Abstract
Background
Chitosan oligosaccharide (COS) is widely consumed as a functional food due to its multiple health effects, but few studies about COS supplement on placental antioxidant and nutrition transport capacity were reported. Taken pregnant sow as a model, we aimed to investigate the effects of dietary COS supplementation during late gestation on placental amino acids transport and antioxidant defense capacity of sows. From day (d) 85 of gestation to parturition, sixteen pregnant sows were divided into a control group (basal diet without COS supplementation) and a COS group (30 mg COS/kg basal diet). Plasma sample of sow was collected on d 110 of gestation, and placenta tissue was obtained during parturition. Then plasma antioxidant enzyme’s activities, the relative level of oxidant stress related genes, amino acids transport related genes and mTOR pathway molecules in placenta were determined.
Results
Results showed that maternal dietary supplementation with COS increased (P < 0.05) plasma total SOD, caused a downtrend in plasma MDA (0.05 < P < 0.10) on d 110 of gestation. Interestingly, the mRNA expression of some antioxidant genes in the placenta were increased (P < 0.05) and pro-inflammatory cytokines were reduced (P < 0.05) by COS supplement, whereas no significant difference was observed in the activities of placental total SOD and CAT between two groups. Additionally, further study demonstrated that COS feeding stimulated mTOR signaling pathway, increased amino acids transporters expression in placenta.
Conclusions
These observations suggested that COS supplement in sow’s diet during late gestation enhanced antioxidant defense capacity of sows, promoted placental amino acids transport, which may contribute to the health of sows and development of fetus during gestation.
Keywords: Chitosan oligosaccharides, Antioxidant defense, Amino acids transport, Sow
Background
Pregnancy is a state of oxidative stress arising from increased placental mitochondrial activity and production of reactive oxygen species (ROS), including nitric oxide, carbon monoxide, and peroxynitrite, which have pronounced effects on placental function including trophoblast proliferation and differentiation and vascular reactivity [1]. The oxidant/antioxidant status affects the entire unit mother-placenta-fetus, but the disturbance of which during pregnancy may be one of the key downstream mediators that initiate programming of the offspring [2]. Excessive free radical production may cause both lipid and protein oxidation and impair normal endothelial cell function [3]. In this regard, oxidative stress and/or low intake of antioxidant involved in the etiopathogenesis of the most frequent disorders in the gestational period, which was closely related to reproductive performance of sows [4]. Consequently, supplementation with antioxidant in sow’s diet during late gestation and lactation periods is necessary.
As a natural polysaccharide, COS is the depolymerized product of chitosan, and has good solubility in water and various biological activities, including immune-stimulant [5], anti-inflammatory [6] and antioxidant properties [7]. Numerous studies have shown that chitosan has beneficial effects on relieving the oxidative stress [8]. Moreover, placenta, as the main interface between the mother and the fetus, has many functions to perform, including producing and secrete hormones and cytokines, and mediatting the transfer of nutrients, oxygen and waste products [9]. Nutrients pass from the maternal to the fetal blood across the syncytiotrophoblast and the endothelium of the fetal capillaries, therefore main determinant of fetal growth is placental nutrient transport, which is essential for fetal growth and development [10]. Jansson et al. (2006) found the pregnant rats subjected to protein malnutrition during gestation down-regulated placental amino acid transport, which may contribute directly to the development of IUGR [11].
Our previous study has found that maternal COS supplement increased birth weight and growth rate of piglets [12], and postpartum upregulates cholesterol accumulation in suckling piglets [13]. Therefore, we hypothesised that supplementation with COS in sow diets could affect the function of the placenta. The aim of the present study was to investigate the effects of maternal supplementation with COS during late gestation on the antioxidant defense capacity and the amino acids transport in placenta.
Methods
Animals and experimental treatment
Sixteen pregnant sows (Large White × Landrace) with the same parturition history were obtained from an experimental livestock farm (Twins, Inc., JiangXi, China), and fed one of two experimental diets from 85 days of gestation to parturition (8 sows/diet). The experiment last for about 30 days. Sows were randomly divided into two groups, 1) all sows were fed with basal diet (Control) (n =20), 2) all sows were fed with basal diet containing 0.03 ‰ (wt/wt) COS (ZTH Tech. Co., Beijing, China), and the dose of chitosan oligosaccharides was determined by preliminary experiment [14]. The gestation diet formulations have been formulated to meet or exceed all the requirements for gestating sows as referred in our previous study [15]. Sows had free access to water at all times. The diet composition was list in Table 1.
Table 1.
