Abstract
Aerosol or inhalational studies of high-consequence pathogens have recently been increasing in number due to the perceived threat of intentional aerosol releases or unexpected natural aerosol transmission. Specific laboratories designed to perform these experiments require tremendous engineering controls to provide a safe and secure working environment and constant systems maintenance to sustain functionality. Class III biosafety cabinets, also referred to as gloveboxes, are gas-tight enclosures with non-opening windows. These cabinets are maintained under negative pressure by double high-efficiency-particulate-air (HEPA)-filtered exhaust systems and are the ideal primary containment for housing aerosolization equipment. A well planned workflow between staff members within high containment from, for instance, an animal biosafety level-4 (ABSL-4) suit laboratory to the ABSL-4 cabinet laboratory is a crucial component for successful experimentation. For smooth study execution, establishing a communication network, moving equipment and subjects, and setting up and placing equipment, requires staff members to meticulously plan procedures prior to study initiation. Here, we provide an overview and a visual representation of how aerobiology research is conducted at the National Institutes of Health, National Institute of Allergy and Infectious Diseases Integrated Research Facility at Fort Detrick, Maryland, USA, within an ABSL-4 environment.
Keywords: Infection, Issue 116, ABSL4, ABSL-4, aerobiology, biosafety, BSL4, BSL-4, biosafety level 4 cabinet laboratory, biosafety level 4 suit laboratory, biosecurity, Class III biosafety cabinet, Class III BSC, high containment, maximum containment, personal protective equipment, positive pressure suit, PPE, basic protocol
Introduction
Transmission of viruses generally occurs by direct or physical contact, but many important viral diseases (e.g., measles, chickenpox, influenza) are caused by pathogens that are transmitted by aerosol or respiratory droplets. Such pathogens have the potential to cause a pandemic with consequences ranging from widespread mild disease associated with loss of work (e.g., common cold) to rarer serious disease with high lethality (e.g., smallpox). High-consequence pathogens that spread naturally by aerosol or by intentional aerosol release (biological weapons) are of particular interest to aerobiology1. Humans may become rapidly infected with some of these pathogens by large respiratory droplets or small-particle nuclei and easily spread these pathogens to others through salivary secretions, coughing, and sneezing2. In the US biodefense community, high-consequence pathogens (e.g., filoviruses or other NIAID Category A-C Priority Pathogens and CDC Bioterrorism Agents) are the focus of aerosol research programs due to high lethality of associated infections3,4. Significant scientific strides within the aerobiology field have been made within the past decade due to technological advances in aerosol equipment and high containment facilities5,6. Research at the National Institutes of Health, National Institute of Allergy and Infectious Diseases (NIH/NIAID), Integrated Research Facility at Fort Detrick located in Frederick, MD, USA (IRF-Frederick) focuses on high-consequence emerging pathogens that require animal biosafety level 4 (ABSL-4) containment. The overall mission of the IRF-Frederick is to evaluate and facilitate the development of candidate vaccines and therapeutics (medical countermeasures).
Research with high-consequence pathogens at the IRF-Frederick is governed by stringent biosafety and animal care and use requirements. These requirements are outlined in the Biosafety in Microbiological and Biomedical Laboratories (BMBL) manual7 and the federal animal welfare regulations. These necessary requirements may restrict the type of research that can be performed and impact overall study design. As we previously described in this journal, all research conducted in an ABSL-4 environment requires particular caution, highly specialized training, and a robust and redundant facility infrastructure8,9.
Entry into the IRF-Frederick ABSL-4 suit laboratory requires donning a positive-pressure encapsulating suit8. Positive-pressure encapsulating suits are not required for entering the ABSL-4 cabinet laboratory. Donning a scrub suit, rubber or nitrile gloves, and close-toed shoes is appropriate when manipulating Risk Group 4 infectious material within a certified Class III biosafety Cabinet (BSC) in an ABSL-4 cabinet laboratory7.
At the IRF-Frederick, aerosol equipment is engineered, assembled, and maintained in two hermetically sealed, stainless steel, air-tight, negative-pressure Class III BSCs, Figure 1. The IRF-Frederick Aerobiology Core employs an automated aerosol management Platform (AAMP) to control and monitor aerosol experimentation within these BSCs, Figure 2. A previous publication outlined the specific functions of the Class III BSCs at the IRF-Frederick and the connection to the suit laboratory via a pass-through port5. The procedure of preparing the Class III BSC prior to experimentation is specific to the IRF. Other Class III BSCs used at other institutions function similarly to the Class III BSC in use at the IRF, but may have different mechanisms for transport, access, or docking.
