Abstract
Objective
Microbial larviciding may be a potential supplement to conventional malaria vector control measures, but scant information on its relative implementation costs and effectiveness, especially in rural areas, are an impediment to expanding its uptake. We perform a costing analysis of a seasonal microbial larviciding program in rural Tanzania.
Methods
We evaluated the financial and economic costs from the perspective of the public provider of a three-month, community-based larviciding intervention implemented in twelve villages in the Mvomero district of Tanzania in 2012–2013. Cost data were collected from financial reports and invoices and through discussion with program administrators. Sensitivity analysis explored the robustness of our results to varying key parameters.
Results
Over the two-year study period, approximately 6,590 breeding sites were treated with larvicide. The average annual economic costs the larviciding intervention in rural Tanzania are estimated at 2014 US$ 1.44 per person protected per year (pppy), US$ 6.18 per household, and US$ 4,481.88 per village, with the larvicide and staffing accounting for 14% and 58% of total costs, respectively.
Conclusions
We found the costs pppy of implementing a seasonal larviciding program in rural Tanzania to be comparable to the costs of other larviciding programs in urban Tanzania and rural Kenya. Further research should evaluate the cost-effectiveness of larviciding relative to, and in combination with, other vector control strategies in rural settings.
Keywords: microbial larviciding, costs, malaria, vector control, Tanzania
INTRODUCTION
Despite progress in malaria control, malaria remains a serious global challenge. WHO estimates that by 2020, 6.4 billion dollars will be needed annually to sustain malaria control and elimination efforts. However, in 2014, global malaria funding was only 2.5 billion dollars (1), underscoring the importance of prudent resource allocation.
Vector control efforts have primarily relied on the use of long-lasting insecticide treated nets (LLINs) and indoor residual spraying (IRS) (2). While these tools have yielded significant reductions in malaria transmission, there is a need to identify synergistic combinations of vector control strategies (3), especially in the face of emerging insecticide resistance (4, 5). WHO has advocated for an Integrated Vector Management (IVM) strategy, a capacity-building approach in which multiple interventions, tailored to unique ecological settings (6), are employed jointly to increase cost-effectiveness and sustainability (7, 8).
Microbial larviciding, a form of larval source management (LSM), may be a valuable supplement to conventional vector control measures (9). A recent Cochrane Review concluded that LSM may reduce malaria morbidity in areas in which a majority of breeding sites can be accessed, but added that more research is necessary to evaluate the feasibility of LSM in rural areas where breeding sites are large or numerous (10). The WHO issued a statement emphasizing that larviciding should be considered as a complement to, and not a replacement for, IRS or LLINs (11). An evaluation of a large-scale larviciding program in Tanzania concluded that larviciding may be cost-effective in urban settings (12).
Few studies have evaluated the costs and feasibility of larviciding in rural areas. One study of a larviciding program in rural Gambia called into question the feasibility of larviciding in areas with extensive larval habitats (e.g., large swamps, rice paddies) and seasonal flooding (13). Another study reported that the economic costs per person protected (inflated to 2014 US$) of a larviciding campaign in an urban area (US$ 1.07) were comparable to that of LLIN and IRS campaigns, while larviciding had higher costs in rural areas (US$ 1.71, US$ 2.85) (14).
In this paper, we present a costing analysis of a two-year, community-based larviciding intervention using the larvicide, Bacillus thuringiensis var. israelensis (Bti), in rural Mvomero, Tanzania. Bti, a commonly-used active ingredient in microbial larviciding, is safe for both humans and the environment (9). This study seeks to inform policymakers in designing malaria control programs for rural areas where malaria persists despite high levels of mosquito net usage.