Composition of gestation and lactation diet (as-fed basis)
| Item | Control | COS | Item | Control | COS |
|---|---|---|---|---|---|
| Ingredient (%) | Nutrient composition | ||||
| Corn | 70.30 | 70.30 | DM, % | 88.2 | 88.2 |
| Soybean meal | 12.00 | 12.00 | ME, MJ/kg | 13.5 | 13.5 |
| Wheat middling | 4.00 | 4.00 | CP, % | 14.7 | 14.7 |
| Rice bran meal | 3.00 | 3.00 | Lys, % | 0.78 | 0.78 |
| Puffed soybean | 3.00 | 3.00 | Met + Cys, % | 0.69 | 0.69 |
| Salt | 0.35 | 0.35 | Ca, % | 0.92 | 0.92 |
| Potassium chloride | 0.75 | 0.75 | Total P, % | 0.67 | 0.67 |
| Vitamin-mineral Premixa | 3.00 | 3.00 | |||
| Dicalcium phosphate | 2.20 | 2.20 | |||
| Limestone | 0.50 | 0.50 | |||
| Soy oil | 0.50 | 0.50 | |||
| Mold-inhibiter | 0.09 | 0.09 | |||
| DL-Met | 0.06 | 0.06 | |||
| L-Thr | 0.05 | 0.05 | |||
aPremix provided the following per kg of diet: Fe (FeSO4 · H2O), 80 mg; Mn (MnSO4 · 5H2O), 45 mg; Zn (ZnO), 100 mg; Cu (CuSO4 · 5H2O), 20 mg; I (KI), 0.70 mg; Se (Na2SeO3 · H2O), 0.25 mg; vitamin A, 10,000 IU; vitamin D3, 2,500 IU; vitamin E, 100 IU; vitamin K, 10 IU; vitamin B2, 10 mg; vitamin B6, 1 mg; vitamin B12 50ug; biotin, 80ug; folic acid, 5 mg; nicotinic acid, 15 mg; choline chloride 1500 mg
The degree of polymerization of COS used in this experiment was 2–7 and was purchased from Zhong Tai He technology co., LTD.
Sample collection
In this study, eight sows/group were randomly selected for sample collection. On d 110 of gestation, a five-mL blood sample of sow was collected from the ear vein. Plasma sample was then obtained by centrifugation at 3,000 × g for 10 min at 4 °C and immediately stored at –80 °C for antioxidant analysis [16]. During parturation, a part of placenta/sow tissue was obtained and immediately frozen in liquid nitrogen and stored at –80 °C until required for analysis.
Measurement of antioxidant enzyme’s activities or oxidant injury product
Plasma glutathione peroxidase (GSH-Px), total superoxide dismutase (T-SOD), catalase (CAT) and malondialdehyde (MDA) in the placenta and plasma were determined by assay kits (Nanjing Jiancheng Biotechnology Institute, Nanjing, China) according to the manufacturer’s instructions.
About 0.5 g placenta tissue was powered in liquid nitrogen and dissolved in 5 mL PBS solution. The total superoxide dismutase and catalase in the supernatant of placenta were determined by ELISA kits (BlueGene, Shanghai, China) according to the manufacturer’s instructions. All samples were measured by UV/visible spectrophotometer (UV-2450, Shimadzu, Kyoto, Japan).
RNA isolation and real-time polymerase chain reaction
Total RNA of placenta was isolated using TRIzol reagent (Life Technologies, Tokyo, Japan) according to the manufacturer’s protocol. The concentration of total RNA in each sample was quantified spectrophotometrically at 260 nm and established by 260/280 values to assess RNA quality. The mRNA expression of placental genes and β-actin were quantified by SYBR real-time polymerase chain reaction (PCR) (SYBR Premix Ex Taq; Takara bio Inc., Shiga, Japan). Primers were designed with Primer 5.0 according to the gene sequence of pigs (http://www.ncbi.nlm.nih.gov/pubmed/) to produce an amplification product (Table 2). The amplification reactions were carried out in an ABI Prism 7900 HT sequence detection system (Applied Biosystems, Foster, CA). The relative level of mRNA expression was calculated using the 2−ΔΔCt method after normalization with β-actin as a housekeeping gene.
Table 2.
Primers used for real-time PCR analyzing
| Genes | Nucleotide sequence of primers (5’–3’) | Size (bp) | Ref. |
|---|---|---|---|
| Gpx1 | F: TGGGGAGATCCTGAATTG R: GATAAACTTGGGGTCGGT |
183 | [19] |
| Gpx4 | F: GATTCTGGCCTTCCCTTGC R: TCCCCTTGGGCTGGACTTT |
172 | |
| Ucp2 | F: CCAATGTCGCTCGTAATG R: TGGCAGGGAAGGTCATC |
109 | |
| p53 | F: CTGCTTCCTGAAAACAACC R: AAGGGACAAAGGACGACA |
199 | |
| Mn-SOD | F: GGACAAATCTGAGCCCTAACG R: CCTTGTTGAAACCGAGCC |
159 | |
| Cu/Zn-SOD | F: CAGGTCCTCACTTCAATCC R: CCAAACGACTTCCASCAT |
255 | |
| CAT | F: CGAAGGCGAAGGTGTTTG R: AGTGTGCGATCCATATCC |
374 | This study |
| Hsp70 | F: GCCCTGAATCCGCAGAATA R: TCCCCACGGTAGGAAACG |
152 | [17] |
| TNFα | F: CCACGTTGTAGCCAATGTCA R: CAGCAAAGTCCAGATAGTCG |
395 | |
| IL-6 | F: TCAGTCCAGTCGCCTTCTCC R: GGCATTTGTGGTGGGGTTAG |
494 | |
| IL-8 | F: CTGGCTGTTGCCTTCTTG R: TCGTGGAATGCGTATTTATG |
113 | |
| IL-1β | F: GCTAACTACGGTGACAACAA R: TCTTCATCGGCTTCTCCACT |
196 | |
| EAAT1 | F: GATGGGACCGCCCTCTAT R: CGTGGCTGTGATGCTGATG |
105 | This study |
| EAAT2 | F: GGCTGCTGGACAGGATGA R: TAAATGGACTGGGTCTTGGT |
154 | This study |
| PAT1 | F: TGTGGACTTCTTCCTGATTGTC R: CATTGTTGTGGCAGTTATTGGT |
125 | This study |
| PAT2 | F: GGGCTACTTGCGGTTCGG R: GCGCTTTGACACCTGGGAG |
181 | This study |
| LAT1 | F: TTTGTTATGCGGAACTGG R: AAAGGTGATGGCAATGAC |
155 | This study |
| ASCT2 | F: GATTGTGGAGATGGAGGATGTGG R: GCGAGTGAAGAGGAAGTAGATGA |
128 | |
| PEPT1 | F: CATCGCCATACCCTTCTG R: TTCCCATCCATCGTGACATT |
143 | |
| SNAT2 | F: TACTTGGTTCTGCTGGTGTCC R: GTTGTGGGCTGTGTAAAGGTG |
212 | This study |
| VEGF-A | F: CAACGACGAAGGTCTGGAGTG R: GCCTCGCTCTATCTTTCTTTGG |
155 | [15] |
| β-actin | F: CGTTGGCTGGTTGAGAATC R: CGGCAAGACAGAAATGACAA |
132 | This study |
Total protein extraction and western blotting
Placental tissue were pulverized in liquid nitrogen and lysed in RIPA buffer (Beyotime Biotechnology, China) plus 1 mM PMSF and 1 % phosphatase inhibitor. After the sample was centrifuged at 12,000 × g, 4 °C, for 10 min, then the protein concentration in the supernatant was determined using a Bicinchoninic Acid assay (Beyotime Biotechnology, China).