To further understand how high-consequence pathogens remain infectious and spread through aerosol transmission, safe aerobiological experimentation must be conducted in these Class III BSCs according to a specific workflow procedure. Researchers have been carefully and thoroughly trained to ensure this workflow is followed in a safe and consistent manner. Prior to nonhuman primate (NHP) aerosol challenge, several aerosol characterization or sham aerosol runs are performed to test the stability and viability of an agent when in aerosol form. The aerosol characterization process mimics the actual aerosol challenge, and the researcher evaluates the variables associated with aerosol studies.
Another part of the workflow is to record physical manipulations, administration or anesthetics or other agents, or routine procedures on charts for each NHP. These subject charts are analyzed thoroughly to ensure procedural consistency and standardization. Subjects are anesthetized prior to aerosol exposure. Example anesthetics include tiletamine/zolazepam, ketamine/acepromazine, and ketamine. Anesthetics are chosen based on minimizing respiratory suppression and promotion of controlled, steady-state breathing. Additional anesthesia supplies are maintained in the animal procedure rooms and transported on the transfer cart with the NHP to the aerobiology ABSL-4 cabinet laboratory.
Within the ABSL-4 suit laboratory, NHPs undergo plethysmography via one of two methods (i.e., head-out plethysmography, respiratory inductive plethysmography [RIP]) to determine inspiratory tidal volume and breathing rate changes10-12. These derived parameters are used for accurate calculation of the estimated inhaled dose of the pathogen immediately prior to or during an aerosol exposure. Head-out plethysmography uses a long, cylindrical chamber that houses the NHP13. The pressure drop created when an animal is in the cylinder is captured by a pneumotachograph, relayed to the amplifier, processed by the alternating current/direct current converter, and integrated into the software to derive the above pulmonary parameters. RIP uses sensors made of inductive coiled copper wires that are embedded in elastic bands around the subject's chest and abdomen11,12. An inductive-capacitor generates a magnetic field in the sensor. Breathing changes the magnetic field, and the resulting voltage changes are relayed from a transmitter next to the elastic band to a receiver in the computer via short-wavelength ultra-high frequency radio waves. Dedicated software determines breathing rate and tidal volume from total thoracic displacement.
The minute volume (MV) obtained through plethysmography is used in the calculation of the estimated inhaled dose (D). In generating and sampling an aerosol, the aerosol concentration (AC) is calculated by multiplying the biosampler concentration (BC) by the volume of media (V) and dividing by result of multiplying the flow rate of the biosampler (FL) by the exposure time (T). The simplified formula is represented as AC = BC x V ÷ FL x T. In turn, for the actual aerosol challenge in NHPs, D is calculated by multiplying AC by MV and the exposure duration (time = T). The simplified formula is represented as D = AC x MV x T.
The purpose of this article is to visually demonstrate the entire aerosol challenge procedure using NHPs from two viewpoints, the ABSL-4 suit laboratory side and the ABSL-4 cabinet laboratory side. Although these procedures may be general in nature for several practices mentioned, they are specific to the IRF-Frederick Aerobiology Core and represent the actual practices used at this institution. This article focuses on the biosafety procedures needed to safely perform an aerosol challenge, not the actual aerosol challenge itself. In these procedures, we are using a dummy subject to show biosafety practices, due to the risk associated with anesthetizing an NHP. However, the process of performing an aerosol challenge is written in a general way because the procedure is the same regardless of high-consequence pathogen used. We aim to enhance knowledge and understanding of scientists about the rigors of conducting aerosol studies of high consequence pathogens under maximum containment conditions.
Protocol
This protocol adheres to the following animal care guidelines. Animals were housed in a facility accredited by the Association for Assessment and Accreditation of Laboratory Animal Care International. All experimental procedures were approved by the National Institute of Allergy and Infectious Diseases, Division of Clinical Research, Animal Care and Use Committee and were in compliance with the Animal Welfare Act regulations, Public Health Service policy, and the Guide for the Care and Use of Laboratory Animals recommendations.
1. Aerobiology: Animal Biosafety Level 4 (ABSL-4) Suit Laboratory
- Laboratory Preparation
- Complete the ABSL-4 suit laboratory entry procedures (outlined in detail in 8).
