Abstract
Cancer is currently a leading cause of deaths worldwide and the number of new cases is growing rapidly in both, developed and developing countries. Nutritional management during and after cancer treatment affects treatment efficacy and patient quality of life (QOL). This review systemically examined the effect of oral nutritional interventions on nutritional and clinical outcomes in cancer patients. We especially focused on outcomes such as nutritional status indices, immune-associated biochemical markers, and QOL assessments to provide insights on the applicability of different outcomes. A total of 28 papers were selected for systematic review. The nutritional composition of oral nutritional supplements (ONS), outcome measures, and efficacy of the oral nutritional interventions were summarized and discussed. Most ONS contain 1 or more functional components in addition to basic nutrients. Each study used various outcome measures and significant efficacy was observed for a limited number of measures. Nutritional status indices, QOL measures, and the duration of hospital stay improved in about 40% of the studies. One or more markers of immune function and inflammatory responses were improved by ONS in 65% of the selected studies. These results suggest that appropriate use of ONS may be an ideal way to improve treatment efficacy; however, additional intervention trials are required to confirm these findings.
Keywords: Enteral nutrition, Nutritional status, Neoplasm, Formula
INTRODUCTION
Cancer is a major cause of mortality in both developing and developed countries, with an estimated 14.1 million new cancer cases and 8 million cancer deaths in 2012 [1]. Nevertheless, early detection and advancements in medical treatment have greatly increased the number of cancer survivors. However, many cancer patients experience malnutrition and significant weight loss due to decreased food intake, emotional stress, and tumor-associated metabolic alterations. The nutritional status of cancer patients is a critical determinant of successful treatment and quality of life (QOL). Cancer therapy-induced adverse events also contribute to malnutrition and delays in cancer therapies and may contribute to cancer deaths in a large proportion of patients [2,3,4,5].
Cancer cachexia occurs in up to 80% of patients [6] and is responsible for 20% of cancer-related deaths [7,8]. A diagnosis of cancer cachexia is made only if at least three of the following 5 criteria are met: decreased muscle strength, fatigue, anorexia, low fat-free mass index, and abnormal biochemistry findings (increased C-reactive protein [CRP] concentration, anemia, and low serum albumin levels), including > 5% weight loss in less than 12 months [9,10]. Tumor-associated development of cancer cachexia is indicated by anorexia and substantial metabolic alteration with respect to carbohydrate, fat, and protein, which increases the risk of severe malnutrition accompanied by the loss of total body mass [11,12]. Major alterations in carbohydrate metabolism include increased gluconeogenesis using amino acids and lactic acid, and insulin resistance [13]. Increased gluconeogenesis accompanies peripheral insulin resistance, resulting in the decreased use of glucose in the muscles and muscle wastage [14]. Recent studies have reported cancer cachexia to be associated with the transformation of white adipose tissue to beige adipocytes through the browning, which upregulates the expression of uncoupling protein 1 (UCP-1), accelerating thermogenesis and energy expenditure [15,16]. Cachexic patients also experience a significant loss of lean body mass due to increased proteolysis and decreased protein synthesis. Blood amino acid concentrations are often decreased, mostly due to accelerated hepatic gluconeogenesis [17].
Cancer therapies, including surgery, chemotherapy, and radiation, are also associated with malnutrition. Surgery-related adverse effects are mostly derived from the surgical removal of cancerous tissue [13]. The most frequent adverse events include difficulties in chewing and swallowing in oral cancer patients; a previous study reported that approximately 50% of oral cancer patients experienced difficulties in ingestion after surgery [18]. Esophageal resection often induces dysphagia, dumping syndrome, and increased defecation. In fact, 80%–90% and 50%–60% of surgical patients exhibit early satiety and reflux, respectively, after food intake [19]. Also, nutrient absorption is decreased due to decreased hormonal and enzymatic activity owing to removal of pancreas [13,20].
Anti-cancer drugs often result in vomiting, mucositis, diarrhea, and dysphagia [21]. Within 24 hours of anti-cancer drug administration, more than 90% of patients complain of nausea and often experience vomiting [22]. Many anti-cancer drugs target not only cancer cells but also other rapidly proliferating normal cells, resulting in adverse events. Many cancer patients undergoing therapy also experience oral mucositis, resulting in difficulties in chewing and swallowing. In cases of gastrointestinal cancers, intestinal mucositis reduces nutrient absorption, leading to malnutrition [2]. Adverse events in radiation therapy are similar to those in chemotherapy, with more than 90% of patients experiencing vomiting [23].
Nutritional support for cancer patients has been achieved by providing high-energy and high-protein nutritional formulas. In recent years, specialized nutritional formulas for cancer patients have been introduced to boost immune regulatory functions and delay muscle degradation. Although the efficacy of oral nutritional interventions remains controversial due to limited evidence, the use of these products to support malnourished cancer patients has grown steadily.
This review has systemically examined the effect of oral nutritional interventions on nutritional and clinical outcomes in cancer patients. We especially focused on outcomes such as nutritional status indices, immune-associated biochemical markers, and QOL assessments to provide insights on their applicability to different outcomes.
MATERIALS AND METHODS
Database search
Research articles describing randomized controlled oral nutritional supplements (ONS) and enteral nutrition (EN) intervention trials to assess their efficacy on nutritional outcomes in cancer patients were retrieved from the Medical Literature Analysis and Retrieval System Online (MEDLINE) and Elsevier database of abstracts and citations (SCOPUS) electronic databases. The search terms included cancer, nutritional intervention, EN, ONS, and randomized controlled trials. Studies published in English between November 2001 and May 2015 were included. Parenteral nutrition intervention studies were excluded.
Study selection
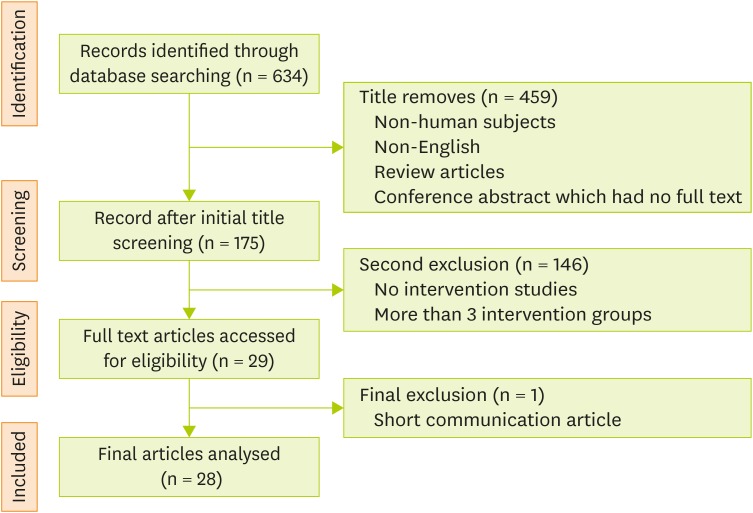
Randomized controlled intervention trials performed in adult oncology patients (> 19 years of age) were selected. The types of treatment (surgery, chemotherapy, radiotherapy or combinations of therapies) and stages or sites of cancer were not considered criteria for study selection. Control groups received usual diet, routine care or placebo ONS. In this review, ONS was defined as a nutritional formula either in liquid or powder form that was used as a supplement. Papers were excluded if they did not describe an original study (Figure 1).
Figure 1.
Flowchart of the article-selection process.
Search strategy and number of trials identified for inclusion in the literature review. The searches were performed between November 2001 and May 2015. The search strategy evolved in line with the changes in information technology and was designed with advice from information specialists. The databases searched in the study included Medical Literature Analysis and Retrieval System Online (MEDLINE), and the Elsevier database of abstracts and citations (SCOPUS).
RESULTS
Study characteristics
A total of 28 studies meeting selection criteria were retrieved. The studies included patients with gastrointestinal cancers and cancer of the lung, head and neck, and liver. Ten studies used ONS with isocaloric or isosource formulas, 11 studies compared ONS with standard formulas, and 7 studies compared ONS with usual diets.
The number of papers by cancer site were: 9 for head and neck, 4 for esophageal, 2 for both head and neck and esophageal, 2 for gastric, 2 for liver, 1 for colon, 1 for gastrointestinal, 2 for both pancreatic and gastric, 1 for both reproductive system and lower intestinal tract, and 2 for lung cancer. Two studies did not specify the cancer sites. A large proportion of studies included patients with gastrointestinal cancers, which indicated that these patients were at a high risk for malnutrition. The types of treatment included surgery (15 studies), chemotherapy (1 study), radiotherapy (5 studies), combined therapies (4 studies), and radiofrequency ablation (1 study). Two studies did not mention the treatment regimen.