Western blotting were performed as described previously [17]. The membranes were incubated with primary antibodies, including total mTOR (#2972; Cell Signaling Technology), p-mTOR (#5536; Cell Signaling Technology), p-4EBP1 (#9451; Cell Signaling Technology), p-p70S6K (ab126818; Abcam) and β-actin (sc-47778; Santa Cruz) antibodys at 1:1000 dilution. After washed with TBST, the membranes were incubated for 2 h with horseradish peroxidase-linked secondary antibodies (Beijing ZhongShan Golden Bridge Biological Technology Co., LTD, China). Finally, the membranes were washed with TBST, and then developed using Supersignal West Dura Extended Duration Substrate according to the manufacturer’s instructions (Pierce, Rockford, IL). Western blots images were quantified by measuring the intensity of correctly sized bands using Alpha Imager 2200 (Alpha Innotech Corporation, CA, USA) software, and all protein measurements were normalized to β-actin.
Statistical analysis
Statistical analyses were carried out using a t test, SPSS statistics 17. All the results are expressed as means with their standard errors (SPSS Institute, Inc.). Differences were considered to be statistically significant, and probability P values < 0.05 were taken to indicate statistical significance, and probability values between 0.05 and 0.10 were considered to be trends.
Results
Plasma antioxidant enzymes’ activities and oxidant injury product
To investigate the effects of supplementation with COS during late gestation on anti-oxidant capacity, plasma GSH-Px, total-SOD and CAT were analyzed (Table 3). The total SOD activity in the COS group was increased (P < 0.05), whereas plasma GSH-Px and CAT weren’t affected on d 110 of gestation compared with that in the control group (P > 0.10). The most common product of lipid peroxidation MDA, as an oxidative damage level of sows, also presented the downtrend in the COS group on d 110 of gestation compared with that in the control group (0.05 < P < 0.10).
Table 3.
Plasma antioxidant enzyme’s activity and oxidant injury product of sows
| Item | Dietary treatment | P-value | |
|---|---|---|---|
| Control | COS | ||
| GSH-Px (U/mL) | 629 ± 23.0 | 675 ± 11.2 | 0.105 |
| T-SOD (U/mL) | 72.7 ± 2.55b | 81.6 ± 2.17a | 0.027 |
| CAT (U/mL) | 4.19 ± 0.67 | 4.05 ± 0.64 | 0.857 |
| MDA (nmol/mL) | 3.95 ± 0.42 | 2.81 ± 0.38 | 0.069 |
Dietary treatment: control = basal diet, COS = basal diet + COS (30 mg/kg basal diet). Data are expressed as mean ± SEM, n = 8. a, bMeans values were significantly different compared with normal sows (P < 0.05). The same as below
Antioxidant related gene expression and contents of total-SOD and catalase in placenta
To investigate the effect of dietary supplementation with COS on the oxidant stress and antioxidant capacity of placenta, we studied the mRNA expression of several anti-oxidant (Fig. 1(a)) or pro-inflammation cytokine (Fig. 2) genes in the placenta. The mRNA levels of anti-oxidant gene Cu/Zn-SOD (P < 0.05) and CAT (P < 0.01) were increased in the COS group, but Ucp2 was down-regulated (P < 0.05) compared with that in the control group. Meanwhile, COS supplementation resulted in decreased IL-6 (P = 0.001) and IL-8 (P < 0.05), or a downtrend (0.05 < P < 0.10) in Hsp70 and IL-1β, but no significant difference was observed (P > 0.10) in the mRNA levels of GPx1, GPx4, p53, TNFα and Mn-SOD between the two groups, which was consistent with the contents of total-SOD and CAT in the placenta (P > 0.10) (Fig. 1(b), (c)).
Fig. 1.
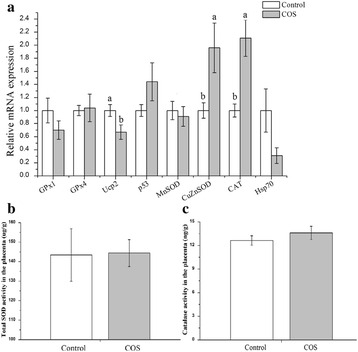
Oxidative stress-related genes expression (a), total SOD (b) and catalase (c) in the placenta of sows consuming control, COS diets during late gestation and lactation. Values are means (n = 8) with their standard errors represented by vertical bars
Fig. 2.