METHODS
Study Area
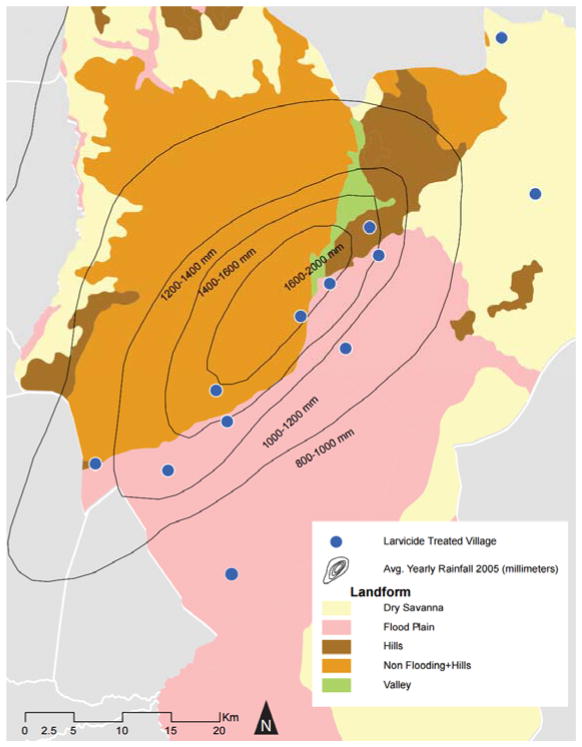
The study was conducted in the northern part of the Mvomero district (Mvomero and Turiani divisions), Morogoro Region, Tanzania. The larviciding intervention was conducted in 2012–2013 in twelve randomly-selected villages across multiple landform types (Figure 1) involved in a larger two-by-two factorial study, described elsewhere (15). In 2012, the population of the Mvomero district was 312,109 people, with a population density of 47.1 people/km2 and an average of 4.3 inhabitants per household (16). Based on this, the estimated population in the area covered by the intervention in 2012 is 37,083 people (estimated to include 8,624 households), with 3,090 people per village. The population covered by the intervention in 2013 was estimated using the average annual population growth rate in the Mvomero district (+1.86%/year from 2002–2012) (16).
Figure 1.
Map of larvicide treated villages in Mvomero District
Average rainfall in Mvomero is high (1146 mm per year) (17). The rainy seasons are from March to May and October to December (15). The average maximum temperature is 30 °C, and the average minimum is 20 °C (18). Over 80% of adults work in subsistence agriculture (19).
The 2011–12 Tanzania HIV/AIDS and Malaria Indicator Survey (THMIS) reports that malaria prevalence among children aged 6–59 months in the Morogoro Region was 13% (20). Parasitemia prevalence varies by agroecosystem, with higher prevalence in villages with flooding rice irrigation (22). Malaria is transmitted year-round, with peak transmission during the March-May rainy season. The most common vector is Anopheles gambiae (58.9%), with An. funestus being the second most common vector (12.0%), and the mean annual entomological inoculation rate (EIR) for An. gambiae sensu lato was 728 infective bites per person per year (19).
Baseline mosquito net coverage was high following a recent government LLIN distribution campaign. The 2011–12 THMIS reports that 84.2% of household members in the Morogoro region had slept under a mosquito net before surveying, while only 1.4% of surveyed households had received IRS (20). Throughout implementation, no other large-scale vector control activities (i.e., IRS, other LSM programs, etc.) were taking place.
Larvicide intervention
The design of the larviciding intervention is described elsewhere (15). Briefly, in each of the 12 intervention villages, the study recruited two village members to apply larvicide. Knowledgeable trainers (including a field supervisor and an international technical adviser) convened the staff for hands-on instruction on how and where to apply larvicide and to monitor and record information about breeding sites and work activities. Potential breeding sites (water bodies within one km of a household in a study village) were identified by local staff in consultation with community members. Water body types included puddles, natural and man-made ponds, roadside ditches and canals, stagnant water alongside streams, irrigated and non-irrigated rice paddies, and temporary wetlands. Staff recorded information about each site, including date(s) visited, type, location, and size, estimated by calculating the area based on length and width of the site as measured by number of steps multiplied by the individual’s gait. Larval density was measured using a 350 ml mosquito dipper, in accordance with WHO standards (24). The number of capture stations where dipping was conducted per site was proportional to the size of the breeding habitat, with up to five dispersed dipping locations for large sites. Staff applied larvicide to sites where larvae were detected, measuring and recording the amount applied as dictated by site size (at an application dosage of 10 kg per hectare, according to manufacturer’s instructions). To ensure sufficient dosage, staff were trained and periodically evaluated by the field supervisor on how to estimate the amount to be applied, and were provided with job aids to facilitate calculations. The larvicide was a commercially available, granular formulation (VectoBac® CG, since renamed VectoBac® GS) of Bti strain AM65-52, Valent BioSciences Corporation (VBC, Libertyville, IL, USA). Staff applied and reapplied the larvicide roughly every 7–10 days based on the results of regular dipping at identified breeding sites (i.e., when mosquito larvae were found during dipping) (15). In small habitats, larvicide was applied by hand, and in larger habitats, Cifarelli backpack sprayers were used. The application of larvicide took place over approximately the same three-month period in two consecutive years, coinciding with the peak rainy season (in the second year, larviciding began just before the start of the rainy season) (25). The supervisor oversaw and reported on field activities, conducted quality control assessments, and restocked supplies, visiting within the first week of the three-month implementation period in each village, and at least once every two weeks thereafter on a rotating basis throughout the implementation period.
