Abstract
Left ventricular (LV) thrombus is usually seen in situations with reduced LV function, and is mostly seen in patients with large anterior ST-elevation myocardial infarction (MI). Most embolic events, in patients with LV thrombus formation, occur within the first 3–4 months, thus the recommendations regarding the duration of anticoagulant therapy. According to guidelines, an oral vitamin K antagonist, warfarin, is being used as an anticoagulant for this period. Novel oral anticoagulants were found to be either non-inferior or superior compared with warfarin in prevention of thromboembolism in patients with non-valvular atrial fibrillation. However, the data about their role in the management of LV thrombus are limited to case reports. Here, we report on the dissolution of LV apical thrombus in 3 patients with anterior ST-elevation MI receiving dual antiplatelet therapy and rivaroxaban on a reduced dose for 3 months.
Background
Left ventricular (LV) thrombus is usually seen in situations with reduced LV function, and is mostly seen in patients with large anterior ST-elevation myocardial infarction (MI) with anteroapical aneurysm formation.1 Many of these patients will have an LV apical aneurysm with akinesis or dyskinesis. In most cases, thrombus is located within or adjacent to the LV apex1 but can also occur with large inferolateral infarctions/aneurysms.
In observational studies and meta-analyses, most embolic events, in patients with LV thrombus formation, occur within the first 3–4 months, thus the recommendations regarding the duration of anticoagulant therapy.2–6
According to guidelines, an oral vitamin K antagonist (VKA), warfarin, is being used as an anticoagulant for this period.7 8
Novel oral anticoagulants (NOACs: dabigatran, rivaroxaban, apixaban, etc) were found to be either non-inferior or superior compared with warfarin in prevention of thromboembolism in patients with non-valvular atrial fibrillation.9 However, the data about the role of NOACs in the management of LV thrombus are scarce and mostly limited to case reports.
Here, we report on the dissolution of LV apical thrombus in three patients with anterior ST-elevation MI receiving dual antiplatelet therapy (DAPT) and rivaroxaban on a reduced dose (15 mg) for 3 months.
Case presentation
Case 1
A Caucasian male aged 52 years was admitted with retrosternal chest pain evolving during the past 5 days. The ECG showed a subacute anterior STEMI with marked ST elevation and Q waves in leads V2–V6.
Transthoracic echocardiography revealed an anteroapical severe hypokinesia with an EF of 35% and an apical sessile thrombus which was confirmed using contrast (figure 1).
Figure 1.

Contrast echocardiography study confirmed the presence of an apical sessile thrombus and a severe anteroapical hypokinesia with an EF of 35%.
HAS-BLED score was 1 point.
The coronary angiogram revealed a total occlusion of the midpart of the left anterior descending coronary artery (LAD) and collateral circulation from the right coronary artery. The vessel was treated using newer-generation drug-eluting stent (Resolute Onyx stents, 3.5 Å∼ 26 mm) with a good angiographic final result.
HAS-BLED score was 1 point.
Case 2
A Caucasian male aged 75 years was admitted with a left-sided thoracic chest pain that started 4 hours prior to presentation. The ECG showed an acute anteroseptal ST-elevation MI with subtle ST elevation in leads V2–V4.
Coronary angiography revealed a tight proximal LAD disease that was directly stented using an everolimus 4 Å∼ 18 mm drug-eluting stent with great angiographic final result. DAPT was started using acetylsalicylic acid (150 mg/day) and prasugrel (10 mg/day).
Transthoracic echocardiography was performed 3 days after the percutaneous coronary invention and revealed a penduculated apical thrombus measuring 1.6×1.7 cm (figure 2) in an akinetic distal anteroapical area and hypokinetic anteroseptal segment with an estimated EF of 35–40%.
Figure 2.