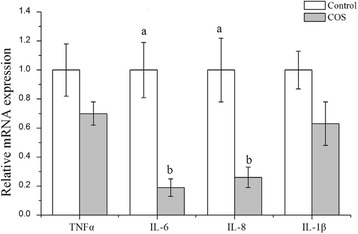
Pro-inflammatory cytokines expression in the placenta of sows consuming control, COS diets during late gestation and lactation. Values are means (n = 8) with their standard errors represented by vertical bars
Relative expression of amino acid transporters in placenta
Except for the effect of COS on antioxidant defense in placenta, we also studied the relative expression of several amino acid transport-related genes (Fig. 3(a)). Compared with that in the control group, the mRNA levels of EAAT1, PAT1, PAT2 and ASCT2 in the COS group were 2.81, 2.82, 3.76 and 1.82-fold (P < 0.05), respectively. Noticeably, the mRNA level of vascular endothelial growth factor A (VEGF-A) in the COS group was 2.23-fold (P < 0.05) compared that in the control group (Fig. 2(b)). However, no significant difference was observed in mRNA expression of LAT1, EAAT2, PEPT1 and SNAT2 between the control and COS groups (P > 0.10).
Fig. 3.

Amino acid transport-related genes (a) and VEGF-A expression (b) in the placenta of sows consuming control, COS diets during late gestation and lactation. Values are means (n = 8) with their standard errors represented by vertical bars
Relative protein expression of mTOR signaling pathway in the placenta
It has been demonstrated intracellular or extracellular cues, such as amino acids, oxygen, and stress, could function to regulate mTOR pathway. In this study, the activity of the mTOR pathway was detected by measuring the protein abundances of p-mTOR, p-4EBP1, p-p70S6K and total mTOR. As shown in Fig. 4, mTOR signaling pathway in the placenta was stimulated. Compared with the control group, relative abundances of p-mTOR and total mTOR in placenta were increased (P < 0.05). In addition, the level of p-4EBP1, major downstream target of mTOR, was also up-regulated (P < 0.05), whereas the p-p70S6K level only exhibited an uptrend in the COS group (0.05 < P < 0.10).
Fig. 4.
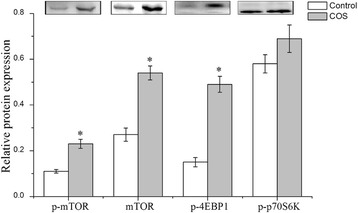
Relative protein expression of mTOR pathway in the placenta of sows consuming control, COS diets during late gestation and lactation. Values are means (n = 4) with their standard errors represented by vertical bars
Discussion
It has been shown that pregnant sows had elevated oxidative stress during late gestation [18]. Oxidative damage is a strong indicator of health status and wellbeing of animals in relation to stress, nutritional status, and disease. Increased oxidative stress is responsible for impaired milk production, reproductive performance, and finally longevity of sows [4]. Antioxidant defenses can be enzymatic and non-enzymatic, and enzymatic defense includes SOD, CAT and GSH-Px, which act as a major part of antioxidant system [19].
Increased defense against oxidative stress of sows during gestation by supplementing with COS in diet was confirmed by an increase in total SOD activity. SOD is responsible for degrading superoxide radical into oxygen and hydrogen peroxide, which is then degraded by CAT. COS treatment could effectively increase the SOD level, a natural power that can be quickly used by the cells as a defense against oxidative stress [20]. Oxidative stress is described as an imbalance in the production of reactive oxygen species (ROS) and the ability of antioxidant defenses to scavenge them [1]. As the key ROS metabolic biomarker, MDA is from a series of reactions during lipid peroxidation caused by ROS [19]. The plasma MDA in the COS group, at least, partially was for the release of antioxidant enzymes, which scavenged excessive ROS. From the results of plasma analysis on d 110 of gestation, we concluded that COS supplementation could improve anti-oxidative capacity of pregnant sows.
The placenta appears particularly vulnerable to oxidative stress because of its extensive cell division and high metabolic activity [21]. ROS accumulation in placenta is limited by a range of major antioxidant, including Mn and Cu/Zn-SOD, CAT, GSH, GSH-Px, and vitamins C and E are present in the placenta [1]. Although these antioxidants, such as vitamins E, C and β-carotenes, could transfer via placenta during the last days of gestation, the antioxidant system is still insufficient to scavenge the excessive ROS [22]. The relative mRNA levels of Cu/Zn-SOD and CAT in the placenta were significantly increased by COS supplement, which was similar to the results of plasma MDA content and total SOD activity during gestation. However, inconsistent results were observed in the contents of total SOD and CAT, which may be explained that COS supplementation just increased the transcription level of some antioxidant genes in the placenta of sows without severe oxidative stress.
Previous study reported Ucp2-null mice showed increased ROS production in several cell types including macrophages [23] and adipocytes [24], indicating that mitochondrial Ucp2 may limit oxidative stress by reducing ROS production. It is unknown, however, whether Ucp2 plays a similar role in placental tissue remains to be established. Jones et al. (2010) found that dexamethasone reduced Ucp2 expression of placenta in the rat during late gestation in labyrinth zone [25], and is consistent with similar effects observed in bovine mammary epithelial cell cultures [26]. Consequently, the lower mRNA level of Ucp2 in the COS group may serve to enhance antioxidant protection in the late gestation placenta, and impact on placental nutrient metabolism, especially at times of increased energy demand [27].
