Abstract
Purpose
To determine the short-term effect of rigid gas permeable (RGP) contact lenses on corneal aberrations in keratoconic patients.
Method
Sixteen keratoconic eyes with no history of RGP lens wear were included. They all had corneal aberrometry using Pentacam, and different aberration indices of the anterior and posterior surfaces of the cornea were measured before and 3 months after fitting RGP lenses. The effect of baseline parameters on these changes was tested in univariate and multiple models.
Results
Total aberrations and individual Zernike coefficients did not show statistically significant changes after using RGP lenses. Although not statistically significant, vertical coma decreased in the anterior (p = 0.073) and posterior surface (p = 0.095). Relationships that remained statistically significant in the multiple model were between baseline central corneal thickness and changes in total higher order aberrations and anterior 4th order astigmatism 0°, and between baseline 2nd order astigmatism 45° and its changes.
Conclusion
In this study, corneal aberrations remained unchanged 3 months after wearing RGP contact lens. Further studies with sufficient samples in different groups of keratoconus severity or baseline aberrations are needed to obtain more accurate results.
Keywords: Aberrometry, Keratoconus, Rigid gas permeable contact lens, Pentacam
Introduction
The cornea is a major source of aberrations which can cause limitations in visual acuity and quality.1, 2, 3 In keratoconus patients, decreased visual acuity is one of the main complaints, and in comparison with normal corneas, keratoconic eyes exhibit many corneal irregularities, irregular astigmatism, and aberrations.4, 5, 6, 7 Coma, especially vertical coma, is the most common aberration in keratoconic patients.8 These aberrations are found and can be evaluated in both the posterior and anterior surfaces of the cornea.9 Measuring corneal aberrations changes improves our understanding of the changes in the shape and optical properties of the cornea and keratoconus progression.10 Studies suggest that vertical coma and total root mean square (RMS) aberrations are the best aberrometry indices to detect keratoconus.11, 12, 13
Vision improvement in keratoconic patients can be achieved through the use of contact lenses or surgical methods such as corneal ring implantation and corneal grafting. Rigid gas permeable (RGP) lenses, the first lens choice for keratoconic patients, are believed to change corneal astigmatism as a result of the optical characteristics of the tear layer behind the lens.14 However, studies in this regard are inconclusive; they vary in methodology and follow-up time, and there are still many questions concerning the effects of RGP lenses on different corneal parameters.15, 16, 17, 18 This study was designed to examine changes in the total RMS and Zernike polynomials in keratoconic patients after 3 months of RGP lens wear.
Method
In this prospective, before–after case series, patients with mild to severe keratoconus referring to the contact lens clinic were included. The study was approved by the Ethics Committee of Iran University of Medical Sciences. All patients had already had complete ophthalmic evaluation by a cornea specialist, based on which the diagnosis of keratoconus was made and confirmed through imaging modalities. Objectives and methods of the study were explained to patients, and they all signed informed consents before participation in the study.
Inclusion criteria were age between 19 and 35 years and being eligible for fitting RGP spherical lenses. Patients with a history of RGP lens use, corneal scarring, infectious or inflammatory ocular diseases, corneal graft surgery, ring implantation or corneal collagen crosslinking, and those referred for fitting mini-scleral and ClearKone lenses were excluded.
Patients had complete ocular examination including the measurement of visual acuity using a Snellen chart (Nidek-34605-6004-LCD Chart, Japan) at 4 m, objective refraction with a retinoscope (Heine Beta 200, Germany) and an auto-refractometer (Nidek, Japan), and subjective refraction with a trial lens set and frame. The appropriate aspheric RGP lens (Iran, Lens Gostar, Tehran, Iran) was prescribed using the diagnostic fitting method.19 On slit-lamp examination, good tear exchange was verified by observing the fluorescein pattern with mild apical clearance over the corneal cone and slight edge and midperipheral clearance.20 Patients were instructed to wear their lenses 3 h a day during the first week, and add an hour a day per week up to a maximum of 8 h daily. Follow-up calls were made to patients to stay in touch with them and ensure adherence to the study protocol.