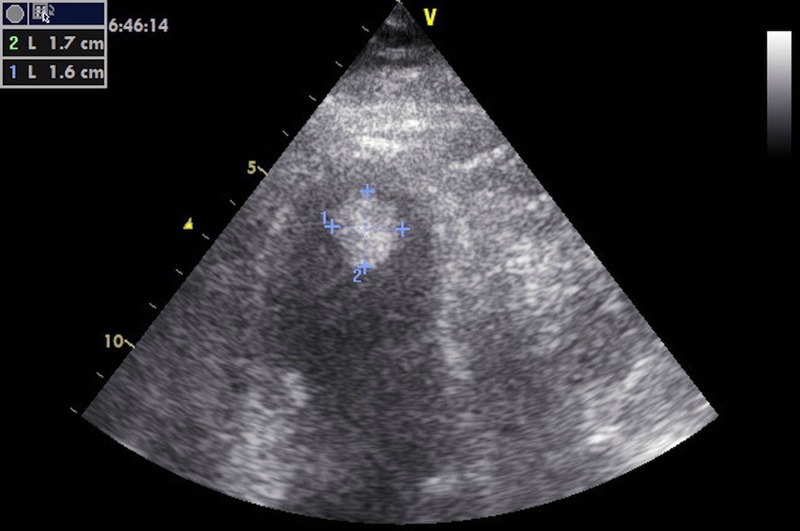
Transthoracic echocardiography revealed a penduculated apical thrombus measuring 1.6×1.7 cm in an akinetic distal anteroapical area and hypokinetic anteroseptal segment with an estimated EF of 35–40%.
HAS-BLED score was 2 points.
Case 3
A Caucasian female aged 69 years was admitted with an epigastric pain that started 11 hours prior to presentation. The ECG showed an acute anterolateral ST-elevation MI with ST elevation in leads V1–V6, I, aVL.
Coronary angiography revealed a tight proximal to mid-long LAD disease that was directly stented using an everolimus 4 Å∼ 32 mm drug-eluting stent with great angiographic final result. DAPT was started using acetylsalicylic acid (75 mg/day) and ticagrelor (180 mg/day).
Transthoracic echocardiography was performed 4 days after the percutaneous coronary invention and revealed a penduculated and elongated apical thrombus measuring 2.5×1.8 cm (figure 3) and a severely anteroapically hypokinetic LV with an EF of 30%.
Figure 3.
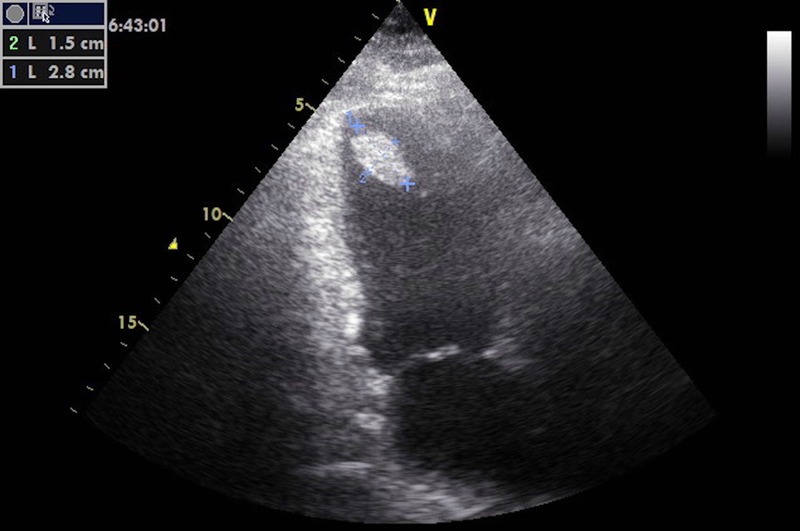
Transthoracic echocardiography revealed a penduculated and elongated apical thrombus measuring 2.5×1.8 cm and a severely anteroapically hypokinetic left ventricle with an EF of 30%.
HAS-BLED score was 2 points.
Treatment
Regarding the patient reported in case 1, DAPT was initiated with acetylsalicylic acid (100 mg/day) and clopidogrel (75 mg/day), while a reduced dose of rivaroxaban (15 mg/day) was given in order to limit the bleeding risk (triple therapy). At 1 month, echocardiography was repeated and revealed complete dissolution of the thrombus, despite persistence of the apical akinesia. The triple therapy was continued for another 2 months.
