Abstract
Background:
Pattern of recurrence of glioblastoma (GBM) seems to have undergone some shifts from distant metastasis as a rarity to a higher proportion, including disease disseminated via cerebrospinal fluid (CSF) pathway. There is still no report on the pattern of recurrence for Chinese population. Here, we evaluated the pattern of recurrence of GBM in Chinese patients along with factors that could affect the distribution of recurrence.
Methods:
Medical records of GBM patients with definite recurrence were reviewed. Local recurrence was defined as tumor regrowth within the preoperative abnormal signals on magnetic resonance imaging (MRI) T2 sequence. New recurrence was a new lesion away from the preoperative T2 abnormalities. New recurrence in contact with CSF pathways was registered as new CSF dissemination. Progress-free survival (PFS) and survival after progress were compared using the Kaplan–Meier survival curves. Potential risk factors for new CSF dissemination were assessed using univariate models followed by multivariate analysis.
Results:
Thirty-six patients were proven to have recurrence; 22 local and 14 new recurrences. Among the 14 patients, 11 had new CSF dissemination. Median PFS for local, new parenchymal recurrence, and new CSF dissemination were 5.5 months, 9.9 months, and 12.1 months, whereas survival after progress were 6.1 months, 5.7 months, and 16.9 months, respectively. The ventricular entry during surgery and the completion of concomitant chemoradiotherapy were risk factors for new CSF dissemination. O6-methylguanine-DNA methyltransferase methylation was associated with the development of CSF dissemination.
Conclusion:
The majority of recurrence remained local (22/36, 61%). However, CSF dissemination was up to 30% (11/36). PFS for patients with CSF dissemination was the longest, and paradoxically survival after progress was the shortest. Ventricular entry should be avoided. Whole craniospinal MRI surveillance should be included for these patients.
Keywords: CSF dissemination, glioblastoma, pattern of recurrence
INTRODUCTION
Glioblastoma (GBM) is the most common primary brain tumor. It is treated aggressively with maximum safe resection followed by irradiation and temozolomide. Although both the progress-free survival (PFS) and the overall survival (OS) are significantly prolonged, recurrence is inevitable for almost every patient.
Several studies have evaluated the pattern of recurrence of GBM after concomitant chemoradiotherapy (CCRT) has become a standard treatment. Recent studies reported that temozolomide might have impacted the timing and distribution of recurrence.[15] With intense local control and longer survival, the pattern of recurrence of GBM may have changed from distant spread as rarity to a higher proportion.[3,6,15] Molecular markers such as O6 -methylguanine-DNA methyltransferase (MGMT) methylation not only contributed to the prolonged survival duration but also increased the proportion of distant metastasis.[3] Some authors even suggested that surgical manipulation including the extent of resection[6] or ventricular entry during surgery[10,17] could alter the pattern of recurrence. Cerebrospinal fluid (CSF) spread of GBM, an indication of terminal stage for patients, is also becoming another increasing thorny problem for clinicians in recent years because scarce effective options could be offered.[12,18]
There is still no presented report on the pattern of recurrence for Chinese population; hence, we reviewed the brain tumor registry of the CUHK Otto Wong brain tumor center from 2009 to 2013 to evaluate the pattern of recurrence of GBM in Chinese patients. By subgrouping them according to different factors including the extent of resection, ventricular entry during surgery, MGMT status, usage of steroid, and concurrent chemotherapy, we explored potential factors that might cause CSF dissemination recurrence.
MATERIALS AND METHODS
Patients eligibility
We reviewed medical records of patients with the diagnosis of GBM from 2009 to 2013. Patients were eligible for the study if they underwent surgical excision for GBM and completed the preplanned irradiation. Those who had primary infratentorial GBM or failed in following the scanning protocol were excluded.