- Test the functionality of all equipment (e.g., plethysmography equipment, laptop, biohazardous trash cans, biohazardous sharps containers, subject monitoring devices) involved in aerobiology procedures occurring within the ABSL-4 suit laboratory according to manufacturer's protocol.
- Ensure the transfer cart is biologically clean prior to testing the functionality of the rapid transfer port (RTP), which connects the transport cart through the wall to the Class III BSC).
- Handle and dilute pathogen only within certified BSCs. Prepare the pathogen in the appropriate formulation within a Class II BSC that contains appropriate disinfectants. Transport the pathogen in an air-tight secondary container labeled with a biohazard symbol on wet ice in the transport cart. Pass the pathogen through the RTP into the Class III BSC in the ABSL-4 cabinet laboratory, Figure 1.
2. Plethysmography: Animal Biosafety Level 4 (ABSL-4) Suit Laboratory
- Plethysmography Setup and Calibration
- Determine which method of plethysmography acquisition (head-out plethysmography or respiratory inductance plethysmography [RIP]) will be used and connect equipment components together.
- Calibrate the plethysmograph prior to the experiment using manufacturer's protocol.
- Plethysmography Acquisition
- When handling NHPs, don an external pair of latex or nitrile gloves over top of the suit gloves to prevent cross contamination and promote safe practices. When finished handling NHPs, remove these extra gloves and discard in the biohazardous trash can within the room.
- If using head-out plethysmography, attach a new rubber/dental dam to the front of the cylinder. Cut a small hole in the dam for the head of the NHP to fit through the top of the cylinder. When seated, the dam creates a seal around the NHP's neck.
- If using RIP, check that the RIP bands are properly fitted around the chest and abdomen of the NHP and the electronic connections are snapped tightly.
- Send all data acquired from the plethysmography procedure to the researchers in the ABSL-4 cabinet laboratory. Export the tidal volume and minute volume data for each animal through a compatible program for use during the aerosol process.
3. Nonhuman Primate Transport and Handling: Animal Biosafety Level 4 Suit Laboratory
- NHP Handling
- Monitor and record any physical manipulations, administrations, or routine procedures on charts for each NHP.
- When an aerosol challenge is completed, place the NHP inside the transportation container and return NHP to the home cage located in the animal holding room.
- When handling a live animal, follow the mandatory rule that requires 2 staff members to be present.
- NHP Transport
- Determine the type of anesthesia, duration of anesthesia (covers transport, plethysmography acquisition, and aerosol challenge) and corresponding dose of anesthesia prior to administration. Fully anesthetize the NHP based on the process chosen by the Comparative Medicine staff. If additional anesthesia is required, ensure all needles, sharps, syringes, and caps are discarded in a sharps container located in any of the animal procedure rooms. Do not recap any needles after use.
- Transport anesthetized NHPs in clear containers that are secured by a latch on the lid of the transport box.
- Load transport containers onto a mobile cart to allow fully suited researchers to move freely using breathing air lines and through the air pressure resistant (APR) doors, Figure 1.
- As no additional breathing air for the NHP is supplied to the transport container, minimize transport time.
4. Aerobiology: ABSL-4 Cabinet Laboratory
- Class III BSC Setup
- Concurrently with animal preparation performed by Comparative Medicine staff, prepare the Class III BSC. Visually verify that negative pressure in the Class III BSC is maintained within specified range (125 Pa or -0.5 in water gauge (wg) minimum; 250 Pa or -1.0 in wg recommended). Inspect the Class III BSC for any potential leaks or cracks (see Figure 1).
- Physically and visually inspect the Class III BSC synthetic rubber gloves and O-rings attached to the Class III BSC for weak spots, tears, rips, or dry rot. Replace the damaged Class III synthetic rubber gloves and/or O-rings immediately prior to use. At this point, the Class III BSC is not contaminated.
- If a leak occurs while the Class III BSC is contaminated, identify the location of the breach and alert facility management and biosafety personnel. If a Class III BSC integrated glove is torn or breached, replace the damaged glove immediately by following the properly trained technique and internal Class III BSC standard operating procedure.
- To change an integrated glove containing a small tear or breach during an exposure, first spray the tear or breach excessively with the appropriate concentration of a dual quaternary ammonium (n-alkyl dimethyl benzyl ammonium chloride, n-alkyl dimethyl ethyl benzyl ammonium chloride) disinfectant. Do not make excessive movements during this time that create an increase in airflow.