Nutritional formulas
All of the ONS used in the selected studies were nutritionally complete supplements. The supplementation routes included oral (12 studies), enteral (14 studies), and both oral and enteral (2 studies). The ONS were either powdered or liquid, and 1 study used ONS in a jelly form. Twenty-two papers described the name of the product and manufacturer: Forticare from Nutricia (2 studies), Nutrison medium-chain triglycerides (MCT) from Nutricia (1 study), Prosure from Abott (4 studies), Impact from Novartis Consumer Health (5 studies), Reconvan from Fresenius Kabi (2 studies), Supportan from Fresenius Kabi (10 studies), Impact from Nestle Healthcare Nutrition (1 study), Impact from Anjimoto (1 study), Aminoleban EN from Otsuka (2 studies), Neomune from Thai Otsuka Pharmaceutical Company (1 study), E028 Extra from SHS International (1 study), and Nutri-jelly from Dental Innovation (1 study). The daily caloric intake from the products varied between 400 and 640 kcal. Most studies, except for three, used nutritional formulas containing functional compounds. Twenty-five studies used ONS or EN products fortified with functional compounds specifically aimed at boosting immune function and preventing tissue loss. The most frequently used compounds were omega-3 fatty acids (n-3 fatty acids, 17 studies) with or without arginine, ribonucleic acid, and glutamine. Arginine was used in 13 studies with or without fiber, n-3 fatty acids, ribonucleic acids, and glutamine.
Outcomes
The intervention outcomes used in selected studies included indices of nutritional status, inflammation, immune responses, and others. The nutritional status indices included anthropometric measures, biochemical measures, dietary assessments, and combinations of two or more indices. The most frequently used indices were serum albumin level, body weight, serum prealbumin level, serum complete blood cell count (CBC), body mass index (BMI), body composition, serum transferrin level, and patient-generated subjective global assessments (PG-SGA) (Table 1). More than half of the studies used serum albumin levels as a measure of nutritional status. Body weight and serum prealbumin levels were used in 16 and 10 studies, respectively.
Table 1. Characteristics and information of the selected studies.
| Ref. | Participants | Control group | EN/ONS | Outcome | ||||
|---|---|---|---|---|---|---|---|---|
| No. | Cancer site | Additional component | Nutrition status | Inflammation & immune | Others | Length of intervention | ||
| [24] | 64 | Esophageal | Isocaloric | Leucine, emulsified fish oil | Body weight, CBC, BMI, ECOG, prealbumin, albumin | PGE2, PBMC (cytokine, PGE2), ConA-stimulated T-lymphocyte proliferation, cytokine, WBC count | Liver & kidney function, PT activity, QOL (EORTC QLQ-C30, OES18, EuroQOL-5D) | 4 weeks |
| [34] | 109 | Gastric | Standard EN | Arginine, n-3 PUFA, RNA, glutamin | Protein, albumin, transferrin | SIRS, postoperative complication, late postoperative period-infectious complication, WBC count | Motality, hospital stay | 7 days |
| [79] | 96 | Liver | Usual diet | BCAA | Body weight, AMC, albumin, total cholesterol, cholinesterase | - | QOL (SF-36) | 2 weeks |
| [80] | 8 | Head & neck | Isosource | Arginine, n-3 PUFA, nucleotides | Pre-illness weight, total body protein, plasma PC fatty acid | TNF-α, IL-6, IL-10, CRP, Ig A, G, M general infections, flap anastomosis complications | Hospital stay | 5 days |
| [30] | 71 | Esophageal | Standard EN | Arginine, n-3 PUFA, glutamine | Body weight | IL-6, IL-10, TNF-α, IFN, CRP, CD3, CD4, CD8, WBC, PMN, lymphocyte count, AE | - | 28 days |
| [81] | 40 | Head & neck | Standard EN | Arginine, n-3 PUFA, RNA | Albumin, prealbumin, fibrinogen | CRP, Il-6, TNF, postoperate complicantion | - | Median 12 days |
| [25] | 66 | Head & neck | Usual diet | - | Presence of symptoms influencing nutritional status, PG-SGA, weight loss | Treatment tolerance | - | Median 100 days |
| [27] | 37 | Head & neck esophageal | Isocaloric | Arginine, n-3 PUFA, RNA | BMI, weight loss, FM, CBC, mGPS, NRI, albumin, plasma antioxidant capacity, AMS, WHO PS | CRP, RCT toxicity | Karnofsky index, QOL (EORTC QLQ-C30, QOL H & N 35) | For 5 days before to the end of the RCT (5–7 weeks) |
| [82] | 50 | Gynaecological, urological or lower gastrointestinal | Usual diet | MCT | Body weight, BMI, dietary assessment | Feacal calprotectin, gastrointestinal toxicity (IBDQ, IBDQ-B, VIQ, RTOG) | - | 3 weeks |
| [26] | 13 | Colorectal | Usual diet | EPA | Body weight, SGA, dietary assessment, protein, total cholesterol | Chemotherapy tolerability | QOL (EORTC QLQ-C30) | 12 weeks |
| [38] | 80 | Head & neck | Usual diet | - | BMI | - | Percentage of tube feeding use, QOL (EORTC QOL H & N 35) | 5–7 weeks |
| [83] | 38 | Non specific | Isocaloric | High in protein, leucine, emulsified fish oil, specific oligosaccharides | CBC, pre-albumin, albumin, calcium, weight | IL-8, IL-1β, IL-6, TNF-α, IFN-γ, IL-10, CRP, PGE2, the ex vivo LPS-stimulated cytokine, PGE2 | Liver & kidney function, thromboplastin time, percentages of EPA and DHA, arachidonic acid of total phospholipid fatty acids of WBC, percentages of EPA and DHA, arachidonic acid, DPA of total phospholipid fatty acids of RBC | 7 days |
| [28] | 40 | Lung | Isocaloric | n-3 PUFA | Handgrip strength, PAM, Karnofsky performance status | - | QOL (EORTC QLQ-C30) | 5 weeks |
| [37] | 229 | Gastrointestinal | Isocaloric | MCT | Prealbumin, albumin, TG, cholesterol | Gastrointestinal problems, postoperative | Hospital stay | At least 5 days |
| [36] | 32 | Head & neck | Standard EN | Arginine | - | - | Survival, second primary tumor, locoregional recurrence | 10 days |
| [84] | 49 | Hepatocellular carcinoma | Usual diet | BCAA | Albumin, CBC, calorie intake | Six events (death, recurrence of HCC, rupture of esophageal varices, and liver failure), tumor markers in blood (AFP, L3-AFP) | Envent free survivla rate, QOL (SF-8), liver & kidney function, prothrombin time, raspiratory rate (npRQ), non-protein respiratory quotient | 12 months |
| [85] | 15 | Head & neck | Standard EN | Arginine, RNA, n-3 PUFA, glutamine | PG-SGA, CBC, albumin, prealbumin, body weight | CRP, WBC, total lymphocyte count, T-lymphocyte subsets, ASEPSIS tool, DTH skin test | - | 7 days |
| [31] | 29 | Esophageal | Standard EN | Arginine, n-3 PUFA, RNA, MCT | CBC, platelet count, plasma nitrate nitrite | IL-6, IL-8, maximum body temperature, PHA-induced lymphocyte transformation tests, T-cell subsets | PT activity, thrombin-antithrombin 3 complex, PIC, hospital stay | 7 days |
| [86] | 25 | Non specific | Standard EN | Fish oil, leucine | - | - | HOMA, FSR, plasma luecine, serum glucose, insulin | 1 day |
| [87] | 40 | Non-small cell lung | Isocaloric | n-3 PUFA (EPA, DHA) | REE, body weight, FFM, MUAC, energy intake, albumin | IL-6, CRP, sTNF-p55, HLA-DR expression on monocytes | EPA, DHA, AA in plasma phospholipids | 5 weeks |
| [88] | 244 | Gastric adenocarcinoma | Usual diet | Arginine, n-3 PUFA, RNA | Prognostic nutritional index, albumin, weight loss | Surgical-site infection, infectious complication, complication SIRS, CRP | Hospital stay | 5 days |
| [35] | 305 | Pancreatic & gastric | Standard EN | Arginine, n-3 PUFA glutamine | CBC, albumin, prealbumin | Postoperative complications, CRP | Morbidity, mortality, hospital stay | 7 days |
| [32] | 72 | Head & neck | Isocaloric | Arginine, fiber | Weight loss, albumin, prealbumin, transferrin | Lyphocytes, postoperative infections complications, local complications, gastrointestinal tolerance | Hospital stay | Minimum 10 days |
| [33] | 47 | Head & neck | Isocaloric | Arginine, fiber | Weight, dietary assesment, albumin, prealbumin, transferrin | Postoperative infection complications, local complecations gastrointestinal tolerance, lymphocyte | Hospital stay, mortality | 22 ± 12 days |
| [89] | 36 | Head & neck | Isocaloric | Arginine, fiber | Albumin, prealbumin, transferrin, body weight | Total No.of lymphocytes, IL-6, TNF-α, CRP | - | Average of 20 days |
| [29] | 111 | Head & neck esophageal | Standard EN | n-3 PUFA | Body cell mass, body weight, BMI, Kondrup score, SGA, handgrip strength, TG | IL-6, TNF-α | QOL (EORTC QLQ-C30) | 14 weeks |
| [90] | 196 | Pancreatic & gastric | Standard EN | - | Prealbumin, albumin, CBC | Postoperative complications, total lymphocyte count | Hospital stay, liver & kidney function | 7 days |
| [91] | 53 | Esophageal | Standard EN | EPA, DHA | Body coposition, albumin | IL-10, IL-8, TNF-α, postoperative complications, body temperature, CRP, IL-6, amyloid A, serum EPA, PBMC membrane EPA | - | 26 days |
Bold words indicates those indices with statistical significance.
