguia C, Yang G, Ruf W, Samad F. Tissue factor-protease-activated receptor 2 signaling promotes diet-induced obesity and adipose inflammation. Nat Med. 2011;17:1490–1497. doi: 10.1038/nm.2461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Anstee QM, Dhar A, Thursz MR. The role of hypercoagulability in liver fibrogenesis. Clin Res Hepatol Gastroenterol. 2011;35:526–533. doi: 10.1016/j.clinre.2011.03.011. [DOI] [PubMed] [Google Scholar]
- 97.Wright M, Goldin R, Hellier S, Knapp S, Frodsham A, Hennig B, Hill A, Apple R, Cheng S, Thomas H, Thursz M. Factor V Leiden polymorphism and the rate of fibrosis development in chronic hepatitis C virus infection. Gut. 2003;52:1206–1210. doi: 10.1136/gut.52.8.1206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Poujol-Robert A, Boëlle PY, Conti F, Durand F, Duvoux C, Wendum D, Paradis V, Mackiewicz V, Chazouillères O, Corpechot C, Poupon R. Aspirin may reduce liver fibrosis progression: Evidence from a multicenter retrospective study of recurrent hepatitis C after liver transplantation. Clin Res Hepatol Gastroenterol. 2014;38:570–576. doi: 10.1016/j.clinre.2014.07.004. [DOI] [PubMed] [Google Scholar]
- 99.Yoshida S, Ikenaga N, Liu SB, Peng ZW, Chung J, Sverdlov DY, Miyamoto M, Kim YO, Ogawa S, Arch RH, Schuppan D, Popov Y. Extrahepatic platelet-derived growth factor-β, delivered by platelets, promotes activation of hepatic stellate cells and biliary fibrosis in mice. Gastroenterology. 2014;147:1378–1392. doi: 10.1053/j.gastro.2014.08.038. [DOI] [PubMed] [Google Scholar]
- 100.Hugenholtz GC, Northup PG, Porte RJ, Lisman T. Is there a rationale for treatment of chronic liver disease with antithrombotic therapy? Blood Rev. 2015;29 doi: 10.1016/j.blre.2014.10.002. [DOI] [PubMed] [Google Scholar]