Methylation-specific polymerase chain reaction (MSPCR) was adopted in our institution, which was previously described by our group.[7]
Radiotherapy
Radiotherapy was delivered in a conventionally fractionated 6-week regimen, consisting of a total dosage of 60 Gy given in 30 fractions. For contouring methodology, a consistent protocol with either EORTC/NCIC or RTOG was used in our institution. For the tumors with relatively small volume of edema, EORTC/NCIC guideline was adopted. If tumors resulted in massive edema seen on T2-weighted sequence, the RTOG guideline would be introduced with the aim to cover the edematous volume.
Chemotherapy
Temozolomide was prescribed concurrently during radiotherapy at 75 mg/d/m2 for 6 weeks, followed by 6 or more cycles of maintenance TMZ at a dosage of 150–200 mg/d/m2 for 5 consecutive days every 28 days. No other chemotherapeutic agents were prescribed. Temozolomide would be suspended if true recurrence or drug-related toxicity was detected or a minimum of 6-cycle maintenance was accomplished.
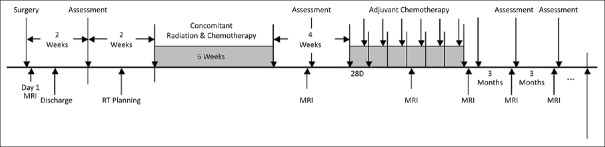
Follow-up schedule and pattern of recurrence
Patients were followed up with both clinical and radiological assessments. As a standard practice, all recruited patients were subjected to the scanning protocol with an MRI scan on postoperative day 1, 2 weeks after the completion of radiotherapy, and then every 3 months thereafter [Figure 1]. Postoperative day 1 MRI was usually performed within 24 hours after the tumor excision, or no later than 48 hours, so as to define the extent of resection and detect any residual tumor. Total resection was defined as no residual contrast enhancement seen on MRI T1 sequence. Anything less than total resection was a qualifier of subtotal resection. The postoperative day 1 MRI also served as the baseline MRI for future comparison of recurrence.
Figure 1.
Scanning Protocol. MRI denotes for magnetic resonance imaging, RT for radiotherapy and D for days
An experienced neuroradiologist (specialist or consultant) was responsible for determining radiographic recurrence in accordance to the McDonald's Criteria.[13] The issue of pseudoprogression was resolved by reviewing clinical notes during follow-up and series of interval MRI scans. Once recurrence was diagnosed, the ongoing therapy would be regarded as treatment failure. The data on the received best treatment would be recorded.
Local recurrence implied that the growth of contrast enhancement at primary tumor bed or within the T2 abnormalities of the preoperative image. New recurrence was an enhancing lesion that appeared separately from the primary T2 abnormalities. New recurrences situated in brain parenchyma were classified as parenchymal infiltration. While the new recurrences with new ependymal enhancement away from the primary tumour site along the ventricle lining or intraventricular lesion or spinal metastasis would be termed as CSF. Dosimetric classification would be applied for the CSF disseminated cases. If more than 95% of the lesion fell within the 95% isodose line of 60 Gy, it would then be categorized as “in-field,” 20–95% as “marginal,” and less than 20% as “out-field.”
The cases in which local recurrence appeared synchronously with new recurrence would be assigned as new recurrence.
Statistical analysis
Both PFS and OS were calculated from the excision of GBM to disease recurrence and death. Survival after progress was from the time of diagnosis of recurrence to death. The Kaplan–Meier survival curve was used for survival comparison. The Log-rank test was chosen to investigate the divergence among groups with different types of recurrence.
It is known that GBM can spread along the white matter tract in parenchymal. The primary interest of this study was CSF dissemination of GBM; we grouped local and new parenchymal recurrence together during the risk factor analysis. Regarding exploring factors for CSF dissemination, ventricular entry, extent of resection (EOR), MGMT promotor status, use of baseline steroid, concurrence, and completion of temozolomide, primary or secondary GBM were labelled as categorical variants in the univariate analysis. Age was regarded as a continuous factor. Chi-Square test, Fischer's exact test and discriminant analysis were chosen accordingly to test the significant level. A variant with a P value of less than 0.05 was regarded as a potential candidate for the multivariate analysis. A binary logistic regression model with a backward stepwise procedure was applied to generate the possible best predicting model for new CSF dissemination. Factors with a P value of less than 0.05 were regarded as statistically significant. All analyses were done with Statistical Package for the Social Sciences Version 22 (SPSS, IBM Corporation, Armonk, New York).