At the end of the program, three larvicide applicators provided feedback on the feasibility of their work through interviews with trained staff.
Estimation of costs
Data sources for the cost data include semiannual budgetary reports for the intervention and discussions with program administrators. The cost of the intervention was estimated using an ingredients approach (26): first, inputs necessary to the intervention are identified, next, the unit cost of the inputs are determined, and finally the costs are calculated by multiplying the unit costs with the utilized quantity of the input (Appendix S2). For most inputs, the number of units consumed was known. For inputs where only aggregate costs were available, we estimated the number of units consumed through discussion with program administrators. Costs incurred during the intervention period which would not be required for implementation outside of the context of the research study were excluded. These costs included salary and travel for US-based research staff (with the exception of the international technical advisor), university overhead costs, and costs associated with conducting annual parasitological surveying to measure study endpoints. The perspective of the public provider was taken in determining costs, as is commonly used in malaria costing and cost-effectiveness studies (28–30). This perspective only considers the costs incurred by the provider entity in implementing the intervention, and disregards costs incurred solely by the community (e.g., community members’ time spent in sensitization meetings).
Inflation factors for the larvicide were derived from US Bureau of Labor Statistics (BLS) Producer Price Index for “all other basic organic manufacturing sector” (Appendix S1). Inflation factors for all other products and services were derived from the US BLS Consumer Price Index (Appendix S1). Exchange rates were derived from the International Financial Statistics (IFS) database (Appendix S1). The financial and economic costs per person protected per year (pppy) and per household were determined by dividing the total financial or economic costs by the estimated population or number of households in the villages covered by the intervention.
Financial Costing
Financial costing accounts for the measured costs of purchased resources necessary in implementing the intervention (26). Project staff clarified expenses and their proper allocation among project activities. Most financial costs were initially measured in the local currency (Tanzanian shillings). Using the market exchange rate for the year in which the cost was incurred (Appendix S1), the costs were converted into US dollars and subsequently inflated to March 2014 values (30).
Economic Costing
While financial costing captures the expenditures for purchased inputs (32), economic costing accounts for the value of all inputs required for the intervention, including the opportunity costs of donated or pre-existing resources and equipment (26). Transfer costs that do not reflect actual resource consumption (e.g. taxes) were excluded. Economic costing also accounted for inputs anticipated to be necessary for sustainable public provider-led implementation of the program, yet may not have been included in our trial intervention. A discount rate of 3% was applied, as per the U.S. Panel on Cost-Effectiveness in Health and Medicine (33). Capital costs were annualized over their useful lives (Appendix S1) (27, 34). Costs were presented in March 2014 values. The effect of varying key parameters on the economic costs per person protected per year (pppy) was evaluated in one-way sensitivity analysis.
Cost Classification
Costs were separated into capital and recurrent costs. Resources that had a useful life of over a year were treated as capital costs, while recurrent costs generally lasted for one year or less and were regularly purchased (32, 34). Capital costs included purchased vehicles and equipment and storage. Recurrent costs included staffing, information, education, and communication (IEC), transport, the larvicide, and operational costs.
Ethical considerations
The overall study protocol received ethical approval from both the Medical Research Coordination Committee of the National Institute for Medical Research and the Institutional Review Board of Duke University. Before implementation the project team briefed the community on the intervention through sensitization meetings in all villages.