Regarding the patient reported in case 2, low dose of rivaroxaban was initiated (15 mg/day), while prasugrel was switched to clopidogrel (75 mg/day) and aspirin to 75 mg/day in order again to reduce the bleeding risk as possible. At 1 month, echocardiography was repeated and revealed complete dissolution of the thrombus and normal LV systolic function. Again, and in concordance with the guidelines that refer to VKA after acute coronary syndrome and LV thrombus formation, the above triple therapy (DAPT+rivaroxaban 15 mg/day) was continued for a total of 3 months.
The patient on case 4 was started on rivaroxaban (15 mg/day), and ticagrelor was replaced by clopidogrel (75 mg/day). At 2 weeks, echocardiography was repeated and revealed complete dissolution of the thrombus and an improved LV systolic function (EF 40–45%).
Again, the above triple therapy was continued for a total of 3 months.
Outcome and follow-up
All three patients received a triple therapy that consisted of low dose of rivaroxaban (15 mg/day), and DAPT (aspirin 75–100 mg/day plus clopidogrel 75 mg/day) for a total of 3 months. In all patients, complete dissolution of the thrombi was evident by repeat echocardiography study in 2 weeks–1 month. Follow-up for a year was uneventful for all three cases.
Discussion
Rivaroxaban is an oral inhibitor that binds directly to factor Xa. It is currently approved for the treatment of deep venous thrombosis, non-valvular atrial fibrillation and pulmonary embolism.9–12
Azizi et al13 describe a case of postinfarction LV thrombus dissolution using a combination of DAPT (aspirin 100 mg/day plus clopidogrel 75 mg/day) plus rivaroxaban for 3 months; nevertheless, the daily dose of rivaroxaban they used was 20 mg/day. We, however, used the low dose of rivaroxaban (15 mg/day) for the reasons we will advocate further down.
Ventricular thrombi have been successfully treated using novel anticoagulant, either in cases of old myocardial infarction, where dabigatran was used (220 mg/day),14 or in cases of LV thrombus secondary to tachycardia-induced heart failure using rivaroxaban 15 mg/day.15
Rivaroxaban was also used for treating a case of intraventricular thrombus in Chagas disease16 and in a setting of dilated cardiomyopathy where again 15 mg/day was used.17
Similarly, reported cases have shown the effectiveness of apixaban as well, in the resolution of left atrial thrombus.18
Another case report described the growth of a left atrial appendage thrombus, despite well-conducted treatment with a VKA, which then disappeared during treatment with rivaroxaban 15 mg/day.19 In this report, repeated TEE showed a markedly increased giant thrombus mass in the LAA under well-controlled VKA therapy for 6 weeks. After that, the authors decided to switch the oral anticoagulation to rivaroxaban based on the increasing evidence that VKAs had a poor capability to resolve large intracardiac thrombi. This novel direct acting factor Xa inhibitor is reported to have the potential not only to prevent a thrombosis but also to resolve established thrombi by direct inhibition of free and thrombus-associated Factor Xa.20 Note that in a congestive heart failure rat model, rivaroxaban reduced platelet activation by attenuating the secondary phase of ADP-induced platelet aggregation.21
In the reported cases, we demonstrate LV thrombus dissolution using a rivaroxaban 15 mg/day in the setting of acute coronary syndromes that forced administration of DAPT.
In general, in the setting of ACS, triple therapy with DAPT and NOACs is associated with at least a doubling of the risk of major bleeding, as similarly reported for VKAs in the WOEST trial22 and consistent with the nationwide registry data from Denmark.23 Therefore, there is no strong evidence to suggest that NOACs behave differently to VKAs in the setting of ACS or stenting.
Thus and even though data are limited, the principle of continuing an existing NOAC seems reasonable at present as stated by the European Society of Cardiology Working Group on Thrombosis, European Heart Rhythm Association (EHRA), European Association of Percutaneous Cardiovascular Interventions (EAPCI) and European Association of Acute Cardiac Care (ACCA).24 It is also stated at the same paper that when VKA is given in combination with clopidogrel and/or low-dose aspirin, the dose intensity of VKA should be carefully regulated, with a target INR range of 2.0–2.5 (Class IIa) and where an NOAC is used in combination with clopidogrel and/or low-dose aspirin, the lower tested dose for stroke prevention in AF (ie, dabigatran 110 mg two times per day, rivaroxaban 15 mg o.d. or apixaban 2.5 mg two times per day) may be considered (Class IIb).
