Abstract
Background:
To determine the mean and median delays in pulmonary tuberculosis (PTB) diagnosis among adults in one of the world's highest gross domestic product per capita countries and identify patient and health system-related reasons for these delays.
Methods:
This is a cross-sectional, face-to-face, prospective study of 100 subjects with confirmed PTB, conducted at main tuberculosis (TB) admitting facilities in Qatar. The mean and median diagnostic delays were measured. The Chi-square test with two-sided P < 0.05 was considered to determine the association between factors and diagnostic delay.
Results:
The mean and median total diagnostic delays of PTB were 53 (95% confidence interval [CI] 42.61–63.59) and 30 (interquartile range; Q1–Q3, 15–60) days, respectively. The mean patient factor delay was 45.7 (95% CI 28.1–63.4) days, and the median was 30 (interquartile range; Q1–Q3, 15–60) days. The mean health system factor delay was 46.3 (95% CI 35.46–57.06) days, and the median was 30 (interquartile range; Q1–Q3, 18–60) days. The most common cause of patient factor delay was neglect of TB symptoms by patients (in 39% of cases), and for health-care system factor delay was a failure (mostly at general and private care levels) to suspect PTB by doctors (in 57% of cases). There were no significant associations between the presence of language barrier, patient occupation or nationality, and diagnostic delay.
Conclusions:
Despite a favorable comparison to other countries, there is a substantial delay in the diagnosis of PTB in Qatar. Relevant actions including health education on TB are required to minimize this delay.
Keywords: Delay, diagnosis, pulmonary tuberculosis
INTRODUCTION
Despite the global falling of tuberculosis (TB) incidence, TB continues to be one of the major threats to mankind. Around 9.6 million new TB cases reported in the year 2014 worldwide with over 1.5 million people died from the disease in the same year.[1] In addition to increasing morbidity and mortality of the source case, delay in pulmonary TB (PTB) diagnosis can lead to multiple secondary cases. It is estimated that a single untreated smear-positive case can lead to more than ten secondary cases annually.[2,3] Early diagnosis of PTB is thus of paramount importance. Although the delay in PTB diagnosis is common to both high- and low-income countries, the magnitude of the problem seems more in the latter and can reach up to 185 days or higher.[4] Qatar is an oil and gas-rich country with the highest gross domestic product (GDP) per capita in the world (2014 estimates)[5] and the highest per capita health expenditure in the Gulf Cooperation Council.[6] TB remains a common health problem in the state of Qatar with an incidence of 40/100,000 populations per year. About 97% of TB patients are expatriates (mostly from Asian countries with high TB prevalence).[7] This is because the country relies heavily on labor force from this part of the world for its economic and industrial projects. Qatar has a highly effective National TB Program with one National TB Reference Laboratory that performs a full range of laboratory diagnosis and a case detection rate exceeding 70%. All medications, laboratory and radiological investigations for diagnosis of TB are provided free-of-charge to all patients.[8] The objectives of this study were to determine the mean and median delays in the diagnosis of PTB and identify patient and health-system reasons for these delays in this wealthy nation.
METHODS
Study design and participants
This was a cross-sectional prospective study of randomly selected adult subjects (defined as ≥15 years old by Qatari health system) with confirmed PTB who were admitted to Hamad General Hospital or TB Unit in Qatar from January 2007 to December 2015. Inclusion criteria included; adult subjects with confirmed diagnosis of PTB by positive acid fast Bacilli smear from sputum or bronchoalveolar lavage (BAL) or a positive sputum mycobacterial TB culture at the time of admission to the hospital, in addition to the presence of symptoms and signs suggestive of PTB. Patients in whom PTB diagnosis was assumed on basis of symptom or radiological findings alone without microbiologic confirmation were excluded from the study. In addition, cases of extra-pulmonary TB and mentally ill patients were also excluded from the study.