RESULTS
Over the course of the two three-month intervention periods, breeding sites were larvicided 86% of the time, based on dipping results. For sites where larvicide status was recorded, site size was estimated for 96% of sites, ranging from less than one square meter to 6.0 hectares. Among these sites, the total area larvicided across both intervention years was approximately 457 hectares (6,590 sites, mean 694 square meters per site), using 4,752.6 kg of larvicide (mean 10.34 kg per hectare).
As presented in Table 1, the annual average financial costs for the Mvomero larviciding program were US$ 42,649.25. The financial cost per person protected per year (pppy) was US$ 1.15, per household protected US$ 4.90, and per village US$ $3,554.10. The majority of financial costs (72%) were incurred in the first year because the larvicide for both rounds of the interventions was shipped and purchased in the first year. Also, costs associated with hiring and travel of an international technical adviser were incurred in the first year.
Table 1.
Larviciding in Mvomero: Financial costs for twelve villages (US$ 2014)
| Cost category | Year 1 | Year 2 | Annual Average | Proportion of Total Average: |
|---|---|---|---|---|
|
| ||||
| RECURRENT COSTS | ||||
|
| ||||
| Staff Costs | 23,425.95 | 10,683.95 | 17,054.95 | .40 |
| Information, Education, Communication | 5,320.29 | 5,320.29 | 5,320.29 | .12 |
| Transport | 6,363.16 | 2,727.30 | 4,545.23 | .11 |
| Larvicide | 15,226.87 | 0.00 | 7,613.43 | .18 |
| Operational Costs | 3,302.16 | 3,302.16 | 3,302.16 | .01 |
|
| ||||
| SUBTOTAL RECURRENT COSTS | 53,638.43 | 22,033.71 | 37,836.07 | .89 |
|
| ||||
| CAPITAL COSTS | ||||
|
| ||||
| Vehicles | 0.00 | 2,202.89 | 1,101.45 | .03 |
| Equipment and Storage | 7,423.48 | 0.00 | 3,711.74 | .09 |
|
| ||||
| SUBTOTAL CAPITAL COSTS | 7,423.48 | 2,202.89 | 4,813.19 | .11 |
|
| ||||
| TOTAL COSTS OF PROGRAM | 61,061.91 | 24,236.60 | 42,649.25 | |
Economic costs are presented in Table 2. Details regarding the unit costs and the number of units consumed can be found in Appendix S2. The total average annual economic cost was US$ 53,782.53. The economic cost pppy was US$ 1.44, per household US$ 6.18, and per village US$ 4,481.88. Staffing accounted for 58% of total economic costs. Project oversight from a district-level public health officer and additional managerial staff (project manager and administrative assistant), absent in the trial intervention, was included in the economic costs as these inputs were deemed necessary for sustainable government-directed implementation. The district public health officer would be engaged in comprehensive oversight of program implementation, as well as integration and coordination of the program within broader Tanzanian Ministry of Health and Social Welfare operations. The project manager would report to the public health officer and be chiefly responsible for coordinating on-the-ground program implementation and operations, including management of field staff, developing IEC activities, central procurement, monitoring, and reporting. The administrative assistant would support the public health officer and project manager in carrying out their duties, including financial reporting, recordkeeping, and administrative and operational tasks. IEC inputs, consisting of community sensitization efforts and training workshops for the larvicide applicators, accounted for 10% of total economic costs. The transportation category, which included costs associated with renting vehicles and shipping equipment and larvicide, made up 8% of total economic costs. Larvicide was shipped as ocean freight from the U.S. A truck was rented to transport supplies and the larvicide. A motorcycle was also rented for the field supervisor. The larvicide, priced at US$1.50 per pound (approximately US$3.31 per kg), made up 14% of total economic costs. Operational costs, including office space, utilities, housing supplies, and communication expenses, made up 5% of economic costs. Vehicles (bicycles), accounting for only 1% of economic costs, were purchased for the larvicide applicators. Equipment, comprising handheld Pf-Cifarelli motorized sprayers, mosquito dippers, protective clothing, and GPS units for mapping breeding sites, accounted for 4% of total economic costs.
Table 2.
