Abstract
Background and Purpose
Following transient ischemic attack (TIA), there is increased risk for ischemic stroke. The American Heart Association recommends admission of patients with ABCD2 scores ≥3 for observation, rapid performance of diagnostic tests, and potential acute intervention. We aimed to determine if there is a relationship between ABCD2 scores, in-hospital ischemic events, and in-hospital treatments after TIA admission.
Methods
We reviewed consecutive patients admitted between 2006 and 2011 following a TIA, defined as transient focal neurological symptoms attributed to a specific vascular distribution and lasting <24 h. Three interventions were prespecified: anticoagulation for atrial fibrillation, carotid or intracranial revascularization, and intravenous or intra-arterial reperfusion therapies. We compared rates of in-hospital recurrent TIA or ischemic stroke and the receipt of interventions among patients with low (<3) versus high (≥3) ABCD2 scores.
Results
Of 249 patients, 11 patients (4.4%) had recurrent TIAs or strokes during their stay (8 TIAs, 3 strokes). All 11 had ABCD2 scores ≥3, and no neurological events occurred in patients with lower scores (5.1 vs. 0%; p = 0.37). Twelve patients (4.8%) underwent revascularization for large artery stenosis, 16 (6.4%) were started on anticoagulants, and no patient received intravenous or intra-arterial reperfusion therapy. The ABCD2 score was not associated with anticoagulation (p = 0.59) or revascularization (p = 0.20).
Conclusions
Higher ABCD2 scores may predict early ischemic events after TIA but do not predict the need for intervention. Outpatient evaluation for those with scores <3 would potentially have delayed revascularization or anticoagulant treatment in nearly one-fifth of ‘low-risk’ patients.
Key Words: Transient ischemic attack, Acute stroke
Background and Purpose
Transient ischemic attack (TIA) is associated with increased risk for subsequent stroke. The initial 48 h following TIA are especially of high risk, with estimates of stroke incidence ranging from 1.4 to 9.9% [1]. A prospective population-based study of stroke following TIA further quantified the 6-, 12-, and 24-hour risks of stroke following TIA as 1.2, 2.1, and 5.1%, respectively [2]. In patients who had a stroke within 30 days of their first TIA, about half of the strokes occurred within the first 48 h [3,4], emphasizing the importance of early triage decision-making. Multiple tools have been used to help assess and stratify a patient's risk for subsequent stroke, including the ABCD2 score, diffusion-weighted imaging (DWI), and neurovascular imaging [5]. The ABCD2 score can be quickly calculated and inform emergency department (ED) decision-making. Although validation studies of the ABCD2 score have produced inconsistent results relating to its predictive value, it remains the simplest and most commonly used tool to evaluate TIA patients in the ED [5,6,7,8]. Currently, the American Heart Association/American Stroke Association (AHA/ASA) guidelines state that it is reasonable to admit patients presenting within 72 h of symptom onset who have an ABCD2 score ≥3, as they may be at higher risk for impending stroke; these guidelines also allow for consideration of admission of patients with lower scores and signs of focal ischemia or the inability to have workup completed in an expedited manner [9]. Those with scores <3 may be at lower stroke risk and could alternately be evaluated rapidly with improved cost-effectiveness in outpatient clinics [10,11]. However, the role of the ABCD2 score in predicting the need for acute interventions, such as revascularization and anticoagulation, is less established [12]. Some investigators have found that patients with low scores have an equal risk of subsequent stroke [13]. In particular, ABCD2 scores may not accurately predict clinically significant carotid stenosis [14]. Therefore, we investigated whether the ABCD2 score predicted in-hospital events and interventions including recurrent ischemia, thrombolysis, carotid and intracranial revascularization procedures, and initiation of anticoagulation for atrial fibrillation. Our objective was to determine if the ABCD2 score was an effective way to triage patients presenting to the ED with symptoms concerning for TIA based on the occurrence of in-hospital deterioration, the subsequent occurrence of management changes, or the need for in-hospital interventions.