To measure aberrations of the anterior and posterior surfaces of the cornea at baseline and at 3 months, we used the Pentacam corneal topographer (Oculus Optikgeräte GmbH, Wetzlar, Germany) which has shown to be highly reliable.21 Extracted indices for the anterior and posterior corneal surfaces included the total RMS, 2nd order astigmatism 45°, 3rd order coma 0° and 90°, 3rd order trefoil 0° and 30°, and 4th order secondary astigmatism 0° and 45° measured over a 6.0 mm aperture.
Statistical analyses were done using the Statistical Package for Social Sciences (SPSS) Version 20.0 (Chicago, IL, USA). Results were compared using repeated measures analysis of covariance (ANCOVA), and the correlation between fellow eyes was accounted for. Changes were considered significant based on a significance level of 5%. Relationships between aberration changes and other variables were also explored using single and multiple linear regression analyses.
Results
A total of 10 patients, 3 women and 7 men, with a mean age of 27.2 ± 4.9 years (range, 20–35) were enrolled, and their 16 keratoconic eyes were evaluated. Based on the indices and classification scheme suggested by Rabinowitz, the number of eyes that could be classified as keratoconus and early keratoconus was 12 and 4, respectively.22 The diameter of the prescribed RGP lenses was 9.60 mm in all cases, and they had a mean base curve radius of 7.70 ± 0.28 mm (range, 7.20–8.10) and a mean power of −1.56 ± 1.26 diopters (D) (range, −3.00 to +1.25). At baseline, patients had a mean maximum keratometry reading of 54.06 ± 5.73D (range, 43.90–67.10 D), mean central corneal thickness (CCT) of 468.40 ± 56.11 μm (range, 381–547), and mean anterior Q-value of −0.80 ± 0.39 (range, −1.52 to −0.28), as determined with the Pentacam. Table 1 presents the mean values for these variables at 3 months and their changes.
Table 1.
Corneal curvature, thickness, Q-value, and anterior and posterior aberrations in the studied sample at baseline and 3 months after wearing rigid gas permeable contact lenses.
| Baseline | At 3 months | Mean change (95% confidence interval) | p Valuea | |
|---|---|---|---|---|
| Maximum k-reading (diopter) | 54.06 ± 5.73 | 54.52 ± 6.07 | 0.46 ± 2.10 (−0.70, 1.62) | 0.410 |
| Central corneal thickness (micron) | 468.40 ± 56.11 | 465.40 ± 59.34 | −3.00 ± 10.34 (−8.73, 2.73) | 0.280 |
| Anterior Q-value | −0.79 ± 0.39 | −0.80 ± 0.45 | −0.01 ± 0.20 (−0.13, 0.10) | 0.785 |
| Posterior Q-value | −0.87 ± 0.66 | −0.84 ± 0.76 | 0.03 ± 0.27 (−0.12, 0.18) | 0.658 |