Thus, our decision to use the low dose of rivaroxaban stated (15 mg/day).
In the setting of patients requiring oral anticoagulation after percutaneous coronary intervention, the European Society of Cardiology25 states that triple therapy should be limited in duration, depending on the clinical setting, thromboembolic (CHA2DS2-VASc) score and bleeding risks (HAS-BLED) score (Hypertension, Abnormal renal/liver function, Stroke, Bleeding history or predisposition, Labile INR, Elderly, Drugs/alcohol). The duration depends on the individual risk for ischaemic and bleeding events.
The use of prasugrel or ticagrelor as part of triple therapy should be avoided, given the lack of established benefit and the greater risk of major bleeding compared with clopidogrel.
In a prospective observational study of 377 patients who underwent drug-eluting stent placement and who had an indication for OAC, 5.6% received prasugrel and the rest ckopidogrel.26 All patients were treated with triple therapy for at least 6 months. The primary end point of thrombolysis in MI major and minor bleeding occurred more often in the prasugrel group (28.6% vs 6.7%).
In an analysis of the TRANSLATE-ACS study with 11 756 MI patients, 526 (4.5%) were discharged on triple therapy that included aspirin, clopidogrel and warfarin and 91 (0.8%) on triple prasugrel, aspirin and warfarin therapy.27 Triple therapy of the prasugrel arm was associated with a greater risk of any bleeding events compared with the triple-clopidogrel arm.
Gastric protection should be implemented with a proton-pump inhibitor.
Triple therapy using an NOAC could be hazardous and only a few studies have investigated triple therapy, including an NOAC in patients suffering from coronary artery disease and non-valvular atrial fibrillation.
In the APPRAISE-2, apixaban was combined with aspirin and clopidogrel in 81% of patients, and led to a significant increase in fatal and intracranial bleeding without clinical benefit.28
In ATLAS ACS 2, low-dose rivaroxaban (2.5–5 mg two times per day) was administered with aspirin and clopidogrel in 92% of patients. This was associated with a 16% reduction in the composite efficacy end point (cardiovascular death, myocardial infarction and stroke) and a small increase in major bleedings.29
The twice daily 2.5 mg dose of rivaroxaban resulted in significantly lower rates of all-cause and cardiovascular mortality, which was not observed with the twice daily 5.0 mg dose.
The HAS-BLED score was 1–2 for the abovementioned patients, who had normal creatinine clearance and based on the above as well as on observational studies and meta-analyses, that report that most embolic events, in patients with LV thrombus formation, occur within the first 3–4 months, we decided to use rivaroxaban 15 mg/day in addition to DAPT (aspirin 75 mg/day plus clopidogrel 75 mg/day) for a total of 3 months.
All patients had complete thrombus resolution and no bleeding complications.
Learning points.
Short-duration rivaroxaban at a low dose (15 mg/day) in combination with a dual antiplatelet therapy (DAPT) was effective for the treatment of left ventricular (LV) thrombus in patients with acute coronary syndromes and drug-eluting stent implantation, and at low to intermediate bleeding risk.
Randomised controlled trials are needed to confirm these encouraging observational data, and to possibly confirm the optimal low dosage of NOACs when associated with DAPT, demonstrating that these molecules can effectively replace VKAs in the treatment of post-STEMI LV thrombi in patients undergoing percutaneous coronary intervention.
