Abstract
Background & objectives:
Ingestion of Cleistanthus collinus causes hypokalemia and cardiac arrhythmias leading to mortality in most cases. We undertook this retrospective study to evaluate the clinical presentation and predictors of outcome in critically ill patients admitted with C. collinus poisoning.
Methods:
The case records of 56 patients admitted to the medical intensive care unit (MICU) of a tertiary care teaching hospital in south India (2000-2014) with C. collinus poisoning were retrospectively analysed.
Results:
The mean age of patients was 36.7±13.3 yr; there were 30 males. Salient clinical manifestations included hypokalemia (58%), neutrophilic leucocytosis (48.2%), acute kidney injury (AKI) (42.9%), acute respiratory failure requiring mechanical ventilation (AcRFMv) (32.1%), shock (21.4%); cardiac arrhythmias and neuromuscular weakness (19.6% each); 21 patients (37.5%) had adverse outcome. Longer time-lapsed from consumption to reaching emergency room [median (interquartile range)] (hours) [49 (22-97) vs. 28 (7-56), P=0.038]; higher acute physiology and chronic health evaluation II (APACHE II) score at presentation [14 (8.25-14.75) vs. 2 (0-6) P<0.001]; and presence of the following [odds ratio (95% confidence intervals)] at initial presentation: shock [37.40 (4.29-325.98), P=0.001]; AcRFMv [26.67 (5.86-121.39), P<0.001]; elevated alanine aminotransferase [5.71 (1.30-25.03), P=0.021]; metabolic acidosis [5.48 (1.68-17.89), P=0.005]; acute kidney injury (AKI) [5 (1.55-16.06), P=0.007]; hyponatremia [4.67 (1.25-17.44), P=0.022]; and neutrophilic leucocytosis [3.80 (1.02-14.21), P=0.047] predicted death. A significant (P<0.001) increasing trend in mortality was observed with increasing International Program on Chemical Safety Poisoning Severity Score (IPCS-CSS) grade.
Interpretation & conclusions:
C. collinus is a lethal poison associated with high mortality for which there is no specific antidote. Careful search and meticulous monitoring of the predictors of death and initiating appropriate corrective measures can be life saving.
Keywords: Acute kidney injury, acute respiratory failure, APACHE II, Cleistanthus collinus, outcome, poisoning
Cleistanthus collinus, a plant belonging to the family Euphorbiaceae is commonly encountered in the south India1. All parts of this plant are poisonous. C. collinus is a commonly used suicidal poison with the victims intentionally ingesting any part of the plant (usually leaves)1. Mortality with C. collinus is about 30 per cent with death occurring in 3-7 days following ingestion2. The toxic active ingredients in leaves of this plant are aryl naphthalene lignan lactones, namely, diphyllin and its glycoside derivatives cleistanthin A, cleistanthin B; and collinusin3. Ingestion of this plant causes hypokalemia and cardiac arrhythmias peaking on the third or fourth day of ingestion. Mortality may result from arrhythmias, renal failure, shock or respiratory failure4. However, the pathogenetic mechanisms of toxicity are poorly understood till date. The present study was undertaken to document the clinical presentation and predictors of outcome in patients with C. collinus poisoning seen in a tertiary care hospital in south India.
Material & Methods
The case records of 56 patients diagnosed to have and treated for C. collinus poisoning during the period April, 2000 to October, 2014 at the Sri Venkateswara Institute of Medical Sciences (SVIMS), a tertiary care teaching hospital in Tirupati, Andhra Pradesh, India, were retrospectively studied. The study was approved by the Institutional Ethics Committee.
At the time of initial evaluation in the emergency room (ER), all patients received gastric lavage, and symptomatic treatment including intravenous (iv) fluids, inotropic support, correction of electrolyte abnormalities, metabolic acidosis; anti-arrhythmic therapy, renal replacement therapy and assisted mechanical ventilation, among others if needed. Following initial stabilization in the ER, they were transferred to the medical intensive care unit (MICU) for further management. On admission, the following investigations were done: portable chest radiograph, 12-lead electrocardiogram (ECG); complete haemogram, serum biochemistry and arterial blood gases.
In all of them the following data were recorded in a case record form: demographic data; details of plant part used and method of consumption for poisoning; time-lag between consumption of the poison and arrival at the ER, acute physiology and chronic health evaluation II (APACHE II) score5, laboratory characteristics; need for assisted mechanical ventilation, duration of mechanical ventilation; duration of MICU stay, hospital stay; and treatment outcome. In all patients International Program on Chemical Safety Poisoning Severity Score (IPCS-PSS)6 was also calculated at the time of admission to MICU. The IPCS-PSS6 allows grading of the severity of acute poisonings regardless of the type and number of agents involved. As per the IPCS-PSS6, the severity of poisoning at the time of initial presentation was graded as grades 0 (none), 1 (mild), 2 (moderate), 3 (severe).