Larviciding in Mvomero: Average annual economic costs for twelve villages (US$ 2014)
| Cost category | Average Annual Costs: | Proportion of Total Average |
|---|---|---|
|
| ||
| RECURRENT COSTS | ||
|
| ||
| Staff | 31,180.56 | .58 |
| Information, Education, Communication | 5,242.81 | .10 |
| Transport | 4,304.14 | .08 |
| Larvicide | 7,613.43 | .14 |
| Operational Costs | 2,690.76 | .05 |
|
| ||
| SUBTOTAL RECURRENT COSTS | 50,433.01 | .96 |
|
| ||
| CAPITAL COSTS | ||
|
| ||
| Vehicles (bicycles) | 406.65 | .01 |
| Equipment and Storage | 2,344.17 | .04 |
|
| ||
| SUBTOTAL CAPITAL COSTS | 2,750.82 | .05 |
|
| ||
| TOTAL COSTS OF PROGRAM | 53,782.53 | |
|
| ||
| COST PER PERSON PROTECTED PER YEAR | 1.44 | |
Sensitivity analysis (Table 3) reveals that the estimates for economic costs per person protected per year are highly sensitive to the staff salary costs and our estimate of the population covered by the intervention, and moderately sensitive to the larvicide cost.
Table 3.
Results of one-way sensitivity analysis on economic cost per person protected per year (US$ 2014)
| Variation Tested | Cost per person protected |
|---|---|
| Base Case | 1.44 |
| Increasing discount rate to 5% or reducing to 0% (base case 3%) | 1.43/1.52 |
| Increasing cost of salaries of all staff (or reducing) by 20% | 1.60/1.27 |
| Increasing cost of larvicide (or reducing) by 20% | 1.48/1.40 |
| Increasing (or reducing) the estimate of the population covered by the intervention by 20% | 1.20/1.80 |
The three interviewed larvicide applicators said they were comfortable and satisfied with their work and commented that covering a village was manageable for a team of two people. They also felt that their work became easier and more manageable as they gained confidence and experience in the second year of implementation. In general, larvicide applicators felt they could cover even more breeding sites than they did in practice.
DISCUSSION
We measured the costs of a seasonal larviciding program for malaria control in rural Tanzania. The total annual average economic costs (US$ 53,782.53) exceeded the total annual average financial costs (US$ 42,649.26). This is primarily because the economic costing accounted for the value of inputs (additional staffing roles) anticipated to be required by the public provider in sustainably integrating and institutionalizing a community-based larviciding program into existing public health activities (14, 36).
Our estimate for the economic cost per person protected per year (pppy) of our rural larviciding intervention is 2014 US$ 1.44. This estimate is comparable to larviciding cost pppy estimates (inflated to 2014 US$) in urban Tanzania (US$ 1.07) and in the rural Kenyan highlands (US$ 1.71), yet lower than in the rural Kenyan lakeside (US$ 2.85) (14). The duration of larviciding campaigns varied significantly across settings, underscoring the need to design larviciding programs tailored to regional malaria transmission patterns. A direct comparison of our estimates with literature estimates is challenging due to the lack of standardization in costing methods (29). However, there appears to be variation in the cost pppy of larviciding across diverse rural settings, and our estimate falls within the range of costing estimates for other larviciding programs in Sub-Saharan Africa.
Our estimate can be further contextualized through comparisons with estimates of the cost pppy for other vector control tools. In a review article, Yukich et al. report that for LLINs, the cost per treated net year (TNY) of protection (inflated to 2014 US$) ranged from US$ 1.67 to 2.30, and for IRS, the cost pppy (inflated to 2014 US$) ranged from US$ 3.96 to 4.73 (28). While the meaning of protection varies across these interventions, precluding a direct comparison, the relatively low pppy of larviciding suggests its fiscal viability as a supplement to traditional vector control methods.
Our larviciding program used the granular larvicide formulation, which can be more expensive than other formulations (14). The choice of larvicide formulation depends upon the types of habitats covered, and as such, program costs are also related to the types of habitats covered. The density of larval habitats in relation to human population density also affects program costs (14). Future development of longer-lasting formulations may not only improve the efficacy of larviciding campaigns (25), but also reduce the labor required, which accounts for a significant portion of total costs (Table 2).