MUAC, mid-upper arm circumference; REE, resting energy expenditure; FFM, fat free mass; EN, enteral nutrition; ONS, oral nutritional supplements; PGE2, prostaglandin E2; PBMC, peripheral blood mononuclear cell; WBC, white blood cell; QOL, quality of life; PC, phosphatidylcholine; PMN, polymorphonuclear; PG-SGA, patient-generated subjective global assessments; SGA, subjective global assessments; LPS, lipopolysaccharide; DPA, docosapentaenoic acid; TG, triglyceride; HCC, hepatocellular carcinoma; AFP, alpha-fetoprotein; ASEPSIS, Acronym of Seven Wound Assessment of Tool; DTH, delayed-type hypersensitivity; PHA, phytohemagglutinin; HOMA, insulin resistant; FSR, muscle protein fractional synthesis rate; PIC, alpha 2-plasmin inhibitor-plasmin complex; npRQ, raspiratory rate; PAM, physical activity monitor; IBDQ, Inflammatory Bowel Disease Questionnaire; IBDQ-B, Inflammatory Bowel Disease Questionnaire-Bowel sub-set; VIQ, Vaizey Incontinence Questionnaire; RTOG, radiation therapy oncology group; NRI, nutritional risk index; CBC, complete blood cell count; BMI, body mass index; PT activity, prothrombin activity; SIRS, systemic inflammatory response syndrome; AMC, arm muscle circumference; TNF, tumor necrosis factor; IL, interleukin; Ig, immunoglobulin; AE, adverse effect; CRP, C-reactive protein; FM, fat mass; AMS, arm muscular strength; RCT, radiochemotherapy; SF-8, short form-8 health survey; RNA, ribonucleic acid; EPA, eicosapentaenoic acid; BCAA, branched-chain amino acid; MCT, medium-chain triglyceride; DHA, docosahexaenoic acid; n-3 PUFA, n-3 polyunsaturated fatty acid; ECOG, Eastern Cooperative Oncology Group; WHO PS, World Health Organization Performance Status; AA, arachidonic acid.
Plasma CRP level, complications and infection frequencies, serum interleukin-6 (IL-6) levels, white blood cell (WBC) counts, and serum tumor necrosis factor-alpha (TNF-α) levels were the most frequently used indices of inflammation and immune function. A total of 11 studies used plasma CRP and another 11 studies measured the frequencies of complication or infection. Four studies used WBC counts, nine studies used serum IL-6 level, and eight studies used serum TNF-α levels. Patient QOL were assessed in 9 studies by the period of hospital stay, eight studies as QOL score, and 4 studies used either mortality or survival rates.
Efficacy
1) Nutritional status
Eleven of 28 studies showed that nutritional intervention improved nutritional status indices, especially body weight, performance status scores, and body composition. A four-week intervention in esophageal cancer patients administered ONS containing leucine and fish oil significantly improved body weight change (p < 0.05) and Eastern Cooperative Oncology Group (ECOG) score (p < 0.05) [24]. Similarly, nutritional intervention significantly reduced weight loss in head and neck cancer patients (p = 0.024) [25]. Increased body weight gain was observed in colon cancer patients after 12 weeks of nutritional intervention with ONS containing eicosapentaenoic acid (EPA) compared to that of the control patients (4.94 vs. −1.17; p = 0.045) [26]. Head and neck cancer patients in intervention groups showed improved World Health Organization Performance Status (WHO PS) scores (1.00 ± 0.41 vs. 1.67 ± 0.72; p < 0.05), and fat mass loss (−0.6 ± 0.9 vs. 0.7 ± 1.3 kg; p < 0.05) [27]. Another study involving lung cancer patients showed that five weeks of nutritional intervention improved Karnofsky performance scores (p = 0.04) [28]. A 14-week intervention trial involving head and neck and esophageal cancer patients improved Kondrup scores only in the experimental group and not in the control group (p < 0.05) [29].
2) Inflammation and immune function indices
One or more indices of inflammation and immune function, especially infections, complications, plasma CRP levels, and serum cytokine levels, improved in 65% of the selected studies. Treatment-induced increases in plasma CRP and inflammatory cytokine concentrations were significantly lowered by nutritional intervention [30]. Increases in plasma CRP and TNF-α concentrations in esophageal cancer patients were significantly lowered by four weeks of EN supplementation, which contained arginine, n-3 fatty acid, and glutamine. Patients who received EN containing arginine, n-3 fatty acid, ribonucleic acid, and MCT showed lower serum IL-8 concentration compared to that in the control patients [31]. ONS containing leucine, and fish oil resulted in decreased serum prostaglandin E2 (PGE2) concentrations [24].
3) Other measures and indices
Control group patients had significantly more unplanned hospital admissions during the treatment period compared with the experimental group (p < 0.05) [32,33]. Statistical differences were detected in local complications and fistulas diagnosed by X-ray were less frequent in the experimental group (5.2% experimental group vs. 17.6% control group; p = 0.026). Systemic inflammatory response syndrome (SIRS) disappeared faster and complications were lower in gastric cancer patients who received 1 week of nutrition compared to those in control group patients. The duration of SIRS in the experimental group (1.10 ± 0.89 days) was significantly shorter than that in the control group (2.20 ± 1.02 days; p = 0.036) [34]. Nutrition intervention with EN included arginine, n-3 fatty acid, and glutamine administered for one week decreased infection-associated complications and mortality in pancreatic and gastric cancer patients [35]. Infectious complications were observed in 60 patients (39.2%) in the control group and 43 (28.3%) in the experimental group (p = 0.04). Differences were also observed in overall morbidity (47.1% vs. 33.5%; p = 0.01) and mortality (5.9% vs. 1.3%, p = 0.03)
Twelve of the 28 studies showed significant improvement in other indices, including QOL, survival, and length of hospital stay. In a 10-year follow-up after 10 days of post- or perioperative arginine-containing EN intervention in head and neck cancer patients, the intervention group showed a higher median survival rate (p = 0.019) [36]. In other studies, nutritional intervention reduced the length of hospital stay in head and neck [32,33] and gastrointestinal cancer patients [34,35,37]. The length of postoperative stay was 24.3 ± 14.0 days in the experimental group (EN with arginine and fiber) compared to 36.1 ± 27.0 days in the control group (p = 0.036) [32].
QOL measurements in head and neck cancer patients improved in the intervention group compared to those of the control group. Nutritional supplementation also significantly improved social functions of colon cancer patients and physical function, cognitive function, and social function in lung cancer patients [28]. After receiving radiotherapy, the overall health-related QOL score in the experimental group was significantly higher than that of the control group (no intervention) (p < 0.001) The intervention group (ONS containing leucine and fish oil) showed significantly better global health status (B = 12.2, p = 0.04), physical function (B = 5.3, p = 0.04), cognitive function (B = 20.7, p < 0.01), and social function (B = 22.1, p = 0.04) on the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire (EORTC-QLQC30) subscales than the control group (B is the difference between the intervention and control groups) [28].
DISCUSSION
The main objective of this review was to evaluate the efficacy of ONS and EN in malnourished cancer patients based on a systematic review of recent randomized, controlled nutrition intervention trials. Despite substantial research efforts on cancer treatment, advancements in nutritional support to improve patient QOL and increase treatment efficacy are limited. In this study, we found that ONS- or EN-based nutritional intervention can significantly improve indices of nutrition status, immune functions, and QOL despite a large variability in outcome measures. Additionally, cancer treatment-associated increases in inflammatory response could be alleviated through better nutritional management. Due to the complicated nature of the disease and frequent adverse events due to treatment, nutritional intervention studies in cancer patients have been extremely difficult, especially with high dropout rates. Substantial variabilities in biomarkers caused by site specificity, different treatment protocols, and disease stages also affect the intervention results.
We found that the indices used to measure the efficacy of nutritional interventions have been expanded in recent studies compared to those in previous years. The classic indices of nutritional status in malnourished patients include body weight and serum albumin levels. We found that 48.3% and 58.6% of the collected studies assessed body weight and serum albumin levels, respectively. Among those, only 28.6% and 11.8% of the studies reported improvements. Albumin has a relatively long half-life (14 to 20 days) and has been used to reflect chronic nutritional status [39]. Although albumin has been associated with death rate and duration of hospitalization [40], non-nutritional factors including iron deficiency, estrogen, chronic blood loss, and age affect circulating concentrations of albumin [41] indicating albumin alone might not be an accurate marker of nutritional status [42].
Body weight in combination with albumin and other blood markers has been widely used to assess the nutritional status of cancer patients. It has been suggested that body weight is a key measure to assess not only malnutrition but also the risk of adverse events associated with cancer treatments. In recent clinical practice, serum triglyceride (TG) and cholesterol levels are used as markers of cachexia [44]. Cholesterol has been proposed to alleviate tissue inflammatory responses associated with cancer [45], which might be related to the development of cachexia leading to malnutrition.
