Abstract
Anxiety and depression are highly comorbid and share several common etiological processes. Therefore, it may be more efficient to develop interventions that treat or prevent these problems together rather than as separate entities. The present meta-analytic review examined whether interventions for children and adolescents that explicitly targeted either anxiety or depression showed treatment specificity or also impacted the other outcome (i.e., cross-over effects). We addressed this question both within the same type of study (i.e., treatment, prevention) and across study types. Only randomized controlled trials (RCTs) that assessed both constructs with dimensional measures were included in this review. For treatment studies, RCTs targeting anxiety (n=18) showed significant effects on both anxious and depressive symptoms, although more strongly on anxiety than depression; similarly, RCTs treating depression (n=9) yielded significant effects on both depressive and anxious symptoms, but stronger effects on depression than anxiety. Thus, there were cross-over effects in treatments purportedly targeting either anxiety or depression, and also treatment specificity, such that larger effects were seen for the target problem at which the treatment was aimed. Anxiety prevention studies (n=14) significantly affected anxious, but not depressive symptoms, indicating no cross-over effect of anxiety prevention trials on depression. For depression prevention studies (n=15), the effects were not significant for either depressive or anxiety symptoms, although the effect was significantly larger for depressive than for anxious symptoms. Post-hoc analyses revealed that the effect on depressive symptoms was significant in depression preventions trials of targeted but not universal samples. Implications for transdiagnostic interventions are discussed.
Keywords: Depression, Anxiety, Treatment, Prevention, Children, Adolescents, Meta-analysis
Both anxious and depressive symptoms and disorders in youth are prevalent, disabling, and recurrent.1,2 Anxiety and depression interfere with interpersonal relationships and academic achievement,3,4 and are associated with increased risk for substance abuse disorders, risky behaviors, suicide, and poor physical health.4–7 The prognosis for comorbid anxiety and depression in youth is worse than either condition alone, with higher risk of recurrence, longer duration, less favorable response to treatment, and greater utilization of mental health services.8,9
Lifetime prevalence of “any anxiety disorder” in children or adolescents is about 15% to 20% (i.e., separation anxiety: 3–8%; specific phobia: 10%; social phobia: 7%; panic disorder: 2–3%; generalized anxiety disorder: 4.3%).10 About 3–5% of children experience clinically significant depression at any given time, increasing to about 10–20% in the teen years. By the end of adolescence, nearly 1 in 5 youths will have experienced a depressive episode.2
Anxiety and depression are highly comorbid concurrently as well as sequentially. The extent of comorbidity is evident by both high correlations between dimensional measures of anxious and depressive symptoms11,12 and diagnostic comorbidity rates as high as 75% in some clinical samples.13,14 The level of comorbidity is not symmetrical, however. That is, youth with primary depressive disorders tend to have comorbid anxiety more often than do those with primary anxiety disorders have comorbid depression.15–17
The extent of this comorbidity changes with development. Whereas anxiety is more prevalent during childhood, the rate of depression grows during adolescence.18,19 With increasing age, comorbid anxiety and depression tend to be more common than either disorder alone.16 Thus, higher rates of comorbid anxiety and depression tend to be found in adolescents than children.17
Several non-mutually exclusive factors have been proposed to explain the high levels of comorbidity between anxiety and depression including symptom overlap, underlying negative affectivity, shared familial risk (e.g., parental psychopathology), stress, negative cognitions and information processing errors, and similar neural-circuitry dysfunction related to emotion modulation.20–22 Moreover, anxiety often precedes the onset of depression, such that the negative sequelae of anxiety, particularly interpersonal dysfunction, serve as a risk for subsequent depression.23 For example, sensitivity to social evaluative threat and associated social avoidance may increase a child’s vulnerability to developing depression, particularly when accompanied by peer rejection.24, 25
Thus, anxiety and depression are closely associated forms of psychopathology in terms of shared risk and etiological underpinnings and have strong covariance within families and across generations. Given these connections, it may be more efficient and cost-effective to develop models to treat and prevent these problems together rather than as separate entities. Indeed, to the extent that anxiety and depression in youth share common etiologic underpinnings, existing efficacious treatments developed for these disorders already may share common mechanisms of action. For example, both depression and anxiety have been treated effectively with selective serotonin reuptake inhibitors (SSRIs),26,27 presumed to operate through similar biological mechanisms, albeit with different dosing.28 In terms of psychosocial interventions, cognitive behavioral therapy (CBT) packages have shown positive effects in the treatment of both anxiety29 and depression.126 Although these CBT interventions share some common elements (e.g., cognitive restructuring, problem solving) across these conditions, they also have some unique features that target specific characteristics of anxiety (e.g., exposure, relaxation) and depression (e.g., behavioral activation).
In the current review, we probed the existing psychosocial intervention literature to assess the extent to which current interventions for anxiety or depression already operate on common mechanisms of action. Specifically, we tested whether interventions that explicitly targeted one condition (e.g., anxiety) also affected the other condition (e.g., depression). That is, do interventions for one condition have beneficial spillover effects on comorbid symptoms of the other disorder? We conducted a meta-analysis of RCTs that aimed to either treat or prevent anxiety or depression, and also measured the other construct. The results of this analysis were designed to inform future efforts to create transdiagnostic or sequential intervention programs across internalizing problems.
The question of crossover effects is not yet settled. Whereas some studies have shown that treatments for depression also positively affect anxiety,30 other studies have found that the presence of one condition actually reduces the efficacy of the treatment for the other condition.31–33 Moreover, long-term data on the efficacy of anxiety interventions have not demonstrated preventive effects on depression,34 despite strong theoretical reasons to hypothesize this chain of effects.22
The current literature on treatment and prevention of anxiety and depression in children and adolescents falls into four groups: (1) RCTs that intervened on and measured either anxiety or depression, but not both. This is the larger pool from which the reviewed studies came, but not all met criteria for the present review. (2) RCTs designed to treat or prevent anxiety or depression, and also measured the other construct; this was the primary focus of the current review. (3) RCTs that were intended to affect both anxiety and depression and measured both, but not always separately (e.g., internalizing symptoms) and not in an intentionally integrated program;35–38 and (4) RCTs that were explicitly conceptualized and designed to test a transdiagnostic intervention. This is a growing area of inquiry,13,39 but there are not yet enough completed RCTs to review at this time.
Thus, the purpose of the present meta-analytic review was to address the second question (above). What is the effect on depressive symptoms of interventions aimed at treating or preventing anxiety, and similarly what is the effect on anxiety symptoms of interventions aimed at treating or preventing depression? That is, are there cross-over effects? If so, what are the relative sizes of these effects? Finally, is there a difference between treatment and prevention trials regarding cross-over effects, and does this vary for anxiety versus depression?
METHODS
We reviewed the treatment and prevention literatures to identify (a) randomized controlled trials (RCTs), (b) targeting either anxiety or depression, (c) in children and/or adolescents (mean sample age < 20), and (d) including at least one dimensional measure of both anxiety and depression at the post-intervention assessment point. We focused on dimensional measures of anxiety and depression, because they more sensitively assess change as compared to categorical metrics, and they provide a common assessment method across studies varying in target problem focus (i.e., studies that included diagnostic measures, tended to do so mainly for their target outcome and not for comorbid conditions). Use of dimensional measures also was more consistent across both the treatment and prevention literatures, allowing for comparable analyses across studies. Therefore, because our specific question concerned cross-over effects, we only included studies that reported post-intervention results on dimensional measures of both anxiety and depression. Thus, this is a targeted review rather than a comprehensive summary of all RCTs aimed at treating or preventing anxiety or depression.
For our review of the treatment literature, we turned to recent evidence-based treatment updates, conducted under the auspices of the Society of Clinical Child and Adolescent Psychology, to identify the “best-practice” psychosocial intervention models in the literature. For anxiety, CBT was clearly the dominant model and deemed a well-established intervention for both children and adolescents.29 For depression, CBT was the most researched and well-supported intervention for both children and adolescents, with interpersonal psychotherapy (IPT) and attachment-based family therapy (ABFT) also receiving support as interventions for depression in teens.126 Accordingly, we screened all of the behavioral or CBT studies for anxiety (N = 56) and all the CBT (N = 34), IPT (N = 7), and other (e.g., family-focused therapy, bibliotherapy, psychoeducation; N = 7) studies for depression for inclusion in the current review. Of the anxiety trials, 29 were screened out for not including any dimensional measures of depressive symptoms at post-intervention, and 11 were excluded for methodological criteria (i.e., 5 included only youth with specific phobia, 4 did not include a non-active control condition, 1 did not randomize to the control condition, 1 included non-anxious youth), leaving a total of 18 RCTs for this review. Of the 45 independent depression studies, 27 were screened out for not including dimensional measures of anxiety symptoms at post-intervention, 5 were excluded for only assessing anxiety at baseline but not as an outcome, and 4 were excluded for methodological reasons (i.e., better categorized as indicated prevention studies), leaving a total of 9 RCTs for review.
For the review of the prevention literature, we surveyed the references lists of recent meta-analyses of the prevention of anxiety40–44 and the prevention of depression.45–48 We also searched the literature for RCTs of the prevention of depression or anxiety in youth, which yielded 63 depression prevention trials and 54 studies targeting anxiety or the reduction of internalizing problems (across anxiety and depression). Of the 117 prevention trials, 73 studies were excluded for not having dimensional measures of both depression and anxiety at the post-intervention assessment. Another 5 trials were excluded because they only included youth with specific phobias, and 10 did not randomize to a non-active control condition. The final review included 15 depression prevention and 14 anxiety prevention RCTs. Thus, despite the high level of comorbidity between depression and anxiety,11–14 half the anxiety trials and 62% of the depression studies did not include dimensional measures of the other construct.
Statistical Analyses
Modeling approach
We conducted a mixed-effects, multiple-endpoint meta-analysis using the metafor package (version 1.9–7) in R environment (version 3.2.2).49,50 Hedges’ g, a standardized mean difference statistic that corrects for bias in small-sample studies,51 was the primary response variable indicating the number of standard deviations separating treatment and control groups on average. Each study (j) contributed two ESs to the meta-analytic model representing the intervention effect on anxiety and depressive symptoms: and respectively. Parameters were estimated using restricted maximum likelihood (REML).
We ran a single a priori model regressing ESs on an indicator specifying the type of outcome variable (0=Anxiety Symptoms, 1=Depression Symptoms), and two study-level binary predictor variables: an indicator of the primary target of the intervention (0=Anxiety, 1=Depression), and an indicator of the type of intervention (0=Prevention, 1=Treatment). Additionally, we included all two- and three-way interactions of outcome, target, and type. The intercept in this model represented the conditional mean ES when all covariates were equal to 0. When interactions were present, we reran the model multiple times changing the reference levels of the predictor variables to get estimates of the mean ES for different levels of the predictor variables (i.e., the simple slopes approach).55 Our a priori model was as follows:
where gij are individual ESs for outcome i within study j; δj is the intercept for study j; βij is the effect of Outcome in study j; eij are deviations from the within-study intercept; γs are regression coefficients for study-level predictors, and ui represents between-study residuals.
Within-study dependencies
There were several sources of within-study dependencies among ESs, violating the assumption of independent residuals. First, some studies reported statistics for multiple measures of the same construct (anxiety and/or depressive symptoms). In these instances, we averaged across the ESs for the same construct so that each study provided a single estimate for both and using formulas provided by Borenstein et al. (2009).54 When computing a combined variance estimate for ESs measuring the same construct within the same study, it was necessary to account for the correlation between the two estimates.54 Whenever possible, we used correlations provided in the study articles. When these were not available, we used documented correlations from the literature as estimates. When correlations were neither reported in the study articles nor could be located in the literature, we set the correlation between the instruments measuring the same construct equal to 0.80, which was larger than the vast majority of within-study correlations reported in the study articles and literature, and the mean within-construct correlation (r =.61). Using high correlations is a conservative approach that results in the ES of interest having a larger standard error and, thus, less weight in the meta-analytic model.53
A second source of dependency among ES estimates was the result of some studies comparing multiple interventions to the same control conditions.83 In these cases, we computed aggregate summary statistics (means, SDs, and Ns) across the multiple intervention conditions and used these aggregate summary statistics to compute a single estimate of and ; thus, these ESs represented the difference between all study interventions and the control condition.54
Finally, each study provided two ES estimates ( and ), violating the assumption of independent residuals. To account for the correlation of and , we specified a variance-covariance matrix with diagonal elements containing estimates of the sampling variance for each ES and off-diagonal elements containing estimated covariances among ESs from the same study: cov( , ).52 Whenever possible, correlations reported in the study articles or from published sources were used to estimate within-study covariances. For example, several studies contributed ESs for both the Children’s Depression Inventory (CDI; Kovacs, 1992)127 and the Spence Children’s Anxiety Scale (SCAS; Spence, 1997)128 but only some reported the study correlation between these measures; therefore, we based our estimate on a correlation reported in a large psychometric study of the SCAS (r = 0.48).128 When correlations were not reported in study articles and could not be estimated from published sources, we imputed values. Among studies for which correlations between measures of anxiety and depressive symptoms were available, the mean correlation was r = 0.52. In an effort to be conservative, we simulated a normal distribution for the missing cross-construct correlations with a mean of r = 0.65 (range 0.53–0.80), thereby assuming that missing cross-construct correlations had a mean of 0.65, with individual correlations deviating from this mean value to form a normal distribution. Imputing a range of plausible estimates for missing cross-construct correlations is likely to better capture the variability in cross-construct correlations across studies than simply imputing the same estimate (e.g., 0.65) for all missing correlations.