| Total RMS LOA | 9.00 ± 4.40 | 8.69 ± 5.53 | −0.31 ± 2.35 (−1.56, 0.94) | 0.605 |
| Total RMS HOA | 2.54 ± 1.41 | 2.52 ± 2.04 | −0.02 ± 1.10 (−0.60, 0.56) | 0.942 |
| Anterior corneal surface aberrations (micron) | ||||
| Total RMS | 10.95 ± 5.34 | 10.69 ± 4.92 | −0.26 ± 1.42 (−1.04, 0.53) | 0.495 |
| 2nd order astigmatism 0° | −1.00 ± 2.64 | −0.87 ± 2.86 | 0.13 ± 0.49 (−0.13, 0.39) | 0.304 |
| 2nd order astigmatism 45° | −0.29 ± 2.60 | −0.64 ± 2.11 | −0.35 ± 1.43 (−1.11, 0.41) | 0.343 |
| 3rd order coma 0° | −0.40 ± 1.30 | −0.56 ± 1.58 | −0.16 ± 0.75 (−0.56, 0.24) | 0.414 |
| 3rd order coma 90° | −2.09 ± 1.29 | −1.61 ± 1.36 | 0.48 ± 1.00 (−0.05, 1.01) | 0.073 |
| 3rd order trefoil 0° | 0.06 ± 1.12 | 0.38 ± 1.41 | 0.32 ± 0.94 (−0.18, 0.82) | 0.189 |
| 3rd order trefoil 30° | 0.02 ± 0.49 | −0.33 ± 1.15 | −0.35 ± 1.02 (−0.90, 0.19) | 0.187 |
| 4th order spherical aberration | −0.73 ± 0.95 | −0.42 ± 0.72 | 0.31 ± 0.75 (−0.90, 0.71) | 0.119 |
| 4th order vertical astigmatism 0° | 0.03 ± 0.66 | −0.02 ± 0.64 | −0.05 ± 0.18 (−0.15, 0.04) | 0.273 |
| 4th order oblique astigmatism 45° | 0.06 ± 0.61 | 0.17 ± 0.49 | 0.11 ± 0.28 (−0.04, 0.27) | 0.124 |
| Posterior corneal surface aberrations (micron) | ||||
| Total RMS | 2.71 ± 0.98 | 2.75 ± 1.17 | 0.05 ± 0.48 (−0.21, 0.31) | 0.693 |
| 2nd order astigmatism 0° | 0.45 ± 0.27 | 0.47 ± 0.27 | 0.01 ± 0.15 (−0.06, 0.09) | 0.718 |
| 2nd order astigmatism 45° | −0.01 ± 0.39 | 0.02 ± 0.36 | 0.03 ± 0.17 (−0.06, 0.12) | 0.499 |
| 3rd order coma 0° | 0.04 ± 0.31 | 0.05 ± 0.29 | 0.01 ± 0.17 (−0.08, 0.11) | 0.774 |
| 3rd order coma 90° | 0.50 ± 0.28 | 0.39 ± 0.36 | −0.12 ± 0.26 (−0.25, 0.02) | 0.095 |
| 3rd order trefoil 0° | 0.05 ± 0.24 | 0.01 ± 0.12 | −0.04 ± 0.22 (−0.16, 0.08) | 0.472 |
| 3rd order trefoil 30° | −0.09 ± 0.17 | 0.00 ± 0.26 | 0.09 ± 0.25 (−0.04, 0.22) | 0.170 |
| 4th order spherical aberration | 0.03 ± 0.16 | 0.01 ± 0.17 | −0.02 ± 0.06 (−0.05, 0.01) | 0.180 |
| 4th order astigmatism 0° | −0.06 ± 0.10 | −0.05 ± 0.11 | 0.01 ± 0.06 (−0.02, 0.04) | 0.519 |
| 4th order astigmatism 45° | 0.00 ± 0.11 | −0.01 ± 0.13 | −0.01 ± 0.06 (−0.04, 0.02) | 0.635 |
HOA: High order aberration, LOA: Low order aberration, RMS: Root mean square.
Repeated measures analysis of covariance.
Studied aberrations in the anterior and posterior corneal surface before and 3 months after using RGP lenses are summarized in Table 1. None of the studied aberration indices in the anterior or posterior corneal surfaces showed no significant change.