This study was conducted according to the Declaration of Helsinki with the approval issued by the Joint Chinese University of Hong Kong-New Territories East Cluster Clinical Research Ethic Committee in May 2015 (CRE Ref No. 2015-272).
RESULTS
Demography
From 2009 to 2013, 44 consecutive adult patients were diagnosed with GBM in the Prince of Wales Hospital; all the 44 patients accomplished radiotherapy with a median dosage of 60 (range, 40.5–60) Gy. Median time interval between surgery for GBM and radiotherapy was 36 (range, 14–62) days. Five patients were alive at the end of the study; among them 2 had disease recurrence. PFS and OS for the 44 patients were 6.1 (range, 1.0–46.8) months and 13.3 (range, 1.4–62.0) months, respectively.
Pattern of recurrence
Three patients did not experience recurrence at their last follow-up by the end of the study, with a median follow-up period of 28.8 months. Five patients deteriorated rapidly after radiotherapy and succumbed before a determinant MRI to assess the tumor growth morphologically. These patients were not included in the pattern of recurrence analysis.
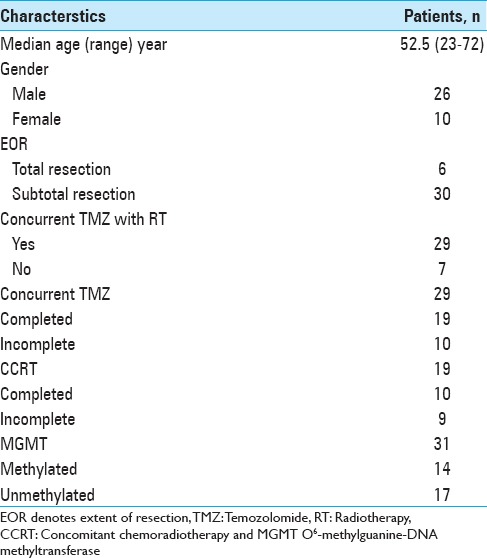
Thirty-six patients were confirmed to be eligible for studying the pattern of recurrence [Table 1]. Seven out the 36 patients did not receive temozolomide due to financial difficulty. Twenty-nine patients received temozolomide after surgery. Among them, 10 were able to complete the CCRT. For the remaining 19 patients, the suspension of temozolomide was due to disease progression for 13 patients and persistent side effects for 4 patients. Initiation of concurrent temozolomide was delayed for 2 patients for 11 days and 14 days after starting irradiation due to financial reasons.
Table 1.
Basic characteristics for 36 patients
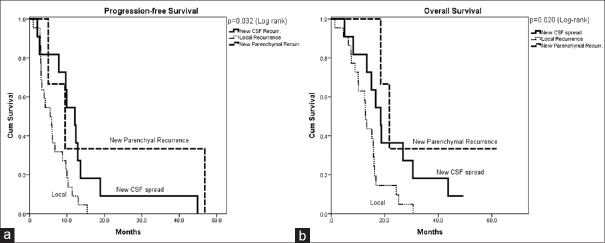
PFS for these 36 patients was 6.8 months and the overall survival was 15.2 months. Recurrence was local in 22 patients (61.1%) [Figure 2a–c] and new in 14 patients (38.9%). For the 14 patients who had new recurrence, 3 were new parenchymal infiltration [Figure 2d–f], and 11 were new CSF dissemination [Figure 2g–i]. Six out of the 11 patients had preoperative ependymal enhancement. The time to develop CSF dissemination was significantly longer. The median time to progress for local, new parenchymal recurrence, and new CSF dissemination were 5.5 months, 9.9 months, and 12.1 months (P = 0.032, log-rank) [Figure 3a], whereas the median overall survival were 12.8 months, 21.7 months, and 18.5 months, respectively (P = 0.020, log-rank) [Figure 3b]. Comparing survival after progression, although without statistical significance, patients with CSF dissemination of disease had the shortest longevity of only 5.7 months, followed by 6.1 for local recurrence and 16.9 for parenchymal infiltration (P = 0.280, log-rank). This might indicate that, despite having longer PFS, the survival after progression for patients with CSF dissemination was ultimately more brief.
