Abstract
Retinal ischemia-reperfusion (I/R) is a pathophysiological process contributing to cellular damage in multiple ocular conditions, including glaucoma, diabetic retinopathy, and retinal vascular occlusions. Rodent models of I/R injury are providing significant insights into mechanisms and treatment strategies for human I/R injury, especially with regard to neurodegenerative damage in the retinal neurovascular unit. Presented here is a protocol for inducing retinal I/R injury in mice through elevation of intraocular pressure (IOP). In this protocol, the ocular anterior chamber is cannulated with a needle, through which flows the drip of an elevated saline reservoir. Using this drip to raise IOP above systolic arterial blood pressure, a practitioner temporarily halts inner retinal blood flow (ischemia). When circulation is reinstated (reperfusion) by removal of the cannula, severe cellular damage ensues, resulting ultimately in retinal neurodegeneration. Recent studies demonstrate inflammation, vascular permeability, and capillary degeneration as additional elements of this model. Compared to alternative retinal I/R methodologies, such as retinal arterial ligation, retinal I/R injury by elevated IOP offers advantages in its anatomical specificity, experimental tractability, and technical accessibility, presenting itself as a valuable tool for examining neuronal pathogenesis and therapy in the retinal neurovascular unit.
Keywords: Medicine, Issue 113, Retina, ischemia, reperfusion, intraocular pressure, neuron, neurodegeneration, neurovascular unit
Introduction
Retinal ischemia-reperfusion (I/R) characterizes many human retinal pathologies, including glaucoma, diabetic retinopathy, and retinal vascular occlusions1. In retinal I/R, reduced blood flow (ischemia) in the retinal vasculature creates a state of retinal hypersensitivity to oxygen and other nutrients, precipitating severe oxidative and inflammatory damage when circulation is subsequently reinstated (reperfusion)2. The neural retina appears particularly vulnerable to these changes, with retinal neurodegeneration being perhaps the most salient feature of I/R-induced damage. Presented here is a protocol for modeling retinal I/R injury in the mouse. This technique enables researchers to examine potential mechanisms and treatment strategies for human diseases of the retinal neurovascular unit.
Pioneered in 1952 by surgeons seeking to understand the neurodegenerative consequences of surgical anemia3, rodent retinal I/R by elevated intraocular pressure (IOP) was reestablished in 1991 for the purpose of standardizing neurodegenerative endpoints after ischemic insult4. Using the drip of a saline reservoir to raise IOP above systolic blood pressure, these studies demonstrated that pressurized ocular cannulation was sufficient to suspend the retinal circulation and thereby initiate neuronal degeneration. More recent efforts using retinal I/R by elevated IOP have begun to elaborate the mechanisms underlying I/R-induced retinal neurodegeneration5-12. Multiple groups have reported additional pathologic changes including inflammation13,14, vascular permeability15,16, and capillary degeneration14,17. Taken together, these studies have established retinal I/R injury by elevated IOP as a model of retinal neurovascular disease more generally.
Characterizing the mechanisms of I/R injury is essential for the study of vascular disease. Retinal I/R injury by elevated IOP is one of many hypoxia-induced injury models, including I/R injuries in lung18, heart19, brain20, liver21, kidney22, and intestine23. These models have been paramount in advancing our understanding of vascular illness and its clinical remedies. By extending the investigation of I/R processes to ocular tissues, retinal I/R injury by elevated IOP helps to paint a more comprehensive picture of these related conditions.
Corresponding closely with clinical neurodegenerative conditions in retina, retinal I/R injury by elevated IOP presents a valuable tool for researchers interested in exploring ischemic pathogenesis. The protocol described herein is targeted, tractable, and accessible. It is complemented well by endpoints in neuronal degeneration, such as quantification of retinal neurons, measurement of retinal thickness, and electrophysiological recording of retinal neuron function. This model has proven its utility in advancing neurovascular inquiry, and it shows promise in earning status as a foundational protocol in visual medicine research.
Protocol
Ethics Statement: All procedures were performed in accordance with the guidelines set forth by the Johns Hopkins University Institutional Animal Care and Use Committee.