Other than reduced Ucp2 expression, the major pro-inflammatory IL-6, IL-8, and IL-1β were decreased or presented a downtrend. Similar results were observed in rats [28], and mice [29]. Several studies reported that oxidative stress status in obese women during pregnancy was always associated with a pro-inflammatory state [2]. Hsp70 have been implicated in stress regulation, including heat shock, oxidative stress, and other environmental stresses [30]. In line with the relative expression of IL-6 and IL-8, the relative mRNA expression of Hsp70 in placenta had a downtrend in the COS group, which was consistent with previous study that activation of Hsp70 could mitigates inflammatory response of kidney [31]. These observation clearly indicated that COS supplementation in sow’s diet contributed reducing placental oxidative stress and inflammatory response, enhanced anti-oxidant defense capacity of placenta.
It has been demonstrated that mTOR is a central integrator of various signals, such as growth factors, nutrients, energy, and stress [32]. As an essential serine/threonine kinase, mTOR is a central regulator of cell growth and proliferation, which can directly phosphorylates the ribosomal p70S6K and the initiation factor 4E-BP1 to initiate translation of distinct mRNAs [33]. For example, stimulating mTOR signaling pathway could increase protein synthesis, and decrease protein degradation in porcine conceptus trophectoderm cells [34] and porcine enterocytes [35]. It has been shown that mTOR/4EBP1 could offer cellular protection during oxidant stress, and knockdown of 4EBP1 induces oxidative stress-induced apoptosis through a caspase-dependent pathway in human endothelial progenitor cells [36]. Consequently, the abundance of mTOR/4EBP1 may be the result of lower oxidative stress by COS supplementation in sow’s diet, and p70S6K being relative independent on the mTOR pathway in this study.
The mTOR pathway is regulated by a multitude of intracellular and extracellular signals, and is inhibited by hypoxia [37], then significantly reduces the activity of placental amino acid transporters [38]. SNAT2 and PAT are important amino acid transporters in stimulating mTOR pathway [39]. In the present study, we found that the relative mRNA levels of most of amino acid transporter EAAT1, PAT1, PAT2 and ASCT2 in the COS group were increased or presented uptrend compared with that in the control group, which was consistent with previous report that mTOR increased total amino acid transporter gene expression with enhanced surface expression in mouse lymphoma cells, and the great expression of amino acid transporter increased the mTOR activity [40]. These observations are in line with our hypothesis that the mTOR pathway in the placenta functions as a nutrient sensing pathway.
It has been shown that inhibiting the phosphorylation of mTOR down-regulated the PlGF mRNA level (PlGF, a member of the VEGF family proteins) [41]. In agreement with previous study, the relative mRNA level of VEGF-A in placenta was increased by COS supplementing. During pregnancy, VEGF-A protein increases in the maternal circulation during pregnancy in humans [42] and mice [43]. It has been shown that it was sufficient to cause embryonic lethality when the mRNA level of VEGF-A fall by half [44]. Furthermore, VEGF-A gene deletion in the conceptus itself may result in alteration placental gene expression, reduced fetal body weight, and higher maternal cardiac output [45]. In this study, COS supplement significantly increased the VEGF-A mRNA level in placenta, indicating that supplementation with COS in sow diets could affect fetal development by stimulating mTOR pathway, involved in VEGF-A.
Conclusion
In summary, these observations suggested that maternal dietary supplementation with COS protected sows against oxidative stress by increasing plasma antioxidants and blocking inflammatory response, which may contribute to promoting placental amino acids transport by activating mTOR signaling pathway. Consequently, COS supplementation during late gestation may be an effective means in conforming the health of pregnant sows and nutrition transport from sows to fetus.
Acknowledgements
The authors appreciated Xiaoyun Guo and Huiqi Zhou for their kind help in Western blotting and RT-PCR study.
Funding
This paper was jointly supported by grants from the NSFC (31330075,31640078), the National Key Technology Research and Development Program of the Ministry of Science and Technology of China (2012BAD39B00), Key Technology Support Program of Jiangxi Province (No. 20151BBF60006), and Major Project of Hunan Province (2015NK1002).
Availability of data and materials
If the reader requires further information to help interpret the results, please contact the corresponding author.
Authors’ contributions
XW, YY and CX designed the experiment and analyzed the data, and CX, CL and QW performed the experiments. CX and XW wrote the paper, and ZF and SL contributed to data collection and analysis. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics and consent to participate
This study was carried out in accordance with the Chinese guidelines for animal welfare and experimental protocol, and was approved by the Animal Care Committee of the Institute of Subtropical Agriculture, Chinese Academy of Science.
Potential referees
Qingsong Xu, Qingsongxu2003@163.com, Dalian Institute of Chemical Physics CAS.
Haifeng Wang, 1438637738@qq.com, He is a famous animal nutrition scientist in China. ZHEJIANG A & F UNIVERSITY.
Andrew Adegboyega Fatufe, andrewfatufe@yahoo.com. Department of Animal Nutrition, Federal University of Agriculture, He is a professor on nutrition.