RESULTS
Tables 1 presents descriptive characteristics and effects sizes for each of the 56 intervention studies meeting inclusion criteria for this review, and Table 2 provides an overall summary of this information. Participants in depression treatment trials were, on average, almost three years older than those in the anxiety treatment studies, which is consistent with the typical age of onset of these disorders.18,19 Prevention trials had much larger samples than treatment studies, likely due to the high number of prevention studies with universal samples. Whereas most studies assessed each construct with one measure, anxiety treatment studies included 2 to 3 measures of anxiety. The CDI was the most common measure of depressive symptoms, except in the depression treatment studies, which used other depression measures as often as the CDI.
Table 1.
Randomized Controlled Trials of Treatment and Prevention of Depression and Anxiety
| Depression randomized controlled treatment trials | ||||||
|---|---|---|---|---|---|---|
| Author(s) | Target Population | Sample Characteristics | Treatment(s) | Control | Anxiety Outcomes: ES(s) at Post | Depression Outcomes: ES(s) at Post |
| De Cuyper et al. (2004)77 | Non-diagnosed, with ≥ 1 criterion symptom of DSM-III-R MDD and CDI > 11 | N = 20; 75% female 10–12 years (M = 10.0) 100% Caucasian STAIC: M = 38.35 |
CBT (16 sessions – individual + 2 Taking Action) | Wait list (8 months) | STAIC: −0.25 | CDI: 0.27 |
| Diamond et al. (2002)78 | Primary care with DSM-III-R MDD | N = 32; 78% female 13–17 years (M = 14.9) 31% Caucasian 47.0% Anxietyb |
Individual ABFT (12 weeks) | Wait list (6 weeks) | STAIC: 1.03 | BDI: 0.75 |
| Fleming et al. (2012)79 | In alternative school; CDRS-R ≥ 30 | N = 32; 44% female 13–16 years (M 14.9) 25% New Zealand European SAS: M = 27.8 |
Technology-assisted CBT (7 modules; SPARX) | Wait list (5 weeks) | SAS: 0.40 | RADS-2: 0.75 |
| Melvin et al. (2006)80 | DSM-IV MDD, Dysthymia, or Depression NOS | N = 73; 66% female 12–18 years (M = 15.3) Race: NR (Australian) 27.0% Anxietyb |
CBT alone (12 + 3 sessions; CWD) | SSRI, alone |
CBT vs. SSRI RCMAS: 0.34 |
CBT vs. SSRI RADS: 0.41 |
| COMB = CBT + SSRI |
COMB vs. SSRI RCMAS: 0.23 |
COMB vs. SSRI
RADS: 0.07 |
||||
| Merry et al. (2012)81 | Treatment-seeking; CDRS-R ≥ 30 |
N = 187; 66% female 12–19 years (M = 15.6) 59% New Zealand European 15.6% GADb 16.7% Specific Phobiab 7.9% Separation Anxiety Disb |
Smart, Positive, Active, Realistic, X-factor Thoughts (SPARX) | Care as Usual (7 weeks) | SAS: 0.09 | RADS-2: 0.23 MFQ: 0.32 |
| Reynolds & Coats (1986)82 | BDI ≥ 12, RADS ≥ 72, and BID ≥ 20, indicating moderate levels of depression | N = 30; 63% female M = 15.7 years 100% Caucasian STAI-T: M = 53.3 |
Group CBT (10 sessions) | Wait list (10 weeks) |
CBT vs. WL STAI-T: 0.40 |
CBT vs. WL BDI: 1.40 RADS: 1.16 BID: 2.16 |
| Relaxation Training (10 sessions) |
RT vs. WL STAI-T: 1.65 |
RT vs. WL BDI: 1.53 RADS: 1.23 BID: 2.31 |
||||
| Stark, Reynolds, & Kaslow (1987)83 | CDI > 16, Time 1 & CDI ≥ 13, Time 2 | N = 29; 43% female 9–12 years (M = 11.2) Race: NR RCMAS: M = 17.9 |
Self-control Therapy (12 sessions) | Wait list (5 weeks) |
SCT vs. WL RCMAS: 0.60 |
SCT vs. WL CDI: 1.19 CDS: 0.78 |
| Behavioral Problem-Solving (12 sessions) |
BPS vs. WL RCMAS: 0.01 |
BPS vs. WL CDI: 1.00 CDS: 0.40 |
||||
| Vostanis et al. (1996)84 | Recruited from community clinics; DSM-III-R depression | N = 57; 56% female 8–17 years (M = 12.7) 87% Caucasian 45.7% Anxietyb |
CBT (9 sessions- individual) | Nonspecific Therapy | RCMAS: −0.09 RCMAS-P: 0.24 |
MFQ: 0.05 MFQ-P: 0.51 |
| Wood et al. (1996)85 | Treatment-seeking with DSM-III-R MDD or RDC minor depression, and MFQ ≥ 15 |
N = 48; 69% female 9–17 years (M = 14.2) Race: NR (UK) 56.3% Overanxious Dis.b |
CBT (DTP) individual sessions | Progressive Muscle Relaxation |
RCMAS: 0.97 RCMAS-P: 0.34 |
MFQ: 0.80 MFQ-P: 0.40 |
| Anxiety randomized controlled treatment trials | ||||||
| Author(s) | Target Population | Sample Characteristics | Treatment(s) | Control | Anxiety Outcomes: ESs at Post | Depression Outcomes: ESs at Post |
| Baer & Garland (2005)86 | Social Phobia (DSM-IV) | N = 12; 58% female 13–18 years (M = 15.5) Race: NR 8% Depressionb |
School SET-C (12 sessions) | Wait list (3 months) | SPAI: 1.16 | BDI-II: 0.20 |
| Barrett et al. (1996)87 | Anxiety Dis. (DSM-III-R) 38% Overanxious Disorder 38% Separation Anxiety Dis. 24% Social Anxiety Disorder |
N = 79; 43% female 7–14 yearsa Race: NR 6% Depressionb |
I-CBT (12 sessions; Coping Koala) | Wait list (12 weeks) |
I-CBT v. WL: FSSC-R: 0.49 RCMAS: 0.40 |
I-CBT v. WL:
CDI: 0.50 |
| I-CBT + Family Manage (12 sessions; Coping Koala with Family Management) | ||||||
|
I-CBT+FAM v. WL: FSSC-R: 0.74 RCMAS: 0.93 |
I-CBT+FAM v. WL: CDI: 0.53 |
|||||
| Beidel et al. (2000)88 | Social Phobia (DSM-IV) | N = 67; 60% female 8–12 years (M = 10.5) 70% Caucasian 1% Adjustment Disorderb |
SET-C (24 sessions) | Testbusters (24 sessions) | SPAI-C: 0.89 STAIC-State: 0.01 STAIC-Trait: 0.67 |
CDI: 0.91 |
| Flannery-Schroeder & Kendall (2000)89 | Anxiety disorder (DSM-IV) 57% GAD 30% Separation Anxiety Dis. 14% Social Phobia |
N = 37; 40% female 8–14 yearsa 89% Caucasian 3% MDDb |
I-CBT (18 sessions; Coping Cat) | Wait list (9 weeks) |
G-CBT v. WL: RCMAS: 1.05 SASC-R: 1.05 STAIC-State: 1.40 STAIC-Trait: 1.58 |
G-CBT v. WL: CDI: 0.90 |
| G-CBT (18 sessions; Coping Cat) |
I-CBT v. WL: RCMAS: 0.80 SASC-R: 0.67 STAIC-State: 1.06 STAIC-Trait: 1.08 |
I-CBT v. WL: CDI: 0.91 |
||||
| Gallagher et al. (2004)90 | Social Phobia (DSM-IV) | N = 23; 52% female 8–11 yearsa 57% Caucasian 9% Dysthymic Disorderb |
G-CBT (3 sessions; 3 hours each) | Wait list (3 weeks) | RCMAS: 0.71 SASC-R: 0.94 SPAI-C: 0.09 |
CDI: −0.06 |
| Ingul, Aune, & Nordahl (2014)91 | Social Phobia (DSM-IV) | N = 57; 56% female 8–10 grade (M = 14.5) Race: NR 9 % Depressionb |
I-CBT (12 sessions) | Attention Placebo (10 sessions) |
I-CBT v. AP: SPAI-C: 1.26 SCARED Total: 0.78 |
I-CBT v. AP: CDI:−0.39) |
| G-CBT (10 sessions) |
G-CBT v. AP:
SPAI-C: −0.57 SCARED Total: −0.15 |
G-CBT v. AP: CDI: −1.00 |
||||
| Kendall et al. (1997)92 | Anxiety Dis. (DSM-III-R) 59% Overanxious Disorder 23% Separation Anxiety Dis. 18% Avoidant Disorder |
N = 94; 38% female 9–13 yearsa 85% Caucasian 6% MDDb |
I-CBT (16 sessions; Coping Cat) | Wait list (8 weeks) | FSSC-R: 0.51 RCMAS: 0.58 STAIC-State: 0.40 STAIC-Trait: 0.71 STAIC-Father: 0.48 STAIC-Mother: 0.60 |
CDI: 0.75 |
| Kendall (1994)93 | Anxiety Dis. (DSM-III-R) 64% Overanxious Disorder 17% Separation Anxiety Dis. 19% Avoidant Disorder |
N = 47; 40% female 9–13 yearsa 76% Caucasian 32% Depressionb |
I-CBT (16 sessions; Coping Cat) | Wait list (8 weeks) | FSSC-R: 0.37 RCMAS: 0.86 STAIC-State: 0.86 STAIC-Trait: 0.78 STAIC-Parent: 0.41 |
CDI: 0.55 |
| Khanna & Kendall (2010)94 | Anxiety Dis. (DSM-IV): 57% GAD 16% Social Phobia 14% Separation Anxiety Dis. 8% Specific Phobia 4% Panic Disorder |
N = 49; 32% female 7–13 years (M = 10.1) 84% Caucasian Comorbidity: NR |
I-CBT (12 sessions; Coping Cat) | Computer-assisted Education Support (12 sessions) |
I-CBT v. Comp-assist Ed Suppt: MASC: 0.22 |
I-CBT v. Comp-assist Ed Suppt: CDI: −0.10 |
| Computer-assisted CBT (12 sessions; Camp Cope-a-lot) |
Comp-assist CBT v. Comp-assist Ed Suppt: MASC: 0.26 |
Comp-assist CBT v. Comp-assist Ed Suppt: CDI: 0.05 |
||||
| Last et al. (1998)95 | Anxiety Dis. & anxiety-based school refusal (DSM-III-R) 58% Simple/Social Phobia 32% Separation Anxiety Dis. 4% Overanxious Disorder 4% Avoidant Disorder 2% Panic Disorder |
N = 56; 59% female 6–17 years (M = 12.0) 90% Caucasian 0% comorbid MDD |
I-CBT (12 sessions) | Ed Support (12 sessions) | FSSC-R: 0.48 STAIC-modified Total: 0.31 |
CDI: 0.65 |
| Lyneham & Rapee (2006)96 | Anxiety disorder (DSM-IV) 40% GAD 22% Separation Anxiety Dis. 21% Social Phobia 9% OCD 7% Specific Phobia 1% Panic Disorder |
N = 100; 49% female 6–12 years (M = 9.4) 90% Australian 6% Mood Disorderb |
Bibliotherapy plus client initiated contact (12 sessions; Helping Your Anxious Child) | Wait list (12 weeks) |
Client-Initiated v. WL: RCMAS: 0.71 SCAS: 0.51 SCAS-F: 0.62 SCAS-M: 0.96 |
Client-Initiated v. WL: CDI: 0.20 |
| Bibliotherapy plus e-mail contact (12 sessions; Helping Your Anxious Child) | ||||||
| Bibliotherapy plus telephone contact (12 sessions; Helping Your Anxious Child) |
E-mail v. WL: RCMAS: 1.02 SCAS: 0.63 SCAS-F: 0.70 SCAS-M: 1.09 |
Telephone v. WL: CDI: 0.37 | ||||
|
Telephone v. WL: RCMAS: 0.69 SCAS: 0.68 SCAS-F: 0.44 SCAS-M: 1.09 | ||||||
| March et al. (2009)97 | Anxiety disorder (DSM-IV) 38% Social Phobia 32% Separation Anxiety Dis. 23% GAD 7% Specific Phobia |