Figure 2.
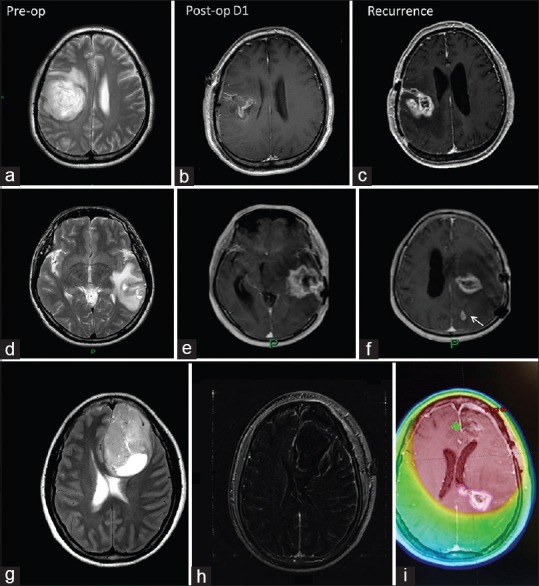
Illustrations for patterns of recurrence. (a-c) Local recurrence, (d-f) new parenchymal infiltration, (g-i) New CSF dissemination; (g) pre-operative MRI showing left frontal lobe GBM; 2h. MRI T1 + C fat subtraction suggested total resected lesion; (i) MRI T1 + C showing new enhancing metachronous lesion with subependymal enhancement (100% within irradiation high-dose zone) 12.4 months after surgery. MRI denotes for magnetic resonance imaging, Pre-op for Pre-operation, Post-op D1 for post-operative day 1
Figure 3.
Kaplan-Meier Survival Curve for 36 eligible patients. (a) Progression free survival curves for 3 patterns of recurrence; (b) overall survival curves for 3 patterns of recurrence
When applying dosimetric method onto CSF-spread cases, recurrences were in-field in 4 patients, marginal in 1, and out-field in 6 patients. Five (45.5%) patients developed CSF dissemination despite stable local disease. Six (54.5%) patients suffered from symptomatic CSF spread of disease, including paraparesis in 2, hemiparesis in 2, bilateral facial palsy in 2, ataxia in 2, and double incontinence in 1 patient.