Our results demonstrate that the implementation of a larviciding program can have significant start-up costs (Table 1), including the initial purchase and shipping of the larvicide for use over a two-year period, as well as technical support from an international adviser. In practice, larvicide could be purchased annually in smaller quantities to offset startup costs. International support may only be required at the outset of the program, after which local staff may acquire the technical expertise to independently administer the program (12).
Apart from costs, operational feasibility is also an important consideration for policymakers. Our interviews with larvicide applicators suggest that the workload was feasible. Another consideration is community acceptability and the societal costs of community engagement. Community support for larviciding was high at baseline in the study area (9). During implementation, community-level involvement included optional attendance at annual meetings convened by staff to share information on program activities, and donated time from community members related to their engagement in study activities (offering information about locating and accessing breeding sites, providing consent as necessary). Hiring local staff to apply larvicide in their own villages meant that the staff entered with a baseline familiarity with and access to the community in which they worked, reducing the need to rely on volunteer guides. We therefore estimate that the opportunity costs for community involvement were low and unlikely to significantly affect the cost estimates, similar to the conclusions of two cost-effectiveness studies of larviciding programs (12, 37).
This study has several limitations. First, the sensitivity analysis reveals the dependence of our cost on the estimate of population size, which may be skewed if the average population of larvicide-treated villages differs significantly from the average village size in the Mvomero district. Also, in our economic costing, we sought to account for the costs of resources that may not have been part of this trial intervention, but would be necessary in practice for the public provider to scale the program. However, we may not have captured all necessary public provider inputs, especially those related to infrastructure development (36).
The direct application of our findings to other settings is limited by the dependence of cost pppy on the number and types of breeding sites, which can vary dramatically even within a small area due to differences in environmental and land-use conditions. Differences in breeding site number, size, and type would affect staff and larvicide requirements. This program targets the application of larvicide to the three-month period just before and during the rainy season, when malaria transmission peaks, but optimal program duration may vary by setting (14). Future research could examine the sensitivity of costs to the number and type of breeding sites, as well as the duration of programming.
Our findings add to the limited knowledge base regarding the cost of larviciding in rural Sub-Saharan Africa. In considering larviciding, decision-makers should consider local environmental and land-use context, as well as available cost-effectiveness data. While the implementation costs for larviciding compare favorably with other vector control measures, larviciding should not be considered as a stand-alone approach, but rather as a complimentary intervention within a broader IVM strategy.
Supplementary Material
Acknowledgments
This study received funding from the National Institute of Allergy and Infectious Diseases (NIAID). The content is the responsibility of the authors and does not necessarily represent the official views of the NIAID or the National Institutes of Health. We acknowledge Yahya Derua and Dionis Rwegoshora of the National Institute for Medical Research for technical and field assistance, and Joshua Tootoo of Rice University for creating Figure 1. This manuscript is published with permission from the Director General, NIMR – Tanzania. Valent BioSciences Corporation (VBC, Libertyville, IL, USA) donated larvicide and expertise to the implementation of the project in Mvomero, but VBC did not impact data analysis or the decision to publish.