Abbreviation
- 4E-BP1
The initiation factor 4E-binding protein 1
- ASCT2
Alanine-serine-cysteine-threonine transporter
- CAT
Catalase
- COS
Chitosan oligosaccharide
- EAAT
Glutamate transporter
- GSH-Px
Glutathione peroxidase
- LAT1
L-type amino-acid transporter 1
- MDA
Malondialdehyde
- mTOR
Mammalian target of rapamycin
- p70S6K
Phosphorylates the ribosomal p70S6 kinase
- PAT
Proton-assisted amino acid transporter
- PEPT
Peptide transporter
- Per1
Negative-regulated element period 1, CLOCK, circadian locomotor output cycles kaput
- ROS
Reactive oxygen species
- SNAT
Sodium-coupled neutral amino acid transporter
- T-SOD
Total superoxide dismutase
- Ucp2
Uncoupling protein
- VEGF-A
Vascular endothelial growth factor A
Contributor Information
Xin Wu, Email: wuxin@isa.ac.cn.
Yulong Yin, Email: yinyulong@isa.ac.cn.
References
- 1.Myatt L, Cui XL. Oxidative stress in the placenta. Histochem Cell Biol. 2004;122:369–82. doi: 10.1007/s00418-004-0677-x. [DOI] [PubMed] [Google Scholar]
- 2.Malti N, Merzouk H, Merzouk SA, Loukidi B, Karaouzene N, Malti A, Narce M. Oxidative stress and maternal obesity: Feto-placental unit interaction. Placenta. 2014;35:411–6. doi: 10.1016/j.placenta.2014.03.010. [DOI] [PubMed] [Google Scholar]
- 3.Serdar Z, Gur E, Colakoethullary M, Develioethlu O, Sarandol E. Lipid and protein oxidation and antioxidant function in women with mild and severe preeclampsia. Arch Gynecol Obstet. 2003;268:19–25. doi: 10.1007/s00404-002-0302-y. [DOI] [PubMed] [Google Scholar]
- 4.Zhao Y, Flowers WL, Saraiva A, Yeum KJ, Kim SW. Effect of social ranks and gestation housing systems on oxidative stress status, reproductive performance, and immune status of sows. J Anim Sci. 2013;91:5848–58. doi: 10.2527/jas.2013-6388. [DOI] [PubMed] [Google Scholar]
- 5.Xiong QY, Wei YN, Xie HD, Feng ZX, Gan Y, Wang CL, Liu MJ, Bai FF, Xie F, Shao GQ. Effect of different adjuvant formulations on the immunogenicity and protective effect of a live Mycoplasma hyopneumoniae vaccine after intramuscular inoculation. Vaccine. 2014;32:3445–51. doi: 10.1016/j.vaccine.2014.03.071. [DOI] [PubMed] [Google Scholar]
- 6.Villiers C, Chevallet M, Diemer H, Couderc R, Freitas H, Van Dorsselaer A, Marche PN, Rabilloud T. From Secretome Analysis to Immunology chitosan induces major alterations in the activation of dendritic cells via a TLR-4 dependent mechanism. Mol Cell Proteomics. 2009;8:1252–64. doi: 10.1074/mcp.M800589-MCP200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mendis E, Kim MM, Rajapakse N, Kim SK. An in vitro cellular analysis of the radical scavenging efficacy of chitooligosaccharides. Life Sci. 2007;80:2118–27. doi: 10.1016/j.lfs.2007.03.016. [DOI] [PubMed] [Google Scholar]
- 8.Anandan R, Ganesan B, Obulesu T, Mathew S, Kumar RS, Lakshmanan PT, Zynudheen AA. Dietary chitosan supplementation attenuates isoprenaline-induced oxidative stress in rat myocardium. Int J Biol Macromol. 2012;51:783–7. doi: 10.1016/j.ijbiomac.2012.07.016. [DOI] [PubMed] [Google Scholar]
- 9.Roos S, Powell TL, Jansson T. Placental mTOR links maternal nutrient availability to fetal growth. Biochem Soc T. 2009;37:295–8. doi: 10.1042/BST0370295. [DOI] [PubMed] [Google Scholar]
- 10.Wu GY, Bazer FW, Cudd TA, Meininger CJ, Spencer TE. Maternal nutrition and fetal development. J Nutr. 2004;134:2169–72. doi: 10.1093/jn/134.9.2169. [DOI] [PubMed] [Google Scholar]
- 11.Jansson N, Pettersson J, Haafiz A, Ericsson A, Palmberg I, Tranberg M, Ganapathy V, Powell TL, Jansson T. Down-regulation of placental transport of amino acids precedes the development of intrauterine growth restriction in rats fed a low protein diet. J Physiol Lond. 2006;576:935–46. doi: 10.1113/jphysiol.2006.116509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Xie C, Guo X, Long C, Fan Z, Xiao D, Ruan Z, Deng ZY, Wu X, Yin Y. Supplementation of the sow diet with chitosan oligosaccharide during late gestation and lactation affects hepatic gluconeogenesis of suckling piglets. Anim Reprod Sci. 2015;159:109–17. doi: 10.1016/j.anireprosci.2015.06.004. [DOI] [PubMed] [Google Scholar]
- 13.Xie C, Wu X, Guo X, Long C, Li S, Hu C-AA, Yin Y. Maternal chitosan oligosaccharide supplementation affecting expression of circadian clock genes, and possible association with hepatic cholesterol accumulation in suckling piglets. Biol Rhythm Res. 2016;47:253–65. doi: 10.1080/09291016.2015.1108059. [DOI] [Google Scholar]