- Carefully, remove the outer O-rings (2 of them) leaving the damaged integrated glove still attached to the Class III BSC. Slightly move the damaged integrated glove cuff away from the port while ensuring the integrated glove seal remains intact. If the seal is compromised, an alarm will sound indicating the procedure was not done correctly. The integrated glove cuff should remain attached to the port after the second O-ring is removed from the Class III BSC.
- Place a new Class III BSC synthetic rubber glove over of the old glove in same orientation. Place this new glove fully over the port similarly to the other Class III BSC glove ports.
- Replace the O-ring closest to the Class III BSC over the new integrated glove. Using an adjacent integrated glove port, carefully pull the damaged Class III BSC synthetic rubber glove inside the Class III BSC. The new Class III synthetic rubber glove will act as the barrier to maintain containment. Once the other damaged Class III synthetic rubber glove is removed (pulled inward), replace the other outer O-ring and continue working.
- Record all details concerning glove tear/breach in the specific Class III BSC log book. If the damaged integrated glove is removed or a breach in containment occurs, the compromised integrated glove/port still maintains an inward air flow of 0.47 m3/sec. This inward airflow is the same airflow used with a Class II BSC, thus maintaining consistency between Class II and Class III BSCs.
- Inspect dunk tank and verify that the dunk tank is filled with disinfectant to the marked level inside the dunk tank, Figure 1. Verify the concentration of disinfectant in the dunk tank is a minimum of 3,500 µS using a conductivity meter. This conductivity is equivalent to 5% concentration of the disinfectant.
- Ensure the Class III BSC autoclave is functional and operational so all contaminated waste and equipment can be autoclaved, Figure 1. Autoclave only equipment known to sustain the rigors of the sterilization process.
- Test the functionality of other aerobiology equipment (e.g., AAMP components, laptop) and air and vacuum lines involved in the experiment, Figure 2.
- Place signs on the Class III BSC indicating the current contamination status of the unit.
- Assembly and System Setup of NHP Head-only Exposure Chamber
- Assemble a 16-l NHP head-only exposure chamber by inserting the stainless steel delivery and exhaust lines, Figure 2. Configure the chamber in a push/pull, dynamic configuration by connecting the appropriate air, vacuum, and pressure lines to the AAMP. Connect the AAMP to a power source within the Class III BSC and a laptop computer through a hermetically sealed port located on top of the Class III BSC (Figure 1).
- Inspect the assembled NHP head-only exposure chamber for any leaks or cracks, and ensure that the chamber is properly assembled.
- Attach an aerosol generator and aerodynamic particle size reading instrument to the NHP head-only exposure chamber.
- Open the air and vacuum source to the AAMP.
- Launch the aerosol protocol software on the laptop computer. Enter the appropriate NHP head-only exposure chamber, aerosol generator and biosampler flow rate, and administrative information into the software menus.
- Calculate the aerosol challenge time from the data acquired during the plethysmography procedure, step 2.2.4. If using the head-out plethysmography, calculate the dose prior to the aerosol exposure. If using RIP, calculate the dose simultaneously during the aerosol exposure.
- Fill the aerosol generator with the pathogen.
- Through the aerosol software, turn the aerosol generator "on" and spray the inside of the NHP head-only exposure chamber with the challenge material for 10 min.
- Turn off the aerosol generator, empty the challenge material, and discard the challenge material into a biohazardous trash bag located inside of the Class III BSC.
- NHP Head-only Exposure
- Attach a biosampler to the NHP head-only exposure chamber, fill the biosampler with collection media, and attach the appropriate vacuum line to the biosampler.
- Check the depth of anesthesia of the NHP. If the depth of anesthesia is considered adequate (e.g., unresponsive to external stimuli, muscular tone, stable respiratory, and heart rates), pass the anesthetized NHP through the rapid transfer port (RTP) into the Class III BSC. If the depth of anesthesia is inadequate, administer additional anesthesia via IV, direct injection, or through an anesthetic pump prior to passing the NHP through the RTP (Comparative Medicine staff in the suit laboratory). Pass additional anesthetic supplies through the RTP.
- Place the NHP in the supine position onto the NHP exposure ramp.