Note: Mice used during filming are C57BL/6 mice from Jackson, although other rodent strains or species may also be used. When using other strains or species, be aware that anesthesia dosages and injury timeline may vary. It is important to adapt I/R conditions to accommodate strain, species, and experimental variations.
1. Prepare the Anesthesia Cocktail
Combine 1.25 ml Ketamine, 0.625 ml Xylazine, 0.375 ml Acepromazine, and 22.75 ml phosphate buffered saline in a 50 ml centrifuge tube. NOTE: For the remainder of the manuscript, this solution will be referred to as the cocktail.
Filter the cocktail into a new sterile 50 ml centrifuge tube using a 60 ml syringe and a 0.20 µm filter. Label and date this new tube.
Fully wrap the cocktail tube in aluminum foil to prevent light-induced degradation of the anesthetic. NOTE: The cocktail may be stored at room temperature and reused until the expiration date of its earliest-expiring ingredient.
2. Prepare the Anesthesia Booster
In a 50 ml centrifuge tube, combine 4 ml Ketamine and 16 ml phosphate buffered saline. NOTE: This solution will henceforth be referred to as the booster.
Filter the booster into a new sterile 50 ml centrifuge tube using a 60 ml syringe and a 0.20 µm filter. Label and date this new tube. NOTE: The booster may be stored at room temperature and reused until the expiration date of its earliest-expiring ingredient.
3. Prepare the Surgical Suite
Set the room temperature between 18 °C and 21 °C.
Turn on the surgery table, and adjust its surface heat to the highest temperature.
Cover all work surfaces with surgical underpads.
Arrange an empty cage or other container on the surgical table to warm.
Arrange a scale and an ear tagger on the worktop.
4. Prepare the Balanced Salt Solution with Heparin Sodium
Add 0.5 ml of heparin sodium to a 500 ml IV bottle of balanced salt solution (HBSS).
Insert the sharp end of the primary set prepierced Y-site tubing into the bottle of 0.1% heparin sodium.
5. Set up the IV Pole
Hang the bottle of 0.1% heparin sodium from the IV pole extension, and snap open the air filter cap on the primary set prepierced Y-site tubing.
Elevate the 0.1% heparin sodium bottle to 163 cm (120 mm Hg). Measure the height from the tabletop to the peak of the sodium heparin drip.
Remove any air bubbles in the IV tubing by manually flicking the primary set prepierced Y-site tubing.
6. Set up the Sodium Heparin Drip
Connect the primary set prepierced Y-site tubing to the five-valve manifold.
Connect 30-gauge ½ inch needles to the five-port manifold using Luer male to Luer male tube fittings.
Insert each of the 30-gauge ½ inch needles into its own 10-inch segment of 30-gauge tubing.
Using hemostats, break the needle tips from new 30-gauge ½ inch needles and insert their blunt ends into the 30-gauge tubing. Sterility or disinfection of the needle tips will be necessary for Step 8.3.
Using tape, arrange the 30-gauge tubes with needles such that the tubes connected to the inner ports are positioned on top of the tubes connected to the outer ports. This arrangement will prevent tangling of tubing during anterior chamber cannulation.
- Turn on the 0.1% heparin sodium flow to the five-valve manifold and to each individual port.
- Ensure that the 0.1% heparin sodium is flowing strongly for each port. If a port is flowing weakly, replace the port or clear it with air from a sterile syringe.
- Allow the 0.1% heparin sodium to flow for 2 - 3 min to remove air bubbles from the 30-gauge tubes and 5-valve manifold.
Turn off all the ports on the 5-valve manifold.
7. Prepare the Mice for Surgery
Bring the mice to the surgical suite. Supply water bottles for each cage in order to prevent animal dehydration during surgery.
Record the weight of each mouse.
Inject each mouse intraperitoneally with 0.02 ml cocktail per gram bodyweight.
Tag and record the number of each mouse.
Place all the mice into the empty container on the surgery table. Allow 5-10 min for all the mice to achieve deep anesthetization as confirmed by absence of the pedal withdrawal response to toe pinch.
For each mouse, administer one drop of Tropicamide into each eye for pupil dilation and short-term lubrication.
For each mouse, administer one drop of Proparacaine into each eye for local anesthesia and short-term lubrication.