- 14.Tang ZR, Yin YL, Nyachoti CM, Huang RL, Li TJ, Yang C, Yang XJ, Gong J, Peng J, Qi DS, et al. Effect of dietary supplementation of chitosan and galacto-mannan-oligosaccharide on serum parameters and the insulin-like growth factor-I mRNA expression in early-weaned piglets. Domest Anim Endocrin. 2005;28:430–41. doi: 10.1016/j.domaniend.2005.02.003. [DOI] [PubMed] [Google Scholar]
- 15.Liu XD, Wu X, Yin YL, Liu YQ, Geng MM, Yang HS, Blachier F, Wu GY. Effects of dietary L-arginine or N-carbamylglutamate supplementation during late gestation of sows on the miR-15b/16, miR-221/222, VEGFA and eNOS expression in umbilical vein. Amino Acids. 2012;42:2111–9. doi: 10.1007/s00726-011-0948-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wu X, Yin YL, Liu YQ, Liu XD, Liu ZQ, Li TJ, Huang RL, Ruan Z, Deng ZY. Effect of dietary arginine and N-carbamoylglutamate supplementation on reproduction and gene expression of eNOS, VEGFA and PlGF1 in placenta in late pregnancy of sows. Anim Reprod Sci. 2012;132:187–92. doi: 10.1016/j.anireprosci.2012.05.002. [DOI] [PubMed] [Google Scholar]
- 17.Wu X, Xie C, Yin Y, Li F, Li T, Huang R, Ruan Z, Deng Z. Effect of L-arginine on HSP70 expression in liver in weanling piglets. BMC Vet Res. 2013;9:63. doi: 10.1186/1746-6148-9-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Berchieri-Ronchi CB, Zhao Y, Correa CR, Ferreira ALD, Yeum KJ, Kim SW. Oxidative stress status of high prolific sows during pregnancy and lactation. Faseb J. 2010;24. [DOI] [PubMed]
- 19.Yin J, Ren W, Liu G, Duan J, Yang G, Wu L, Li T, Yin Y. Birth oxidative stress and the development of an antioxidant system in newborn piglets. Free Radic Res. 2013;47:1027–35. doi: 10.3109/10715762.2013.848277. [DOI] [PubMed] [Google Scholar]
- 20.Joodi G, Ansari N, Khodagholi F. Chitooligosaccharide-mediated neuroprotection is associated with modulation of Hsps expression and reduction of MAPK phosphorylation. Int J Biol Macromol. 2011;48:726–35. doi: 10.1016/j.ijbiomac.2011.02.011. [DOI] [PubMed] [Google Scholar]
- 21.Jauniaux E, Poston L, Burton GJ. Placental-related diseases of pregnancy: involvement of oxidative stress and implications in human evolution. Hum Reprod Update. 2006;12:747–55. doi: 10.1093/humupd/dml016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Robles R, Palomino N, Robles A. Oxidative stress in the neonate. Early Hum Dev. 2001;65:S75–81. doi: 10.1016/S0378-3782(01)00209-2. [DOI] [PubMed] [Google Scholar]
- 23.Arsenijevic D, Onuma H, Pecqueur C, Raimbault S, Manning BS, Miroux B, Couplan E, Alves-Guerra MC, Goubern M, Surwit R, et al. Disruption of the uncoupling protein-2 gene in mice reveals a role in immunity and reactive oxygen species production. Nat Genet. 2000;26:435–9. doi: 10.1038/82565. [DOI] [PubMed] [Google Scholar]
- 24.Chevillotte E, Giralt M, Miroux B, Ricquier D, Villarroya F. Uncoupling protein-2 controls adiponectin gene expression in adipose tissue through the modulation of reactive oxygen species production. Diabetes. 2007;56:1042–50. doi: 10.2337/db06-1300. [DOI] [PubMed] [Google Scholar]
- 25.Jones ML, Mark PJ, Lewis JL, Mori TA, Keelan JA, Waddell BJ. Antioxidant defenses in the rat placenta in late gestation: increased labyrinthine expression of superoxide dismutases, glutathione peroxidase 3, and uncoupling protein 2. Biol Reprod. 2010;83:254–60. doi: 10.1095/biolreprod.110.083907. [DOI] [PubMed] [Google Scholar]
- 26.Yonezawa T, Sanosaka M, Haga S, Kobayashi Y, Katoh K, Obara Y. Regulation of uncoupling protein 2 expression by long-chain fatty acids and hormones in bovine mammary epithelial cells. Biochem Biophys Res Commun. 2008;375:280–5. doi: 10.1016/j.bbrc.2008.08.021. [DOI] [PubMed] [Google Scholar]
- 27.Wu X, Xie C, Zhang Y, Fan Z, Yin Y, Blachier F. Glutamate–glutamine cycle and exchange in the placenta–fetus unit during late pregnancy. Amino Acids. 2015;47:45–53. doi: 10.1007/s00726-014-1861-5. [DOI] [PubMed] [Google Scholar]
- 28.Fang IM, Yang CM, Yang CH. Chitosan oligosaccharides prevented retinal ischemia and reperfusion injury via reduced oxidative stress and inflammation in rats. Exp Eye Res. 2015;130:38–50. doi: 10.1016/j.exer.2014.12.001. [DOI] [PubMed] [Google Scholar]
- 29.Chung MJ, Park JK, Park YI. Anti-inflammatory effects of low-molecular weight chitosan oligosaccharides in IgE-antigen complex-stimulated RBL-2H3 cells and asthma model mice. Int Immunopharmacol. 2012;12:453–9. doi: 10.1016/j.intimp.2011.12.027. [DOI] [PubMed] [Google Scholar]