Methods
Patients
This cross-sectional retrospective study was performed with approval from the institutional research board. All patients hospitalized at our institution, a teaching hospital which was a primary stroke center at the time of this study, with a diagnosis of TIA between August 2006 and March 2011 were prospectively entered into a registry and included in this study; data collection was done by the study authors. TIA was defined as transient focal neurological symptoms attributed to a specific vascular distribution and lasting less than 24 h [15]. All patients suspected of having TIA within the ED are first evaluated by an emergency physician and subsequently by a neurology resident, and are admitted to the stroke inpatient service while undergoing diagnostic workup. All TIAs were diagnosed by vascular board-certified neurologists, and all patients discharged with a diagnosis of TIA were captured by our registry. Patients who were initially admitted with possible TIA or stroke but not discharged with either diagnosis were systematically excluded from the registry. A CT of the brain was obtained for all patients at the time of admission, and advanced imaging (such as MRI) was obtained for patients without contraindications. Although a newer definition of TIA incorporates MRI findings and classifies restricted diffusion lesions as representing a stroke instead of a TIA, for the purpose of our study, patients with DWI lesions but resolution of symptoms within 24 h were considered TIAs. Additional diagnostic evaluations were at the discretion of the admitting physician, but typically included vascular imaging of the cervical carotid arteries, a transthoracic echocardiogram, telemetry, and additional Holter monitoring. Demographics, type and duration of clinical symptoms, initial National Institutes of Health Stroke Scale (NIHSS) score, medical comorbidities, in-hospital treatments including initiation of intravenous or intra-arterial thrombolysis, large artery revascularization, and anticoagulation were collected. Results of carotid ultrasounds, CT angiogram of the neck, and MR angiogram of the neck were reviewed to determine if there was a >50% stenosis on the symptomatic side. An ABCD2 score was calculated for each patient by the primary study physician based on clinical data available in the patient's chart [7]. Patients initially admitted for possible TIA but later determined to have an alternate diagnosis were excluded from our study.
Events
The primary outcome measure was in-hospital ischemic events, defined as a return of previously resolved symptoms or new focal neurological symptoms. Patients were considered to have had an ischemic stroke if follow-up MRI or CT confirmed new areas of ischemia not previously present, with persistent clinical symptoms lasting >24 h and to have recurrent TIA if symptoms lasted ≤24 h. Secondary outcome measures included all in-hospital intervention as detailed below. In-hospital use of intravenous tissue plasminogen activator and/or endovascular reperfusion therapy (i.e. intra-arterial lytic or mechanical embolectomy) was ascertained. Revascularization of symptomatic arterial stenosis was defined as either endarterectomy or angioplasty/stenting of an extracranial internal carotid artery or angioplasty/stenting of an intracranial artery. Anticoagulation was defined as initiation of intravenous or oral anticoagulation during hospitalization or at discharge (i.e. heparin, warfarin, or novel anticoagulants). In-hospital intervention plus in-hospital ischemic events were combined to form a composite risk in order to more fully understand events following the index symptoms.
Statistical Analysis
Patients' ABCD2 scores were dichotomized into low risk and high risk. Low risk was defined as having a score <3 and high risk as having a score ≥3. χ2 or Fisher's exact tests were used to examine the relationship between demographics, clinical features, DWI positivity, and ABCD2 category on (1) the occurrence of in-hospital recurrent TIA or stroke and (2) in-hospital treatments. A p value ≤0.05 was considered significant in all analyses. Data analysis was performed using SPSS 16.0 (Chicago, Ill., USA).