Arrange the mice in the order of anesthetization so that the first mouse to be anesthetized will be the first mouse to be cannulated.
Allow approximately 2 min for the eye drops to take effect.
Prepare straight 4-inch pieces of tape by pulling tightly on the tape. Set aside one piece of tape for each mouse. NOTE: Failing to pull tightly on the tape will result in curling of the tape.
8. Cannulate the Anterior Chamber
Arrange the first mouse under the surgical microscope, and focus the microscope on the preferred cornea. NOTE: Cannulation may be performed on either eye. Right-hand dominant surgeons may find it easiest to cannulate the left eye, while left-hand dominant surgeons may prefer the right.
Turn on the first 0.1% heparin sodium port on the five-valve manifold.
- Under the surgical microscope, use a pair of forceps to gently proptose the eye. Insert the 30-gauge cannula needle into the anterior chamber approximately halfway between the zonule fibers and the apex of the cornea.
- Take care to avoid scratching or puncturing the iris, lens, or inner corneal surface.
- Avoid penetrating the cornea a second time.
- Using a gentle twisting motion to overcome friction between the cannula and the cornea, insert the cannula deeply in the anterior chamber.
Use a strip of tape to secure the 30-gauge tubing to the table. To minimize movement of the inserted cannula, press the 30-gauge tubing against the tabletop while reaching for the tape.
Record the start time of the surgery.
Using the microscope, verify that no leakage is apparent. If leakage is present, the movement of fluid will be visible near the eye.
Visually confirm ocular distention by observing that the I/R eye is larger than the contralateral eye. Together, the absence of leakage and the presence of ocular distention demonstrate a successful elevation of intraocular pressure.
Apply hypromellose to both eyes. Hypromellose serves to lubricate the cornea and seal microleaks. Reapply hypromellose as needed (approximately every 30 min) for sustained lubrication.
Repeat Step 8 until all animals have been cannulated.
9. Monitor Anesthesia
Use the toe pinch, visual observation of the whiskers, or visual observation of the tail to verify that each mouse remains anesthetized. Should a mouse demonstrate a pedal withdrawal response, whisker twitching, or tail movement, proceed immediately to Step 9.2.
If a mouse begins to awaken during surgery, lift the tail to inject 0.05 ml booster intraperitoneally into the lower abdomen from behind the mouse. Allow 1 - 2 min for the booster to take effect.
Should a mouse require additional sedation, repeat Step 9 as necessary.
10. Remove the Cannula from the Anterior Chamber
For each animal, after 90 min have elapsed, gently pull the cannula from the anterior chamber.
Untape the mouse from the surgical table, taking care not to disturb the cannula tubing of adjacent animals.
Lubricate both eyes with lubricating jelly.
As subsequent cannulae are removed, arrange the mice in the empty container on the surgical table to recover from surgery. Do not turn off the heat of the surgical table.
Allow, at minimum, 2 - 3 hr for recovery on the heated surgical table. Observe the mice frequently until they have fully recovered from the anesthesia.
11. Clean the Equipment
Disinfect the cannulae using alcohol wipes. NOTE: Other methods for disinfection or sterilization, such as autoclaving, may be substituted.
Expel 0.1% heparin sodium from the 5-valve manifold, 30-gauge needles, 30-gauge tubing, and cannulae using a 60 ml syringe filled with air.
Rinse the 5-valve manifold, 30-gauge needles, 30-gauge tubing, and cannulae using a 60 ml syringe filled with distilled water.
Expel distilled water from the 5-port manifold, 30-gauge needles, 30-gauge tubing, and cannulae using a 60 ml syringe filled with air.
After disinfecting the cannulae and rinsing the tubing apparatus, store this equipment for reuse.
Store, discard, or turn off all other equipment. Leave the heat of the surgical table on.
12. Return All Mice to Their Home Cages
After the mice awaken from surgery (after 2 - 3 hr), return each animal to its home cage. Provide gel food for each cage. Return all cages to their designated rooms.
Turn off the heat of the surgical table. Discard all waste, and wipe down the surgical suite.
13. Perform Retinal Assessment
As appropriate, collect retinas for histological analysis or dark adapt mice for electroretinogram recording.