- 30.Daugaard M, Rohde M, Jaattela M. The heat shock protein 70 family: Highly homologous proteins with overlapping and distinct functions. FEBS Lett. 2007;581:3702–10. doi: 10.1016/j.febslet.2007.05.039. [DOI] [PubMed] [Google Scholar]
- 31.Peng ZY, Zhou FH, Wang HZ, Wen XY, Nolin TD, Bishop JV, Kellum JA. The anti-oxidant effects are not the main mechanism for glutamine’s protective effects on acute kidney injury in mice. Euro J Pharm. 2013;705:11–9. doi: 10.1016/j.ejphar.2013.02.028. [DOI] [PubMed] [Google Scholar]
- 32.Zoncu R, Efeyan A, Sabatini DM. mTOR: from growth signal integration to cancer, diabetes and ageing. Nat Rev Mol Cell Biol. 2011;12:21–35. doi: 10.1038/nrm3025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hay N, Sonenberg N. Upstream and downstream of mTOR. Gene Dev. 2004;18:1926–45. doi: 10.1101/gad.1212704. [DOI] [PubMed] [Google Scholar]
- 34.Kong XF, Tan B, Yin YL, Gao HJ, Li XL, Jaeger LA, Bazer FW, Wu GY. L-Arginine stimulates the mTOR signaling pathway and protein synthesis in porcine trophectoderm cells. J Nutri Biochem. 2012;23:1178–83. doi: 10.1016/j.jnutbio.2011.06.012. [DOI] [PubMed] [Google Scholar]
- 35.Rhoads JM, Chen W, Gookin J, Wu GY, Fu Q, Blikslager AT, Rippe RA, Argenzio RA, Cance WG, Weaver EM, et al. Arginine stimulates intestinal cell migration through a focal adhesion kinase dependent mechanism. Gut. 2004;53:514–22. doi: 10.1136/gut.2003.027540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tang YB, Jacobi A, Vater C, Zou XN, Stiehler M. Salvianolic acid B protects human endothelial progenitor cells against oxidative stress-mediated dysfunction by modulating Akt/mTOR/4EBP1, p38 MAPK/ATF2, and ERK1/2 signaling pathways. Biochem Pharm. 2014;90:34–49. doi: 10.1016/j.bcp.2014.04.008. [DOI] [PubMed] [Google Scholar]
- 37.Arsham AM, Howell JJ, Simon MC. A novel hypoxia-inducible factor-independent hypoxic response regulating mammalian target of rapamycin and its targets. J Biol Chem. 2003;278:29655–60. doi: 10.1074/jbc.M212770200. [DOI] [PubMed] [Google Scholar]
- 38.Roos S, Kanai Y, Prasad PD, Powell TL, Jansson T. Regulation of placental amino acid transporter activity by mammalian target of rapamycin. Am J Physiol-Cell Ph. 2009;296:C142–50. doi: 10.1152/ajpcell.00330.2008. [DOI] [PubMed] [Google Scholar]
- 39.Heublein S, Kazi S, Ogmundsdottir MH, Attwood EV, Kala S, Boyd CAR, Wilson C, Goberdhan DCI. Proton-assisted amino-acid transporters are conserved regulators of proliferation and amino-acid-dependent mTORC1 activation. Oncogene. 2010;29:4068–79. doi: 10.1038/onc.2010.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Edinger AL. Growth factors regulate cell survival by controlling nutrient transporter expression. Biochem Soc T. 2005;33:225–7. doi: 10.1042/BST0330225. [DOI] [PubMed] [Google Scholar]
- 41.Knuth A, Liu L, Nielsen H, Merril D, Torry DS, Arroyo JA. Placenta growth factor induces invasion and activates p70 during rapamycin treatment in trophoblast cells. Ameri J Reprod Immunol. 2015;73:330–40. doi: 10.1111/aji.12327. [DOI] [PubMed] [Google Scholar]
- 42.Anthony FW, Evans PW, Wheeler T, Wood PJ. Variation in detection of VEGF in maternal serum by immunoassay and the possible influence of binding proteins. Ann Clin Biochem. 1997;34:276–80. doi: 10.1177/000456329703400309. [DOI] [PubMed] [Google Scholar]
- 43.Woods AK, Hoffmann DS, Weydert CJ, Butler SD, Zhou Y, Sharma RV, Davisson RL. Adenoviral delivery of VEGF121 early in pregnancy prevents spontaneous development of preeclampsia in BPH/5 mice. Hypertension. 2011;57:94–102. doi: 10.1161/HYPERTENSIONAHA.110.160242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Carmeliet P, Ferreira V, Breier G, Pollefeyt S, Kieckens L, Gertsenstein M, Fahrig M, Vandenhoeck A, Harpal K, Eberhardt C, et al. Abnormal blood vessel development and lethality in embryos lacking a single VEGF allele. Nature. 1996;380:435–9. doi: 10.1038/380435a0. [DOI] [PubMed] [Google Scholar]
- 45.Li H, Qu DW, McDonald A, Isaac SM, Whiteley KJ, Sung HK, Nagy A, Adamson SL. Trophoblast-specific reduction of VEGFA alters placental gene expression and maternal cardiovascular function in mice. Biol Reprod. 2014;91:87. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
If the reader requires further information to help interpret the results, please contact the corresponding author.