Results
Two hundred and 49 patients were admitted for TIA during the study period; 45% were male, with a mean age of 64 years (range 18-97), and 47% were Caucasian. The mean length of stay was 2.6 days (median 2), and most patients (94%) were discharged home. The length of time between symptom onset and presentation to the ED was <12 h for 146 patients (59%), <24 h for 45 patients (18%), <48 h for 18 patients (7%), and >48 h (n = 15, 6%) or unknown (n = 30, 12%) for the remaining patients. The majority of patients had hypertension (73%) and hyperlipidemia (50%). Mean systolic and diastolic blood pressure at presentation was 145 and 79 mm Hg, respectively. The median ABCD2 score was 4; 216 patients (86.7%) were considered high-risk (scores ≥3). Symptomatic carotid stenosis >50% was present in 16 patients (8%, out of 201 available studies). Table 1 summarizes patient demographics and clinical characteristics overall and between groups. The ABCD2 score, in-hospital ischemic events, and in-hospital intervention data were available for all patients.
Table 1.
Demographic, medical, and clinical characteristics of the cohort
| Total number (n = 249) | Low ABCD2 score (n = 33) | High ABCD2 score (n = 216) | |
|---|---|---|---|
| Demographics | |||
| Age, years | 63.9 ± 14.4 | 58.3 ± 13.5 | 64.7 ± 14.4 |
| Male | 111 (45) | 12 (36) | 99 (46) |
| Caucasian | 118 (47) | 20 (61) | 98 (45) |
| African-American | 104 (42) | 10 (30) | 94 (44) |
| Hispanic | 21 (8) | 3 (9) | 18 (8) |
| Asian | 6 (2) | 0 | 6 (3) |
| Medical comorbidities | |||
| Hypertension | 183 (73) | 21 (63) | 162 (75) |
| High cholesterol | 125 (50) | 13 (39) | 112 (52) |
| Atrial fibrillation | 21 (9) | 1 (3) | 20 (9) |
| CAD | 57 (23) | 8 (24) | 49 (23) |
| Current smoker | 58 (23) | 7 (21) | 51 (24) |
| Prior TIA | 38 (15) | 5 (15) | 33 (15) |
| Prior stroke | 54 (22) | 8 (24) | 46 (21) |
| Diabetes | 71 (29) | 4 (12) | 67 (31) |
| Hospitalization characteristics | |||
| Initial systolic BP in the ED, mm Hg | 146 ± 29 | 134 ± 37 | 147 ± 27 |
| Initial diastolic BP in the ED, mm Hg | 79 ± 17 | 75 ± 18 | 79 ± 16 |
| Motor symptoms | 145 (58) | 3 (9) | 142 (66) |
| Speech disturbances | 128 (51) | 9 (27) | 119 (55) |
| Duration of episode | (n = 208) | (n = 28) | (n = 180) |
| <10 min | 35 (17) | 14 (50) | 21 (12) |
| 10–59 min | 72 (35) | 8 (29) | 64 (36) |
| >59 min, <24 h | 101 (49) | 6 (21) | 95 (53) |
| Single episode at presentation | 212 (85) | 28 (85) | 184 (85) |
| DWI MRI | (n = 211) | (n = 27) | (n = 184) |
| Abnormal | 61 (29) | 5 (19) | 56 (30) |
| Length of stay, days | |||
| Mean ± SD | 2.6 ± 3.2 | 2.7 ± 3.6 | 2.6 ± 3.1 |
| Median (IQR) | 2 (2) | 2 (2) | 2 (2) |
| Discharge disposition | |||
| Home or left AMA | 233 (94) | 31 (94) | 202 (94) |
| Inpatient rehabilitation | 11 (4) | 2 (6) | 9 (4) |
| Long-term acute care | 3 (1) | 0 | 3 (1) |
| Transfer to another hospital | 1 | 0 | 1 |
| Expired | 1 | 0 | 1 |
| Symptomatic carotid stenosis >50% | 15 (6) | 2 (6) | 13 (6) |
Data are given as n (%) or mean ± SD, unless otherwise indicated. CAD = Coronary artery disease; BP = blood pressure; IQR = interquartile range; AMA = against medical advice.