Procedures
One hundred patients who fulfilled the inclusion criteria were interviewed face-to-face by one of the investigators to determine the time interval from symptom onset to the confirmation of the diagnosis of PTB. For quality assurance, all investigators received a prior training on how to conduct the interview and fill a structured questionnaire. We defined the total delay in diagnosis of PTB as the time interval from symptom onset to the microbiologic confirmation of PTB. We defined patient-related delay as the time interval from PTB symptom onset to the first visit to any health-care facility in Qatar. Health system-related delay was defined as the time interval from the first care-seeking visit (at any health facility) to the microbiologic confirmation of PTB. Estimation of delay and reasons for patient delay were confirmed directly from questioning patients using a structured questionnaire. Health system-related reasons were confirmed by direct questioning of patients about details of their prior visits to health-care facilities for their PTB symptoms as well as from patient electronic records. Sputum and BAL samples for all these patients were followed after 2 months from the interview to determine the final culture and sensitivity results. The study was approved by the Medical Research Council at Hamad Medical Corporation (Project No 7005/07)
Statistical analysis
Qualitative and quantitative data values were expressed as frequency along with percentage and mean ± standard deviation with median. Descriptive statistics were used to summarize demographic and all other clinical characteristics of the participants. The mean delay with 95% confidence interval (CI) and the median delay with interquartile range (Q1–Q3) were calculated. Associations between factors such as language barrier, occupation, and nationality (that were hard for patients to judge as possible reasons of delay) and the length of delay were assessed using Chi-square test. A two-sided P < 0.05 was considered to be statistically significant. All Statistical analyses were done using Statistical Packages SPSS-21 (SPSS Inc., Chicago, IL, USA).
RESULTS
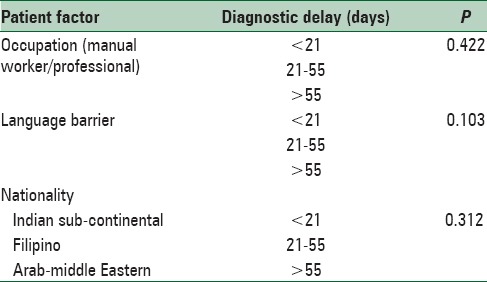
One hundred patients who fulfilled the inclusion criteria and signed consent for the study were included in the analysis (100% participation rate). The characteristics of the study population are shown in Table 1. The mean age at diagnosis was 33.8 (±13.5) years. Reasons for delay in PTB diagnosis are shown in Table 2. The mean and median total diagnostic delays of PTB were 53 (95% CI 42.61–63.59) and 30 (interquartile range; Q1–Q3, 15–60) days, respectively. The mean patient factor delay was 45.7 (95% CI 28.1–63.4) days and the median was 30 (interquartile range; Q1–Q3, 15–60) days. The mean health system factor delay was 46.3 (95% CI 35.46–57.06) days and the median was 30 (interquartile range; Q1–Q3, 18–60) days. Although the lengths of delay were almost equal, health-care system factor was responsible for more cases of delay than patient factor (45% vs. 35% of cases). Among patient factors, minimization (neglect) of PTB symptoms by patients was the most common cause of delay in diagnosis (in 39% of cases) while failure to suspect PTB was the most common health-care system factor (in 57% of cases). Private and general practices were the most common type of doctor practices associated with failure to suspect PTB. There were no significant associations between presence of language barrier, patient occupation or nationality and the delay in PTB diagnosis [Table 3].
Table 1.
Characteristics of the study population
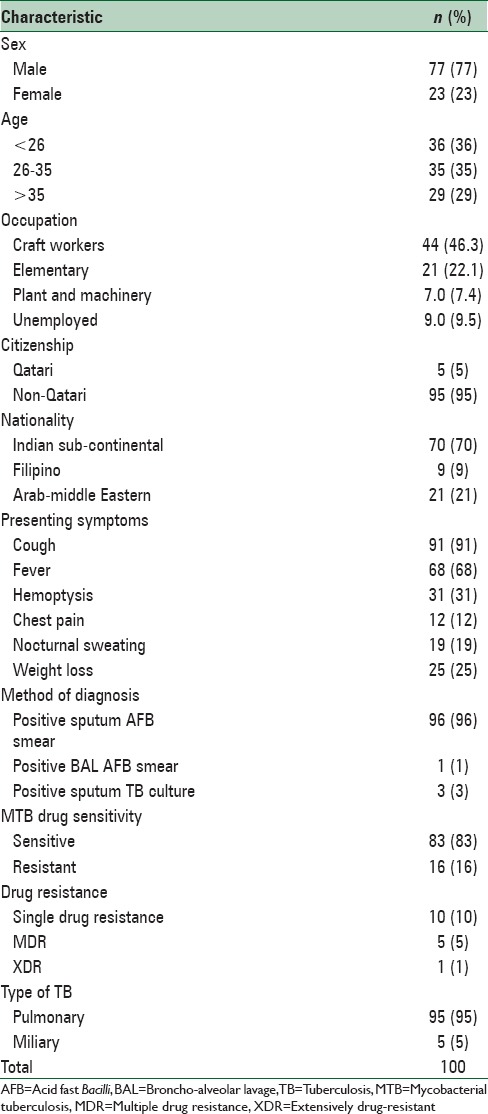
Table 2.