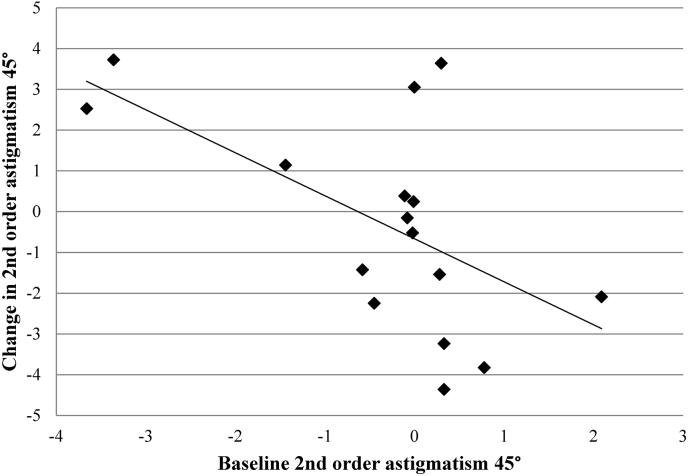
In the second set of analyses, we examined the effect of baseline values of different parameters on the amount of 3-month changes in the studied aberrations. With univariate regression analyses, baseline CCT significantly impacted changes in total RMS HOA (β = 0.009, p = 0.017), anterior surface 3rd order coma 90° (β = −0.010, p = 0.034), and anterior surface 4th order astigmatism 0° (β = 0.002, p = 0.029). CCT relationships with total RMS HOA and anterior 4th order astigmatism 0° retained their significance in the multiple model as well (β = −0.841, p = 0.001 and β = 0.003, p = 0.045, respectively). Also, changes in anterior spherical aberration (β = −0.525, p = 0.005), 2nd order astigmatism 45° (β = −0.321, p = 0.018), and 4th order astigmatism 45° (β = −0.279, p = 0.014) significantly related with their baseline values; the second relationship retained its significance in the multiple model (β = −0.313, p = 0.045) and is illustrated in Fig. 1. No other significant relation was found between changes in any of the aberration variables and baseline maximum keratometry reading, CCT, or anterior Q-value (all Ps > 0.05).
Fig. 1.
Regression line showing the relation between changes in 2nd order oblique astigmatism in microns 3 months after wearing rigid gas permeable contact lenses and its baseline values in the studied sample of keratoconus patients.
Discussion
The impacts of contact lens wear on the human corneal topography and optical performance have been examined through various studies which vary by design, sample size and type, follow-up periods, and measurement tools. Similarly, studies of RGP lenses on keratoconus patients not only vary by these parameters, but also fitting methods and choice of lens, and results have been inconclusive. Of note, most of the few available studies have focused on changes after suspending contact lens wear or with lenses in place.18, 23, 24 In this study, we examined changes in ocular aberrations after 3 months of RGP lens wear in keratoconus patients using the Pentacam Zernike Analysis software. Determining the role of baseline parameters may provide practitioners with information that can be useful for predicting outcomes.
As presented in Table 1, we observed no significant change in any aberration index of the anterior or posterior cornea. Total RMS is an important parameter for the analysis and understanding the theoretical values of ocular aberrations25 and encompasses all higher and lower order aberrations. In a recent comparative study of apical touch and three point touch fitting methods in 50 keratoconic eyes of 31 patients, total RMS, as measured with the Pentacam, was reported to decrease after 14 days of RGP lens wear.26 In terms of total RMS HOA reduced levels were observed in a study of 40 keratoconic eyes using a Hartman Shack aberrometer before and after fitting RGP lenses.27 In a retrospective study by Negishi et al, changes were examined in 13 eyes of 10 patients with mild keratoconus, and the authors reported significant decreases in the total RMS HOA, third order coefficients, and fourth order Zernike coefficients.17
In our study, vertical coma slightly reduced 3 months after RGP lens wear; mean change was 0.48 ± 0.10 μm for the anterior corneal surface and −0.11 ± 0.26 μm for the posterior corneal surface. Statistical analysis showed a borderline significant decrease 3 months after using RGP lenses. The importance of this finding is that a larger sample size may generate results with statistical significance. Also, changes in the vertical coma of the anterior and posterior corneal surfaces had opposite signs. In keratoconic eyes, coma, especially vertical coma, tends to increase as the disease progresses28 which is due to the inferior position of the corneal cone in most patients.29, 30, 31 Very few studies have evaluated coma changes in relation to RGP lens wear in keratoconus patients. Kosaki et al studied 19 eyes of 15 keratoconic patients and reported a decrease in coma from 0.35 ± 0.29 μm to 0.16 ± 0.08 μm and secondary astigmatism from 0.11 ± 0.07 μm to 0.04 ± 0.02 μm in the anterior surface of the cornea.32 They also examined the effect of RGP lens wear on the posterior surface of the cornea.32 In agreement with our results, the posterior surface was less influenced by RGP lens wear, compared to the anterior corneal surface.