Representative Results
The neurodegenerative effects of retinal I/R by elevated IOP are commonly evaluated using two standard approaches. NeuN immunolabeling of neuronal nuclei has revealed significant neuronal cell loss following I/R insult (Figure 1). Briefly, eyes enucleated 7 days after I/R were fixed in paraformaldehyde, labeled with the neuronal cell marker NeuN, and whole-mounted. Images were captured using confocal microscopy, and cells labeled with NeuN were quantified by counting11. Decreases in ganglion cell layer neuron counts indicate I/R-induced cell death.
Impairments in retinal neuron function have been documented using electroretinography (Figure 2). Briefly, seven days after I/R, scotopic electroretinograms were recorded at multiple flash intensities. Amplitudes of the a- and b-waves were quantified using image analysis software12. Here, lower a- and b-wave amplitudes signify I/R-induced impairments in retinal neuronal function. In these and other I/R endpoints, the non-I/R eye serves as a robust negative control for I/R-induced damage.
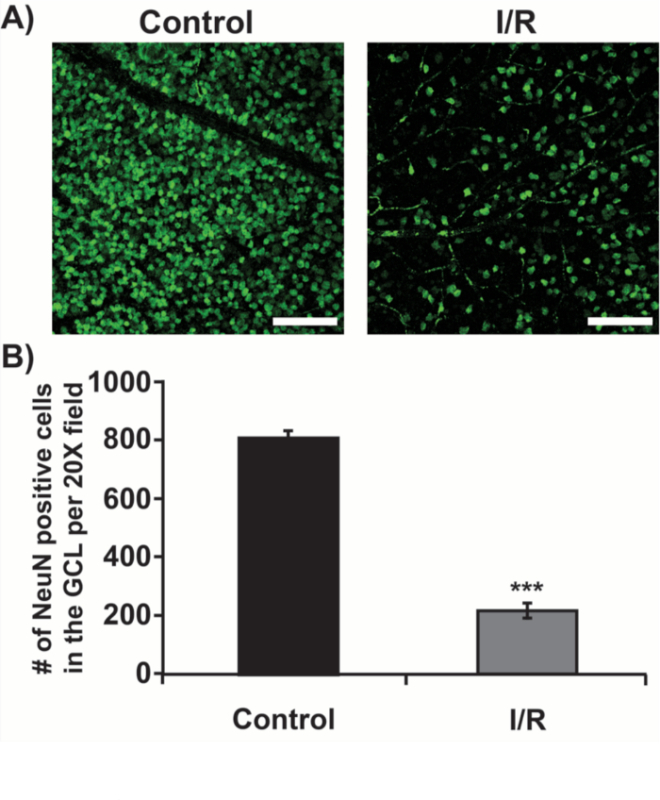 Figure 1.Retinal I/R Induces Neuronal Cell Death in the Ganglion Cell Layer (GCL). Representative retinal images from control and I/R eyes are shown with scale bars denoting 100 µm. (A) The number of NeuN-positive cells in the GCL is significantly reduced in I/R eyes as compared to controls (B). n = 9, error bar: standard error, ***p < 0.0001 Please click here to view a larger version of this figure.
Figure 1.Retinal I/R Induces Neuronal Cell Death in the Ganglion Cell Layer (GCL). Representative retinal images from control and I/R eyes are shown with scale bars denoting 100 µm. (A) The number of NeuN-positive cells in the GCL is significantly reduced in I/R eyes as compared to controls (B). n = 9, error bar: standard error, ***p < 0.0001 Please click here to view a larger version of this figure.
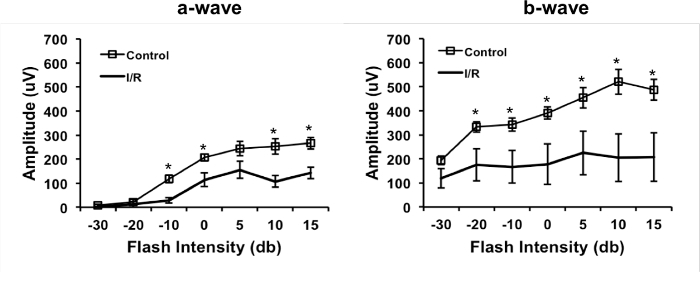 Figure 2.Retinal I/R Impairs Retinal Neuron Function. Decreased a- and b-wave amplitudes indicate impaired membrane physiology in neuronal cells following I/R. n = 6, error bar: standard error, *p < 0.05 Please click here to view a larger version of this figure.