Delay in pulmonary tuberculosis diagnosis

Table 3.
Association between diagnostic delay and patient factors that could not be ascertained from patients as reasons of delay
DISCUSSION
There is no unified definition for the delay in diagnosis of PTB. Different studies have used different definitions such as debut of symptoms, time interval from symptom onset to diagnosis, time from symptom onset to starting treatment, etc.[9] The definition of total delay in this study was similar to most of the previous studies.[9] In addition, there is almost always no delay between microbiologic confirmation and initiating treatment for TB cases in Qatar. Regardless of the definition used, delay in the diagnosis of PTB seems common to both high and low-income countries. The current study demonstrated that Qatar was not an exception. There was a substantial delay in diagnosing PTB in this wealthy country with a median total delay of 30 days. Interestingly, despite this substantial delay, Qatar seems to compare favorably with both developed and developing countries with regard to the median total diagnostic delay. For example, the median total delays of PTB diagnosis in New York (USA), France, Norway, and Turkey are 57, 68, 63, and 49 days, respectively,[10,11,12,13] while in Ethiopia, Nepal, and Ghana are 80, 60, and 104, respectively[14,15,16] with the highest median delay of 126 days reported in Tanzania.[4] Nevertheless, data from each of these countries may not necessarily represent the entire country, and the significant delay in PTB diagnosis in Qatar (despite the highly effective National TB Program and the free high standard public health system) remains striking. In agreement with other studies, health-care system delay in this country was significantly observed at the primary and private health-care sector levels.[17] There are plausible explanations for this observation. First, primary and private health-care sectors usually constitute the first encounter for patients in their early stages of the disease. Second, despite the extensive reforms in the Qatari's health-care system (with the aim to achieve a world-class, patient-centered healthcare system by the year 2030), the newly developed family physician program that replaced the old general practice system is still in its early milestones. Globally, hospitals tend to have more specialized teams and diagnostic technologies (such as microscopes) than health centers.[17] Qatar is witnessing a rapid industrial and economic development with over-reliance on labor force from countries with high TB prevalence with the subsequent rapid turn-over of this labor force. Screening of these workers for infectious diseases on their arrival is mandatory in Qatar; however, counseling and education regarding symptoms and signs of TB is rarely done. This could have contributed to the finding that minimization (neglect) of TB symptoms by patients being the most common cause of patient factor delay. The finding that financial reasons responsible for a small percentage (8%) of patient delay is expected. In Qatar, all high standard governmental health-care services are provided free-of-charge to all residents, regardless of their nationalities or social background. Patients with suspected PTB are isolated in negative-pressure rooms until two sputum samples are negative. Directly observed therapy is provided free-of-charge to all confirmed TB cases. In contrast to what was reported in other studies, we did not find a significant association between the presence of language barrier and delay in diagnosis of PTB.[10] This could be explained by the multi-national structure of health system in Qatar. The majority of patients with TB in Qatar are nationals of the Indian sub-continent and majority of the health-care staff (particularly nursing staff) speak their languages. Manual workers from these countries constitute the majority of TB patients in Qatar; hence, we could not find a significant association between delay in diagnosis of PTB and patient's occupation or nationality. The current study is the first to address the delay in diagnosis of PTB in a country with the highest GDP per capita in the world and a very effective National TB Program. The findings of this study can be generalized to the whole country as Hamad General Hospital and TB Unit constitute the main admitting health-care facilities for TB cases in Qatar. Furthermore, a precise estimate and causes of delay were obtained directly from patients as well as electronic patient records at the time of diagnosis which helped to minimize recall bias. Our study results also reflected the poor public knowledge and awareness about TB symptoms in Qatar. Nevertheless, this study has potential limitations. Among the most important limitations is the fact that associations between levels of education, monthly income and housing conditions (such as crowding) and delay in TB diagnosis were not addressed in the current study. Crowded accommodation of labor workers is one of the suspected modes of transmission of TB in Qatar. It will be interesting to test this hypothesis in future studies and explore its effect on diagnostic delay of PTB. Furthermore, effects of certain diseases and habits such as human immunodeficiency virus infection, chronic diseases, and alcohol/drug abuse on delay in TB diagnosis were not investigated in this study. It should also be addressed that this study did not include patients who were not diagnosed or did not have access to health care.