Footnotes
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Weinsaft JW, Kim J, Medicherla CB et al. . Echocardiographic algorithm for post-myocardial infarction LV thrombus: a gatekeeper for thrombus evaluation by delayed enhancement CMR. JACC Cardiovasc Imaging 2016;9:505–15. 10.1016/j.jcmg.2015.06.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Visser CA, Kan G, Meltzer RS et al. . Embolic potential of left ventricular thrombus after myocardial infarction: a two-dimensional echocardiographic study of 119 patients. J Am Coll Cardiol 1985;5:1276 10.1016/S0735-1097(85)80336-3 [DOI] [PubMed] [Google Scholar]
- 3.Küpper AJ, Verheugt FW, Peels CH et al. . Left ventricular thrombus incidence and behavior studied by serial two-dimensional echocardiography in acute anterior myocardial infarction: left ventricular wall motion, systemic embolism and oral anticoagulation. J Am Coll Cardiol 1989;13:1514 10.1016/0735-1097(89)90341-0 [DOI] [PubMed] [Google Scholar]
- 4.Keren A, Goldberg S, Gottlieb S et al. . Natural history of left ventricular thrombi: their appearance and resolution in the posthospitalization period of acute myocardial infarction. J Am Coll Cardiol 1990;15:790 10.1016/0735-1097(90)90275-T [DOI] [PubMed] [Google Scholar]
- 5.Vaitkus PT, Barnathan ES. Embolic potential, prevention and management of mural thrombus complicating anterior myocardial infarction: a meta-analysis. J Am Coll Cardiol 1993;22:1004 10.1016/0735-1097(93)90409-T [DOI] [PubMed] [Google Scholar]
- 6.Cregler LL. Antithrombotic therapy in left ventricular thrombosis and systemic embolism. Am Heart J 1992;123(Pt 2):1110 10.1016/0002-8703(92)91069-D [DOI] [PubMed] [Google Scholar]
- 7.American College of Emergency Physicians; Society for Cardiovascular Angiography and Interventions O'Gara PT, Kushner FG, Ascheim DD et al. . 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2013;61:e78–140. 10.1016/j.jacc.2012.11.019 [DOI] [PubMed] [Google Scholar]
- 8.Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC) Steg PG, James SK, Atar D et al. . ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J 2012;33:2569–619. 10.1093/eurheartj/ehs213 [DOI] [PubMed] [Google Scholar]
- 9.Heidbuchel H, Verhamme P, Alings M et al. . European Heart Rhythm Association practical guide on the use of new oral anticoagulants in patients with non-valvular atrial fibrillation. Europace 2013;15:625–51. 10.1093/europace/eut083 [DOI] [PubMed] [Google Scholar]
- 10.Harder S. Pharmacokinetic and pharmacodynamic evaluation of rivaroxaban: considerations for the treatment of venous thromboembolism. Thromb J 2014;12:22 10.1186/1477-9560-12-22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kirchhof P, Benussi S, Kotecha D et al. . 2016 ESC guidelines for the management of atrial fibrillation developed in collaboration with EACTS: the Task Force for the management of atrial fibrillation of the European Society of Cardiology (ESC) developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESCEndorsed by the European Stroke Organisation (ESO). Europace 2016;18:1455–90.27402624 [Google Scholar]
- 12.Saar JA, Maack C. Diagnosis and management of acute pulmonary embolism. ESC guidelines 2014. Herz 2015;40:1048–54. 10.1007/s00059-015-4378-0 [DOI] [PubMed] [Google Scholar]
- 13.Azizi A, Puricel S, Cook S et al. . Rivaroxaban dissolves postinfarction left ventricular thrombus. Cardiovascular Medicine—Kardiovaskuläre Medizin—Médecine Cardiovasculaire 2016;19:25–7. [Google Scholar]
- 14.Nagamoto Y, Shiomi T, Matsuura T et al. . Resolution of a left ventricular thrombus by the thrombolytic action of dabigatran. Heart Vessels 2014;29:560–2. 10.1007/s00380-013-0403-5 [DOI] [PubMed] [Google Scholar]