Figure 2.Retinal I/R Impairs Retinal Neuron Function. Decreased a- and b-wave amplitudes indicate impaired membrane physiology in neuronal cells following I/R. n = 6, error bar: standard error, *p < 0.05 Please click here to view a larger version of this figure.
Discussion
Retinal I/R injury by elevated IOP has proven its utility in modeling cellular damage and dysfunction, particularly neurodegeneration, in the rodent retinal neurovascular unit. This procedure provides a robust control tissue and is easily accessible in terms of technical sophistication. It has been noted in this and other I/R injury models that increasing the pressure and duration of ischemia may increase injury severity24. For this reason, some practitioners have elected to use ischemic pressures and durations differing from those presented here4,6-10,12. Therefore retinal I/R injury by elevated IOP offers an advantage over alternative retinal I/R techniques in that it allows one to adjust surgical parameters to accommodate one's particular experimental goals.
Nonetheless, alternative techniques have been employed for inducing retinal I/R injury in rodents. Ligation of the optic nerve bundle25,26 or the central retinal artery alone27 has been used to arrest retinal blood flow temporarily. Similar strategies for systemic conditions have required ligation of the cerebral artery28 or the cephalic artery29 to reduce blood flow without fully obstructing it. One rarer methodology involves circumferentially compressing the retinal globe using a thread that is weighted on both ends30. While such strategies have successfully contributed to an understanding of hypoxia-induced neurovascular changes in the retina, the technique described herein offers several advantages over these alternatives. Necessitating minimal non-retinal damage only to the cornea, I/R by elevated IOP provides a more specifically targeted retinal injury than is afforded by ligation techniques and so may be more useful for researchers interested in retina-specific disease. Also, elevated IOP methods are more tractable than ligation or compression models, such that the IOP method allows quick attainment of retinal ischemia as well as subsequent reperfusion. Finally, elevated IOP protocols require minimal surgical and technological sophistication and so may be more widely accessible than their alternatives.
Retinal I/R injury by elevated IOP is not without its challenges. Cannulation of the anterior chamber requires manual dexterity, and care must be taken to preserve the integrity of the iris, lens, and cornea. Caution is also advised after insertion of the cannula, as the cannula may be pulled from the anterior chamber while the 30-gauge tubing is secured with tape.
Other critical processes in this protocol include maintaining a warm body temperature for anesthetized animals, administering booster anesthesia in a timely manner, and sustaining lubrication of the cornea using hypromellose. It is also important to note mouse stress or sickness behaviors (for example, lack of grooming, hunching, etc.) prior to surgery, as these extra-surgical variables may influence drug potency and mortality. By attending to these issues, one may achieve a highly regulated and reproducible model for retinal I/R injury.
It should also be acknowledged that retinal I/R injury by elevated IOP is only a model, and caution is advised when extrapolating findings to specific diseases, particularly chronic conditions. While differing from these diseases in time frame and etiological origin, however, retinal I/R injury by elevated IOP may nonetheless provide a sound platform for evaluating mechanisms of retinal degeneration and recovery.
The retina is composed of multiform cells and signaling processes, and a comprehensive story of retinal dysregulation remains to be elucidated. The current literature demonstrates the utility of retinal I/R injury by elevated IOP not only in examining retinal degenerative processes6-8,10,12, but also in identifying targets for therapeutic prevention and intervention7,9,11,12,14. In addition, there is growing evidence to support the utility of retinal I/R injury by elevated IOP in non-neuronal endpoints such as retinal inflammation, vascular degeneration, and leakage14,15,17. Given its anatomical specificity, experimental tractability, and technical accessibility, retinal I/R injury by elevated IOP promises to maintain a leading role in pursuing these inquiries.
Disclosures
The authors have no disclosures.
Acknowledgments
This work was supported by research grants from the National Institutes of Health (EY022383 and EY022683; EJD) and Core grant (P30EY001765), Imaging and Microscopy Core Module.