Although PG-SGA and nutritional risk index (NRI) are ideal assessment methods to evaluate nutritional status, they were not commonly used in the studies included in this review. PG-SGA is a standard nutritional assessment tool recommended by the Oncology Nutrition Dietetic Practice Group of the American Dietetic Association and Oncology Nursing Society [46]. Although PG-SGA scores are determined based on changes in body weight, dietary intake, and physical symptoms, the assessment itself requires highly trained medical staff and well-established guidelines. Therefore, patient PG-SGA scores often differ when measured by different medical staff; in addition, not enough personnel are available in clinical settings [47]. Other nutritional assessment tools include the Malnutrition Universal Screening Tool (MUST), Prognostic Nutritional Index, NRI, Nutritional Screening Tool, Maastricht Index, Instant Nutrition Assessment, and Mini Nutritional Assessment.
The most significant adverse effect of cancer treatment is cytotoxicity in rapidly proliferating normal cells, including epithelial and immune cells, making patients vulnerable to mucositis and infections. Both chemotherapy and radiotherapy accelerate inflammatory responses, which are also related to mucositis and infections. Proinflammatory cytokines and other markers of inflammation are often elevated in patients undergoing cancer therapy. Surgical patients with colon cancer have higher concentrations of IL-6 and IL-10 [48]. Also, patients with prostate cancer who receive radiotherapy have elevated concentrations of IL-6 [49]. The markers of inflammatory responses used in the studies in this review include CRP (11 studies), amyloid A (1 study), TNF-µ (8 studies), IL-6 (9 studies), IL-10 (4 studies), IL-8 (3 studies), interferon-γ (2 studies), IL-1µ (1 study), and PGE2 (2 studies). However, most of the studies did not find significant differences in the concentrations of serum inflammatory markers, possibly due to wide concentration variations, indicating the serum markers of inflammation may not accurately reflect the efficacy of nutritional interventions.
The most frequently used indices of immune function the selected studies were WBC counts (4 studies), total lymphocyte counts (6 studies), T-cell subset populations (4 studies) and adverse events including infections and complications (10 studies), treatment toxicity (6 studies), and other adverse effects (2 studies). Among these indices, T-cell subset populations and events reflecting infections and complications responded relatively well to nutritional intervention.
QOL measures are clinically meaningful indices to determine the efficacy of nutritional interventions in cancer patients. Only eight of the 28 studies used QOL questionnaires as an intervention outcome, and 75% showed positive results with nutritional intervention. A meta-analysis on the efficacy of ONS in malnourished cancer patients indicated that nutritional interventions can improve QOL; however, its effects on survival, body weight, and energy intake are inconsistent [50]. With gradually increasing cancer survival rates, QOL is a valuable intervention outcome of many types of cancer, although QOL assessment results have been rarely applied in clinical settings due to large differences in clinical interpretation of QOL. Recently, however, guidelines for interpreting changes in EORTC QLQ-30 scores have been proposed [51], which includes 5 functional scales (physical, role, emotional, cognitive, and social), three symptom scales (fatigue, nausea and vomiting, and pain), and a global health status/QOL.
As shown in Table 2, many ONS and EN products used in intervention trials contain functional compounds to improve reduced immune function and increased inflammatory responses. N-3 fatty acids, either as fish oil or long-chain fatty acids (EPA and docosahexaenoic acid [DHA]), were the most frequently used immunonutrient components. The use of fish oil as an alternative lipid source in surgical and critically ill patients has been routinely suggested. Long-chain n-3 fatty acids such as EPA and DHA are easily incorporated into cell membranes, altering the properties, followed by accelerated cellular signal transduction pathways. Additionally, eicosanoids synthesized from n-3 fatty acids exert anti-inflammatory effects, while those from n-6 fatty acids accelerate inflammatory responses. Among ONS provided in these 28 studies, 19 studies (68%) contained n-3 fatty acids or fish oil; 9 studies indicated that the intervention suppressed inflammatory responses. An extensive review of nutrition intervention studies in postsurgical and critically ill patients indicated that the use of fish oil in surgical and critically ill patients has not been proven to be beneficial, possibly due to the limited number of studies [52]. However, the use of fish oil in combination with other functional components such as arginine and antioxidants may improve the nutritional status of postsurgical and critically ill patients, respectively. Recent studies have also indicated that long-chain n-3 fatty acid supplementation may exert detrimental effects in acute infections [53], implying that caution may be required in immunosuppressed patients.
Table 2. Frequency of outcomes analyzed in the selected studies.
| Outcome | Reference | ||
|---|---|---|---|
| Nutrition status | |||
| Anthropometry | Body weight | [24,25,26,27,29,30,32,33,79,80,82,83,85,87,88,89] | |
| Body composition | [27,29,87,91] | ||
| Arm muscle circumference | [79,87] | ||
| BMI | [24,27,29,38,82] | ||
| Handgrip strength | [28,29] | ||
| Biochemical | CBC | [24,27,31,35,83,84,85,90] | |
| Protein | [26,34,80] | ||
| Albumin | [24,27,32,33,34,35,37,79,81,83,84,85,87,88,89,90,91] | ||
| Prealbumin | [24,32,33,35,37,81,83,85,89,90] | ||
| Fibrinogen | [81] | ||
| Transferrin | [32,33,34,89] | ||
| Total cholesterol | [26,37,79] | ||
| Triglyceride | [29,37] | ||
| Dietary assessment | [26,33,82,84,87] | ||
| Assessment tool | Kondrup score | [29] | |
| ECOG performance status | [24] | ||
| Karnofsky performance status | [28] | ||
| WHO PS | [27] | ||
| PG-SGA | [25,26,29,85] | ||
| NRI | [27] | ||
| Inflammation & immune | |||
| Biochemical | CRP | [27,30,35,80,81,83,85,87,88,89,91] | |
| Amyloid A | [91] | ||
| TNF-alpha | [29,30,80,81,83,87,89,91] | ||
| IL-6 | [29,30,31,80,81,83,87,89,91] | ||
| IL-10 | [30,80,83,91] | ||
| IL-8 | [31,83,91] | ||
| interferon gamma | [30,83] | ||
| IL-1beta | [83] | ||
| WBC count | [24,30,34,85] | ||
| Total lymphocyte count | [30,32,33,85,89,90] | ||
| T-cell subsets | [24,30,31,85] | ||
| Feacal calprotection | [82] | ||
| PGE2 | [24,83] | ||
| Immunoglobulin A, G, and M | [80] | ||
| Others | Complication & infection | [32,33,34,35,37,80,81,88,90,91] | |
| Treatment toxicity | [25,26,27,32,33,82] | ||
| Adverse effect | [30,84] | ||
| Maximum body temperature | [31,91] | ||
| Others | |||
| QOL | [24,26,27,28,29,38,79,84] | ||
| Motality & survival | [33,34,35,36] | ||
| Length of hospital stay | [31,32,33,34,35,37,80,88,90] | ||
BMI, body mass index; CBC, complete blood cell count; ECOG, Eastern Cooperative Oncology Group; PG-SGA, patient-generated subjective global assessment; CRP, C-reactive protein; QOL, quality of life; WHO PS, World Health Organization Performance Status; NRI, nutritional risk index; TNF, tumor necrosis factor; IL, interleukin; WBC, white blood cell; PGE2, prostaglandin E2.
Cachexia is accelerated by increased concentrations of inflammatory cytokines and is associated with accelerated immune response [54]. In particular, TNF-α, IL-6, IL-1, and interferon-γ have been shown to evoke cancer cachexia [55]. TNF-α, a cachectin, stimulates other secondary cytokines produced in monocytes and macrophages, including IL-1β, IL-6, and IL-8 [56]. TNF- accelerates muscle wasting, anorexia, and fatigue. Increased IL-1β concentration is associated with cachexia progress and anorexia development [57]. IL-6 also produced in cancer cells [58] possibly worsening cachexia. The activated leukocytes are responsible for the production of pro-inflammatory molecules including eicosanoids, inflammatory cytokines, reactive oxygen species, and platelet-activating factors [59]. A previous study showed that DHA- and EPA-rich fish oil supplementation significantly reduced secretion of IL-1β, IL-6, and granulocyte colony-stimulating factor from lipopolysaccharide-stimulated peripheral blood mononuclear cells [60]. A recent mechanistic study showed that dendritic cells exposed to arachidonic acid and DHA reduced T helper cell, which may explain their anti-inflammatory activities [61]. Long chain n-3 polyunsaturated fatty acids (PUFAs) also suppress the nuclear factor kappa-B (NF-κB) signaling pathway, thereby decreasing macrophage production of pro-inflammatory cytokines [62]. In this review, 9 of the 18 studies that used ONS containing fish oil or n-3 fatty acids reported improvements in inflammatory markers.