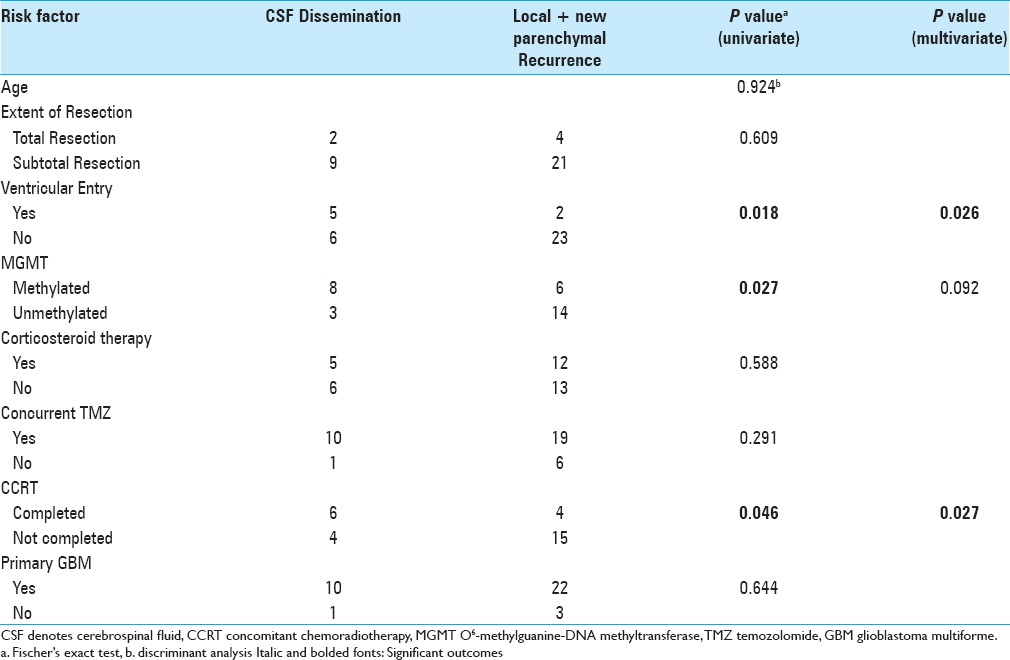
Risk factor comparison
Age was assessed to be a continuous factor and was not a factor for CSF dissemination (P = 0.924, discriminant analysis). Extent of resection did not result in divergent distribution of recurrence. No difference was identified between primary and secondary GBM, neither was the prescription of steroid.
The concurrent use of temozolomide (some versus none) did not alter pattern of recurrence whereas completion of CCRT was correlated to a prevalence of developing CSF dissemination.
Methylated MGMT promotor status (P = 0.028, Fischer's exact test) and ventricular entry during surgery (P = 0.018, Fischer's exact test) were both significant for subsequent CSF dissemination.
After multivariate analysis, completion of CCRT (P = 0.027), and ventricular entry (P = 0.026) were the most important risk factors for CSF dissemination [Table 2].
Table 2.
Univariate and multivariate analyses for risk factors
DISCUSSION
Classification of recurrence
CCRT has been a remarkable milestone for the management of GBM. These combined therapies can significantly lengthen the survival of the patients. However, recurrence is still inevitable. Although the highest tolerable dose of irradiation has already been prescribed to the tumor bulk and its adjacent tissue,[4] the majority of tumor recurrence remained local. There is still no unified classification for the pattern of recurrence, especially “non-local” recurrence. Previous studies usually categorized tumor spread by either dosimetric method or by the distance to the primary tumor bulk.
In this study, we presented a radiological methodology for patterns of recurrence. The accuracy in delineation of GBM is improved by utilization of MRI, especially by using T2-weighed and fluid-attenuated inversion recovery (FLAIR) sequences, for their sensitivity in picking up non-enhancing infiltrative tissue. Moreover, T2 sequence has superiority in picking up signals suggesting edema, where it is believed to shelter scarce GBM cells.[11] It is recommended by the Radiation Therapy Oncology Group that gross tumor volume should be contoured with computed tomography plus either T2 or FLAIR sequence. Thus, using T2-weighed and FLAIR as reference for distinguishing local from non-local recurrence (new parenchymal lesion) are comprehensible and straightforward.