Studies suggest that contact lens wear-related aberrometry changes and direction of coma depend on baseline aberrations and corneal shape.33, 34 In our study, we found significant relationships between baseline CCT and changes in total RMS HOA, anterior surface 3rd order coma 90°, and anterior surface 4th order astigmatism 0°. Also, changes in anterior spherical aberration, 2nd order astigmatism 45°, and 4th order astigmatism 45° significantly related with their baseline values. In a 2007 comparative study between 22 myopic eyes and 14 keratoconic eyes, the authors concluded that HOA can be enhanced or reduced based on baseline ocular aberrations as an effect of changes in vertical coma. In the mentioned study, HOA decreased from 0.54 μm to 0.36 μm while coma increased from −0.185 μm to 0.134 μm, and the orientation of coma changed from inferior to superior cornea in keratoconus patients.16 These observations call for further studies with sufficient samples in different groups of keratoconus severity or baseline aberrations.
This study has several limitations. The sample size of our study was too small to draw a definitive conclusion. Also, the number of eyes in the different subgroups was not enough to allow for analysis in categories defined by corneal thickness, keratoconus grade, and baseline aberrations.
In conclusion short-term RGP lens wear in keratoconus patients seems to be associated with no significant increase or even a decrease in aberrations. Further long-term studies with larger sample sizes are needed to complete our knowledge in these areas.
Footnotes
Conflict of interest: No conflicting relationship exists for any author.
Financial Support: This project was funded by the Noor Ophthalmology Research Center.
Peer review under responsibility of the Iranian Society of Ophthalmology.
References
- 1.Seiler T., Mrochen M., Kaemmerer M. Operative correction of ocular aberrations to improve visual acuity. J Refract Surg. 2000;16:S619–S622. doi: 10.3928/1081-597X-20000901-27. [DOI] [PubMed] [Google Scholar]
- 2.Rabinowitz Y.S. Keratoconus. Surv Ophthalmol. 1998;42:297–319. doi: 10.1016/s0039-6257(97)00119-7. [DOI] [PubMed] [Google Scholar]
- 3.He J.C., Marcos S., Webb R., Burns S.A. Measurement of the wave-front aberration of the eye by a fast psychophysical procedure. JOSA A. 1998;15:2449–2456. doi: 10.1364/josaa.15.002449. [DOI] [PubMed] [Google Scholar]
- 4.Schlegel Z., Lteif Y., Bains H.S., Gatinel D. Total, corneal, and internal ocular optical aberrations in patients with keratoconus. J Refract Surg. 2009;25:951. doi: 10.3928/1081597X-20090915-10. [DOI] [PubMed] [Google Scholar]
- 5.Li X., Yang H., Rabinowitz Y.S. Longitudinal study of keratoconus progression. Exp Eye Res. 2007;85:502–507. doi: 10.1016/j.exer.2007.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zadnik K., Barr J.T., Edrington T.B. Baseline findings in the Collaborative Longitudinal Evaluation of keratoconus (CLEK) study. Invest Ophthalmol Vis Sci. 1998;39:2537–2546. [PubMed] [Google Scholar]