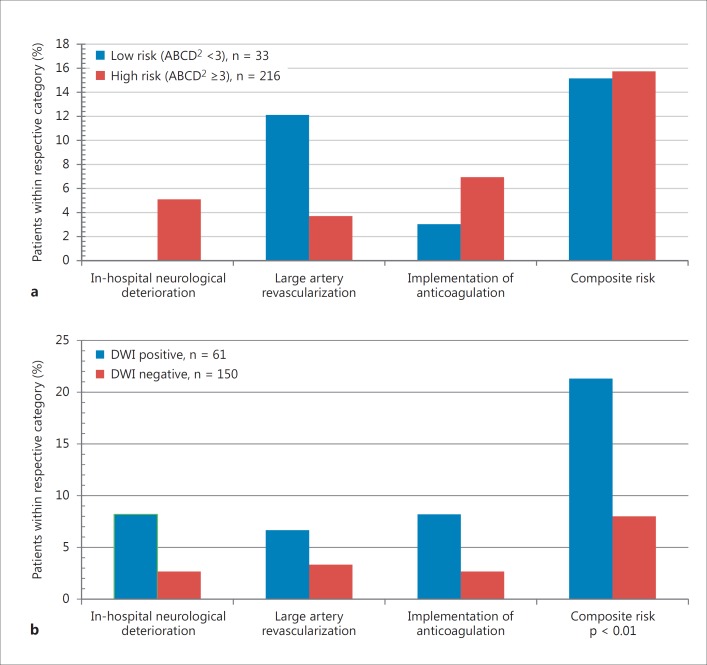
Eleven patients had in-hospital ischemic events: 8 TIAs and 3 ischemic strokes. All patients with recurrent events had ABCD2 scores ≥3, while none of the patients with lower scores had in-hospital ischemic events during their stay (5.1 vs. 0%, p = 0.37; fig. 1a). All 11 patients with in-hospital ischemic events had hospital stays >48 h, and all of the events occurred after the initial 48 h. No patient with recurrent symptoms received intravenous or endovascular reperfusion therapy due to contraindications (recent stroke, low NIHSS score at time of deterioration) or elapsed time window. Two of the 3 ischemic strokes were cryptogenic, while the third was cardioembolic in a patient with a persistently subtherapeutic international normalized ratio and decompensation due to a congestive heart failure exacerbation. On review, no clear change in management could have prevented the first two events. None of the patients with an in-hospital ischemic event had >50% carotid stenosis, although 4 patients had ipsilateral intracranial atherosclerosis.
Fig. 1.
a Findings dichotomized by ABCD2 category. b Findings dichotomized by DWI status.
A total of 12 patients (4.8%) underwent inpatient revascularization for large artery stenosis (3 intracranial, 9 extracranial); none were in the group with recurrent ischemic events while hospitalized. The median time to surgery was 3 days after symptom onset. Nine of the 12 patients (75%) had stenosis that was >70%. There was no difference in the rate of revascularization among patients with low versus high ABCD2 scores (9.1 vs. 4.2%, p = 0.20; fig. 1a). Anticoagulation was initiated in 16 patients (6.4%) and was similar by ABCD2 score groups (p = 0.59). Two patients were started on anticoagulation for arrhythmias seen while in the ED, 1 for atrial fibrillation seen on Holter monitoring, and 5 based on the results of echocardiograms. When combining recurrent ischemic events, revascularization, and initiation of anticoagulation, the ABCD2 score did not predict the composite risk (the high ABCD2 score was 20.4%, versus the low ABCD2 score of 21.2%; p = 0.91).
Two hundred and 11 patients (85%) underwent an MRI, of whom 61 had at least 1 DWI lesion present that correlated to their symptoms. ABCD2 score groups were not associated with DWI findings; 30% of patients with ABCD2 scores ≥3 had DWI lesions compared to 19% of those with low ABCD2 scores (p = 0.26). A positive finding on DWI was not correlated with the likelihood of in-hospital deterioration (p = 0.31), anticoagulation (p = 0.12), or the need for revascularization (p = 0.13); however, it was associated with an increased risk of the composite of revascularization, recurrent TIA or stroke, or initiation of anticoagulation (p < 0.01; fig. 1b).