Arginine was used in 14 studies. It is an important immune regulatory basic amino acid [63] involved in the production of nitric oxide associated with innate immunity [64]. Serum arginine concentration is decreased in cancer patients [65]. Tumor-associated arginine deprivation plays a central role in T-cell-mediated anti-tumor activity [66].
Nucleotides exert immune-stimulatory effects [67]. Preclinical studies have shown that nucleotides, ribonucleotides, and nucleic acids stimulate Th1 and Th2 responses [68,69,70] Nucleotides also accelerate the production of IL-7 in primary cultured murine intestinal epithelial cells promoting intestinal immune function [71].
Among selected studies, 2 studies involving liver cancer patients used branched-chain amino acid (BCAA) including leucine, isoleucine, and valine. Hepatocyte growth factor (HGF) stimulates the proliferation and functions of hepatocytes, and BCAA induces HGF production in the liver [71]. BCAA supplemental therapy has also been used to prevent progressive liver failure [72].
Glutamine has been shown to exert mucosal preservation and immune-stimulatory effects. Extracellular glutamine stimulates the proliferation of T-lymphocytes [73]. Cancer cells have higher glutaminase activity to convert more glutamine to glutamic acids [74,75]. Glutamine supplementation also alleviates cancer treatment-induced mucositis by stimulating rapid epithelial cell production [76,77].
These results indicate that several functional components such as n-3 fatty acids, arginine, nucleotides and glutamine may be best used in medical foods for cancer patients despite the variabilities in study settings. Most of the studies used ONS containing more than one functional component and showed improvement in at least one or more markers. Although it is difficult to determine the independent effects of these functional components, commercial products use these compounds to accelerate the efficacy of ONS, which will benefit the patient. Further clinical trials are required to determine the efficacy of individual component although the European Society for Clinical Nutrition and Metabolism (ESPEN) guidelines on nutrition in cancer patients suggested that nutrition intervention in cancer patients exerts a moderate degree of efficacy.
A major limitation of this review is the small number of intervention studies. In addition, the studies used different groups of cancer patients with different cancer sites and treatment protocols, which may affect the efficacy of nutritional interventions (less than one month), which might not be sufficient to show the effects of the intervention. Additionally, the control groups used in each study were defined differently (7 studies used usual care, 11 studies used standard EN or ONS, and 10 studies used placebo controls), which may have affected the study results.
CONCLUSION
Despite its limitations, the results of this review suggest that nutritional intervention improves the indices of nutritional status, inflammation, immune function, and QOL. Nutritional status indices, QOL measures and duration of hospital stay were improved in about 40% of studies. One or more markers of immune function and inflammatory responses were improved by ONS in 65% of selected studies. Based on the reported mechanistic insights on malnutrition in cancer patients, nutritional formulas containing extra functional components should be considered for further development. Further studies in homogeneous subsets of cancer patients with more specific indices are required to minimize the variation in intervention studies.
Footnotes
Funding: This work was supported by the SRC program (Center for Food and Nutritional Genomics: No.2015R1A5A6001906) of the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science, and Technology.
Conflict of Interest: The authors declare that they have no competing interests.
Author Contributions: Jin-Min Kim contributued to the search of the relevant literatures and the arrangement of the information; Mi-Kyung Sung contributed to the conceptualization and the writing of the manuscrirpt.
References
- 1.Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136:E359–86. doi: 10.1002/ijc.29210. [DOI] [PubMed] [Google Scholar]
- 2.Santarpia L, Contaldo F, Pasanisi F. Nutritional screening and early treatment of malnutrition in cancer patients. J Cachexia Sarcopenia Muscle. 2011;2:27–35. doi: 10.1007/s13539-011-0022-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Macciò A, Madeddu C, Gramignano G, Mulas C, Floris C, Sanna E, Cau MC, Panzone F, Mantovani G. A randomized phase III clinical trial of a combined treatment for cachexia in patients with gynecological cancers: evaluating the impact on metabolic and inflammatory profiles and quality of life. Gynecol Oncol. 2012;124:417–425. doi: 10.1016/j.ygyno.2011.12.435. [DOI] [PubMed] [Google Scholar]
- 4.Van Cutsem E, Arends J. The causes and consequences of cancer-associated malnutrition. Eur J Oncol Nurs. 2005;9(Suppl 2):S51–63. doi: 10.1016/j.ejon.2005.09.007. [DOI] [PubMed] [Google Scholar]
- 5.Caccialanza R, Pedrazzoli P, Cereda E, Gavazzi C, Pinto C, Paccagnella A, Beretta GD, Nardi M, Laviano A, Zagonel V. Nutritional support in cancer patients: a position paper from the Italian Society of Medical Oncology (AIOM) and the Italian Society of Artificial Nutrition and Metabolism (SINPE) J Cancer. 2016;7:131–135. doi: 10.7150/jca.13818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fearon KC, Glass DJ, Guttridge DC. Cancer cachexia: mediators, signaling, and metabolic pathways. Cell Metab. 2012;16:153–166. doi: 10.1016/j.cmet.2012.06.011. [DOI] [PubMed] [Google Scholar]
- 7.Melstrom LG, Melstrom KA, Jr, Ding XZ, Adrian TE. Mechanisms of skeletal muscle degradation and its therapy in cancer cachexia. Histol Histopathol. 2007;22:805–814. doi: 10.14670/HH-22.805. [DOI] [PubMed] [Google Scholar]
- 8.Palesty JA, Dudrick SJ. What we have learned about cachexia in gastrointestinal cancer. Dig Dis. 2003;21:198–213. doi: 10.1159/000073337. [DOI] [PubMed] [Google Scholar]
- 9.Muscaritoli M, Anker SD, Argilés J, Aversa Z, Bauer JM, Biolo G, Boirie Y, Bosaeus I, Cederholm T, Costelli P, Fearon KC, Laviano A, Maggio M, Rossi Fanelli F, Schneider SM, Schols A, Sieber CC. Consensus definition of sarcopenia, cachexia and pre-cachexia: joint document elaborated by Special Interest Groups (SIG) “cachexia-anorexia in chronic wasting diseases” and “nutrition in geriatrics”. Clin Nutr. 2010;29:154–159. doi: 10.1016/j.clnu.2009.12.004. [DOI] [PubMed] [Google Scholar]
- 10.Evans WJ, Morley JE, Argilés J, Bales C, Baracos V, Guttridge D, Jatoi A, Kalantar-Zadeh K, Lochs H, Mantovani G, Marks D, Mitch WE, Muscaritoli M, Najand A, Ponikowski P, Rossi Fanelli F, Schambelan M, Schols A, Schuster M, Thomas D, Wolfe R, Anker SD. Cachexia: a new definition. Clin Nutr. 2008;27:793–799. doi: 10.1016/j.clnu.2008.06.013. [DOI] [PubMed] [Google Scholar]
- 11.Johns N, Stephens NA, Fearon KC. Muscle wasting in cancer. Int J Biochem Cell Biol. 2013;45:2215–2229. doi: 10.1016/j.biocel.2013.05.032. [DOI] [PubMed] [Google Scholar]
- 12.Bozzetti F. Nutritional support of the oncology patient. Crit Rev Oncol Hematol. 2013;87:172–200. doi: 10.1016/j.critrevonc.2013.03.006. [DOI] [PubMed] [Google Scholar]
- 13.Nicolini A, Ferrari P, Masoni MC, Fini M, Pagani S, Giampietro O, Carpi A. Malnutrition, anorexia and cachexia in cancer patients: A mini-review on pathogenesis and treatment. Biomed Pharmacother. 2013;67:807–817. doi: 10.1016/j.biopha.2013.08.005. [DOI] [PubMed] [Google Scholar]
- 14.Argilés JM, Busquets S, Stemmler B, López-Soriano FJ. Cancer cachexia: understanding the molecular basis. Nat Rev Cancer. 2014;14:754–762. doi: 10.1038/nrc3829. [DOI] [PubMed] [Google Scholar]