Statistical analysis: To identify predictors of death in patients with C. collinus poisoning at the time of initial presentation, univariate analysis was carried out to compare the demographic, clinical, and laboratory variables between patients who were alive and dead using unpaired t test, Mann-Whitney U-test for continuous variables and chi-square test, odd's ratio (95% confidence intervals) for categorical variables. All tests were two-tailed. For the purposes of statistical analysis, patients who had “left against medical advice” were considered to have worst outcome i.e. “death”. Statistical softwares IBM SPSS, Version 20, (IBM SPSS Statistics, Somers NY, USA); and MedCalc Version 11.3.0 for Windows 2000/XP/Vista/7 (MedCalc Software bvba, Belgium) were used for statistical analysis.
Results
Their mean age was 36.7±13.3 yr (range 14 to 70 yr); there were 30 males. Thirty nine patients took the boiled extract/decoction of leaves, six took the crushed leaves sweetened with jaggery (traditional unrefined brown sugar made from concentrated sugar cane juice), seven consumed raw leaves and four consumed fruits and seeds of C. collinus plant. Median [interquartile range (IQR)] time-lapsed from consumption to reaching ER was 32 (IQR 8.25-63.5) hours. Salient clinical manifestations observed at the time of admission included acute kidney injury (AKI) [n=24 (42.9%)], acute respiratory failure requiring mechanical ventilation (AcRFMv) [n=18 (32.1%)], shock [n=12 (21.4%)], cardiac arrhythmia and neuromuscular weakness [n=11 (19.6%)]. Myasthenic crisis-like syndrome was observed in one patient7.
Laboratory abnormalities evident at the time of admission included hypokalemia in 58 per cent (29/50), hyponatremia 28 per cent (14/50), and neutrophilic leucocytosis in 54 per cent (27/50) patients. APACHE II score was available for 55 of the 56 patients studied; APACHE II score could not be computed in one patient as he died within an hour of arrival in the ER. Median APACHE II score at the time of initial presentation was 5 (IQR 1-14). As per the IPCS-PSS, the severity of poisoning at the time of initial admission was observed to be grade 0 (n=5, 8.9%); grade 1 (n=19, 33.9%); grade 2 (n=13, 23.2%); and grade 3 (n=19, 33.9%).
Median durations of MICU and total hospital stay were three (IQR 1-5) and four (IQR 2-6) days, respectively. Median duration of mechanical ventilation in patients with AcRFMv was nine (IQR 4-71.5) h. Seventeen patients died. Four of the severely ill patients sought discharge from the hospital against medical advice. Fourteen of 17 patients died within seven days of consumption of C. collinus.
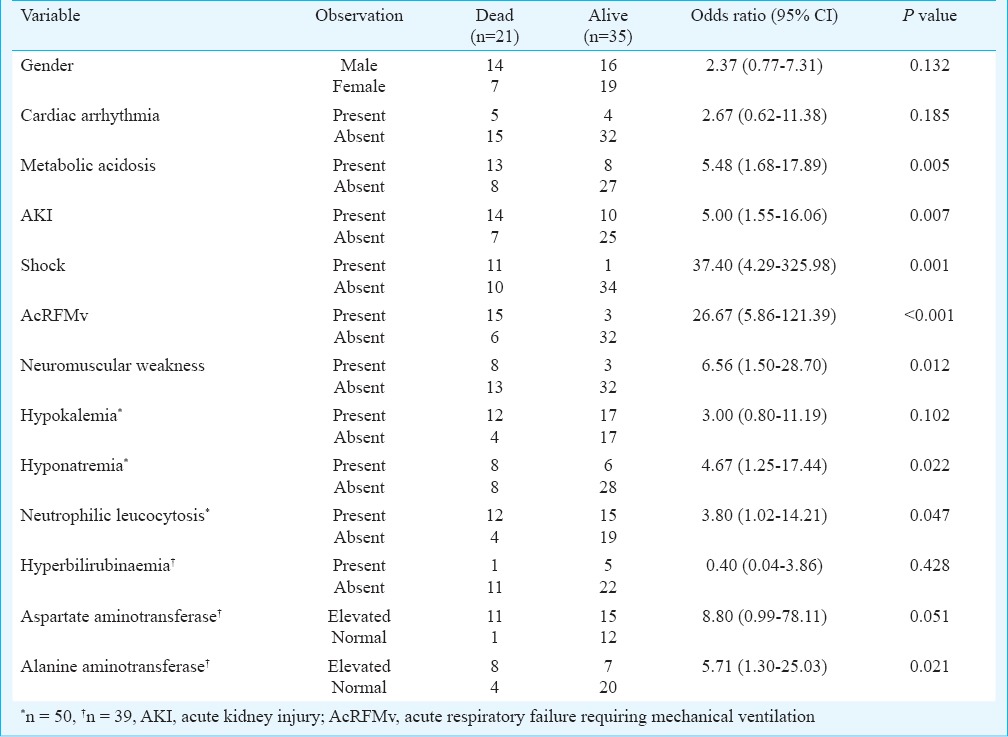
On univariate analysis, the following variables were found to be significant predictors of death: longer median time-lag from consumption to reaching the ER (P=0.038); higher median APACHE II score at presentation (P<0.001) (Table I); presence of shock (P=0.001); AcRFMV (P<0.001); elevated alanine aminotransferase (P=0.021); metabolic acidosis (P=0.005); AKI (P=0.007); hyponatremia (P=0.022); and neutrophilic leucocytosis (P=0.047) (Table II). An increasing trend was seen in mortality with increasing IPCS-CSS severity. None of the patients with IPCS-PSS grade 0 (n=5) died; one of the 19 patients with grade 1 severity; six of the 13 patients with grade 2 severity; and 14 of the 19 patients with grade 3 (73.7%) severity died (P<0.001).