- 7.Alió J.L., Shabayek M.H. Corneal higher order aberrations: a method to grade keratoconus. J Refract Surg. 2006;22:539. doi: 10.3928/1081-597X-20060601-05. [DOI] [PubMed] [Google Scholar]
- 8.Pantanelli S., MacRae S., Jeong T.M., Yoon G. Characterizing the wave aberration in eyes with keratoconus or penetrating keratoplasty using a high–dynamic range wavefront sensor. Ophthalmology. 2007;114:2013–2021. doi: 10.1016/j.ophtha.2007.01.008. [DOI] [PubMed] [Google Scholar]
- 9.Nakagawa T., Maeda N., Kosaki R. Higher-order aberrations due to the posterior corneal surface in patients with keratoconus. Invest Ophthalmol Vis Sci. 2009;50:2660–2665. doi: 10.1167/iovs.08-2754. [DOI] [PubMed] [Google Scholar]
- 10.He J.C., Sun P., Held R., Thorn F., Sun X., Gwiazda J.E. Wavefront aberrations in eyes of emmetropic and moderately myopic school children and young adults. Vis Res. 2002;42:1063–1070. doi: 10.1016/s0042-6989(02)00035-4. [DOI] [PubMed] [Google Scholar]
- 11.Jafri B., Li X., Yang H., Rabinowitz Y.S. Higher order wavefront aberrations and topography in early and suspected keratoconus. J Refract Surg. 2007;23:774–781. doi: 10.3928/1081-597X-20071001-06. [DOI] [PubMed] [Google Scholar]
- 12.Gordon-Shaag A., Millodot M., Ifrah R., Shneor E. Aberrations and topography in normal, keratoconus-suspect, and keratoconic eyes. Optom Vis Sci. Apr 2012;89:411–418. doi: 10.1097/OPX.0b013e318249d727. [DOI] [PubMed] [Google Scholar]
- 13.Agarwal A., Agarwal A., Jacob S. Jaypee Brothers Publishers; 2010. Dr. Agarwal's Textbook on Corneal Topography: Including Pentacam and Anterior Segment OCT. [Google Scholar]
- 14.Lawless M., Coster D.J., Phillips A.J., Loane M. Keratoconus: diagnosis and management. Aust N Z J Ophthalmol. 1989;17(1):33–60. doi: 10.1111/j.1442-9071.1989.tb00487.x. [DOI] [PubMed] [Google Scholar]
- 15.Liu Z., Pflugfelder S.C. The effects of long-term contact lens wear on corneal thickness, curvature, and surface regularity. Ophthalmology. 2000;107:105–111. doi: 10.1016/s0161-6420(99)00027-5. [DOI] [PubMed] [Google Scholar]
- 16.Choi J., Wee W.R., Lee J.H., Kim M.K. Changes of ocular higher order aberration in on-and off-eye of rigid gas permeable contact lenses. Optom Vis Sci. 2007;84:42–51. doi: 10.1097/01.opx.0000254036.45989.65. [DOI] [PubMed] [Google Scholar]
- 17.Negishi K., Kumanomido T., Utsumi Y., Tsubota K. Effect of higher-order aberrations on visual function in keratoconic eyes with a rigid gas permeable contact lens. Am J Ophthalmol. 2007;144:924–929. doi: 10.1016/j.ajo.2007.08.004. e921. [DOI] [PubMed] [Google Scholar]
- 18.Jinabhai A., Radhakrishnan H., O'Donnell C. Corneal changes after suspending contact lens wear in early pellucid marginal corneal degeneration and moderate keratoconus. Eye Contact Lens. 2011;37:99–105. doi: 10.1097/ICL.0b013e31820592b1. [DOI] [PubMed] [Google Scholar]
- 19.Bennett E.S., Weissman B.A. Lippincott Williams & Wilkins; 2005. Clinical Contact Lens Practice. [Google Scholar]
- 20.Herranz R.M., Zarzuelo G.R., de Juan Herráez V. INTECH Open Access Publisher; 2012. Contact Lens Correction of Regular and Irregular Astigmatism. [Google Scholar]