With the presented methodology, differentiation between CSF dissemination and parenchymal infiltration of GBM is also feasible. It is believed that the GBM cells would be able to spread freely and widely within the CSF space if they invaded basal membrane with implantation in the subependyma and choroid plexus.[9] Direct invasion of ependymal and tumor fragmentation in contact with CSF are related to CSF dissemination.[12] Given the information, it is alarming for a clinician to highly suspect CSF dissemination of disease upon detection of ependymal contrast enhancement on MRI. The reported incidence of CSF dissemination of GBM varies from 2 to 25%,[1,10,20] whereas the symptomatic one was around 1.3 to 8.8% only.[16] A more recent review suggested that CSF spread has been increasing steadily over the past few years maybe because of the improvement of imaging modalities as well as prolonged survival.[18]
The current best laboratory study for the diagnosis of CSF spread of malignancy is CSF cytology. While even for patients with genuine leptomeningeal metastasis, 55% of them will have initial false negative CSF cytological results, not mentioning the remaining chances of misdiagnosis still remains up to 14% after 3 lumbar punctures. This high false-negative rate is meaningful for clinical practice. Other abnormalities yield from CSF examinations such as elevated opening pressure or protein level are only suggestive instead of diagnostic.[5] Because CSF dissemination of GBM takes place in terminal stage of disease and the outcome is always dismal,[12] with extremely shortened survival, we are reluctant to administer invasive procedure with such a high false-negative rate.
More importantly, we also demonstrated that the new lesions widely disseminated via CSF could grow within the irradiation high-dose zone. These tumors were usually labelled as central or in-field recurrence (local recurrence) by other studies. This would indicate that conventional dosimetric classification for pattern of recurrence suffered from the drawback of categorizing atypical recurrences.
MGMT methylation
With the ongoing studies focusing on different aspects of the MGMT methylation status, MGMT methylation might also have some impacts on recurrence. Brandes et al. showed that the incidence of distant recurrence for patients with methylated MGMT status was significantly higher than that for patients with non-methylated MGMT status, which were 42 and 15%, respectively.[3]
GBM cells with methylated promotor status are vulnerable to irradiation especially when given concurrently with temozolomide. However, pharmacokinetic study suggested that the efficacious dose of temozolomide for eliminating GBM cells could not be reached within the CSF space.[2,8] It is also fair to theorize that CCRT resulted in therapeutic pressure onto the lesion and might also simultaneously select GBM cells, which have the propensity to migrate and subsequently harbor in the CSF space. The abovementioned hypothesis could also explain the finding of 5 out of 11 patients who received temozolomide suffering from CSF dissemination with stable primary lesion in our study.
Ventricular entry
Whether the ventricular entry during surgery could raise the incidence of CSF spread has remained controversial among studies for decades.[8,10,17] CSF could be contaminated with GBM cells after surgically breaching the ventricular lining. The vitality of dispersed GBM cells, no matter caused by contamination or being pre-existed, could be suppressed by immune reactions within the CSF space. While the current intensive treatments including irradiation and chemotherapy for GBM, in addition to bringing outstanding curative effect intracranially, they are suspected to be causative of compromised immune function, and thus favor those cells with ability and the time needed to propagate within CSF space.[19]
Prolonged survival
Despite no statistical significance, patients suffered from CSF spread of disease who had perceived seemingly better disease control and held the shortest longevity after progression. Thus, early recognition of CSF spread is increasingly important. With improved local control of primary disease as well as survival, CSF spread of disease is becoming an arduous challenge that needs to be tackled.
As both the completion of CCRT and methylated MGMT promotor status in GBM are associated with prolonged patient survival, it is also very reasonable to speculate that these patients live long enough for this rarely seen but possible tumor behavior to occur. Literature suggests that the time for the CSF spread to be manifested ranged from 12–15 months post-surgery,[14,15] which was concordant with longer PFS for patients with MGMT methylated GBM as well as that for patients treated with CCRT in our study. Similar findings were also present in some of the pattern of recurrence studies.[3,15] With the prolonged stable phase, GBM could no longer be regarded simply as local but rather a neuroaxis disease.
Our center looks after about 20 to 30 new cases of GBM annually. A combined neuro-oncology clinic was established in 2009 to serve this group of patients for intensive chemoradiotherapy. A brain tumor registry and clinical and radiological follow-up system was setup. Regarding the limitation of the present study, we acknowledge that the sample size of our cohort was too small to perform further analysis. Since 2011, temozolomide can be provided to all patients with a safety net. Before that, the use of TMZ depended very much on patient's financial status. In addition, due to its retrospective nature, comparisons were difficult to carry out and the conclusions might be preliminary. A collaborative study involving centers with similar treatment and follow-up protocol can be contemplated in the future.