Discussion
In our study, nearly one-fifth of presumed low-risk TIA patients (ABCD2 <3) underwent in-hospital large artery revascularization or initiation of anticoagulation. While only those with ABCD2 scores ≥3 had in-hospital recurrent ischemic events, justifying the current recommendation for hospitalization, our findings suggest that patients with ABCD2 scores <3 may harbor high-risk stroke conditions that require urgent in-hospital management. This includes arrhythmias that may have previously been undetected.
Although the AHA guidelines support the use of the ABCD2 score, the score's ability to triage TIA patients for admission is questioned. This topic was of renewed interest as of late, with a meta-analysis showing that the ABCD2 score does not reliably discriminate between those at low and high risk of early recurrent stroke [14]. Perhaps supplementing this score with the addition of vascular and brain imaging results is preferred, as several studies have noted improved discrimination between different risk groups by doing so [6,15,16,17,18,19]. Indeed, net reclassification into low- and high-risk groups when including vessel and brain imaging approaches one-third of patients compared to the simpler ABCD2 score [20]. Symptom fluctuation and prior TIA within 7 days of index TIA, in combination with the ABCD2 score, may also be valid predictors of early stroke risk [16,21]. Finally, a new prognostic score has recently been described, which may be more accurate in determining high- and low-risk patients [22]. Whether obtaining expedited testing using rapid MRI and telemetry is a feasible option remains to be seen, as one recent paper found that TIA patients had better outcomes when hospitalized in stroke units compared to elsewhere [23], and another suggested that those patients with minor stroke or TIA who are discharged from the ED are less likely to receive timely stroke care interventions [24]. Of note, expedited evaluation in an outpatient clinic or a clinic with 24-hour access may ameliorate this effect [24,25].
Only 2 prior studies have evaluated the relationship between the ABCD2 score and in-hospital intervention, observing that patients with a lower score have a similar probability of requiring in-hospital treatment as those with higher scores [12,13]. Our study expands on these findings by observing that in the 85% of patients who underwent MRI, the presence of DWI lesions strongly correlated with subsequent recurrent TIA or stroke, in-hospital revascularization, or initiation of anticoagulant therapy. An imaging-based triage strategy may therefore be more useful than the ABCD2 score for determining composite risks of stroke and the need for in-hospital risk-modifying treatments.
Our study does have several limitations. First, it was conducted at a single urban tertiary care center, which limits the ability to generalize these findings more broadly. Second, our sample size was small, especially with regard to event rates of recurrent events or revascularization. This likely limited the power to detect small but meaningful differences between groups. Third, we did not systematically perform radiographic assessment after in-hospital deterioration, leading to possible diagnostic misclassification of outcome. In addition, index TIA with normal DWI results may have been misdiagnosed (i.e. migraine) despite expert neurovascular evaluation. Fourth, as we focused solely on deterioration during the initial hospital stay, data were not collected at 7, 30, and 90 days. Lastly, based on the small number of patients admitted with low ABCD2 scores, it is also possible that patients were not recognized as TIA and discharged from the ED without evaluation by the stroke team. Similarly, patients admitted with possible TIA and later given an alternative diagnosis were not captured. This would limit the number of subsequent events captured in that subset of patients. However, the number of patients with ABCD2 scores <3 in our study is similar to that in other cohort studies, mollifying these concerns [7]. In addition, it is the practice of the neurologists at this institution to admit all patients with TIA, regardless of the ABCD2 score, limiting the number of patients lost following an index event.
Conclusions
Our findings suggest that all TIA patients should be considered for hospitalization on the basis of a heightened risk of early ischemic events and rapid access to risk-modifying treatments such as revascularization and anticoagulation. Advanced imaging showing restricted diffusion suggests a higher risk for both in-hospital deterioration and a potential need for in-hospital intervention. Triage based on the ABCD2 score alone may delay revascularization or anticoagulation in nearly 20% of patients.