N = 73; 55% female 7–12 years (M = 9.5) 94% Australian 4% Depression or Dysthymiab |
Internet CBT (10 child sessions + 6 parent sessions, & 1 and 3-month boosters; BRAVE for Children – ONLINE) | Wait list (10 weeks) | SCAS: 0.17 SCAS-P: 0.31 |
CES-D: 0.08 |
| Masia-Warner et al. (2007)98 | Social Phobia (DSM-IV) | N = 36; 83% female 14–16 years (M = 15.1) 72% Caucasian 3% MDDb 8% Dysthymiab 6% Adjustment Disorderb 17% Any mood disorder |
School SET-C (12 sessions + 2 individual sessions, 4 group events, 2 parent- teacher sessions, + two 2-month boosters; Skills for Social and Academic Success) | Educational Support (12 sessions) | SAS-A: SAD: 3.74 SAS-AP: SAD: 1.20 SPAI-C: 5.61 |
BDI-II: 4.98 |
| Muris et al. (2002)99 | Anxiety dis. (DSM-III-R) 35% GAD 15% Social Phobia 50% Separation Anxiety Dis. |
N = 20; 64% female 9–12 years (M = 10.0) 90% Caucasian Comorbidity: NR |
G-CBT (12 sessions; Coping Koala) | Emotional Disclosure (12 sessions) | RCADS-Anx: 0.94 STAIC-Trait anxiety: 1.00 |
RCADS-Dep: 1.09 |
| Pincus et al. (2010)100 | Primary diagnosis of Panic Disorder, with or without Agoraphobia (DSM-IV) | N = 26; 73% female 14–17 years (M = 15.8) 100% Caucasian Comorbidity: NR |
I-CBT (11 sessions; Panic Control Treatment for Adolescents) | Self-Monitor (8 weeks) | MASC: 0.24 | CDI: 0.24 |
| Silverman et al. (1999)101 | Anxiety dis. (DSM-III-R) 21% GAD 27% Social Phobia 52% Overanxious Disorder |
N = 56; 39% female 6–16 years (M = 9.96) 46% Caucasian Comorbidity: NR |
G-CBT (12 sessions) | Wait list (8–10 weeks) | FSSC-R: 0.64 FSSC-R/P: −0.13 RCMAS: 0.57 RCMAS-P: 0.80 |
CDI: −0.12 |
| Spence et al. (2006)102 | Anxiety disorder (DSM-IV) 21% Separation Anxiety Dis. 28% GAD 42% Social Phobia 10% Specific Phobia |
N = 72; 41% female 7–14 years (M = 9.93) 93% Australian 1% Dysthymiab |
G-CBT (10 child sessions + 6 parent sessions, + 1 & 3 month boosters) | Wait list (10 weeks) |
G-CBT v. WL: RCMAS T-score: 0.71 SCAS: 0.27 SCAS-P: 0.81 |
G-CBT v. WL: CDI T-score: 1.13 |
| G-CBT plus online (10 child sessions + 6 parent sessions; 1 & 3 month boosters) |
G-CBT+online v. WL: RCMAS T-score: 0.27 SCAS: −0.09 SCAS-P: 0.48 |
G-CBT + online v. WL: CDI T-score: 0.32 |
||||
| Thirlwall et al. (2013)103 | Anxiety disorder (DSM-IV) 24% GAD 21% Social Phobia 23% Separation Anxiety Dis. 31% Other Anxiety Disorder |
N = 194; 49% female 7–12 yearsa 86% Caucasian 7% MDDb 4% Dysthymiab |
Parent-delivered, Full CBT | Wait list (12 weeks) |
Full CBT v. WL: SCAS: 0.05 SCAS-P: 0.32 CAIS-P: 0.91 |
Full CBT v. WL: SMFQ: 0.17 SMFQ-P: 0.66 |
| Parent-delivered, Brief CBT |
Brief CBT v. WL: SCAS: −0.04 SCAS-P: 0.00 CAIS-P: 0.12 |
Brief CBT v. WL: SMFQ: −0.14 SMFQ-P: 0.06 |
||||
| Depression randomized controlled prevention trials | ||||||
| Author(s) | Target Population | Sample Characteristics | Prevention Program(s) | Control | Anxiety Outcomes: ESs at Post | Depression Outcomes: ESs at Post |
| Challen et al. (2014)104 | Universal | N = 2844; 49% female 11–12 yearsa 67% Caucasian |
Penn Resiliency Program (PRP) | Care as Usual | RCMAS: −0.05 | CDI: 0.13 |
| Dobson et al. (2010)105 | Indicated: subsyndromal depression | N = 46; 69% female M = 15.3 years Race: NR (Canadian) |
Coping With Stress | Attention Control | BAI: 0.11 MASQ-Anx: −0.23 |
CDI: −0.13 MASQ-Dep: 0.14 CES-D: −0.20 |
| Gillham et al. (2012)62 | Indicated: high depressive symptoms | N = 408; 48% female 92% were 11–13 yearsa 77% Caucasian |
Penn Resiliency Program (PRP) | Care as Usual | RCMAS: 0.17 | CDI: 0.26 RADS: 0.17 |
| Gillham, Reivich, et al. (2006)106 | Indicated: high anxiety & depressive symptoms | N = 44; 30% female 6th & 7th gradea 91% Caucasian |
Penn Resiliency Program (PRP) | Care as Usual | RCMAS: 0.07 | CDI: 0.00 |
| Kowalenko et al. (2005)61 | Indicated: high depressive symptoms (CDI) | N = 82; 100% female M = 14.5 years Race: NR (Australian & New Zealander) |
Adolescents Coping with Emotions (ACE) | Wait list | CATS-Anx: 0.47 | CDI: 0.55 |
| Pattison & Lynd-Stevenson (2001)107 | Universal: school-based | N = 66; 52% female M = 10.4 years Race: NR (Australian) |
Penn Prevention Program (PPP) | No participation control | STAIC-T: 0.18 | CDI: 0.05 |
| Roberts et al. (2003)108 | Indicated: high CDI scores | N = 189; 88% female M = 11.9 years Race: NR (Australian) |
Penn Prevention Program (PPP) | Care as Usual | RCMAS: 0.20 | CDI: 0.05 |
| Roberts et al. (2010)109 | Selective: low SES school | N = 496; 55% female M = 12.0 years 44% Australian origin |
Aussie Optimism Program (AOP) | Care as Usual | RCMAS: −0.19 | CDI: −0.14 |
| Rooney et al. (2006)64 | Selective: low SES schools | N = 136; 43% female M = 9.1 years Race: NR (Australian) |
Positive Thinking Program (PTP) | No intervention control | RCMAS: 0.15 | CDI: 0.57 |
| Rooney et al. (2013)65 | Selective: low SES schools | N = 910; 49% female M = 8.8 years 86% Native Australian |
Aussie Optimism Program (AOP) | Care as Usual | SCAS: −0.18 | CDI: 0.14 |
| Sheffield et al. (2006)110 | Universal and indicated: school-based (combined) | N = 2479; 54% female M = 14.3 years Race: NR (Australian) |
Generic Program (based on Problem Solving for Life) | Care as Usual | SCAS: −0.11 | CES-D: −0.00 CDI: 0.13 |
| Spence et al. (2014)111 | Universal: low family support | N = 697; 53% female M = 13.1 years 92% Australian |
Beyondblue | Mental health education class | SCAS: 0.03 | CES-D: 0.00 |
| Universal: regular family support | N = 2917; 53% female M = 13.1 years Race: NR |
Beyondblue | Mental health education class | SCAS: 0.01 | CES-D: −0.01 | |
| Stallard et al. (2012)112 | Indicated: depressive symptoms | N = 1064; 52% female 12–16 yearsa 78% Caucasian (UK) |
Resourceful Adolescent Program (RAP) | Personal, social, & health ed. | RCADS-Anx: −0.17 | RCADS-Dep: −0.27 SMFQ: −0.12 |
| Wong et al. (2014)113 | Universal: grades 9–10 | N = 976; 70% female 14–16 yearsa Race: NR (Australian) |
Combating Depression CBT course |
Health class curriculum | GAD-7: 0.29 | PHQ-9: 0.14 |
| Young et al. (2012)63 | Indicated: ≥ 2 depression symptoms at sub- or threshold levels & CES-D between 16–39; does not meet criteria for a depressive disorder |
N = 98; 70% female | Group IPT-AST (10 sessions) | School Counseling | SCARED: 0.69 | CES-D: 1.05 |
| (Young et al., 2006)33 (Young et al., 2010)114 |
7th–10th grade (M=14.0 yrs.) Race: NR 5.1% GAD 7.1% Simple Phobia 2.4% Social Anxiety Dis. 9th & 10th grade |
|||||
| Anxiety randomized controlled prevention trials | ||||||
| Author(s) | Target Population | Sample Characteristics | Prevention Program(s) | Control | Anxiety Outcomes: ESs at Post | Depression Outcomes: ESs at Post |
| Aune & Stiles, (2009)115 | Universal: grades 6–9 | N = 1439; 52% female 11–15 yearsa Race: NR (Norwegian) |
Norwegian Universal Preventive Program for Social Anxiety (NUPP-SA) | No intervention control | SPAI-C: 0.17 SCARED: 0.19 |
SMFQ: 0.09 |
| Balle & Tortella-Feliu (2010)116 | Indicated: high anxiety sensitivity | N = 613; 61% female M = 13.6 years Race: NR (Spanish) |
FRIENDS – modified version | Wait list | SCAS: −0.09 | CDI: −0.30 |
| Barrett & Turner (2001)117 | Universal: school-based | N = 325; 46% female M = 10.7 years Mostly Caucasian |
FRIENDS – Psychologist led | Care as Usual | SCAS: 0.32 RCMAS: 0.41 |
CDI: 0.08 |
| Universal: school-based | N = 400; 53% female M = 10.7 years Mostly Caucasian |
FRIENDS – Teacher led | Care as Usual | SCAS: 0.31 RCMAS: 0.33 |
CDI: −0.50 | |
| Barrett et al. (2003)118 | Universal: ESL school sample | N = 320; 8% female M = 12.3 years 46% Chinese; 15% NESB 39% former-Yugoslavian |
FRIENDS | Wait list | RCMAS: 0.67 TSCL-Anx: 0.44 |
TSCL-Dep: 0.74 |
| Essau et al. (2012)119 | Universal: school sample | N = 638; 46% female M = 10.9 years 96% Caucasian (German) |
FRIENDS (by school) | Wait list | SCAS: 0.20 | RCADS: 0.38 |
| Gallegos (2008)120 | Mixed | N = 1030; 53% female M = 9.9 years Mexican sample |
FRIENDS (AMISTAD) | Care as Usual (monitoring) | SCAS: 0.09 | CDI: 0.28 |
| Hains & Ellmann (1994)121 | Low emotional arousal youth | N = 11; 76% female 9th – 12th gradea 90% Caucasian |
Stress Inoculation Training | Wait list | STAIC-Trait: −0.16 | RADS: −0.37 |
| High emotional arousal youth | N = 10; 76% female 9th – 12th gradea 90% Caucasian |
Stress Inoculation Training | Wait list | STAIC-Trait: 1.24 | RADS: 1.31 | |
| Hains & Szyjakowski (1990)122 | Universal: school-based | N = 21; 0% female 16–17 yearsa 95% Caucasian |
Cognitive Stress-Reduction Intervention Program for Adolescents | Wait list | STAIC-Trait: 0.31 | BDI: 0.16 |
| Kehoe, Havighurst, & Harley (2014)123 | Universal | N = 224; 51% female M = 12.0 years Mostly Caucasian (Australian) |