CONCLUSION
In conclusion, our study showed that the incidence of CSF spread of GBM was prominent in Chinese population despite the majority of the recurrence still being located within the original tumor bed. Ventricular entry during excision of GBM should be avoided. Patients who are able to complete CCRT have a risk for CSF dissemination. GBM patients with methylated MGMT promotor status are prone to suffer from CSF dissemination recurrence. Surveillance MRI for whole neuroaxis (brain and spine) should be considered, especially for patients with longer PFS.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Contributor Information
Danny T. M. Chan, Email: tmdanny@surgery.cuhk.edu.hk.
Sonia Y. P. Hsieh, Email: sonia@surgery.cuhk.edu.hk.
Michael K. M. Kam, Email: kamkm@yahoo.com.
Tom C. Y. Cheung, Email: tom_cycheung@yahoo.com.
Stephanie Chi P. Ng, Email: staphanieng@surgery.cuhk.edu.hk.
Wai S. Poon, Email: wpoon@cuhk.edu.hk.
REFERENCES
- 1.Arita N, Taneda M, Hayakawa T. Leptomeningeal dissemination of malignant gliomas. Incidence, diagnosis and outcome. Acta Neurochir. 1994;126:84–92. doi: 10.1007/BF01476415. [DOI] [PubMed] [Google Scholar]
- 2.Beier DR. Temozolomide preferentially depletes cancer stem cells in glioblastoma. Cancer Res. 2008;68:5706–15. doi: 10.1158/0008-5472.CAN-07-6878. [DOI] [PubMed] [Google Scholar]
- 3.Brandes AA, Tosoni A, Franceschi E, Sotti G, Frezza G, Amistà P, et al. Recurrence pattern after temozolomide concomitant with and adjuvant to radiotherapy in newly diagnosed patients with glioblastoma: Correlation With MGMT promoter methylation status. J Clin Oncol. 2009;27:1275–9. doi: 10.1200/JCO.2008.19.4969. [DOI] [PubMed] [Google Scholar]
- 4.Brandsma D, Stalpers L, Taal W, Sminia P, van den Bent MJ. Clinical features, mechanisms, and management of pseudoprogression in malignant gliomas. Lancet Oncol. 2008;9:453–61. doi: 10.1016/S1470-2045(08)70125-6. [DOI] [PubMed] [Google Scholar]
- 5.Chamberlain MC. 15 - Neoplastic Meningitis. In: Rees J, Wen PY, editors. Blue Books of Neurology. Vol. 36. Butterworth-Heinemann; 2010. pp. 333–51. ISSN 1877-184X, ISBN 9780750675161. [Google Scholar]
- 6.De Bonis P, Anile C, Pompucci A, Fiorentino A, Balducci M, Chiesa S, et al. The influence of surgery on recurrence pattern of glioblastoma. Clin Neurol Neurosurg. 2013;115:37–43. doi: 10.1016/j.clineuro.2012.04.005. [DOI] [PubMed] [Google Scholar]
- 7.Dong SM, Pang JC, Poon WS, Hu J, To KF, Chang AR, et al. Concurrent hypermethylation of multiple genes is associated with grade of oligodendroglial tumors. J Neuropathol Exp Neurol. 2001;60:808–16. doi: 10.1093/jnen/60.8.808. [DOI] [PubMed] [Google Scholar]
- 8.Elliott JP, Keles GE, Waite M, Temkin N, Berger MS. Ventricular entry during resection of malignant gliomas: Effect on intracranial cerebrospinal fluid tumor dissemination. J Neurosurg. 1994;80:834–9. doi: 10.3171/jns.1994.80.5.0834. [DOI] [PubMed] [Google Scholar]
- 9.Giese A Westphal M. Glioma invasion in the central nervous system. Neurosurgery. 1996;39:235–50. doi: 10.1097/00006123-199608000-00001. [DOI] [PubMed] [Google Scholar]