Disclosure Statement
All authors declare no potential conflicts of interest.
Acknowledgement
This study was conducted with funding from the Department of Neurology at Rush University Medical Center.
References
- 1.Shah KH, Kleckner K, Edlow JA. Short-term prognosis of stroke among patients diagnosed in the emergency department with a transient ischemic attack. Ann Emerg Med. 2008;51:316–323. doi: 10.1016/j.annemergmed.2007.08.016. [DOI] [PubMed] [Google Scholar]
- 2.Chandratheva A, Mehta Z, Geraghty OC, Marquardt L, Rothwell PM. Population-based study of risk and predictors of stroke in the first few hours after a TIA. Neurology. 2009;72:1941–1947. doi: 10.1212/WNL.0b013e3181a826ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Johnston SC, Gress DR, Browner WS, Sidney S. Short-term prognosis after emergency department diagnosis of TIA. JAMA. 2000;284:2901–2906. doi: 10.1001/jama.284.22.2901. [DOI] [PubMed] [Google Scholar]
- 4.Lisabeth LD, Ireland JK, Risser JM, et al. Stroke risk after transient ischemic attack in a population-based setting. Stroke. 2004;35:1842–1846. doi: 10.1161/01.STR.0000134416.89389.9d. [DOI] [PubMed] [Google Scholar]
- 5.Tsivgoulis G, Stamboulis E, Sharma VK, et al. Multicenter external validation of the ABCD2 score in triaging TIA patients. Neurology. 2010;74:1351–1357. doi: 10.1212/WNL.0b013e3181dad63e. [DOI] [PubMed] [Google Scholar]
- 6.Perry JJ, Sharma M, Sivilotti ML, et al. Prospective validation of the ABCD2 score for patients in the emergency department with transient ischemic attack. CMAJ. 2011;183:1137–1145. doi: 10.1503/cmaj.101668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Johnston SC, Rothwell PM, Nguyen-Huynh MN, et al. Validation and refinement of scores to predict very early stroke risk after transient ischaemic attack. Lancet. 2007;369:283–292. doi: 10.1016/S0140-6736(07)60150-0. [DOI] [PubMed] [Google Scholar]
- 8.Chandratheva A, Geraghty OC, Luengo-Fernandez R, Rothwell PM. ABCD2 score predicts severity rather than risk of early recurrent events after transient ischemic attack. Stroke. 2010;41:851–856. doi: 10.1161/STROKEAHA.109.570010. [DOI] [PubMed] [Google Scholar]
- 9.Easton JD, Saver JL, Albers GW, et al. Definition and evaluation of transient ischemic attack: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association Stroke Council; Council on Cardiovascular Surgery and Anesthesia; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular Nursing; and the Interdisciplinary Council on Peripheral Vascular Disease. The American Academy of Neurology affirms the value of this statement as an educational tool for neurologists. Stroke. 2009;40:2276–2293. doi: 10.1161/STROKEAHA.108.192218. [DOI] [PubMed] [Google Scholar]
- 10.Martinez-Martinez MM, Martinez-Sanchez P, Fuentes B, et al. Transient ischaemic attacks clinics provide equivalent and more efficient care than early in-hospital assessment. Eur J Neurol. 2013;20:338–343. doi: 10.1111/j.1468-1331.2012.03858.x. [DOI] [PubMed] [Google Scholar]
- 11.Joshi JK, Ouyang B, Prabhakaran S. Should TIA patients be hospitalized or referred to a same-day clinic? A decision analysis. Neurology. 2011;77:2082–2088. doi: 10.1212/WNL.0b013e31823d763f. [DOI] [PubMed] [Google Scholar]