- Gently pass the NHP's head through the rubber/dental dam attached to the head portal of the NHP head-only exposure chamber. The rubber/dental dam ensures a seal is created around the NHP's neck during the aerosol exposure.
- Verify that the NHP's vital signs are stable visually and with a portable subject monitor.
- Enter the aerosol challenge time calculated from step 4.2.6. and necessary equipment identifiers pertinent to each aerosol run into the aerosol software and begin the aerosol challenge.
- Verify particle size data during each aerosol run with the aerosol particle size analyzer to ensure the desired particle size distribution is achieved. Perform this verification continuously or intermittently throughout the exposure.
- Once the aerosol challenge is complete, remove the NHP from the head-only exposure chamber and wipe the NHP's face/head off with the appropriate disinfectant to reduce potential contamination to laboratory staff.
- Purge the aerosol chamber or air wash the remaining and lagging particles for 5 minutes by passing air and vacuum through the chamber. This procedure will "clean out" and remove residual particles from the aerosol exposure chamber for subsequent NHP aerosol exposures.
- Pass the NHP back through the RTP to the researchers located on inside the ABSL-4 aerobiology suit laboratory.
- Discard all sharps used within the Class III BSC in a designated sharps container that remains in the BSC. When the sharps container is ¾ full, place into the biohazard trash bag.
- Empty the aerosol generator and any of remaining challenge material into the biohazardous trash bag containing trash, disposable equipment, and/or ¾-full sharps container if applicable.
- Empty the collection media from the aerosol biosampler into the appropriately labeled collection tubes and place on wet ice.
- Repeat steps 4.3.1 to 4.3.13 until all scheduled test subjects have been challenged.
- Pass all aerosol biosampler samples through the RTP to the researchers for quantification and back titrations of aerosol dose.
- Place the trash and equipment from the aerosol challenge into the pass-through autoclave attached to the Class III BSC and select an applicable sterilization cycle (Figure 3).
- Disassemble the NHP head-only chamber and decontaminate the head-only chamber and the Class III BSC with a paraformaldehyde gas cycle validated with biological indicators.
Representative Results
The Class III biosafety cabinet (BSC) is a hermetically sealed stainless steel cabinet containing an ABSL-4 environment under negative pressure within an ABSL-4 cabinet laboratory (Figure 1). Materials can be introduced into the BSC by staff working in the ABSL-4 cabinet laboratory through an under-cabinet-mounted stainless steel tank (commonly referred to as a "dunk tank" in ABSL-4 or BSL-4 settings) containing a 5% dual quaternary ammonium (n-alkyl dimethyl benzyl ammonium chloride, n-alkyl dimethyl ethyl benzyl ammonium chloride) disinfectant solution. Because the BSC is built into the wall separating the cabinet laboratory from an ABSL-4 suit laboratory, materials, animals, and viral pathogens can also be moved into the BSC from the ABSL-4 suit laboratory side using a transport cart and a Rapid Transfer Port (RTP). The contents within the BSC can be manipulated from the outside by researchers wearing various types of synthetic rubber gloves, specifically neoprene/chlorosulphonated polyethylene. Contents, excluding infectious samples, are removed from the BSC after sterilization through a double-door autoclave or disinfection via the dunk tank. By checking/verifying that the Class III BSC and bioaerosol equipment (Figure 2) is functioning properly, we maintain a safe and properly operational environment. Proper maintenance and use of the Class III BSC is integral to personal protection for the researcher. Following aerosol exposure, trash and equipment from the aerosol challenge to be sterilized are placed into the pass-through autoclave attached to the Class III BSC, Figure 3. Through strict adherence to these procedures and practices, no laboratory-acquired infections have been recorded during bioaerosol research at the IRF-Frederick.
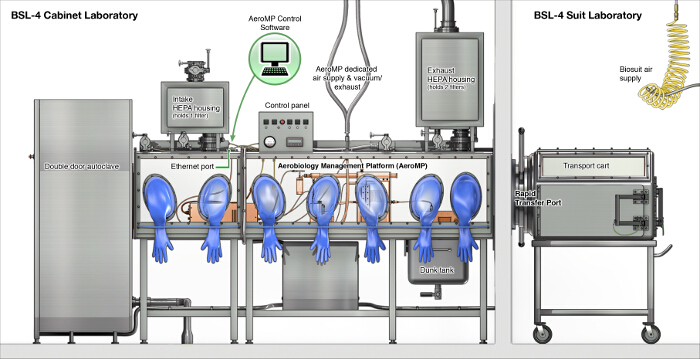 Figure 1. Schematic Presentation of the Class III Biosafety Cabinet Setup at the IRF-Frederick. Presentation of the cabinet in static state (reproduced from 5). Please click here to view a larger version of this figure.