References
- 1.World Malaria Report 2014. Geneva: World Health Organization; 2014. [Google Scholar]
- 2.RBM. Roll Back Malaria Progress & Impact Series. Roll Back Malaria Partnership; 2008. [Google Scholar]
- 3.O’Meara WP, Mangeni JN, Steketee R, Greenwood B. Changes in the burden of malaria in sub-Saharan Africa. The Lancet infectious diseases. 2010;10(8):545–55. doi: 10.1016/S1473-3099(10)70096-7. [DOI] [PubMed] [Google Scholar]
- 4.Trape J-F, Tall A, Diagne N, Ndiath O, Ly AB, Faye J, et al. Malaria morbidity and pyrethroid resistance after the introduction of insecticide-treated bednets and artemisinin-based combination therapies: a longitudinal study. The Lancet infectious diseases. 2011;11(12):925–32. doi: 10.1016/S1473-3099(11)70194-3. [DOI] [PubMed] [Google Scholar]
- 5.Takken W. Do insecticide-treated bednets have an effect on malaria vectors? Tropical Medicine & International Health. 2002;7(12):1022–30. doi: 10.1046/j.1365-3156.2002.00983.x. [DOI] [PubMed] [Google Scholar]
- 6.Mutero CM, Schlodder D, Kabatereine N, Kramer R. Integrated vector management for malaria control in Uganda: knowledge, perceptions and policy development. Malaria journal. 2012;11:21. doi: 10.1186/1475-2875-11-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.WHO. WHO position statement on integrated vector management. Weekly epidemiological record. 2008;20:177–84. [PubMed] [Google Scholar]
- 8.Lizzi KM, Qualls WA, Brown SC, Beier JC. Expanding Integrated Vector Management to promote healthy environments. Trends in parasitology. 2014;30(8):394–400. doi: 10.1016/j.pt.2014.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mboera LE, Kramer RA, Miranda ML, Kilima SP, Shayo EH, Lesser A. Community Knowledge and Acceptance of Larviciding for Malaria Control in a Rural District of East-Central Tanzania. International journal of environmental research and public health. 2014;11(5):5137–54. doi: 10.3390/ijerph110505137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tusting LS, Thwing J, Sinclair D, Fillinger U, Gimnig J, Bonner KE, et al. Mosquito larval source management for controlling malaria. The Cochrane database of systematic reviews. 2013;8:CD008923. doi: 10.1002/14651858.CD008923.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.WHO. Interim Position Statement – the role of larviciding for malaria control in sub-Saharan Africa. World Health Organization; 2012. [Google Scholar]
- 12.Maheu-Giroux M, Castro MC. Cost-effectiveness of larviciding for urban malaria control in Tanzania. Malaria journal. 2014;13(1):477. doi: 10.1186/1475-2875-13-477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Majambere S, Pinder M, Fillinger U, Ameh D, Conway DJ, Green C, et al. Is Mosquito Larval Source Management Appropriate for Reducing Malaria in Areas of Extensive Flooding in The Gambia? A Crossover Intervention Trial. The American Journal of Tropical Medicine and Hygiene. 2010;82(2):176–84. doi: 10.4269/ajtmh.2010.09-0373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Worrall E, Fillinger U. Large-scale use of mosquito larval source management for malaria control in Africa: a cost analysis. Malaria journal. 2011;10:338. doi: 10.1186/1475-2875-10-338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kramer RA, Mboera LE, Senkoro K, Lesser A, Shayo EH, Paul CJ, et al. A Randomized Longitudinal Factorial Design to Assess Malaria Vector Control and Disease Management Interventions in Rural Tanzania. International journal of environmental research and public health. 2014;11(5):5317–32. doi: 10.3390/ijerph110505317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.2012 Population and Housing Census. National Bureau of Statistics, Ministry of Finance; Dar es Salaam: 2012. [Google Scholar]
- 17.Mboera L. Malaria and agriculture in Tanzania: impact of land-use and agricultural practices on malaria burden in Mvomero District. National Institute for Medical Research; 2007. [Google Scholar]
- 18.Mlozi MR, Shayo EH, Senkoro KP, Mayala BK, Rumisha SF, Mutayoba B, et al. Participatory involvement of farming communities and public sectors in determining malaria control strategies in Mvomero District, Tanzania. Tanzan Health Res Bull. 2006;8(3):134–40. doi: 10.4314/thrb.v8i3.45110. [DOI] [PubMed] [Google Scholar]