CONCLUSIONS
Despite a favorable comparison to other countries, there is a substantial delay in the diagnosis of PTB in Qatar. Delay in PTB diagnosis is more due to health-care system factors than patient factors. General and private practices are the most common doctor practices to be associated with delay in PTB diagnosis. There is a range of relevant actions that can be considered to reduce diagnostic delay of PTB in Qatar. Health education on TB (particularly for labor workers) in form of mass campaigns, maintaining appropriate TB awareness in health-care professionals (particularly those in general/private practice) through staff training and workshops, and improving the partnership between general/private practice and National TB Program are examples of such actions.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.World Health Organization. Global Tuberculosis Report. 2015. [Last accessed on 2016 Jan 30]. Available from: http://www.who.int/tb/publications/global_report/en/
- 2.Sepkowitz KA. How contagious is tuberculosis? Clin Infect Dis. 1996;23:954–62. doi: 10.1093/clinids/23.5.954. [DOI] [PubMed] [Google Scholar]
- 3.Styblo K. Current status of the problem.Epidemiology of tuberculosis. Bull Int Union Tuberc. 1978;53:153–66. [PubMed] [Google Scholar]
- 4.Wandwalo ER, Mørkve O. Delay in tuberculosis case-finding and treatment in Mwanza, Tanzania. Int J Tuberc Lung Dis. 2000;4:133–8. [PubMed] [Google Scholar]
- 5.Central Intelligence Agency. The World Fact Book. Estimate. 2014. [Last accessed on 2015 Dec 07]. Available from: https://www.cia.gov/library/publications/the-world-factbook/geos/qa.html .
- 6.World Health Organization. Global Health Observatory Data Repository. Qatar: Statistics Summary (2002-Present) [Last accessed on 2015 Dec 07]. Available from: http://www.apps.who.int/gho/data/node.country.country.QAT .
- 7.Khattab MA, Khan FY, Al Maslamani M, Al-Khal AL, El Gendy A, Al Soub H, et al. Pulmonary and extra pulmonary tuberculosis in Qatar: A first retrospective population-based study. Adv Infect Dis. 2015;5:148–53. [Google Scholar]
- 8.AL-Suwaidi Z. Tuberculosis in Qatar. Int J Mycobacteriol. 2015;4:124. doi: 10.1016/j.ijmyco.2016.10.030. [DOI] [PubMed] [Google Scholar]
- 9.Storla DG, Yimer S, Bjune GA. A systematic review of delay in the diagnosis and treatment of tuberculosis. BMC Public Health. 2008;8:15. doi: 10.1186/1471-2458-8-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sherman LF, Fujiwara PI, Cook SV, Bazerman LB, Frieden TR. Patient and health care system delays in the diagnosis and treatment of tuberculosis. Int J Tuberc Lung Dis. 1999;3:1088–95. [PubMed] [Google Scholar]
- 11.Tattevin P, Che D, Fraisse P, Gatey C, Guichard C, Antoine D, et al. Factors associated with patient and health care system delay in the diagnosis of tuberculosis in France. Int J Tuberc Lung Dis. 2012;16:510–5. doi: 10.5588/ijtld.11.0420. [DOI] [PubMed] [Google Scholar]
- 12.Farah MG, Rygh JH, Steen TW, Selmer R, Heldal E, Bjune G. Patient and health care system delays in the start of tuberculosis treatment in Norway. BMC Infect Dis. 2006;6:33. doi: 10.1186/1471-2334-6-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Okur E, Yilmaz A, Saygi A, Selvi A, Süngün F, Oztürk E, et al. Patterns of delays in diagnosis amongst patients with smear-positive pulmonary tuberculosis at a teaching hospital in Turkey. Clin Microbiol Infect. 2006;12:90–2. doi: 10.1111/j.1469-0691.2005.01302.x. [DOI] [PubMed] [Google Scholar]
- 14.Yimer S, Bjune G, Alene G. Diagnostic and treatment delay among pulmonary tuberculosis patients in Ethiopia: A cross sectional study. BMC Infect Dis. 2005;5:112. doi: 10.1186/1471-2334-5-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Basnet R, Hinderaker SG, Enarson D, Malla P, Mørkve O. Delay in the diagnosis of tuberculosis in Nepal. BMC Public Health. 2009;9:236. doi: 10.1186/1471-2458-9-236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Osei E, Akweongo P, Binka F. Factors associated with delay in diagnosis among tuberculosis patients in Hohoe Municipality, Ghana. BMC Public Health. 2015;15:721. doi: 10.1186/s12889-015-1922-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Makwakwa L, Sheu ML, Chiang CY, Lin SL, Chang PW. Patient and heath system delays in the diagnosis and treatment of new and retreatment pulmonary tuberculosis cases in Malawi. BMC Infect Dis. 2014;14:132. doi: 10.1186/1471-2334-14-132. [DOI] [PMC free article] [PubMed] [Google Scholar]