Figure 1. Schematic Presentation of the Class III Biosafety Cabinet Setup at the IRF-Frederick. Presentation of the cabinet in static state (reproduced from 5). Please click here to view a larger version of this figure.
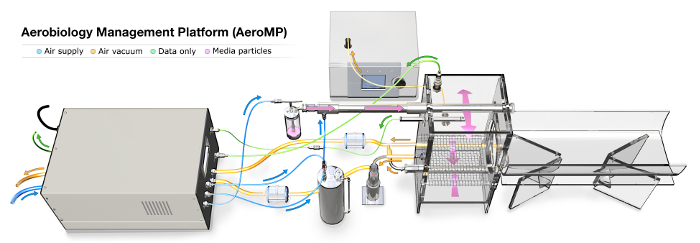 Figure 2.Aerosol Management Platform. Adapted from 5. Please click here to view a larger version of this figure.
Figure 2.Aerosol Management Platform. Adapted from 5. Please click here to view a larger version of this figure.
 Figure 3. Interlocking Double-door Autoclave Attached to the Class III BSC. A researcher is selecting a pre-programmed autoclave cycle to ensure the contents within the autoclave chamber are noninfectious when the outer door is eventually opened. The door located nearest to the researcher cannot be opened until a full sterilization cycle has been completed. Biological indicators inside the autoclave chamber will be analyzed to determine agent inactivation after the sterilization process (reproduced from 5). Please click here to view a larger version of this figure.
Figure 3. Interlocking Double-door Autoclave Attached to the Class III BSC. A researcher is selecting a pre-programmed autoclave cycle to ensure the contents within the autoclave chamber are noninfectious when the outer door is eventually opened. The door located nearest to the researcher cannot be opened until a full sterilization cycle has been completed. Biological indicators inside the autoclave chamber will be analyzed to determine agent inactivation after the sterilization process (reproduced from 5). Please click here to view a larger version of this figure.
Discussion
We outline the aerobiology procedures used at the IRF-Frederick for working with highly hazardous (Risk Group 4) pathogens. One purpose of visualizing the bioaerosol procedures is to emphasize the safety of staff when using a Class III BSC during experimentation with such pathogens to avoid laboratory-acquired infections. Class III BSCs maintain an inward directional airflow that exhausts into double HEPA filters to ensure that pathogens are contained within the laboratory (Figure 1).
As the Class III BSC is the primary barrier in preventing potential pathogen exposure during bioaerosol studies, researchers are required to check the integrity of the Class III BSC and attached integrated gloves for leaks before and after each aerosol experiment. Although every effort is taken to eliminate risk to laboratory researchers, a breach of a Class III BSC integrated synthetic rubber glove may occur. Staff must be provided with both didactic and hands-on training on the proper Class III BSC emergency response procedures. Such procedures include evacuation from the ABSL-4 cabinet laboratory, securing a breach in containment to the Class III BSC, and donning of personal protective equipment when necessary. We have used other gloves of varying thickness in the past that are dependent on the fine motor skills required for the procedure. Regardless of the thickness, all gloves chosen are equally as protective when performing these procedures. Robust training, strict adherence to safety protocols, and engineering controls help to ensure employee safety when using Class III BSCs at the IRF-Frederick. The processes above are subject to change due to new methodologies or safety reevaluations based on improving the workflow.
While the aerobiological procedures presented here generally follow the BMBL recommendations7, these procedures are specific to the IRF-Frederick. Each ABSL-4/BSL-4 facility has different building design specifications that impact the exact methods of laboratory operation. Alternative procedures and techniques for using Class III BSC laboratories depend in part on the design and operation of these laboratories. In addition, varying government regulations in different countries may also have an effect on aerosol research procedures. Nevertheless, a general understanding of ABSL-4 aerosol procedures and the building monitoring systems that support the safety of laboratory researchers will help health administrators, who are contemplating the design of similar buildings, and outside collaborators involved in studies of high-consequence pathogens.