- 10.Grabb PA, Albright AL, Pang D. Dissemination of supratentorial malignant gliomas via the cerebrospinal fluid in children. Neurosurgery. 1992;30:64–71. doi: 10.1227/00006123-199201000-00012. [DOI] [PubMed] [Google Scholar]
- 11.Halperin EC, Bentel G, Heinz ER, Burger PC. Radiation therapy treatment planning in supratentorial glioblastoma multiforme: An analysis based on post mortem topographic anatomy with ct correlations. Int J Radiat Oncol. 1989;17:1347–50. doi: 10.1016/0360-3016(89)90548-8. [DOI] [PubMed] [Google Scholar]
- 12.Lawton CD, Nagasawa DT, Yang I, Fessler RG, Smith ZA. Leptomeningeal spinal metastases from glioblastoma multiforme: Treatment and management of an uncommon manifestation of disease. J Neurosurg Spine. 2012;17:438–48. doi: 10.3171/2012.7.SPINE12212. [DOI] [PubMed] [Google Scholar]
- 13.Macdonald DR, Cascino TL, Schold SC, Cairncross JG. Response criteria for phase II studies of supratentorial malignant glioma. J Clin Oncol. 1990;8:1277–80. doi: 10.1200/JCO.1990.8.7.1277. [DOI] [PubMed] [Google Scholar]
- 14.Maslehaty H, Cordovi S, Hefti M. Symptomatic spinal metastases of intracranial glioblastoma: Clinical characteristics and pathomechanism relating to GFAP expression. J Neurooncol. 2011;101:329–33. doi: 10.1007/s11060-010-0257-y. [DOI] [PubMed] [Google Scholar]
- 15.Milano MT, Okunieff P, Donatello RS, Mohile NA, Sul J, Walter KA, Korones DN. Patterns and Timing of Recurrence After Temozolomide-Based Chemoradiation for Glioblastoma. Int J Radiat Oncol. 2010;78:1147–55. doi: 10.1016/j.ijrobp.2009.09.018. [DOI] [PubMed] [Google Scholar]
- 16.Ng WH, Yeo TT, Kaye AH. Spinal and extracranial metastatic dissemination of malignant glioma. J Clin Neurosci. 2005;12:379–82. doi: 10.1016/j.jocn.2004.11.004. [DOI] [PubMed] [Google Scholar]
- 17.Noh JH, Lee MH, Kim WS, Lim DH, Kim ST, Kong DS, et al. Optimal treatment of leptomeningeal spread in glioblastoma: Analysis of risk factors and outcome. Acta Neurochir. 2015;157:569–76. doi: 10.1007/s00701-015-2344-5. [DOI] [PubMed] [Google Scholar]
- 18.Pietschmann S, von Bueren AO, Henke G, Kerber MJ, Kortmann RD, Müller K. An individual patient data meta-analysis on characteristics, treatments and outcomes of the glioblastoma/gliosarcoma patients with central nervous system metastases reported in literature until 2013. J. Neurooncol. 2014;120:451–7. doi: 10.1007/s11060-014-1596-x. [DOI] [PubMed] [Google Scholar]
- 19.Seiz M, Nölte I, Pechlivanis I, Freyschlag CF, Schmieder K, Vajkoczy P, et al. Far- distant metastases along the CSF pathway of glioblastoma multiforme during continuous low-dose chemotherapy with temozolomide and celecoxib. Neurosurg Rev. 2010;33:375. doi: 10.1007/s10143-010-0253-x. [DOI] [PubMed] [Google Scholar]
- 20.Vertosick FT, Selker RG, Vertosick Jr FT, Selker RG. Brain stem and spinal metastases of supratentorial glioblastoma multiforme: A clinical series. Neurosurgery. 1990;27:516–22. doi: 10.1097/00006123-199010000-00002. [DOI] [PubMed] [Google Scholar]