- 15.Nakasuka K, Ito S, Noda T et al. . Resolution of left ventricular thrombus secondary to tachycardia induced heart failure with rivaroxaban. Case Rep Med 2014;2014:814524 10.1155/2014/814524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Las Casas AA Jr, Las Casas AA, Borges MAF et al. . Rivaroxaban for treatment of intraventricular thrombus in Chagas disease. J Cardiology Cases 2016;16:75–7. 10.1016/j.jccase.2015.10.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Padilla Pérez M, Salas Bravo D, Garcelán Trigo JA et al. . Resolution of left ventricular thrombus by rivaroxaban. Future Cardiol 2014;10:333–6. 10.2217/fca.14.12 [DOI] [PubMed] [Google Scholar]
- 18.Kawakami T, Kobayakawa H, Ohno H et al. . Resolution of left atrial appendage thrombus with apixaban. Thromb J 2013;11:26 10.1186/1477-9560-11-26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hammerstingl C, Pötzsch B, Nickenig G. Resolution of giant left atrial appendage thrombus with rivaroxaban. Thromb Haemost 2013;109:583–4. 10.1160/TH12-11-0821 [DOI] [PubMed] [Google Scholar]
- 20.Yeh CH, Fredenburgh JC, Weitz JI. Oral direct factor xa inhibitors. Circ Res 2012;111:1069–78. [DOI] [PubMed] [Google Scholar]
- 21.Flierl U, Fraccarollo D, Micka J et al. . The direct factor Xa inhibitor Rivaroxaban reduces platelet activation in congestive heart failure. Pharmacol Res 2013;74:49–55. 10.1016/j.phrs.2013.05.002 [DOI] [PubMed] [Google Scholar]
- 22.Dewilde WJ, Oirbans T, Verheugt FW et al. . Use of clopidogrel with or without aspirin in patients taking oral anticoagulant therapy and undergoing percutaneous coronary intervention: an open-label, randomised, controlled trial. Lancet 2013;381:1107–15. 10.1016/S0140-6736(12)62177-1 [DOI] [PubMed] [Google Scholar]
- 23.Lamberts M, Gislason GH, Olesen JB et al. . Oral anticoagulation and antiplatelets in atrial fibrillation patients after myocardial infarction and coronary intervention. J Am Coll Cardiol 2013;62:981–9. 10.1016/j.jacc.2013.05.029 [DOI] [PubMed] [Google Scholar]
- 24.Lip GY, Windecker S, Huber K et al. . Management of antithrombotic therapy in atrial fibrillation patients presenting with acute coronary syndrome and/or undergoing percutaneous coronary or valve interventions: a joint consensus document of the European Society of Cardiology Working Group on Thrombosis, European Heart Rhythm Association (EHRA), European Association of Percutaneous Cardiovascular Interventions (EAPCI) and European Association of Acute Cardiac Care (ACCA) endorsed by the Heart Rhythm Society (HRS) and Asia-Pacific Heart Rhythm Society (APHRS). Eur Heart J 2014;35:3155–79. 10.1093/eurheartj/ehu298 [DOI] [PubMed] [Google Scholar]
- 25.Kolh P, Windecker S, Alfonso F. ESC/EACTS Guidelines on myocardial revascularization: the Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur J Cardiothorac Surg 2014;46:517–92. 10.1093/ejcts/ezu366 [DOI] [PubMed] [Google Scholar]
- 26.Sarafoff N, Martischnig A, Wealer J et al. . Triple therapy with aspirin, prasugrel, and vitamin K antagonists in patients with drug-eluting stent implantation and an indication for oral anticoagulation. J Am Coll Cardiol 2013;61:2060 10.1016/j.jacc.2013.02.036 [DOI] [PubMed] [Google Scholar]
- 27.Jackson LR 2nd, Ju C, Zettler M et al. . Outcomes of patients with acute myocardial infarction undergoing percutaneous coronary intervention receiving an oral anticoagulant and dual antiplatelet therapy: a comparison of clopidogrel versus prasugrel from the TRANSLATE-ACS Study. JACC Cardiovasc Interv 2015;8:1880 10.1016/j.jcin.2015.08.018 [DOI] [PubMed] [Google Scholar]
- 28.Alexander JH, Lopes RD, James S et al. . Apixaban with antiplatelet therapy after acute coronary syndrome. N Engl J Med 2011;365:699–708. 10.1056/NEJMoa1105819 [DOI] [PubMed] [Google Scholar]
- 29.Mega JL, Braunwald E, Wiviott SD et al. . the AACSTI. Rivaroxaban in patients with a recent acute coronary syndrome. N Engl J Med 2012;366:9–19. 10.1056/NEJMoa1112277 [DOI] [PubMed] [Google Scholar]