When designing bioaerosol protocols with outside collaborators, sufficient time should be allotted to perform even basic bioaerosol operations. Expectations of time frames for delivering results have to be adjusted by accepting the difficulties inherent with work in ABSL-4 Class III BSC laboratories. A generalized assumption is that any bioaerosol experiment performed at ABSL-2 (e.g., 2 hr) will require twice the amount of time to perform in ABSL-4 (e.g., 4 hr).
Disclosures
The authors have nothing to disclose.
Acknowledgments
The content of this publication does not necessarily reflect the views or policies of the US Department of Health and Human Services (DHHS) or of the institutions and companies affiliated with the authors. This work was funded in part through Battelle Memorial Institute's prime contract with the US National Institute of Allergy and Infectious Diseases (NIAID) under Contract No. HHSN272200700016I. J.K.B., K.J., M.R.H., D.P., L.B., and J.W. performed this work as employees of Battelle Memorial Institute. Subcontractors to Battelle Memorial Institute who performed this work are: J.H.K., an employee of Tunnell Government Services, Inc.; and M.G.L., an employee of Lovelace Respiratory Research Institute.
References
- Alibek K, Handelman S. The chilling true story of the largest covert biological weapons program in the world-told from inside by the man who ran it. New York, NY: Random House; 1999. [Google Scholar]
- Roy CJ, Pitt LM. Infectious disease aerobiology: aerosol challenge methods. In: Swearingen JR, editor. Biodefense: research methodology and animal models. Boca Raton, FL: Taylor & Francis; 2006. pp. 61–76. [Google Scholar]
- National Institute of Allergy and Infectious Diseases. NIAID Category A, B, and C Priority Pathogens. Bethesda, MD, USA: National Institutes of Health; 2014. Available from: http://www.niaid.nih.gov/topics/biodefenserelated/biodefense/pages/cata.aspx. [Google Scholar]
- National Center for Environmental Health; Agency for Toxic Substances and Disease Registry; National Center for Injury Prevention and Control. Bioterrorism agents/diseases by category. Atlanta, GA, USA: Centers for Disease Control and Prevention; 2014. Available from: http://emergency.cdc.gov/agent/agentlist-category.asp. [Google Scholar]
- Lackemeyer MG, et al. ABSL-4 aerobiology biosafety and technology at the NIH/NIAID integrated research facility at Fort Detrick. Viruses. 2014;6(1):137–150. doi: 10.3390/v6010137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bohannon JK, et al. Generation and characterization of large-particle aerosols using a center flow tangential aerosol generator with a non-human-primate, head-only aerosol chamber. Inhal Toxicol. 2015. [DOI] [PMC free article] [PubMed]
- Chosewood LC, Wilson DE, eds , editors. Biosafety in Microbiological and Biomedical Laboratories. 5th edn. Washington, D.C.: U.S. Dept. of Health and Human Services; 2009. Available from: http://www.cdc.gov/biosafety/publications/bmbl5/ [Google Scholar]
- Janosko K, et al. Safety Precautions and Operating Procedures in an (A)BSL4 Laboratory: 1. Biosafety level 4 suit laboratory suite entry and exit procedures. J Vis Exp. 2015. [DOI] [PMC free article] [PubMed]
- Mazur S, et al. Safety Precautions and Operating Procedures in an (A)BSL4 Laboratory: 2. General Practices. J Vis Exp. 2015. [DOI] [PMC free article] [PubMed]
- Mortola JP, Frappell PB. On the barometric method for measurements of ventilation, and its use in small animals. Can J Physiol Pharmacol. 1998;76(10-11):937–944. doi: 10.1139/cjpp-76-10-11-937. [DOI] [PubMed] [Google Scholar]
- Zhang Z, et al. Development of a respiratory inductive plethysmography module supporting multiple sensors for wearable systems. Sensors (Basel) 2012;12(10):13167–13184. doi: 10.3390/s121013167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ingram-Ross JL, et al. Cardiorespiratory safety evaluation in non-human primates. J Pharmacol Toxicol Meth. 2012;66(2):114–124. doi: 10.1016/j.vascn.2012.04.002. [DOI] [PubMed] [Google Scholar]
- Besch TK, Ruble DL, Gibbs PH, Pitt ML. Steady-state minute volume determination by body-only plethysmography in juvenile rhesus monkeys. Lab Anim Sci. 1996;46(5):539–544. [PubMed] [Google Scholar]