Tuning in to Teen | Care as Usual | SCAS: 0.32 | CDI: 0.14 |
| Liddle & Macmillan (2010)60 | Indicated: high anxiety, low mood, or low self-esteem | N = 58; 47% female 8–14 yearsa Race: NR (British) |
FRIENDS | Wait list | SCAS: 0.25 | CDI: 0.26 |
| Lock & Barrett (2003)124 | Universal: grade 6 | N = 336; 50% female 9–10 yearsa Race: NR (Australian) |
FRIENDS | Wait list | SCAS: 0.39 RCMAS: 0.26 |
CDI: 0.19 |
| Universal: grade 9 | N = 401; 50% female 14–16 yearsa Race: NR (Australian) |
FRIENDS | Wait list | SCAS: 0.20 RCMAS: 0.36 |
CDI: 0.08 | |
| Lowry-Webster, Barrett, & Dadds (2001)125 | Universal: school-based | N = 594; 53% female 10–13 yearsa Race: NR (Australian) |
FRIENDS | Wait list | SCAS: 0.65 RCMAS: 0.33 |
CDI: 0.18 |
| Manassis et al. (2010)37 | Indicated: at risk for internalizing disorders | N = 148; 43% female 3rd – 6th gradea 57% Caucasian |
The Feelings Club | Program on child-rearing, without CBT | MASC: 0.06 | CDI: −0.01 |
| Wong et al. (2014)113 | Universal: grades 9–10 | N = 976; 70% female 14–16 yearsa Race: NR (Australian) |
Overcoming Anxiety CBT course | Regular health class curriculum | GAD-7: 0.18 | PHQ-9: 0.05 |
Note:
Mean age not reported;
Comorbid; ABFT = Attachment Based Family Therapy; Anx = Anxiety Subscale; AP = Attention Placebo; BAI = Beck Anxiety Inventory; BDI = Beck Depression Inventory; BID = Bellevue Index of Depression; BPS = Behavioral Problem Solving; CATS = Children’s Automatic Thoughts Scale; CBT = Cognitive Behavioral Therapy; CDI = Children’s Depression Inventory; CDS = Child Depression Scale; CES-D = Center for Epidemiologic Studies Depression Scale; COMB = Combination Treatment (CBT + SSRI); Comp-assist = Computer–assisted; CWD = Coping with Depression; Dep = Depression Subscale; Dis. = Disorder; DSM = Diagnostic and Statistical Manual; DTP = Depression Treatment Programme; ES = Effect Size; Ed Suppt = Educational Support; ESL = English as a Second Language; FRIENDS = Feeling worried? Relax and Feel Good, Inner Thoughts, Explore Plans, Nice Work, Don’t Forget to Practice, Stay Calm; FSSC-R = Fear Survey Schedule for Children-Revised; FSSC-R/P = Fear Survey Schedule for Children-Parent Report; GAD = Generalized Anxiety Disorder; G-CBT = Group Cognitive Behavioral Therapy; I-CBT = Individual Cognitive Behavioral Therapy; MASC = Multidimensional Anxiety Scale for Children; MDD = Major Depressive Disorder; MFQ = Mood and Feelings Questionnaire; MFQ-P = Mood and Feelings Questionnaire-Parent Report; NESB = Non-English Speaking Background; NOS = not otherwise specified; NR = Not Reported; PHQ = Patient Health Questionnaire; RDC = Research Diagnostic Criteria; RADS = Reynold’s Adolescent Depression Scale; RCADS = Revised Child Anxiety and Depression Scale; RCMAS = Reynolds Children’s Manifest Anxiety Scale; RCMAS-P = Reynolds Children’s Manifest Anxiety Scale-Parent Report; RT = Relaxation Training; SADS = Social Avoidance and Distress Scale; SAS-A = Social Anxiety Scale for Adolescents; SAS-AP= Social Anxiety Scale for Adolescents-Parent report; SASC-R-Total = Social Anxiety Scale for Children-Revised; SCARED = Screen for Child Anxiety Related Emotional Disorders; SAS = Spence Anxiety Scale; SCAS = Spence Children’s Anxiety Scale; SCAS-F = Spence Children’s Anxiety Scale-Father Report; SCAS-M = Spence Children’s Anxiety Scale-Mother Report; SCAS-P = Spence Children’s Anxiety Scale-Parent Report; SCT = Self-control Therapy; SET-C = Social Effectiveness Therapy for Children; SMFQ = Short Moods and Feelings Questionnaire; SMFQ-P= Short Moods and Feelings Questionnaire-Parent report; SPAI-C = Social Phobia and Anxiety Inventory for Children; SPARX = Smart, Positive, Active, Realistic, X-factor Thoughts; SSRI = Selective Serotonin Reuptake Inhibitor; STAIC = State-Trait Anxiety Inventory for Children; STAI-T = State-Trait Anxiety Inventory-Trait Scale; TSCL = Trauma Symptom Checklist for Children; UK = United Kingdom; WL = Wait list
Table 2.
Summary of characteristics of the treatment and prevention randomized controlled trials
| Number of Studies | % Female | Sample sizes | Age in years | Number of Depression Measures | Primary Depression Measures | Number of Anxiety Measures | Primary Anxiety measures | Programs | |
|---|---|---|---|---|---|---|---|---|---|
| Study Type | Mean (range) |
Mean (range) |
Mean (range) |
Mean | Mean | ||||
| Depression Treatment | 9 | 62% (43–78%) |
56.44 (20–187) |
13.83 (8–17) |
1.67 | 3 RADS 2 BDI 2 CDI 2 MFQ |
1.56 | 4 RCMAS 3 STAI 2 SAS |
6 CBT |
| Anxiety Treatment | 18 | 51.72% (32–83%) |
61 (12–194) |
11.07 (6–18) |
1.06 | 13 CDI 2 BDI-II 1 CES-D 1 RCADS-Dep 1 SMFQ |
2.44 | 5 FSSC-R 4 RCMAS 3 SPAI 2 MASC 2 SCAS 1 RCADS-Anx 1 SAS |
14 CBT (6 Coping Cat/Koala) |
| Depression Prevention | 15 [5 Universal (33%)] | 59% (30–100%) |
840.75 (44–2917) |
12.53 (8–16) |
1.33 | 11 CDI 5 CES-D |
1.07 | 6 RCMAS 3 SCAS 1 BAI 1 CATS-Anx 1 GAD-7 1 RCADS-Anx 1 SCARED 1 STAI |
5 PRP/PPP 2 AOP |
| Anxiety Prevention | 14 [9 Universal (64%)] | 50% (0 – 76%) |
538.86 (20–1349) | 12.39 (8–17) |
1.0 | 8 CDI 1 BDI 1 PHQ-9 1 RADS 1 RCADS 1 SMFQ 1 TSCL-Dep |
1.71 | 8 SCAS 2 STAI 1 GAD-7 1 MASC 1 RCMAS 1 SPAI |
10 FRIENDS |
Note: AOP = Aussie Optimism Program; Anx = Anxiety Subscale; BAI = Beck Anxiety Inventory; BDI = Beck Depression Inventory; CATS = Children’s Automatic Thoughts Scale; CBT = Cognitive Behavioral Therapy; CDI = Children’s Depression Inventory; CES-D = Center for Epidemiologic Studies Depression Scale; Dep = Depression Subscale; FRIENDS = Feeling worried? Relax and Feel Good, Inner Thoughts, Explore Plans, Nice Work, Don’t Forget to Practice, Stay Calm; FSSC-R = Fear Survey Schedule for Children-Revised; GAD = Generalized Anxiety Disorder; MASC = Multidimensional Anxiety Scale for Children; MFQ = Mood and Feelings Questionnaire; PHQ = Patient Health Questionnaire; PPP = Penn Prevention Program; PRP = Penn Resiliency Program; RADS = Reynold’s Adolescent Depression Scale; RCADS = Revised Child Anxiety and Depression Scale; RCMAS = Reynolds Children’s Manifest Anxiety Scale; SAS = Spence Anxiety Scale; SCARED = Screen for Child Anxiety Related Emotional Disorders; SCAS = Spence Children’s Anxiety Scale; SMFQ = Short Moods and Feelings Questionnaire; SPAI = Social Phobia and Anxiety Inventory; STAI = State-Trait Anxiety Inventory; TSCL = Trauma Symptom Checklist for Children.
Meta-analysis Results
There was considerable heterogeneity in ES estimates in our meta-analytic model: Q(92) = 4862.77, p<.001. Normal quantile and funnel plots showed that two ESs drawn from the same anxiety treatment study98 were notable outliers, with g scores greater than 3 (see Figure 1). When this study was dropped from the analyses, model results were similar indicating that the study was not influential due to its small sample size (N=32). Apart from these two outliers, there was little evidence of asymmetry in the funnel plot. Additionally, sample size was not associated with ES magnitude as would be expected if there was a systematic bias against inclusion of small studies with null findings.
Figure 1.
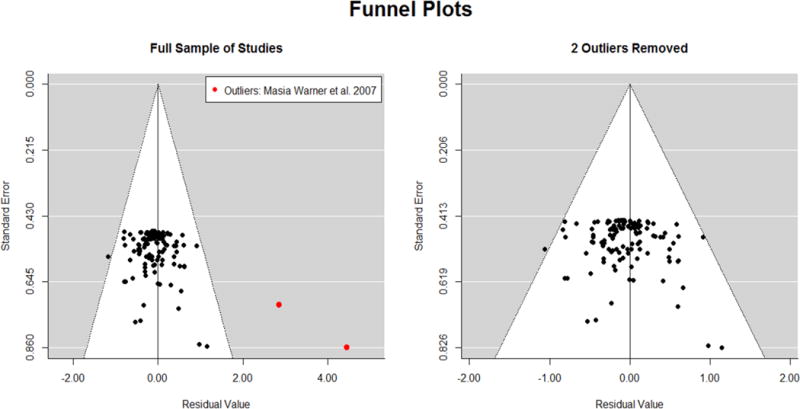
Funnel plots of all effect sizes (Hedges’ g) across treatment and prevention trials and across trials targeting anxiety and depressive symptoms. In the first panel, there were two effect sizes from the same anxiety treatment study (Masia-Warner et al., 2007)98 that were outliers with much larger than average effects on both anxiety and depressive symptoms (red dots). The second panel shows the same funnel plot with these two outliers removed.
The three-way, cross-level interaction of target*outcome*type was significant: , 95% CI [0.48, 0.59] (see Figure 2). The conditional mean ES among treatment studies targeting anxiety was significant for both anxiety symptoms ( , 95% CI [0.41, 0.93]) and depressive symptoms ( , 95% CI [0.28, 0.80]), but the mean ES for anxiety symptoms was significantly larger than the mean ES for depressive symptoms ( , 95% CI [0.11, 0.15]). Similarly, the mean ES among treatment studies targeting depression was significant for both depression ( , 95% CI [0.71, 1.42]) and anxiety symptoms ( , 95% CI [0.16, 0.87]), with the effect on depressive symptoms significantly larger than the effect on anxiety symptoms ( , 95% CI [0.55, 0.553]).
Figure 2.
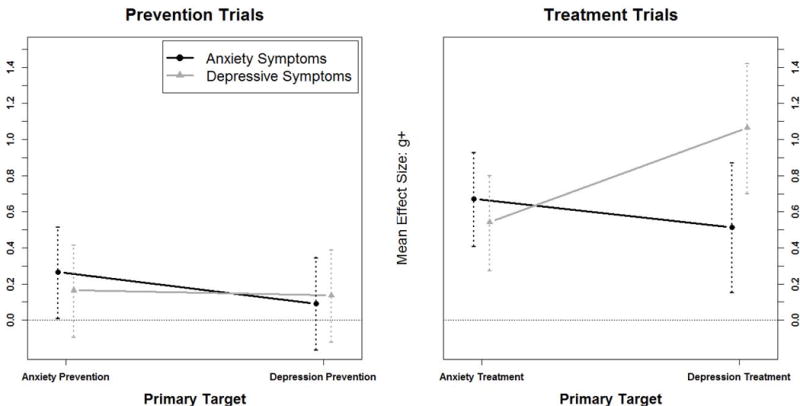
Three-way interaction of target*outcome*type. The magnitude of intervention effects varied as a function of the primary target of the intervention (anxiety or depression), the outcome measured (anxiety or depression symptoms), and the type of intervention (treatment or prevention).