- 12.Lou M, Safdar A, Edlow JA, et al. Can ABCD score predict the need for in-hospital intervention in patients with transient ischemic attacks? Int J Emerg Med. 2010;3:75–80. doi: 10.1007/s12245-010-0176-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Amarenco P, Labreuche J, Lavallée PC. Patients with transient ischemic attack with ABCD2 <4 can have similar 90-day stroke risk as patients with transient ischemic attack with ABCD2 ≥4. Stroke. 2012;43:863–865. doi: 10.1161/STROKEAHA.111.636506. [DOI] [PubMed] [Google Scholar]
- 14.Wardlaw JM, Brazzelli M, Chappell FM, et al. ABCD2 score and secondary stroke prevention: meta-analysis and effect per 1,000 patients triaged. Neurology. 2015;85:373–380. doi: 10.1212/WNL.0000000000001780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Merwick A, Albers GW, Amarenco P, et al. Addition of brain and carotid imaging to the ABCD(2) score to identify patients at early risk of stroke after transient ischaemic attack: a multicentre observational study. Lancet Neurol. 2010;9:1060–1069. doi: 10.1016/S1474-4422(10)70240-4. [DOI] [PubMed] [Google Scholar]
- 16.Calvet D, Touze E, Oppenheim C, Turc G, Meder JF, Mas JL. DWI lesions and TIA etiology improve the prediction of stroke after TIA. Stroke. 2009;40:187–192. doi: 10.1161/STROKEAHA.108.515817. [DOI] [PubMed] [Google Scholar]
- 17.Ay H, Arsava EM, Johnston SC, et al. Clinical- and imaging-based prediction of stroke risk after transient ischemic attack: the CIP model. Stroke. 2009;40:181–186. doi: 10.1161/STROKEAHA.108.521476. [DOI] [PubMed] [Google Scholar]
- 18.Engelter ST, Amort M, Jax F, et al. Optimizing the risk estimation after a transient ischaemic attack - the ABCDE plus sign in circle score. Eur J Neurol. 2012;19:55–61. doi: 10.1111/j.1468-1331.2011.03428.x. [DOI] [PubMed] [Google Scholar]
- 19.Fujinami J, Uehara T, Kimura K, et al. Incidence and predictors of ischemic stroke events during hospitalization in patients with transient ischemic attack. Cerebrovasc Dis. 2014;37:330–335. doi: 10.1159/000360757. [DOI] [PubMed] [Google Scholar]
- 20.Kiyohara T, Kamouchi M, Kumai Y, et al. ABCD3 and ABCD3-I scores are superior to ABCD2 score in the prediction of short- and long-term risks of stroke after transient ischemic attack. Stroke. 2014;45:418–425. doi: 10.1161/STROKEAHA.113.003077. [DOI] [PubMed] [Google Scholar]
- 21.Chatzikonstantinou A, Wolf ME, Schaefer A, Hennerici MG. Risk prediction of subsequent early stroke in patients with transient ischemic attacks. Cerebrovasc Dis. 2013;36:106–109. doi: 10.1159/000352060. [DOI] [PubMed] [Google Scholar]
- 22.Arsava EM, Kim GM, Oliveira-Filho J, et al. Prediction of early recurrence after acute ischemic stroke. JAMA Neurol. 2016;73:396–401. doi: 10.1001/jamaneurol.2015.4949. [DOI] [PubMed] [Google Scholar]
- 23.Cadilhac DA, Kim J, lannin NA, et al. Better outcomes for hospitalized patients with TIA when in stroke units. Neurology. 2016;86:2042–2048. doi: 10.1212/WNL.0000000000002715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kapral MK, Hall R, Fang J, et al. Association between hospitalization and care after transient ischemic attack or minor stroke. Neurology. 2016;86:1582–1589. doi: 10.1212/WNL.0000000000002614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lavallee PC, Mesequer E, Abboud H, et al. A transient ischaemic attack clinic with round-the-clock access (SOS-TIA): feasibility and effects. Lancet Neurol. 2007;6:953–960. doi: 10.1016/S1474-4422(07)70248-X. [DOI] [PubMed] [Google Scholar]