References
- Osborne NN, et al. Retinal ischemia: mechanisms of damage and potential therapeutic strategies. Prog Retin Eye Res. 2004;23(1):91–147. doi: 10.1016/j.preteyeres.2003.12.001. [DOI] [PubMed] [Google Scholar]
- Bonne C, Muller A, Villain M. Free radicals in retinal ischemia. Gen Pharmacol. 1998;30(3):275–280. doi: 10.1016/s0306-3623(97)00357-1. [DOI] [PubMed] [Google Scholar]
- Smith GG, Baird CD. Survival time of retinal cells when deprived of their blood supply by increased intraocular pressure. Am J Ophthalmol. 1952;35(5:2):133–136. doi: 10.1016/0002-9394(52)90266-3. [DOI] [PubMed] [Google Scholar]
- Buchi ER, Suivaizdis I, Fu J. Pressure-induced retinal ischemia in rats: an experimental model for quantitative study. Ophthalmologica. 1991;203(3):138–147. doi: 10.1159/000310240. [DOI] [PubMed] [Google Scholar]
- Block F, Schwarz M. The b-wave of the electroretinogram as an index of retinal ischemia. Gen Pharmacol. 1998;30(3):281–287. doi: 10.1016/s0306-3623(97)00359-5. [DOI] [PubMed] [Google Scholar]
- Katai N, Yoshimura N. Apoptotic retinal neuronal death by ischemia-reperfusion is executed by two distinct caspase family proteases. Invest Ophthalmol Vis Sci. 1999;40(11):2697–2705. [PubMed] [Google Scholar]
- Toriu N, et al. Lomerizine, a Ca2+ channel blocker, reduces glutamate-induced neurotoxicity and ischemia/reperfusion damage in rat retina. Exp Eye Res. 2000;70(4):475–484. doi: 10.1006/exer.1999.0809. [DOI] [PubMed] [Google Scholar]
- Kawai SI, et al. Modeling of risk factors for the degeneration of retinal ganglion cells after ischemia/reperfusion in rats: effects of age, caloric restriction, diabetes, pigmentation, and glaucoma. FASEB J. 2001;15(7):1285–1287. doi: 10.1096/fj.00-0666fje. [DOI] [PubMed] [Google Scholar]
- Chidlow G, Schmidt KG, Wood JP, Melena J, Osborne NN. Alpha-lipoic acid protects the retina against ischemia-reperfusion. Neuropharmacology. 2002;43(6):1015–1025. doi: 10.1016/s0028-3908(02)00129-6. [DOI] [PubMed] [Google Scholar]
- Fei F, et al. Upregulation of Homer1a Promoted Retinal Ganglion Cell Survival After Retinal Ischemia and Reperfusion via Interacting with Erk Pathway. Cell Mol Neurobiol. 2015. [DOI] [PMC free article] [PubMed]
- Xu Z, et al. Neuroprotective role of Nrf2 for retinal ganglion cells in ischemia-reperfusion. J Neurochem. 2015;133(2):233–241. doi: 10.1111/jnc.13064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim BJ, Braun TA, Wordinger RJ, Clark AF. Progressive morphological changes and impaired retinal function associated with temporal regulation of gene expression after retinal ischemia/reperfusion injury in mice. Mol Neurodegener. 2013;8(21) doi: 10.1186/1750-1326-8-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Portillo JA, et al. CD40 mediates retinal inflammation and neurovascular degeneration. J Immunol. 2008;181(12):8719–8726. doi: 10.4049/jimmunol.181.12.8719. [DOI] [PubMed] [Google Scholar]
- Wei Y, et al. Nrf2 has a protective role against neuronal and capillary degeneration in retinal ischemia-reperfusion injury. Free Radic Biol Med. 2011;51(1):216–224. doi: 10.1016/j.freeradbiomed.2011.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abcouwer SF, et al. Effects of ischemic preconditioning and bevacizumab on apoptosis and vascular permeability following retinal ischemia-reperfusion injury. Invest Ophthalmol Vis Sci. 2010;51(11):5920–5933. doi: 10.1167/iovs.10-5264. [DOI] [PubMed] [Google Scholar]