- 15.Petruzzelli M, Schweiger M, Schreiber R, Campos-Olivas R, Tsoli M, Allen J, Swarbrick M, Rose-John S, Rincon M, Robertson G, Zechner R, Wagner EF. A switch from white to brown fat increases energy expenditure in cancer-associated cachexia. Cell Metab. 2014;20:433–447. doi: 10.1016/j.cmet.2014.06.011. [DOI] [PubMed] [Google Scholar]
- 16.Kir S, White JP, Kleiner S, Kazak L, Cohen P, Baracos VE, Spiegelman BM. Tumour-derived PTH-related protein triggers adipose tissue browning and cancer cachexia. Nature. 2014;513:100–104. doi: 10.1038/nature13528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Porporato PE. Understanding cachexia as a cancer metabolism syndrome. Oncogenesis. 2016;5:e200. doi: 10.1038/oncsis.2016.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kazi R, Kanagalingam J, Al-Mutairy A, Nutting CM, Clarke P, Rhys-Evans PH, Harrington KJ. Predictors of speech and swallowing function following primary surgery for oral and oropharyngeal cancer. Clin Otolaryngol. 2006;31:83. doi: 10.1111/j.1749-4486.2006.01145.x. [DOI] [PubMed] [Google Scholar]
- 19.Haverkort EB, Binnekade JM, Busch OR, van Berge Henegouwen MI, de Haan RJ, Gouma DJ. Presence and persistence of nutrition-related symptoms during the first year following esophagectomy with gastric tube reconstruction in clinically disease-free patients. World J Surg. 2010;34:2844–2852. doi: 10.1007/s00268-010-0786-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ryan AM, Healy LA, Power DG, Rowley SP, Reynolds JV. Short-term nutritional implications of total gastrectomy for malignancy, and the impact of parenteral nutritional support. Clin Nutr. 2007;26:718–727. doi: 10.1016/j.clnu.2007.08.013. [DOI] [PubMed] [Google Scholar]
- 21.Bhosle J, Hall J. Principles of cancer treatment by chemotherapy. Surgery. 2006;24:66–69. [Google Scholar]
- 22.Faria C, Li X, Nagl N, McBride A. Outcomes associated with 5-HT3-RA therapy selection in patients with chemotherapy-induced nausea and vomiting: a retrospective claims analysis. Am Health Drug Benefits. 2014;7:50–58. [PMC free article] [PubMed] [Google Scholar]
- 23.Maranzano E, De Angelis V, Pergolizzi S, Lupattelli M, Frata P, Spagnesi S, Frisio ML, Mandoliti G, Malinverni G, Trippa F, Fabbietti L, Parisi S, Di Palma A, De Vecchi P, De Renzis C, Giorgetti C, Bergami T, Orecchia R, Portaluri M, Signor M, Di Gennaro D, Italian Group for Antiemetic Research in Radiotherapy - IGARR A prospective observational trial on emesis in radiotherapy: analysis of 1020 patients recruited in 45 Italian radiation oncology centres. Radiother Oncol. 2010;94:36–41. doi: 10.1016/j.radonc.2009.11.001. [DOI] [PubMed] [Google Scholar]
- 24.Faber J, Uitdehaag MJ, Spaander M, van Steenbergen-Langeveld S, Vos P, Berkhout M, Lamers C, Rümke H, Tilanus H, Siersema P, van Helvoort A, van der Gaast A. Improved body weight and performance status and reduced serum PGE2 levels after nutritional intervention with a specific medical food in newly diagnosed patients with esophageal cancer or adenocarcinoma of the gastro-esophageal junction. J Cachexia Sarcopenia Muscle. 2015;6:32–44. doi: 10.1002/jcsm.12009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Paccagnella A, Morello M, Da Mosto MC, Baruffi C, Marcon ML, Gava A, Baggio V, Lamon S, Babare R, Rosti G, Giometto M, Boscolo-Rizzo P, Kiwanuka E, Tessarin M, Caregaro L, Marchiori C. Early nutritional intervention improves treatment tolerance and outcomes in head and neck cancer patients undergoing concurrent chemoradiotherapy. Support Care Cancer. 2010;18:837–845. doi: 10.1007/s00520-009-0717-0. [DOI] [PubMed] [Google Scholar]
- 26.Trabal J, Leyes P, Forga M, Maurel J. Potential usefulness of an EPA-enriched nutritional supplement on chemotherapy tolerability in cancer patients without overt malnutrition. Nutr Hosp. 2010;25:736–740. [PubMed] [Google Scholar]
- 27.Vasson MP, Talvas J, Perche O, Dillies AF, Bachmann P, Pezet D, Achim AC, Pommier P, Racadot S, Weber A, Ramdani M, Kwiatkowski F, Bouteloup C. Immunonutrition improves functional capacities in head and neck and esophageal cancer patients undergoing radiochemotherapy: a randomized clinical trial. Clin Nutr. 2014;33:204–210. doi: 10.1016/j.clnu.2013.06.008. [DOI] [PubMed] [Google Scholar]
- 28.van der Meij BS, Langius JA, Spreeuwenberg MD, Slootmaker SM, Paul MA, Smit EF, van Leeuwen PA. Oral nutritional supplements containing n-3 polyunsaturated fatty acids affect quality of life and functional status in lung cancer patients during multimodality treatment: an RCT. Eur J Clin Nutr. 2012;66:399–404. doi: 10.1038/ejcn.2011.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fietkau R, Lewitzki V, Kuhnt T, Hölscher T, Hess CF, Berger B, Wiegel T, Rödel C, Niewald M, Hermann RM, Lubgan D. A disease-specific enteral nutrition formula improves nutritional status and functional performance in patients with head and neck and esophageal cancer undergoing chemoradiotherapy: results of a randomized, controlled, multicenter trial. Cancer. 2013;119:3343–3353. doi: 10.1002/cncr.28197. [DOI] [PubMed] [Google Scholar]
- 30.Sunpaweravong S, Puttawibul P, Ruangsin S, Laohawiriyakamol S, Sunpaweravong P, Sangthawan D, Pradutkanchana J, Raungkhajorn P, Geater A. Randomized study of antiinflammatory and immune-modulatory effects of enteral immunonutrition during concurrent chemoradiotherapy for esophageal cancer. Nutr Cancer. 2014;66:1–5. doi: 10.1080/01635581.2014.847473. [DOI] [PubMed] [Google Scholar]
- 31.Aiko S, Yoshizumi Y, Ishizuka T, Horio T, Sakano T, Kumano I, Kanai N, Maehara T. Enteral immuno-enhanced diets with arginine are safe and beneficial for patients early after esophageal cancer surgery. Dis Esophagus. 2008;21:619–627. doi: 10.1111/j.1442-2050.2008.00827.x. [DOI] [PubMed] [Google Scholar]
- 32.De Luis DA, Izaola O, Cuellar L, Terroba MC, Martin T, Aller R. High dose of arginine enhanced enteral nutrition in postsurgical head and neck cancer patients. A randomized clinical trial. Eur Rev Med Pharmacol Sci. 2009;13:279–283. [PubMed] [Google Scholar]
- 33.de Luis DA, Aller R, Izaola O, Cuellar L, Terroba MC. Postsurgery enteral nutrition in head and neck cancer patients. Eur J Clin Nutr. 2002;56:1126–1129. doi: 10.1038/sj.ejcn.1601458. [DOI] [PubMed] [Google Scholar]
- 34.Marano L, Porfidia R, Pezzella M, Grassia M, Petrillo M, Esposito G, Braccio B, Gallo P, Boccardi V, Cosenza A, Izzo G, Di Martino N. Clinical and immunological impact of early postoperative enteral immunonutrition after total gastrectomy in gastric cancer patients: a prospective randomized study. Ann Surg Oncol. 2013;20:3912–3918. doi: 10.1245/s10434-013-3088-1. [DOI] [PubMed] [Google Scholar]
- 35.Klek S, Sierzega M, Szybinski P, Szczepanek K, Scislo L, Walewska E, Kulig J. The immunomodulating enteral nutrition in malnourished surgical patients - a prospective, randomized, double-blind clinical trial. Clin Nutr. 2011;30:282–288. doi: 10.1016/j.clnu.2010.10.001. [DOI] [PubMed] [Google Scholar]
- 36.Buijs N, van Bokhorst-de van der Schueren MA, Langius JA, Leemans CR, Kuik DJ, Vermeulen MA, van Leeuwen PA. Perioperative arginine-supplemented nutrition in malnourished patients with head and neck cancer improves long-term survival. Am J Clin Nutr. 2010;92:1151–1156. doi: 10.3945/ajcn.2010.29532. [DOI] [PubMed] [Google Scholar]
- 37.Wang X, Pan L, Zhang P, Liu X, Wu G, Wang Y, Liu Y, Li N, Li J. Enteral nutrition improves clinical outcome and shortens hospital stay after cancer surgery. J Invest Surg. 2010;23:309–313. doi: 10.3109/08941939.2010.519428. [DOI] [PubMed] [Google Scholar]