Among prevention studies targeting anxiety, the mean ES was significant for anxiety symptoms ( , 95% CI [0.01, 0.52]), but not for depressive symptoms ( , 95% CI [−0.09, 0.42]), and the mean ES for anxious as compared to depressive symptoms was significantly larger ( , 95% CI [0.06, 0.14]). Among depression prevention studies, the mean ESs were not significant for either depressive symptoms ( , 95% CI [−0.12, 0.39]) or anxiety symptoms ( , 95% CI [−0.16, 0.35]), although the mean ES for depressive symptoms was significantly larger than the mean ES for anxiety symptoms ( , 95% CI [0.02, 0.09]).
Among studies targeting anxiety, the mean ES for anxiety symptoms was significantly larger in treatment than prevention studies ( , 95% CI [0.04, 0.77]). Similarly, among studies targeting depression, the mean ES for depressive symptoms was significantly larger in treatment than prevention trials ( , 95% CI [0.49, 1.37]). Cross-over effects of anxiety-focused interventions on depressive symptoms were larger in treatment than prevention studies ( , 95% CI [0.01, 0.74]). Similarly, the cross-over effect of depression interventions on anxiety symptoms tended to be larger in treatment than prevention studies, but this difference was not significant ( , 95% CI [−0.02, 0.86]).
Finally, the intervention effects may have been different among universal prevention trials given that most participants in these studies generally have low symptom levels to start. Therefore, we ran a post-hoc model with only the prevention studies to explore whether effects differed across studies of universal versus targeted samples. As in our primary model, we specified main effects of outcome, target, and risk (0=targeted; 1=universal) and all possible two- and three-way interactions. The three-way interaction of outcome*target*risk was significant: , 95% CI [0.07, 0.35]. Among anxiety prevention studies, the effect on anxiety symptoms was significant in studies with universal samples ( , 95% CI [0.18, 0.44]) but not with targeted samples ( , 95% CI [−0.21, 0.27]), and the magnitude of the mean effect size in studies with universal samples was significantly larger than the mean effect size in studies with targeted samples: , 95% CI [0.01, 0.56]. Among depression prevention studies, the effect on depressive symptoms was significant in studies of targeted samples ( , 95% CI [0.01, 0.30]) and not significant in studies of universal samples ( , 95% CI [−0.15, 0.24]), but the difference in effect magnitude across universal and targeted studies was not significant ( , 95% CI [−0.13, 0.36]). Thus, whether prevention studies recruited high-risk or universal samples did moderate intervention effects, but the pattern of moderation was different for anxiety and depression prevention studies (see Figure 3).
Figure 3.
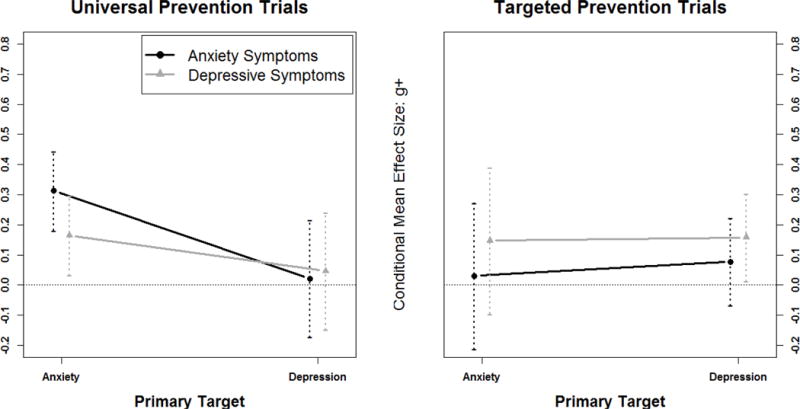
Three-way interaction of outcome*risk*target from the post-hoc analysis. Among prevention trials, the magnitude of intervention effects varied depending on whether trials used universal or targeted participant selection approaches (risk). The pattern of the risk effect differed depending on whether the intervention was primarily targeting anxiety or depression (target) and whether the outcome variable was anxiety or depressive symptoms (outcome). Anxiety prevention programs using universal samples had significant benefits on both anxiety and depressive symptoms (i.e., cross-over effect). Depression prevention programs with targeted (i.e., at risk) samples yielded significant benefits on depressive symptoms, but not anxiety symptoms. There were no benefits on either depressive symptoms or anxiety symptoms among universal depression prevention trials and targeted anxiety prevention trials.
Of particular note was that there was a cross-over effect of universal anxiety prevention programs on depressive symptoms ( , 95% CI [0.03, 0.30]), but no cross-over effects among targeted anxiety prevention programs ( , 95% CI [−0.01, 0.39]); the magnitude of the difference in cross-over effect across universal and targeted anxiety trials was small and not significant ( , 95% CI [−0.26, 0.29]). There was no evidence of cross-over effects of depression prevention programs, regardless of whether they were universal or targeted. These analyses should be interpreted cautiously as they were based on a post-hoc model and cell sizes were small.
DISCUSSION
The primary aim of the current meta-analytic review was to determine whether interventions for children and adolescents that explicitly target either anxiety or depression show treatment specificity, or also significantly impact the other outcome; that is, do they show cross-over effects? We addressed this question both within the same type of study (i.e., treatment, prevention) and across study types. Only RCTs that measured both constructs dimensionally were included in this review.
Results revealed an interesting significant three-way interaction of intervention target (anxiety or depression) by outcome variable (anxious or depressive symptoms) by type of intervention (treatment or prevention). For treatment studies, RCTs targeting anxiety produced significant effects on both anxious and depressive symptoms, although more strongly on anxiety than depression; similarly, RCTs treating depression yielded significant effects on both depressive and anxious symptoms, but with stronger effects on depression than anxiety. Thus, there was evidence of cross-over effects in treatments purportedly targeting either anxiety or depression, as well as treatment specificity, such that the largest ESs were seen for the problem at which the treatment was aimed. These encouraging results indicate that the treatments reviewed here not only successfully affected the targeted problem, but also had broader cross-over effects.
These cross-over effects have several important implications. First, although none of the included interventions were designed to be transdiagnostic, existing disorder-specific treatments for anxiety and depression may already be operating through shared mechanisms that link these conditions. For example, treatments that help children challenge their cognitive distortions or reduce their behavioral avoidance through exposure may be tapping into fundamental cognitive and behavioral processes that underlie both types of symptoms. This argument would be further bolstered by analyses of the mediators of intervention effects on primary and secondary outcomes in these trials. Such analyses are sorely lacking from the youth intervention literature as a whole,56,57 and for the treatment of internalizing disorders, in particular.58
Second, it may be possible to provide youths with interventions that impact both types of symptoms, either directly or through a longitudinal, sequential effect. For example, treatments that decrease anxiety may subsequently reduce or even prevent depressive symptoms that might otherwise follow from the anxiety, if not treated successfully. Overall, these results suggest that current, evidence-based treatments for anxiety and depression in children and adolescents may have broader effects than on just the target symptoms, at least at the post-treatment evaluation.
Not surprisingly, the effects on the targeted outcome were significantly stronger as compared to the other symptoms. Thus, although some cross-over effects were found, augmenting these treatments with procedures known to specifically affect the other disorder may further enhance the impact on the secondary symptoms. This could be done by adding modules explicitly designed to treat each set of symptoms,59 or through a more integrated, transdiagnostic intervention.13
With regard to prevention trials, the findings were more complicated. Anxiety prevention studies significantly affected anxiety symptoms, but not depressive symptoms, and not surprisingly, the ES was significantly larger for anxious than depressive symptoms. Thus, there was no evidence of a significant cross-over effect of anxiety prevention trials on depressive symptoms in our primary model. It is noteworthy, however, that post-hoc analyses showed an interesting pattern of findings. Anxiety prevention programs delivered universally were effective in targeting both anxiety and depressive symptoms (i.e., a cross-over effect), whereas targeted anxiety prevention programs were not. These findings should be interpreted cautiously, however, as they were post-hoc and because there were few targeted anxiety prevention studies.
Results of the analyses of the depression prevention trials were more surprising. In our primary model, for prevention studies targeting depression, the mean ESs were not significant for either depressive or anxious symptoms, although the ES for depressive symptoms was significantly larger than for anxious symptoms. Thus, based on the subset of studies reviewed here, the evidence was not strong for an effect of depression prevention programs on depressive symptoms, and even less of an effect on anxiety. One third of the samples in the depression prevention trials reviewed here were universal, however, which likely contributed to the overall low ES, given that none of these universal trials found significant effects on depressive symptoms. In contrast, 3 of the 7 studies using indicated samples61–63 and 2 of the 3 studies targeting selective (i.e., low income) samples64,65 showed significant effects on depressive symptoms. Post-hoc analyses showed that, among studies with targeted samples, the mean effect size for depression prevention programs on depressive symptoms (but not anxiety symptoms) was significant, but small. Thus, consistent with prior meta-analytic reviews (Horowitz & Garber, 2006; Merry et al., 2011; Stice et al., 2009), these findings indicate that depression prevention programs may be effective in altering depressive symptoms in at-risk youth. In contrast, the mean effect among depression prevention trials using universal samples was not significant for either depression or anxiety symptoms.
Finally, when comparing effects across the type of intervention, mean ESs were significantly larger in treatment than prevention studies for the effect of studies targeting anxiety on anxious symptoms, and for the effect of studies targeting depression on depressive symptoms. Cross-over effects of anxiety-focused interventions on depression symptoms and depression-focused interventions on anxiety symptoms tended to be larger in treatment than prevention studies, although these differences were not significant. One factor that may have contributed to the stronger effects for treatment as compared to prevention studies, was that the treatment trials used in this meta-analysis focused on studies included in reviews of evidence-based interventions.29,126 Although both negative and positive trials are featured in these reports, these intervention models already had been established as typically efficacious for their target problem. In contrast, the prevention trials reviewed here included a broader sampling of studies, likely with more variability in quality than the treatment studies.
Transdiagnostic Perspective
Diagnoses are increasingly being considered as dimensional rather than categorical, along an underlying continuum of pathology.66 High rates of comorbidity and evidence of shared risk processes across psychological disorders (i.e., transdiagnostic) suggest the likelihood of common, ‘higher-order’ pathological mechanisms that could be targeted within the same transdiagnostic intervention.67 Possible imprecision in current nosological systems, however, also may have contributed to the apparent cross-over effects. Nevertheless, the research agenda of the National Institute of Mental Health has shifted toward a shared mechanism perspective, with the Research Domain Criteria (RDoC) initiative proposing an innovative framework for studying common elements of psychopathology, driving discovery of new intervention targets, and shaping development of novel protocols.68
The studies in the current meta-analysis implemented interventions that were not explicitly designed to be transdiagnostic. Rather, because of our specific interest in evaluating cross-over effects, we reviewed RCTs that targeted either anxiety or depression, but also measured the other construct. Nevertheless, our results are promising with regard to the future development of transdiagnostic interventions. Treatments that targeted depression or anxiety, also significantly affected anxiety and depression, respectively. Thus, existing treatments provide a basis on which to build more integrated interventions aimed at reducing both types of symptoms. Given the extent of comorbidity between anxiety and depression, interventions that address only one set of symptoms at a time may be less efficient, whereas targeting common, “transdiagnostic” risk processes has the potential to affect multiple outcomes. From a public health perspective, development of an integrated treatment for internalizing problems could be less demanding on the time and resources of both clinicians and patients.
Several approaches to building effective transdiagnostic interventions are possible. One strategy has been to combine the techniques of two (or more) effective interventions together in a modular, algorithmic approach to comorbidity.59 The challenge here is to determine the “right” dose of each disorder-specific technique without doubling the amount of time in treatment. Another approach has been to select common treatment strategies thought to have effects on multiple symptom domains into a single, unified protocol.13, 72 Disorder-specific programs for treating anxiety and depression in youth have similar structures and use several common intervention strategies such as psychoeducation, coping skills training, problem solving, cognitive restructuring, and behavioral exposure, which then may only require minor modifications to treat both conditions.