- 21.Doménech Amigot B., Mas Candela D., Ronda Pérez E., Pérez Rodríguez J., Espinosa Tomás J., Illueca Contri C. 2009. Repeatability and Concordance of the Pentacam System: Comparative Study of Corneal Parameters Measured with Pentacam and Atlas. [Google Scholar]
- 22.Rabinowitz Y.S. Corneal topography. In: Bennett E.S., Weissman B.A., editors. Clinical Contact Lens Practice. Lippincott, Williams and Wilkins; Philadelphia, PA: 2005. pp. 215–232. [Google Scholar]
- 23.Marsack J.D., Parker K.E., Pesudovs K., Donnelly W.J., 3rd, Applegate R.A. Uncorrected wavefront error and visual performance during RGP wear in keratoconus. Optom Vis Sci. 2007;84:463–470. doi: 10.1097/OPX.0b013e31802e64f0. [DOI] [PubMed] [Google Scholar]
- 24.Jinabhai A., O'Donnell C., Radhakrishnan H. Changes in refraction, ocular aberrations, and corneal structure after suspending rigid gas-permeable contact lens wear in keratoconus. Cornea. May 2012;31:500–508. doi: 10.1097/ICO.0b013e31820f777b. [DOI] [PubMed] [Google Scholar]
- 25.Copeland R., Afshari N. Jaypee Brothers Medical Publishers; New Delhi: 2013. Principles and Practice of Cornea. [Google Scholar]
- 26.Romero-Jiménez M., Santodomingo-Rubido J., Flores-Rodríguez P., González-Méijome J.-M. Short-term corneal changes with gas-permeable contact lens wear in keratoconus subjects: a comparison of two fitting approaches. J Optom. 2015;8:48–55. doi: 10.1016/j.optom.2014.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Baghbani F., Heravian J., Derakhshan A. Evaluation of predictive value of aberrometry visual performance of keratoconus patients before and after rigid gas permable lenses. Arak Med Univ J. 2013;16:23–29. [Google Scholar]
- 28.Schwiegerling J., Greivenkamp J.E. Using corneal height maps and polynomial decomposition to determine corneal aberrations. Optom Vis Sci. 1997;74:906–916. doi: 10.1097/00006324-199711000-00024. [DOI] [PubMed] [Google Scholar]
- 29.Applegate R.A., Hilmantel G., Howland H.C., Tu E.Y., Starck T., Zayac E.J. Corneal first surface optical aberrations and visual performance. J Refract Surg. 2000;16:507–514. doi: 10.3928/1081-597X-20000901-04. [DOI] [PubMed] [Google Scholar]
- 30.Gobbe M., Guillon M. Corneal wavefront aberration measurements to detect keratoconus patients. Contact Lens Anterior Eye. 2005;28:57–66. doi: 10.1016/j.clae.2004.12.001. [DOI] [PubMed] [Google Scholar]
- 31.Wilson S.E., Lin D.T., Klyce S.D. Corneal topography of keratoconus. Cornea. 1991;10:2–8. [PubMed] [Google Scholar]
- 32.Kosaki R., Maeda N., Bessho K. Magnitude and orientation of Zernike terms in patients with keratoconus. Invest Ophthalmol Vis Sci. 2007;48:3062. doi: 10.1167/iovs.06-1285. [DOI] [PubMed] [Google Scholar]
- 33.Lu F., Mao X., Qu J., Xu D., He J.C. Monochromatic wavefront aberrations in the human eye with contact lenses. Optom Vis Sci. 2003;80:135–141. doi: 10.1097/00006324-200302000-00009. [DOI] [PubMed] [Google Scholar]
- 34.Dorronsoro C., Barbero S., Llorente L., Marcos S. On-eye measurement of optical performance of rigid gas permeable contact lenses based on ocular and corneal aberrometry. Optom Vis Sci. 2003;80:115–125. doi: 10.1097/00006324-200302000-00007. [DOI] [PubMed] [Google Scholar]