- 38.Trachootham D, Songkaew W, Hongsachum B, Wattana C, Changkluengdee N, Karapoch J, Thirdsuttironnapumi S, Meennuch E, Klaitong C, Sinthusek T, Lam-ubol A. Nutri-jelly may improve quality of life and decrease tube feeding demand in head and neck cancer patients. Support Care Cancer. 2015;23:1421–1430. doi: 10.1007/s00520-014-2488-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Liumbruno GM, Bennardello F, Lattanzio A, Piccoli P, Rossettias G, Italian Society of Transfusion Medicine and Immunohaematology (SIMTI) Recommendations for the use of albumin and immunoglobulins. Blood Transfus. 2009;7:216–234. doi: 10.2450/2009.0094-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pupim LB, Cuppari L, Ikizler TA. Nutrition and metabolism in kidney disease. Semin Nephrol. 2006;26:134–157. doi: 10.1016/j.semnephrol.2005.09.010. [DOI] [PubMed] [Google Scholar]
- 41.Banh L. Serum proteins as markers of nutrition: what are we treating? Pract Gastroenterol. 2006;30:46–64. [Google Scholar]
- 42.Friedman AN, Fadem SZ. Reassessment of albumin as a nutritional marker in kidney disease. J Am Soc Nephrol. 2010;21:223–230. doi: 10.1681/ASN.2009020213. [DOI] [PubMed] [Google Scholar]
- 43.Aoyama T, Yoshikawa T, Shirai J, Hayashi T, Yamada T, Tsuchida K, Hasegawa S, Cho H, Yukawa N, Oshima T, Rino Y, Masuda M, Tsuburaya A. Body weight loss after surgery is an independent risk factor for continuation of S-1 adjuvant chemotherapy for gastric cancer. Ann Surg Oncol. 2013;20:2000–2006. doi: 10.1245/s10434-012-2776-6. [DOI] [PubMed] [Google Scholar]
- 44.Chawda JG, Jain SS, Patel HR, Chaduvula N, Patel K. The relationship between serum lipid levels and the risk of oral cancer. Indian J Med Paediatr Oncol. 2011;32:34–37. doi: 10.4103/0971-5851.81888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rauchhaus M, Coats AJ, Anker SD. The endotoxin-lipoprotein hypothesis. Lancet. 2000;356:930–933. doi: 10.1016/S0140-6736(00)02690-8. [DOI] [PubMed] [Google Scholar]
- 46.Vigano AL, di Tomasso J, Kilgour RD, Trutschnigg B, Lucar E, Morais JA, Borod M. The abridged patient-generated subjective global assessment is a useful tool for early detection and characterization of cancer cachexia. J Acad Nutr Diet. 2014;114:1088–1098. doi: 10.1016/j.jand.2013.09.027. [DOI] [PubMed] [Google Scholar]
- 47.Boléo-Tomé C, Monteiro-Grillo I, Camilo M, Ravasco P. Validation of the malnutrition universal screening tool (MUST) in cancer. Br J Nutr. 2012;108:343–348. doi: 10.1017/S000711451100571X. [DOI] [PubMed] [Google Scholar]
- 48.Galizia G, Orditura M, Romano C, Lieto E, Castellano P, Pelosio L, Imperatore V, Catalano G, Pignatelli C, De Vita F. Prognostic significance of circulating IL-10 and IL-6 serum levels in colon cancer patients undergoing surgery. Clin Immunol. 2002;102:169–178. doi: 10.1006/clim.2001.5163. [DOI] [PubMed] [Google Scholar]
- 49.Lopes CO, Callera F. Three-dimensional conformal radiotherapy in prostate cancer patients: rise in interleukin 6 (IL-6) but not IL-2, IL-4, IL-5, tumor necrosis factor-α, MIP-1-α, and LIF levels. Int J Radiat Oncol Biol Phys. 2012;82:1385–1388. doi: 10.1016/j.ijrobp.2011.04.040. [DOI] [PubMed] [Google Scholar]
- 50.Baldwin C, Spiro A, Ahern R, Emery PW. Oral nutritional interventions in malnourished patients with cancer: a systematic review and meta-analysis. J Natl Cancer Inst. 2012;104:371–385. doi: 10.1093/jnci/djr556. [DOI] [PubMed] [Google Scholar]
- 51.Cocks K, King MT, Velikova G, de Castro G, Jr, Martyn St-James M, Fayers PM, Brown JM. Evidence-based guidelines for interpreting change scores for the European Organisation for the Research and Treatment of Cancer Quality of Life Questionnaire Core 30. Eur J Cancer. 2012;48:1713–1721. doi: 10.1016/j.ejca.2012.02.059. [DOI] [PubMed] [Google Scholar]
- 52.Calder PC. Rationale and use of n-3 fatty acids in artificial nutrition. Proc Nutr Soc. 2010;69:565–573. doi: 10.1017/S0029665110000157. [DOI] [PubMed] [Google Scholar]
- 53.Fenton JI, Hord NG, Ghosh S, Gurzell EA. Immunomodulation by dietary long chain omega-3 fatty acids and the potential for adverse health outcomes. Prostaglandins Leukot Essent Fatty Acids. 2013;89:379–390. doi: 10.1016/j.plefa.2013.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002;420:860–867. doi: 10.1038/nature01322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Argiles JM, Lopez-Soriano FJ, Busquets S. Counteracting inflammation: a promising therapy in cachexia. Crit Rev Oncog. 2012;17:253–262. doi: 10.1615/critrevoncog.v17.i3.30. [DOI] [PubMed] [Google Scholar]
- 56.Sommer C, Kress M. Recent findings on how proinflammatory cytokines cause pain: peripheral mechanisms in inflammatory and neuropathic hyperalgesia. Neurosci Lett. 2004;361:184–187. doi: 10.1016/j.neulet.2003.12.007. [DOI] [PubMed] [Google Scholar]
- 57.Graziano F, Ruzzo A, Santini D, Humar B, Tonini G, Catalano V, Berardi R, Pizzagalli F, Arduini F, Bearzi I, Scartozzi M, Cascinu S, Testa E, Ficarelli R, Magnani M. Prognostic role of interleukin-1beta gene and interleukin-1 receptor antagonist gene polymorphisms in patients with advanced gastric cancer. J Clin Oncol. 2005;23:2339–2345. doi: 10.1200/JCO.2005.02.345. [DOI] [PubMed] [Google Scholar]
- 58.Kuroda K, Nakashima J, Kanao K, Kikuchi E, Miyajima A, Horiguchi Y, Nakagawa K, Oya M, Ohigashi T, Murai M. Interleukin 6 is associated with cachexia in patients with prostate cancer. Urology. 2007;69:113–117. doi: 10.1016/j.urology.2006.09.039. [DOI] [PubMed] [Google Scholar]
- 59.Calder PC. n-3 polyunsaturated fatty acids, inflammation, and inflammatory diseases. Am J Clin Nutr. 2006;83(Suppl):1505S–19S. doi: 10.1093/ajcn/83.6.1505S. [DOI] [PubMed] [Google Scholar]
- 60.Vedin I, Cederholm T, Freund Levi Y, Basun H, Garlind A, Faxén Irving G, Jönhagen ME, Vessby B, Wahlund LO, Palmblad J. Effects of docosahexaenoic acid-rich n-3 fatty acid supplementation on cytokine release from blood mononuclear leukocytes: the OmegAD study. Am J Clin Nutr. 2008;87:1616–1622. doi: 10.1093/ajcn/87.6.1616. [DOI] [PubMed] [Google Scholar]
- 61.Han SN, Lichtenstein AH, Ausman LM, Meydani SN. Novel soybean oils differing in fatty acid composition alter immune functions of moderately hypercholesterolemic older adults. J Nutr. 2012;142:2182–2187. doi: 10.3945/jn.112.164335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Calder PC. Marine omega-3 fatty acids and inflammatory processes: effects, mechanisms and clinical relevance. Biochim Biophys Acta. 2015;1851:469–484. doi: 10.1016/j.bbalip.2014.08.010. [DOI] [PubMed] [Google Scholar]
- 63.Bronte V, Zanovello P. Regulation of immune responses by L-arginine metabolism. Nat Rev Immunol. 2005;5:641–654. doi: 10.1038/nri1668. [DOI] [PubMed] [Google Scholar]
- 64.Popovic PJ, Zeh HJ, 3rd, Ochoa JB. Arginine and immunity. J Nutr. 2007;137(Suppl 2):1681S–6S. doi: 10.1093/jn/137.6.1681S. [DOI] [PubMed] [Google Scholar]
- 65.Zea AH, Rodriguez PC, Atkins MB, Hernandez C, Signoretti S, Zabaleta J, McDermott D, Quiceno D, Youmans A, O’Neill A, Mier J, Ochoa AC. Arginase-producing myeloid suppressor cells in renal cell carcinoma patients: a mechanism of tumor evasion. Cancer Res. 2005;65:3044–3048. doi: 10.1158/0008-5472.CAN-04-4505. [DOI] [PubMed] [Google Scholar]
- 66.Werner A, Amann E, Schnitzius V, Habermeier A, Luckner-Minden C, Leuchtner N, Rupp J, Closs EI, Munder M. Induced arginine transport via cationic amino acid transporter-1 is necessary for human T-cell proliferation. Eur J Immunol. 2016;46:92–103. doi: 10.1002/eji.201546047. [DOI] [PubMed] [Google Scholar]
- 67.Sakai T, Taki T, Nakamoto A, Tazaki S, Arakawa M, Nakamoto M, Tsutsumi R, Shuto E. Dietary ribonucleic acid suppresses inflammation of adipose tissue and improves glucose intolerance that is mediated by immune cells in C57BL/6 mice fed a high-fat diet. J Nutr Sci Vitaminol (Tokyo) 2015;61:73–78. doi: 10.3177/jnsv.61.73. [DOI] [PubMed] [Google Scholar]