A somewhat more challenging way to go is to identify the shared core etiological or maintaining mechanisms common to the two conditions, and then create an intervention that directly tackles these processes (e.g., emotion dysregulation, negative affectivity, cognitive distortions, behavioral avoidance). For example, targeting negative affectivity has been suggested rather than the discrete disorders of anxiety and depression, especially for children and adolescents, for whom these symptoms are less differentiated than in adults.69, 129
Promising developments for transdiagnostic intervention approaches have been emerging for adults,70,71 and children.13,39,72,73 For example, Weersing and colleagues13 designed a treatment that condensed existing CBT protocols for anxiety and depression to their core components and combined them into a brief, integrated treatment protocol that targeted common underlying processes such as behavioral avoidance and withdrawal. In the area of prevention, a group prevention program called EMOTION73 recently was developed to integrate core components of empirically supported treatments for anxiety and depression into a preventive intervention for indicated samples of youth.74–76 Because these few transdiagnostic interventions for anxiety and depression for children and adolescents are still relatively new, results from randomized efficacy trials are not yet available. Initial data from open trials indicate that transdiagnostic treatments for teens may impact both anxiety and depression similarly during treatment, although continued improvements over post-treatment may be stronger for anxiety than depression.39
Limitations and Future Directions
Limitations of the current meta-analysis highlight directions for future research. First, the studies reviewed here were a subset of RCTs testing the efficacy of interventions for anxiety or depression, selected on the basis of having included dimensional measures of both anxiety and depression. Studies that only assessed categorical diagnoses were excluded, as were studies that included measures of anxiety and depression at baseline but did not provided data on both constructs at post. Thus, the findings of this meta-analysis may not be representative of all RCTs evaluating interventions aimed at treating or preventing anxiety or depression. For example, the mean ES for depression treatment was high (i.e., over 1.0) as compared to what has been reported using the broader pool of depression treatment studies (i.e., about .40).30 This difference may have been due to several factors, including the exclusion of some notable treatment trials for depression in adolescents (e.g., TADS, 2004),130 or our focus on dimensional outcomes and exclusion of diagnostic data from the ES means (i.e., ESs on dimensional measures may be larger than for measures of disorder remission). Also, our review only had two depression treatment studies with child samples, which tend to have weaker effects than studies with adolescents.126
Second, the inclusion of several RCTs that used universal samples might have contributed to the relatively low ESs for depression prevention trials. Previous meta-analyses have found that depression prevention studies with universal samples tend not to do as well as those with either selective or indicated samples.45,47 A larger pool of prevention trials is needed in order to more thoroughly examine differences in the ESs for depression and anxiety symptoms as a function of sample type (i.e., universal vs. targeted).
Third, studies varied with regard to the number of interventions tested and in the number of measures of anxiety and depression used. For studies that included multiple interventions, we computed aggregate summary statistics across the multiple comparisons prior to calculating g; in these studies, g represented the average difference between all intervention conditions and the control condition. When multiple measures of a construct were included within the same study, we aggregated across measures of the same construct to yield a single ES for both anxiety and depressive symptoms from each study. We chose this strategy rather than randomly selecting only one measure so as to use all available data. Using a composite index across measures, of course, diminishes the contribution of any particular measure. These mean ESs might have been either an underestimate or a more reliable indicator of the effects. Anxiety treatment studies were more likely than the other three study types to include multiple measures of anxiety symptoms.
Finally, the current meta-analysis focused on the effects at post-intervention. Future reviews should examine longer-term cross-over effects. It is possible that improvements in one type of symptom (e.g., anxiety) precede changes in the other symptoms (e.g., depression). In addition, further research is needed regarding the mechanisms specific to changes in each type of symptoms as well as the shared processes that simultaneously or sequentially affect both.
Acknowledgments
This work was supported in part by grants from the National Institute of Mental Health (R01MH100258; R01MH64735; R01MH100260; R01MH084935; T32MH018921). We would like to thank Ellen M. Hart and Colin D. Freilich for their assistance with this project.
Footnotes
Disclosures and Conflicts of Interest: The authors have no disclosures or conflicts of interest to report.
Contributor Information
Steven M. Brunwasser, Vanderbilt University
Argero A. Zerr, San Diego State University
Karen T.G. Schwartz, San Diego State University
Karen Sova, Vanderbilt University.
V. Robin Weersing, San Diego State University.
References
- 1.Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and Development of Psychiatric Disorders in Childhood and Adolescence. Arch Gen Psychiatry. 2003 Aug;60(8):837–44. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- 2.Avenevoli S, Knight E, Kessler RC, Merikangas KR. Epidemiology of depression in children and adolescents. In: Abela JRZ, Hankin BL, editors. Handbook of depression in children and adolescents [Internet] New York, NY, US: Guilford Press; 2008. pp. 6–32. [cited 2015 Oct 16] Available from: http://search.proquest.com.proxy.library.vanderbilt.edu/psycinfo/docview/622102474/1AF14F79944040DFPQ/1. [Google Scholar]
- 3.Kessler RC, Foster CL, Saunders WB, Stang PE. Social consequences of psychiatric disorders I: Educational attainment. Am J Psychiatry. 1995 Jul;152(7):1026–32. doi: 10.1176/ajp.152.7.1026. [DOI] [PubMed] [Google Scholar]
- 4.Jaycox LH, Stein BD, Paddock S, Miles JNV, Chandra A, Meredith LS, et al. Impact of teen depression on academic, social, and physical functioning. Pediatrics. 2009 Oct;124(4):e596–605. doi: 10.1542/peds.2008-3348. [DOI] [PubMed] [Google Scholar]
- 5.Barbe RP, Bridge J, Birhamer B, Kolko D, Brent DA. Suicidality and its relationship to treatment outcome in depressed adolescents. Suicide Life Threat Behav. 2004 Spr;34(1):44–55. doi: 10.1521/suli.34.1.44.27768. [DOI] [PubMed] [Google Scholar]
- 6.Goodman E, Whitaker RC. A prospective study of the role of depression in the development and persistence of adolescent obesity. Pediatrics. 2002;110(3):497–504. doi: 10.1542/peds.110.3.497. [DOI] [PubMed] [Google Scholar]
- 7.Rice F, Lifford KJ, Thomas HV, Thapar A. Mental health and functional outcomes of maternal and adolescent reports of adolescent depressive symptoms. J Am Acad Child Adolesc Psychiatry. 2007 Sep;46(9):1162–70. doi: 10.1097/chi.0b013e3180cc255f. [DOI] [PubMed] [Google Scholar]
- 8.Birmaher B, Ryan ND, Williamson DE, Brent DA, Kaufman J, Dahl RE, et al. Childhood and adolescent depression: A review of the past 10 years, Part I. J Am Acad Child Adolesc Psychiatry. 1996 Nov;35(11):1427–39. doi: 10.1097/00004583-199611000-00011. [DOI] [PubMed] [Google Scholar]
- 9.Ezpeleta L, Domènech JM, Angold A. A comparison of pure and comorbid CD/ODD and depression. J Child Psychol Psychiatry. 2006 Jul;47(7):704–12. doi: 10.1111/j.1469-7610.2005.01558.x. [DOI] [PubMed] [Google Scholar]
- 10.Beesdo K, Knappe S, Pine DS. Anxiety and anxiety disorders in children and adolescents: Developmental issues and implications for DSM-V. Psychiatr Clin North Am. 2009 Sep;32(3):483–524. doi: 10.1016/j.psc.2009.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cole DA, Peeke LG, Martin JM, Truglio R, Seroczynski AD. A longitudinal look at the relation between depression and anxiety in children and adolescents. J Consult Clin Psychol. 1998 Jun;66(3):451–60. doi: 10.1037//0022-006x.66.3.451. [DOI] [PubMed] [Google Scholar]
- 12.Stark KD, Laurent J. Joint factor analysis of the Children’s Depression Inventory and the Revised Children’s Manifest Anxiety Scale. J Clin Child Psychol. 2001 Nov;30(4):552–67. doi: 10.1207/S15374424JCCP3004_11. [DOI] [PubMed] [Google Scholar]
- 13.Weersing VR, Gonzalez A, Campo JV, Lucas AN. Brief behavioral therapy for pediatric anxiety and depression: Piloting an integrated treatment approach. Cogn Behav Pract. 2008 May;15(2):126–39. [Google Scholar]
- 14.Sørensen MJ, Nissen JB, Mors O, Thomsen PH. Age and gender differences in depressive symptomatology and comorbidity: An incident sample of psychiatrically admitted children. J Affect Disord. 2005 Jan;84(1):85–91. doi: 10.1016/j.jad.2004.09.003. [DOI] [PubMed] [Google Scholar]
- 15.Axelson DA, Birmaher B. Relations between anxiety and depressive disorders in childhood and adolescence. Depress Anxiety. 2001;14(2):67–78. doi: 10.1002/da.1048. [DOI] [PubMed] [Google Scholar]
- 16.Merikangas KR, Avenevoli S. Epidemiology of mood and anxiety disorders in children and adolescents. In: Tsuang MT, Tohen M, editors. Textbook in psychiatric epidemiology [Internet] 2nd. New York, NY, US: Wiley-Liss; 2002. pp. 657–704. [cited 2015 Oct 16] Available from: http://search.proquest.com.proxy.library.vanderbilt.edu/psycinfo/docview/620085905/21D9360139F84FBEPQ/1. [Google Scholar]
- 17.Ollendick TH, Shortt AL, Sander JB, Maddux JE, Winstead B. Psychopathology: Foundations for a contemporary understanding [Internet] Lawrence Erlbaum Associates Publishers; 2005. A Internalizing Disorders of Childhood and Adolescence; pp. 353–76. [cited 2015 Oct 16] Available from: http://search.proquest.com.proxy.library.vanderbilt.edu/psycinfo/docview/620509707/846D34674CB642D3PQ/1. [Google Scholar]
- 18.Hankin BL, Roberts J, Gotlib IH. Elevated self-standards and emotional distress during adolescence: Emotional specificity and gender differences. Cogn Ther Res. 1997 Dec;21(6):663–79. [Google Scholar]
- 19.Woodward LJ, Fergusson DM. Life course outcomes of young people with anxiety disorders in adolescence. J Am Acad Child Adolesc Psychiatry. 2001 Sep;40(9):1086–93. doi: 10.1097/00004583-200109000-00018. [DOI] [PubMed] [Google Scholar]
- 20.Cummings CM, Caporino NE, Kendall PC. Comorbidity of anxiety and depression in children and adolescents: 20 years after. Psychol Bull. 2014 May;140(3):816–45. doi: 10.1037/a0034733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dozois DJA, Seeds PM, Collins KA. Transdiagnostic approaches to the prevention of depression and anxiety. J Cogn Psychother. 2009;23(1):44–59. [Google Scholar]
- 22.Garber J, Weersing VR. Comorbidity of anxiety and depression in youth: Implications for treatment and prevention. Clin Psychol Sci Pract. 2010 Dec;17(4):293–306. doi: 10.1111/j.1468-2850.2010.01221.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Starr LR, Hammen C, Connolly NP, Brennan PA. Does relational dysfunction mediate the association between anxiety disorders and later depression? Testing an interpersonal model of comorbidity. Depress Anxiety. 2014 Jan;31(1):77–86. doi: 10.1002/da.22172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Grant DM, Beck JG, Farrow SM, Davila J. Do interpersonal features of social anxiety influence the development of depressive symptoms? Cogn Emot. 2007 Apr;21(3):646–63. [Google Scholar]
- 25.Silk JS, Davis S, McMakin DL, Dahl RE, Forbes EE. Why do anxious children become depressed teenagers? The role of social evaluative threat and reward processing. Psychol Med. 2012 Oct;42(10):2095–107. doi: 10.1017/S0033291712000207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Treatment for Adolescents with Depression Study (TADS) Team. Fluoxetine, cognitive-behavioral therapy, and their combination for adolescents with depression: Treatment for Adolescents with Depression Study (TADS) randomized controlled trial. JAMA J Am Med Assoc. 2004 Aug;292(7):807–20. doi: 10.1001/jama.292.7.807. [DOI] [PubMed] [Google Scholar]