Table I.
Comparison of continuous variables between survivors and non-survivors with Cleistanthus collinus poisoning
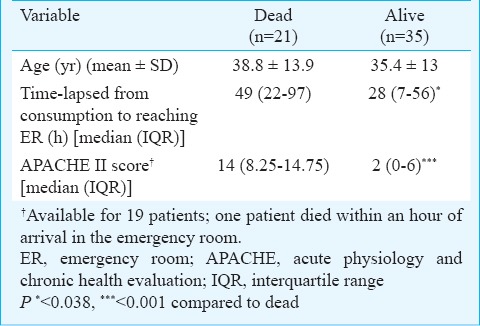
Table II.
Comparison of categorical variables between survivors and non-survivors with Cleistanthus collinus poisoning
Discussion
There are only a few published human studies1,4,8,9,10 available on C. collinus poisoning. However, in these studies severity of illness scoring systems was not used.
C. collinus is commonly used for acute deliberate self-poisoning in south India1,2,4,7,8,10 including the Rayalaseema area of Andhra Pradesh State where Tirupati is located. In the present study, the patients were older when compared with the patients seen at Vellore, India8,9. Consumption of C. collinus was found equal among women and men (male:female=1.1:1) in the present study while in other studies a female preponderance was observed. Metabolic acidosis, the most common clinical manifestation in two earlier reports from Puducherry (21.7%)1 and Vellore (100%)9 was only observed in 32 per cent of patients in the current study. Hypokalemia (58%) was the most common clinical feature in our patients which was similar to the figure documented in earlier reports8,10. Hypokalemia can be due to vomiting, and probable renal tubular loss of potassium associated with severe metabolic acidosis8. Hyponatremia was found to be a predictor of death in the present study as also reported in an earlier study1. Cardiac arrhythmia was seen in 19.6 per cent of our patients at presentation, which could have resulted from hypokalemia, direct effect of the poison on myocardium and also possible direct cardiodepressant effect of the plant toxins11. An interesting observation was myasthenic crisis like syndrome with ptosis, dysphagia and neuromuscular weakness in a patient who required ventilator support7. In this patient, predominant neuromuscular manifestations were potentially reversible with neostigmine which resulted in a striking improvement. Animal experimental data seem to support the use of neostigmine in patients with C. collinus poisoning who develop myasthenic syndrome. In Albino rat model, injecting lethal dose 50 (LD50) of leaf extracts of C. collinus intraperitoneally caused neuromuscular junctional blockade at postsynaptic acetylcholine receptors resulting in decremental response which was potentially reversible with the administration of neostigmine and aminopyridine12,13,14,15.
The presence of neutrophilic leucocytosis, hypokalemia, metabolic acidosis, cardiac arrhythmia, neuromuscular weakness and respiratory failure suggests that C. collinus is a systemic poison with multitude of effects4,8. The vomiting and severe abdominal pain noticed on the first day of ingestion implicates the direct effect of the poison on the gastric mucosa. The usual causes of death are respiratory failure requiring ventilator support and cardiac arrhythmia4,8. In the present study, 37.5 per cent mortality was observed which was higher than that observed in earlier reports1,4,8,9,10. This difference may be because of older age and delayed presentation to hospital in the present study.
In a study from Vellore7, Cox regression modelling revealed mode of ingestion, older age and history of chronic disease as predictors of death, while higher plasma potassium levels were associated with a significant 58 per cent risk reduction in mortality per 1 mmol/l increase in plasma potassium level. In the present study, longer median time-lag from consumption to reaching the ER; higher median APACHE II score at presentation, presence of shock, AcRFMV, elevated alanine aminotransferase, metabolic acidosis, AKI, hyponatremia and neutrophilic leucocytosis were predictors of death. By identifying and correcting these factors and instituting early and aggressive supportive management, there is a potential to reduce mortality in patients with C. collinus poisoning.