- 68.Nagafuchi S, Hachimura S, Totsuka M, Takahashi T, Goto M, Yajima T, Kuwata T, Habu S, Kaminogawa S. Dietary nucleotides can up-regulate antigen-specific Th1 immune responses and suppress antigen-specific IgE responses in mice. Int Arch Allergy Immunol. 2000;122:33–41. doi: 10.1159/000024356. [DOI] [PubMed] [Google Scholar]
- 69.Jyonouchi H, Sun S, Winship T, Kuchan MJ. Dietary ribonucleotides increase antigen-specific type 1 T-helper cells in the regional draining lymph nodes in young BALB/cJ mice. Nutrition. 2003;19:41–46. doi: 10.1016/s0899-9007(02)00931-0. [DOI] [PubMed] [Google Scholar]
- 70.Sudo N, Aiba Y, Takaki A, Tanaka K, Yu XN, Oyama N, Koga Y, Kubo C. Dietary nucleic acids promote a shift in Th1/Th2 balance toward Th1-dominant immunity. Clin Exp Allergy. 2000;30:979–987. doi: 10.1046/j.1365-2222.2000.00811.x. [DOI] [PubMed] [Google Scholar]
- 71.Tomiya T, Omata M, Fujiwara K. Significance of branched chain amino acids as possible stimulators of hepatocyte growth factor. Biochem Biophys Res Commun. 2004;313:411–416. doi: 10.1016/j.bbrc.2003.07.017. [DOI] [PubMed] [Google Scholar]
- 72.Tajiri K, Shimizu Y. Branched-chain amino acids in liver diseases. World J Gastroenterol. 2013;19:7620–7629. doi: 10.3748/wjg.v19.i43.7620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Newsholme P. Why is L-glutamine metabolism important to cells of the immune system in health, postinjury, surgery or infection? J Nutr. 2001;131(Suppl):2515S–22S. doi: 10.1093/jn/131.9.2515S. [DOI] [PubMed] [Google Scholar]
- 74.Gottfried E, Kreutz M, Mackensen A. Tumor metabolism as modulator of immune response and tumor progression. Semin Cancer Biol. 2012;22:335–341. doi: 10.1016/j.semcancer.2012.02.009. [DOI] [PubMed] [Google Scholar]
- 75.Sikalidis AK. Amino acids and immune response: a role for cysteine, glutamine, phenylalanine, tryptophan and arginine in T-cell function and cancer? Pathol Oncol Res. 2015;21:9–17. doi: 10.1007/s12253-014-9860-0. [DOI] [PubMed] [Google Scholar]
- 76.Melis GC, Boelens PG, van der Sijp JR, Popovici T, De Bandt JP, Cynober L, van Leeuwen PA. The feeding route (enteral or parenteral) affects the plasma response of the dipetide Ala-Gln and the amino acids glutamine, citrulline and arginine, with the administration of Ala-Gln in preoperative patients. Br J Nutr. 2005;94:19–26. doi: 10.1079/bjn20051463. [DOI] [PubMed] [Google Scholar]
- 77.Diestel CF, Marques RG, Lopes-Paulo F, Paiva D, Horst NL, Caetano CE, Portela MC. Role of L-glutamine and glycine supplementation on irradiated colonic wall. Int J Colorectal Dis. 2007;22:1523–1529. doi: 10.1007/s00384-007-0341-8. [DOI] [PubMed] [Google Scholar]
- 78.Arends J, Bachmann P, Baracos V, Barthelemy N, Bertz H, Bozzetti F, Fearon K, Hütterer E, Isenring E, Kaasa S, Krznaric Z, Laird B, Larsson M, Laviano A, Mühlebach S, Muscaritoli M, Oldervoll L, Ravasco P, Solheim T, Strasser F, de van der Schueren M, Preiser JC. de van der Schueren M, Preiser JC.ESPEN guidelines on nutrition in cancer patients. Clin Nutr. 2016 doi: 10.1016/j.clnu.2016.07.015. Forthcoming. [DOI] [PubMed] [Google Scholar]
- 79.Okabayashi T, Iyoki M, Sugimoto T, Kobayashi M, Hanazaki K. Oral supplementation with carbohydrate- and branched-chain amino acid-enriched nutrients improves postoperative quality of life in patients undergoing hepatic resection. Amino Acids. 2011;40:1213–1220. doi: 10.1007/s00726-010-0748-3. [DOI] [PubMed] [Google Scholar]
- 80.Turnock A, Calder PC, West AL, Izzard M, Morton RP, Plank LD. Perioperative immunonutrition in well-nourished patients undergoing surgery for head and neck cancer: evaluation of inflammatory and immunologic outcomes. Nutrients. 2013;5:1186–1199. doi: 10.3390/nu5041186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Felekis D, Eleftheriadou A, Papadakos G, Bosinakou I, Ferekidou E, Kandiloros D, Katsaragakis S, Charalabopoulos K, Manolopoulos L. Effect of perioperative immuno-enhanced enteral nutrition on inflammatory response, nutritional status, and outcomes in head and neck cancer patients undergoing major surgery. Nutr Cancer. 2010;62:1105–1112. doi: 10.1080/01635581.2010.494336. [DOI] [PubMed] [Google Scholar]
- 82.McGough C, Wedlake L, Baldwin C, Hackett C, Norman AR, Blake P, Harrington K, Tait D, Khoo V, Frost G, Andreyev HJ. Clinical trial: normal diet vs. partial replacement with oral E028 formula for the prevention of gastrointestinal toxicity in cancer patients undergoing pelvic radiotherapy. Aliment Pharmacol Ther. 2008;27:1132–1139. doi: 10.1111/j.1365-2036.2008.03665.x. [DOI] [PubMed] [Google Scholar]
- 83.Faber J, Berkhout M, Fiedler U, Avlar M, Witteman BJ, Vos AP, Henke M, Garssen J, van Helvoort A, Otten MH, Arends J. Rapid EPA and DHA incorporation and reduced PGE2 levels after one week intervention with a medical food in cancer patients receiving radiotherapy, a randomized trial. Clin Nutr. 2013;32:338–345. doi: 10.1016/j.clnu.2012.09.009. [DOI] [PubMed] [Google Scholar]
- 84.Kuroda H, Ushio A, Miyamoto Y, Sawara K, Oikawa K, Kasai K, Endo R, Takikawa Y, Kato A, Suzuki K. Effects of branched-chain amino acid-enriched nutrient for patients with hepatocellular carcinoma following radiofrequency ablation: a one-year prospective trial. J Gastroenterol Hepatol. 2010;25:1550–1555. doi: 10.1111/j.1440-1746.2010.06306.x. [DOI] [PubMed] [Google Scholar]
- 85.Sorensen D, McCarthy M, Baumgartner B, Demars S. Perioperative immunonutrition in head and neck cancer. Laryngoscope. 2009;119:1358–1364. doi: 10.1002/lary.20494. [DOI] [PubMed] [Google Scholar]
- 86.Deutz NE, Safar A, Schutzler S, Memelink R, Ferrando A, Spencer H, van Helvoort A, Wolfe RR. Muscle protein synthesis in cancer patients can be stimulated with a specially formulated medical food. Clin Nutr. 2011;30:759–768. doi: 10.1016/j.clnu.2011.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.van der Meij BS, Langius JA, Smit EF, Spreeuwenberg MD, von Blomberg BM, Heijboer AC, Paul MA, van Leeuwen PA. Oral nutritional supplements containing (n-3) polyunsaturated fatty acids affect the nutritional status of patients with stage III non-small cell lung cancer during multimodality treatment. J Nutr. 2010;140:1774–1780. doi: 10.3945/jn.110.121202. [DOI] [PubMed] [Google Scholar]
- 88.Fujitani K, Tsujinaka T, Fujita J, Miyashiro I, Imamura H, Kimura Y, Kobayashi K, Kurokawa Y, Shimokawa T, Furukawa H, Osaka Gastrointestinal Cancer Chemotherapy Study Group Prospective randomized trial of preoperative enteral immunonutrition followed by elective total gastrectomy for gastric cancer. Br J Surg. 2012;99:621–629. doi: 10.1002/bjs.8706. [DOI] [PubMed] [Google Scholar]
- 89.de Luis DA, Izaola O, Cuellar L, Terroba MC, Arranz M, Fernandez N, Aller R. Effect of c-reactive protein and interleukins blood levels in postsurgery arginine-enhanced enteral nutrition in head and neck cancer patients. Eur J Clin Nutr. 2003;57:96–99. doi: 10.1038/sj.ejcn.1601512. [DOI] [PubMed] [Google Scholar]
- 90.Klek S, Kulig J, Sierzega M, Szczepanek K, Szybiński P, Scislo L, Walewska E, Kubisz A, Szczepanik AM. Standard and immunomodulating enteral nutrition in patients after extended gastrointestinal surgery--a prospective, randomized, controlled clinical trial. Clin Nutr. 2008;27:504–512. doi: 10.1016/j.clnu.2008.04.010. [DOI] [PubMed] [Google Scholar]
- 91.Ryan AM, Reynolds JV, Healy L, Byrne M, Moore J, Brannelly N, McHugh A, McCormack D, Flood P. Enteral nutrition enriched with eicosapentaenoic acid (EPA) preserves lean body mass following esophageal cancer surgery: results of a double-blinded randomized controlled trial. Ann Surg. 2009;249:355–363. doi: 10.1097/SLA.0b013e31819a4789. [DOI] [PubMed] [Google Scholar]