- 27.Walkup JT, Albano AM, Piacentini J, Birmaher B, Compton SN, Sherrill JT, et al. Cognitive behavioral therapy, sertraline, or a combination in childhood anxiety. N Engl J Med. 2008 Dec;359(26):2753–66. doi: 10.1056/NEJMoa0804633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bridge JA, Iyengar S, Salary CB, Barbe R, Birmaher B, Pincus HA, et al. Clinical response and risk for reported suicidal ideation and suicide attempts in pediatric antidepressant treatment: A meta-analysis of randomized controlled trials. JAMA J Am Med Assoc. 2007 Apr;297(15):1683–96. doi: 10.1001/jama.297.15.1683. [DOI] [PubMed] [Google Scholar]
- 29.Higa-McMillan CK, Francis SE, Rith-Najarian L, Chorpita BF. Evidence base update: 50 years of research on treatment for child and adolescent anxiety. J Clin Child Adolesc Psychol. 2015:1–23. doi: 10.1080/15374416.2015.1046177. [DOI] [PubMed] [Google Scholar]
- 30.Weisz JR, McCarty CA, Valeri SM. Effects of psychotherapy for depression in children and adolescents: A meta-analysis. Psychol Bull. 2006;132(1):132. doi: 10.1037/0033-2909.132.1.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Berman SL, Weems CF, Silverman WK, Kurtines WM. Predictors of outcome in exposure-based cognitive and behavioral treatments for phobic and anxiety disorders in children. Behav Ther. 2000 Fal;31(4):713–31. [Google Scholar]
- 32.Curry J, Rohde P, Simons A, Silva S, Vitiello B, Kratochvil C, et al. Predictors and moderators of acute outcome in the treatment for adolescents with depression study (TADS) J Am Acad Child Adolesc Psychiatry. 2006 Dec;45(12):1427–39. doi: 10.1097/01.chi.0000240838.78984.e2. [DOI] [PubMed] [Google Scholar]
- 33.Young JF, Mufson L, Davies M. Efficacy of Interpersonal Psychotherapy-Adolescent Skills Training: An indicated preventive intervention for depression. J Child Psychol Psychiatry. 2006 Dec;47(12):1254–62. doi: 10.1111/j.1469-7610.2006.01667.x. [DOI] [PubMed] [Google Scholar]
- 34.Benjamin CL, Harrison JP, Settipani CA, Brodman DM, Kendall PC. Anxiety and related outcomes in young adults 7 to 19 years after receiving treatment for child anxiety. J Consult Clin Psychol. 2013 Oct;81(5):865–76. doi: 10.1037/a0033048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ahlen J, Breitholtz E, Barrett PM, Gallegos J. School-based prevention of anxiety and depression: A pilot study in Sweden. Adv Sch Ment Health Promot. 2012 Oct;5(4):246–57. [Google Scholar]
- 36.Calear AL, Christensen H, Mackinnon A, Griffiths KM, O’Kearney R. The YouthMood Project: A cluster randomized controlled trial of an online cognitive behavioral program with adolescents. J Consult Clin Psychol. 2009 Dec;776:1021–32. doi: 10.1037/a0017391. [DOI] [PubMed] [Google Scholar]
- 37.Manassis K, Wilansky-Traynor P, Farzan N, Kleiman V, Parker K, Sanford M. The feelings club: Randomized controlled evaluation of school-based CBT for anxious or depressive symptoms. Depress Anxiety. 2010 Oct;27(10):945–52. doi: 10.1002/da.20724. [DOI] [PubMed] [Google Scholar]
- 38.Manicavasagar V, Horswood D, Burckhardt R, Lum A, Hadzi-Pavlovic D, Parker G. Feasibility and effectiveness of a web-based positive psychology program for youth mental health: Randomized controlled trial. J Med Internet Res. 2014 Jun;16(6):23–39. doi: 10.2196/jmir.3176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Queen AH, Barlow DH, Ehrenreich-May J. The trajectories of adolescent anxiety and depressive symptoms over the course of a transdiagnostic treatment. J Anxiety Disord. 2014 Aug;28(6):511–21. doi: 10.1016/j.janxdis.2014.05.007. [DOI] [PubMed] [Google Scholar]
- 40.Bennett K, Manassis K, Duda S, Bagnell A, Bernstein GA, Garland EJ, et al. Preventing child and adolescent anxiety disorders: Overview of systematic reviews. Depress Anxiety [Internet] 2015 Aug 18; doi: 10.1002/da.22400. [cited 2015 Oct 16]; Available from: http://search.proquest.com.proxy.library.vanderbilt.edu/psycinfo/docview/1707076628/4A04EEB2E9484EFFPQ/1. [DOI] [PubMed]
- 41.Bienvenu OJ, Ginsburg GS. Prevention of anxiety disorders. Int Rev Psychiatry. 2007 Dec;19(6):647–54. doi: 10.1080/09540260701797837. [DOI] [PubMed] [Google Scholar]
- 42.García-Campayo J, del Hoyo VL, Valero MS, Yus MCP, Esteban EA, Guedea MP, et al. Primary prevention of anxiety disorders in primary care: A systematic review. Prev Med Int J Devoted Pract Theory. 2015 Jul;76(Suppl):S12–5. doi: 10.1016/j.ypmed.2014.10.015. [DOI] [PubMed] [Google Scholar]
- 43.Feldner MT, Zvolensky MJ, Schmidt NB. Prevention of anxiety psychopathology: A critical review of the empirical literature. Clin Psychol Sci Pract. 2004 Nov;11(4):405–24. [Google Scholar]
- 44.Neil AL, Christensen H. Efficacy and effectiveness of school-based prevention and early intervention programs for anxiety. Clin Psychol Rev. 2009 Apr;29(3):208–15. doi: 10.1016/j.cpr.2009.01.002. [DOI] [PubMed] [Google Scholar]
- 45.Horowitz JL, Garber J. The prevention of depressive symptoms in children and adolescents: A meta-analytic review. J Consult Clin Psychol. 2006 Jun;74(3):401–15. doi: 10.1037/0022-006X.74.3.401. [DOI] [PubMed] [Google Scholar]
- 46.Merry SN, Hetrick SE, Cox GR, Brudevold-Iversen T, Bir JJ, McDowell H. Psychological and educational interventions for preventing depression in children and adolescents. Evid-Based Child Health Cochrane Rev J. 2011;7(5):1409–685. doi: 10.1002/14651858.CD003380.pub3. [DOI] [PubMed] [Google Scholar]
- 47.Stice E, Shaw H, Bohon C, Marti CN, Rohde P. A meta-analytic review of depression prevention programs for children and adolescents: Factors that predict magnitude of intervention effects. J Consult Clin Psychol. 2009 Jun;77(3):486–503. doi: 10.1037/a0015168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Stockings EA, Degenhardt L, Dobbins T, Lee YY, Erskine HE, Whiteford HA, et al. Preventing depression and anxiety in young people: A review of the joint efficacy of universal, selective and indicated prevention. Psychol Med [Internet] 2015 Aug 28; doi: 10.1017/S0033291715001725. [cited 2015 Oct 16]; Available from: http://search.proquest.com.proxy.library.vanderbilt.edu/psycinfo/docview/1709218818/7B02E65960BB4E96PQ/2. [DOI] [PubMed]
- 49.R Core Team. R: A language and environment for statistical computing [Internet] Vienna, Austria: R Foundation for Statistical Computing; 2014. Available from: http://www.R-project.org/ [Google Scholar]
- 50.Viechtbauer W. Metafor: meta-analysis package for R. 2010;2010:1–0. R Package Version. [Google Scholar]
- 51.Hedges LV. Distribution theory for Glass’s estimator of effect size and related estimators. J Educ Stat. 1981;6(2):107–28. [Google Scholar]
- 52.Olkin I, Gleser L. Stochastically dependent effect sizes. In: Cooper H, Hedges LV, Valentine JC, editors. The handbook of research synthesis and meta-analysis. 2nd. New York, NY, US: Russell Sage Foundation; 2009. [Google Scholar]
- 53.Snijders TAB, Bosker RJ. Multilevel analysis: An introduction to basic and advanced multilevel modeling. 2nd. SAGE Publications Inc; 2012. [Google Scholar]
- 54.Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to meta-analysis [Internet] John Wiley & Sons Ltd; 2009. [cited 2015 Oct 16]. Available from: http://www.wiley.com/WileyCDA/WileyTitle/productCd-EHEP002313.html. [Google Scholar]
- 55.Aiken LS, West SG, Reno RR. Multiple regression – testing and interpreting interactions [Internet] Newbury Park: CA: Sage; 1991. p. 211. [cited 2015 Oct 16] Available from: http://search.proquest.com.proxy.library.vanderbilt.edu/psycinfo/docview/37424468/771E17BDCD0B4C8CPQ/9. [Google Scholar]
- 56.Weersing VR, Weisz JR. Mechanisms of action in youth psychotherapy. J Child Psychol Psychiatry. 2002 Jan;43(1):3–29. doi: 10.1111/1469-7610.00002. [DOI] [PubMed] [Google Scholar]
- 57.Kazdin AE, Nock MK. Delineating mechanisms of change in child and adolescent therapy: methodological issues and research recommendations. J Child Psychol Psychiatry. 2003 Nov;44(8):1116–29. doi: 10.1111/1469-7610.00195. [DOI] [PubMed] [Google Scholar]
- 58.Weersing VR, Rozenman M, Gonzalez A. Core components of therapy in youth: do we know what to disseminate? Behav Modif. 2009 Jan;33(1):24. doi: 10.1177/0145445508322629. [DOI] [PubMed] [Google Scholar]
- 59.Weisz JR, Chorpita BF, Palinkas LA, Schoenwald SK, Miranda J, Bearman SK, et al. Testing standard and modular designs for psychotherapy treating depression, anxiety, and conduct problems in youth: A randomized effectiveness trial. Arch Gen Psychiatry. 2012 Mar;69(3):274–82. doi: 10.1001/archgenpsychiatry.2011.147. [DOI] [PubMed] [Google Scholar]
- 60.Liddle I, Macmillan S. Evaluating the FRIENDS programme in a Scottish setting. Educ Psychol Pract. 2010;26(1):53. [Google Scholar]
- 61.Kowalenko N, Rapee RM, Simmons J, Wignall A, Hoge R, Whitefield K, et al. Short-term effectiveness of a school-based early intervention program for adolescent depression. Clin Child Psychol Psychiatry. 2005;10(4):493–507. [Google Scholar]
- 62.Gillham JE, Reivich KJ, Brunwasser SM, Freres DR, Chajon ND, Kash-MacDonald VM, et al. Evaluation of a group cognitive-behavioral depression prevention program for young adolescents: A randomized effectiveness trial. J Clin Child Adolesc Psychol. 2012 Sep;41(5):621–39. doi: 10.1080/15374416.2012.706517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Young JF, Kranzler A, Gallop RJ, Mufson L. Interpersonal Psychotherapy-Adolescent Skills Training: Effects on school and social functioning. School Ment Health. 2012 Dec;4(4):254–64. doi: 10.1007/s12310-012-9078-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Rooney RM, Roberts CM, Kane R, Pike L, Winsor A, White J, et al. The prevention of depression in 8-to 9-year-old children: a pilot study. Aust J Guid Couns. 2006;16(01):76–90. [Google Scholar]
- 65.Rooney RM, Hassan S, Kane R, Roberts CM, Nesa M. Reducing depression in 9–10 year old children in low SES schools: A longitudinal universal randomized controlled trial. Behav Res Ther. 2013 Dec;51(12):845–54. doi: 10.1016/j.brat.2013.09.005. [DOI] [PubMed] [Google Scholar]
- 66.Brown TA, Barlow DH. A proposal for a dimensional classification system based on the shared features of the DSM-IV anxiety and mood disorders: Implications for assessment and treatment. Psychol Assess. 2009 Sep;21(3):256–71. doi: 10.1037/a0016608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ehrenreich-May J, Chu BC. Transdiagnostic treatments for children and adolescents: Principles and practice [Internet] New York, NY, US: Guilford Press; 2014. [cited 2015 Oct 16]. Available from: http://search.proquest.com.proxy.library.vanderbilt.edu/psycinfo/docview/1678756305/A54D146EE66D43E3PQ/1. [Google Scholar]
- 68.Cuthbert BN, Insel TR. Toward the future of psychiatric diagnosis: the seven pillars of RDoC. BMC Med. 2013;11(1):126. doi: 10.1186/1741-7015-11-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Patrick J, Dyck M, Bramston P. Depression Anxiety Stress Scale: Is it valid for children and adolescents? J Clin Psychol. 2010 Sep;66(9):996–1007. doi: 10.1002/jclp.20696. [DOI] [PubMed] [Google Scholar]
- 70.Barlow DH, Allen LB, Choate ML. Toward a unified treatment for emotional disorders. Behav Ther. 2004 Spring;35(2):205–30. doi: 10.1016/j.beth.2016.11.005. [DOI] [PubMed] [Google Scholar]
- 71.Mansell W, Harvey A, Watkins E, Shafran R. Conceptual Foundations of the Transdiagnostic Approach to CBT. J Cogn Psychother. 2009;23(1):6–19. [Google Scholar]
- 72.Ehrenreich JT, Goldstein CR, Wright LR, Barlow DH. Development of a Unified Protocol for the Treatment of Emotional Disorders in Youth. Child Fam Behav Ther. 2009 Jan;31(1):20. doi: 10.1080/07317100802701228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Martinsen KD, Kendall PC, Stark K, Neumer SP. Prevention of Anxiety and Depression in Children: Acceptability and Feasibility of the Transdiagnostic EMOTION Program. Cogn Behav Pract [Internet] In press [cited 2015 Oct 16]; Available from: http://www.sciencedirect.com/science/article/pii/S1077722914000959.