Further prospective studies are required to elucidate the clinical manifestations of C. collinus poisoning. Further research is also needed to understand the mechanisms of toxicity as well as for the development of potential antidotes, to reduce mortality. Careful search and meticulous monitoring of the predictors of death and early initiation of appropriate corrective measures can be life-saving.
Footnotes
Conflicts of Interest: None.
References
- 1.Subrahmanyam DK, Mooney T, Raveendran R, Zachariah B. A clinical and laboratory profile of Cleistanthus collinus poisoning. J Assoc Physicians India. 2003;51:1052–4. [PubMed] [Google Scholar]
- 2.Benjamin SP, Fernando ME, Jayanth JJ, Preetha B. Cleistanthus collinus poisoning. J Assoc Physicians India. 2006;54:742–4. [PubMed] [Google Scholar]
- 3.Govindachari TR, Sathe SS, Viswanathan N, Pai BR, Srinivasan M. Chemical constituents of Cleistanthus collinus (Roxb) Tetrahedron. 1969;25:2815–21. [Google Scholar]
- 4.Devaprabhu S, Manikumar S, David SS. Toxico-epidemiology and prognostic profile of patients with Cleistanthus collinus poisoning. Indian J Trauma Anaesth Crit Care. 2007;8:642–6. [Google Scholar]
- 5.Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13:818–29. [PubMed] [Google Scholar]
- 6.Persson HE, Sjِberg GK, Haines JA, Pronczuk de Garbino J. Poisoning severity score. Grading of acute poisoning. J Toxicol Clin Toxicol. 1998;36:205–13. doi: 10.3109/15563659809028940. [DOI] [PubMed] [Google Scholar]
- 7.Damodaram P, Manohar IC, Prabath Kumar D, Mohan A, Vengamma B, Rao MH. Myasthenic crisis-like syndrome due to Cleistanthus collinus poisoning. Indian J Med Sci. 2008;62:62–4. [PubMed] [Google Scholar]
- 8.Shankar V, Jose VM, Bangdiwala SI, Thomas K. Epidemiology of Cleistanthus collinus (oduvan) poisoning: clinical features and risk factors for mortality. Int J Inj Contr Saf Promot. 2009;16:223–30. doi: 10.1080/17457300903307094. [DOI] [PubMed] [Google Scholar]
- 9.Nampoothiri K, Chrispal A, Begum A, Jasmine S, Gopinath KG, Zachariah A. A clinical study of renal tubular dysfunction in Cleistanthus collinus (Oduvanthalai) poisoning. Clin Toxicol (Phila) 2010;48:193–7. doi: 10.3109/15563651003641786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bammigatti C, Surynarayana BS, Harichandra Kumar KT, Ganesh Kumar S. Pattern and outcome of Cleistanthus collinus (Oduvanthalai) poisoning in a tertiary care teaching hospital in South India. J Forensic Leg Med. 2013;20:959–61. doi: 10.1016/j.jflm.2013.08.011. [DOI] [PubMed] [Google Scholar]
- 11.Jose VM, Anand KN, Jeyaseelan L, Ernest K, Kuruvilla A. Effect of potassium channel modulators on toxicity of Cleistanthus collinus. Indian J Exp Biol. 2004;42:81–5. [PubMed] [Google Scholar]
- 12.Nandakumar NV, Vijayalakshmi KM. Experimental myasthenic crisis like neuromuscular impairement with Cleistanthus collinus leaf extract administration in rat. Physiother Res. 1996;10:121–6. [Google Scholar]
- 13.Vijayalakshmi KM, Nandakumar NV, Pagala MKD. Confirmatory in vivo electrodiagnositic and electromyographic studies for neuromuscular junctional blocking action of Cleistanthus collinus leaf extract administration in rat. Physiother Res. 1996;10:215–9. [Google Scholar]
- 14.Nandakumar NV, Pagala MKD, Venkatachari SAT, Namba T, Grob D. Effect of Cleistanthus collinus leaf extract on neuromuscular junction of the isolated mouse phrenic nerve-diaphram. Toxicon. 1989;27:1219–28. doi: 10.1016/0041-0101(89)90030-5. [DOI] [PubMed] [Google Scholar]
- 15.Rao RR, Nair TB. Investigations on induction of neutrophilic granulocystosis and toxicity of Cleistanthin-CIBA Go.4350-a new glycoside from Cleistanthus collinus (Roxb) Pharmacology. 1970;4:347–58. doi: 10.1159/000136164. [DOI] [PubMed] [Google Scholar]