- Abcouwer SF, et al. Minocycline prevents retinal inflammation and vascular permeability following ischemia-reperfusion injury. J Neuroinflammation. 2013;10(149) doi: 10.1186/1742-2094-10-149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng L, Gong B, Hatala DA, Kern TS. Retinal ischemia and reperfusion causes capillary degeneration: similarities to diabetes. Invest Ophthalmol Vis Sci. 2007;48(1):361–367. doi: 10.1167/iovs.06-0510. [DOI] [PubMed] [Google Scholar]
- Weyker PD, Webb CA, Kiamanesh D, Flynn BC. Lung ischemia reperfusion injury: a bench-to-bedside review. Semin Cardiothorac Vasc Anesth. 2013;17(1):28–43. doi: 10.1177/1089253212458329. [DOI] [PubMed] [Google Scholar]
- Raedschelders K, Ansley DM, Chen DD. The cellular and molecular origin of reactive oxygen species generation during myocardial ischemia and reperfusion. Pharmacol Ther. 2012;133(2):230–255. doi: 10.1016/j.pharmthera.2011.11.004. [DOI] [PubMed] [Google Scholar]
- Di Y, et al. MicroRNAs expression and function in cerebral ischemia reperfusion injury. J Mol Neurosci. 2014;53(2):242–250. doi: 10.1007/s12031-014-0293-8. [DOI] [PubMed] [Google Scholar]
- Saidi RF, Kenari SK. Liver ischemia/reperfusion injury: an overview. J Invest Surg. 2014;27(6):366–379. doi: 10.3109/08941939.2014.932473. [DOI] [PubMed] [Google Scholar]
- Malek M, Nematbakhsh M. Renal ischemia/reperfusion injury; from pathophysiology to treatment. J Renal Inj Prev. 2015;4(2):20–27. doi: 10.12861/jrip.2015.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mallick IH, Yang W, Winslet MC, Seifalian AM. Ischemia-reperfusion injury of the intestine and protective strategies against injury. Dig Dis Sci. 2004;49(9):1359–1377. doi: 10.1023/b:ddas.0000042232.98927.91. [DOI] [PubMed] [Google Scholar]
- Hesketh EE, et al. Renal ischaemia reperfusion injury: a mouse model of injury and regeneration. J Vis Exp. 2014. [DOI] [PMC free article] [PubMed]
- Stefansson E, Wilson CA, Schoen T, Kuwabara T. Experimental ischemia induces cell mitosis in the adult rat retina. Invest Ophthalmol Vis Sci. 1988;29(7):1050–1055. [PubMed] [Google Scholar]
- Honjo M, et al. Statin inhibits leukocyte-endothelial interaction and prevents neuronal death induced by ischemia-reperfusion injury in the rat retina. Arch Ophthalmol. 2002;120(12):1707–1713. doi: 10.1001/archopht.120.12.1707. [DOI] [PubMed] [Google Scholar]
- Otori Y, et al. Expression of c-fos and c-jun mRNA following transient retinal ischemia: an approach using ligation of the retinal central artery in the rat. Surv Ophthalmol. 1997;42:96–104. doi: 10.1016/s0039-6257(97)80032-x. Suppl 1. [DOI] [PubMed] [Google Scholar]
- Liu J, et al. Epac2-deficiency leads to more severe retinal swelling, glial reactivity and oxidative stress in transient middle cerebral artery occlusion induced ischemic retinopathy. Sci China Life Sci. 2015;58(6):521–530. doi: 10.1007/s11427-015-4860-1. [DOI] [PubMed] [Google Scholar]
- Zhang Y, Zhang Z, Yan H. Simvastatin inhibits ischemia/reperfusion injury-induced apoptosis of retinal cells via downregulation of the tumor necrosis factor-alpha/nuclear factor-kappaB pathway. Int J Mol Med. 2015. [DOI] [PMC free article] [PubMed]
- Li B, Pang IH, Barnes G, McLaughlin M, Holt W. A new method and device to induce transient retinal ischemia in the rat. Curr Eye Res. 2002;24(6):458–464. doi: 10.1076/ceyr.24.6.458.8596. [DOI] [PubMed] [Google Scholar]