- 19.Mboera LE, Senkoro KP, Mayala BK, Rumisha SF, Rwegoshora RT, Mlozi MR, et al. Spatio-temporal variation in malaria transmission intensity in five agro-ecosystems in Mvomero district, Tanzania. Geospatial health. 2010;4(2):167–78. doi: 10.4081/gh.2010.198. [DOI] [PubMed] [Google Scholar]
- 20.TACAIDS Z, NBS OCGS I. Tanzania HIV/AIDS and Malaria Indicator Survey 2011–12. Dar es Salaam, Tanzania Dar es Salaam, Tanzania: Tanzania Commission for AIDS (TACAIDS), Zanzibar AIDS Commission (ZAC), National Bureau of Statistics (NBS), Office of the Chief Government Statistician (OCGS), and ICF International; 2013. [Google Scholar]
- 21.Ngasongwa J. Profile–Tanzania, Morogoro Region. Ministry of Planning, Economy and Empowerment; Tanzania: 2007. [Google Scholar]
- 22.Mboera LE, Senkoro KP, Rumisha SF, Mayala BK, Shayo EH, Mlozi MR. Plasmodium falciparum and helminth coinfections among schoolchildren in relation to agro-ecosystems in Mvomero District, Tanzania. Acta tropica. 2011;120(1):95–102. doi: 10.1016/j.actatropica.2011.06.007. [DOI] [PubMed] [Google Scholar]
- 23.Randell HF, Dickinson KL, Shayo EH, Mboera LE, Kramer RA. Environmental Management for Malaria Control: Knowledge and Practices in Mvomero, Tanzania. EcoHealth. 2010;7(4):507–16. doi: 10.1007/s10393-010-0343-9. [DOI] [PubMed] [Google Scholar]
- 24.World Health Organization. Larval source management: a supplementary malaria vector control measure: an operational manual. Geneva: World Health Organization; 2013. [Google Scholar]
- 25.Zhou G, Afrane YA, Dixit A, Atieli HE, Lee M-C, Wanjala CL, et al. Modest additive effects of integrated vector control measures on malaria prevalence and transmission in western Kenya. Malaria journal. 2013;12(1):256. doi: 10.1186/1475-2875-12-256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Creese A, Parker D. Cost analysis in primary health care. Geneva: World Health Organization; 1994. [Google Scholar]
- 27.Drummond M, Schulpher M, Torrance G, O’Brien B, Stoddart G. Methods for the Economic Evaluation of Health Care Programmes. 3. Oxford: Oxford University Press; 2005. [Google Scholar]
- 28.Yukich JO, Lengeler C, Tediosi F, Brown N, Mulligan JA, Chavasse D, et al. Costs and consequences of large-scale vector control for malaria. Malaria journal. 2008;7:258. doi: 10.1186/1475-2875-7-258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kolaczinski J, Hanson K. Costing the distribution of insecticide-treated nets: a review of cost and cost-effectiveness studies to provide guidance on standardization of costing methodology. Malaria journal. 2006;5:37. doi: 10.1186/1475-2875-5-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.White MT, Conteh L, Cibulskis R, Ghani AC. Costs and cost-effectiveness of malaria control interventions--a systematic review. Malaria journal. 2011;10:337. doi: 10.1186/1475-2875-10-337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yukich JO, Zerom M, Ghebremeskel T, Tediosi F, Lengeler C. Costs and cost-effectiveness of vector control in Eritrea using insecticide-treated bed nets. Malaria journal. 2009;8:51. doi: 10.1186/1475-2875-8-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Phillips M, Mills A, Dye C. Guidelines for cost-effectiveness analysis of vector control. World Health Organization; 1993. [Google Scholar]
- 33.Weinstein MC, Siegel JE, Gold MR, Kamlet MS, Russell LB. Recommendations of the Panel on Cost-effectiveness in Health and Medicine. Jama. 1996;276(15):1253–8. [PubMed] [Google Scholar]
- 34.Walker D, Kumaranayake L. Allowing for differential timing in cost analyses: discounting and annualization. Health policy and planning. 2002;17(1):112–8. doi: 10.1093/heapol/17.1.112. [DOI] [PubMed] [Google Scholar]
- 35.Gold M, Russel L, Siegel J, Weinstein M. Cost-effectiveness in health and medicine. 1996 [Google Scholar]
- 36.Chaki PP, Kannady K, Mtasiwa D, Tanner M, Mshinda H, Kelly AH, et al. Institutional evolution of a community-based programme for malaria control through larval source management in Dar es Salaam, United Republic of Tanzania. Malaria journal. 2014;13(1):245. doi: 10.1186/1475-2875-13-245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Suaya JA, Shepard DS, Chang MS, Caram M, Hoyer S, Socheat D, et al. Cost-effectiveness of annual targeted larviciding campaigns in Cambodia against the dengue vector Aedes aegypti. Tropical Medicine & International Health. 2007;12(9):1026–36. doi: 10.1111/j.1365-3156.2007.01889.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.