- 74.Kendall PC, Hedtke KA. Cognitive-behavioral therapy for anxious children: Therapist manual. Workbook Pub.; 2006. [Google Scholar]
- 75.Kendall PC, Hedtke KA. The coping cat workbook. Workbook Pub.; 2006. [Google Scholar]
- 76.Stark KD, Kendall PC. Treating depressed children: Therapist manual for Taking Action. Workbook; 1996. [Google Scholar]
- 77.De Cuyper S, Timbremont B, Braet C, De Backer V, Wullaert T. Treating depressive symptoms in schoolchildren: A pilot study. Eur Child Adolesc Psychiatry. 2004 Apr;13(2):105–14. doi: 10.1007/s00787-004-0366-2. [DOI] [PubMed] [Google Scholar]
- 78.Diamond GS, Reis BF, Diamond GM, Siqueland L, Isaacs L. Attachment-based family therapy for depressed adolescents: A treatment development study. J Am Acad Child Adolesc Psychiatry. 2002 Oct;41(10):1190–6. doi: 10.1097/00004583-200210000-00008. [DOI] [PubMed] [Google Scholar]
- 79.Fleming T, Dixon R, Frampton C, Merry SN. A pragmatic randomized controlled trial of computerized CBT (SPARX) for symptoms of depression among adolescents excluded from mainstream education. Behav Cogn Psychother. 2012 Oct;40(5):529–41. doi: 10.1017/S1352465811000695. [DOI] [PubMed] [Google Scholar]
- 80.Melvin GA, Tonge BJ, King NJ, Heyne D, Gordon MS, Klimkeit E. A Comparison of Cognitive-Behavioral Therapy, Sertraline, and Their Combination for Adolescent Depression. J Am Acad Child Adolesc Psychiatry. 2006 Oct;45(10):1151–61. doi: 10.1097/01.chi.0000233157.21925.71. [DOI] [PubMed] [Google Scholar]
- 81.Merry SN, Stasiak K, Shepherd M, Frampton C, Fleming T, Lucassen MFG. The effectiveness of SPARX, a computerised self help intervention for adolescents seeking help for depression: randomised controlled non-inferiority trial. BMJ. 2012;344 doi: 10.1136/bmj.e2598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Reynolds WM, Coats KI. A comparison of cognitive-behavioral therapy and relaxation training for the treatment of depression in adolescents. J Consult Clin Psychol. 1986 Oct;54(5):653–60. doi: 10.1037//0022-006x.54.5.653. [DOI] [PubMed] [Google Scholar]
- 83.Stark KD, Reynolds WM, Kaslow NJ. A comparison of the relative efficacy of self-control therapy and a behavioral problem-solving therapy for depression in children. J Abnorm Child Psychol. 1987 Mar;15(1):91–113. doi: 10.1007/BF00916468. [DOI] [PubMed] [Google Scholar]
- 84.Vostanis P, Feehan C, Grattan E, Bickerton W-L. Treatment for children and adolescents with depression: Lessons from a controlled trial. Clin Child Psychol Psychiatry. 1996 Apr;1(2):199–212. [Google Scholar]
- 85.Wood A, Harrington R, Moore A. Controlled trial of a brief cognitive-behavioural intervention in adolescent patients with depressive disorders. Child Psychol Psychiatry Allied Discip. 1996 Sep;37(6):737–46. doi: 10.1111/j.1469-7610.1996.tb01466.x. [DOI] [PubMed] [Google Scholar]
- 86.Baer S, Garland EJ. Pilot Study of Community-Based Cognitive Behavioral Group Therapy for Adolescents With Social Phobia. J Am Acad Child Adolesc Psychiatry. 2005 Mar;44(3):258–64. doi: 10.1097/00004583-200503000-00010. [DOI] [PubMed] [Google Scholar]
- 87.Barrett PM, Dadds MR, Rapee RM. Family treatment of childhood anxiety: A controlled trial. J Consult Clin Psychol. 1996 Apr;64(2):333–42. doi: 10.1037//0022-006x.64.2.333. [DOI] [PubMed] [Google Scholar]
- 88.Beidel DC, Turner SM, Morris TL. Behavioral treatment of childhood social phobia. J Consult Clin Psychol. 2000 Dec;68(6):1072–80. [PubMed] [Google Scholar]
- 89.Flannery-Schroeder EC, Kendall PC. Group and individual cognitive–behavioral treatments for youth with anxiety disorders: A randomized clinical trial. Cogn Ther Res. 2000 Jun;24(3):251–78. [Google Scholar]
- 90.Gallagher HM, Rabian BA, McCloskey MS. A brief group cognitive-behavioral intervention for social phobia in childhood. J Anxiety Disord. 2004;18(4):459–79. doi: 10.1016/S0887-6185(03)00027-6. [DOI] [PubMed] [Google Scholar]
- 91.Ingul JM, Aune T, Nordahl HM. A randomized controlled trial of individual cognitive therapy, group cognitive behaviour therapy and attentional placebo adolescent social phobia. Psychother Psychosom. 2014 Nov;83(1):54–61. doi: 10.1159/000354672. [DOI] [PubMed] [Google Scholar]
- 92.Kendall PC, Flannery-Schroeder E, Panichelli-Mindel SM, Southam-Gerow M, Henin A, Warman M. Therapy for youths with anxiety disorders: A second randomized clincal trial. J Consult Clin Psychol. 1997 Jun;65(3):366–80. doi: 10.1037//0022-006x.65.3.366. [DOI] [PubMed] [Google Scholar]
- 93.Kendall PC. Treating anxiety disorders in children: Results of a randomized clinical trial. J Consult Clin Psychol. 1994 Feb;62(1):100–10. doi: 10.1037//0022-006x.62.1.100. [DOI] [PubMed] [Google Scholar]
- 94.Khanna MS, Kendall PC. Computer-assisted cognitive behavioral therapy for child anxiety: Results of a randomized clinical trial. J Consult Clin Psychol. 2010 Oct;78(5):737–45. doi: 10.1037/a0019739. [DOI] [PubMed] [Google Scholar]
- 95.Last CG, Hansen C, Franco N. Cognitive-behavioral treatment of school phobia. J Am Acad Child Adolesc Psychiatry. 1998 Apr;37(4):404–11. doi: 10.1097/00004583-199804000-00018. [DOI] [PubMed] [Google Scholar]
- 96.Lyneham HJ, Rapee RM. Evaluation of therapist-supported parent-implemented CBT for anxiety disorders in rural children. Behav Res Ther. 2006 Sep;44(9):1287–300. doi: 10.1016/j.brat.2005.09.009. [DOI] [PubMed] [Google Scholar]
- 97.March S, Spence SH, Donovan CL. The efficacy of an Internet-based cognitive-behavioral therapy intervention for child anxiety disorders. J Pediatr Psychol. 2009 Jun;34(5):474–87. doi: 10.1093/jpepsy/jsn099. [DOI] [PubMed] [Google Scholar]
- 98.Masia Warner C, Fisher PH, Shrout PE, Rathor S, Klein RG. Treating adolescents with social anxiety disorder in school: An attention control trial. J Child Psychol Psychiatry. 2007 Jul;48(7):676–86. doi: 10.1111/j.1469-7610.2007.01737.x. [DOI] [PubMed] [Google Scholar]
- 99.Muris P, Meesters C, van Melick M. Treatment of childhood anxiety disorders; A preliminary comparison between cognitive-behavioral group therapy and a psychological placebo intervention. J Behav Ther Exp Psychiatry. 2002 Dec;33(3–4):143–58. doi: 10.1016/s0005-7916(02)00025-3. [DOI] [PubMed] [Google Scholar]
- 100.Pincus DB, May JE, Whitton SW, Mattis SG, Barlow DH. Cognitive-behavioral treatment of panic disorder in adolescence. J Clin Child Adolesc Psychol. 2010 Sep;39(5):638–49. doi: 10.1080/15374416.2010.501288. [DOI] [PubMed] [Google Scholar]
- 101.Silverman WK, Kurtines WM, Ginsburg GS, Weems CF, Lumpkin PW, Carmichael DH. Treating anxiety disorders in children with group cognitive-behavioral therapy: A randomized clinical trial. J Consult Clin Psychol. 1999 Dec;67(6):995–1003. doi: 10.1037//0022-006x.67.6.995. [DOI] [PubMed] [Google Scholar]
- 102.Spence SH, Holmes JM, March S, Lipp OV. The feasibility and outcome of clinic plus Internet delivery of cognitive-behavior therapy for childhood anxiety. J Consult Clin Psychol. 2006 Jun;74(3):614–21. doi: 10.1037/0022-006X.74.3.614. [DOI] [PubMed] [Google Scholar]
- 103.Thirlwall K, Cooper PJ, Karalus J, Voysey M, Willetts L, Creswell C. Treatment of child anxiety disorders via guided parent-delivered cognitive–behavioural therapy: Randomised controlled trial. Br J Psychiatry. 2013 Dec;203(6):436–44. doi: 10.1192/bjp.bp.113.126698. [DOI] [PubMed] [Google Scholar]
- 104.Challen AR, Machin SJ, Gillham JE. The UK Resilience Programme: A school-based universal nonrandomized pragmatic controlled trial. J Consult Clin Psychol. 2014 Feb;82(1):75–89. doi: 10.1037/a0034854. [DOI] [PubMed] [Google Scholar]
- 105.Dobson KS, Hopkins JA, Fata L, Scherrer M, Allan LC. The prevention of depression and anxiety in a sample of high-risk adolescents: A randomized controlled trial. Can J Sch Psychol. 2010 Dec;25(4):291–310. [Google Scholar]
- 106.Gillham JE, Reivich KJ, Freres DR, Lascher M, Litzinger S, Shatté A, et al. School-based prevention of depression and anxiety symptoms in early adolescence: A pilot of a parent intervention component. Sch Psychol Q Vol. 2006 Fal;213:323–48. [Google Scholar]
- 107.Pattison C, Lynd-Stevenson RM. The prevention of depressive symptoms in children: The immediate and long-term outcomes of a school based program. Behav Change. 2001;182:92–102. [Google Scholar]
- 108.Day C, Kane RT, Roberts C. The prevention of depressive symptoms in rural Australian women. J Community Appl Soc Psychol. 2003;131(2003):1–14. [Google Scholar]
- 109.Roberts CM, Kane R, Bishop B, Cross D, Fenton J, Hart B. The prevention of anxiety and depression in children from disadvantaged schools. Behav Res Ther. 2010 Jan;48(1):68–73. doi: 10.1016/j.brat.2009.09.002. [DOI] [PubMed] [Google Scholar]
- 110.Sheffield JK, Spence SH, Rapee RM, Kowalenko N, Wignall A, Davis A, et al. Evaluation of universal, indicated, and combined cognitive-behavioral approaches to the prevention of depression among adolescents. J Consult Clin Psychol. 2006 Feb;74(1):66–79. doi: 10.1037/0022-006X.74.1.66. [DOI] [PubMed] [Google Scholar]
- 111.Spence SH, Sawyer MG, Sheffield J, Patton G, Bond L, Graetz B, et al. Does the absence of a supportive family environment influence the outcome of a universal intervention for the prevention of depression? Int J Environ Res Public Health. 2014;11(5):5113–32. doi: 10.3390/ijerph110505113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Stallard P, Sayal K, Phillips R, Taylor JA, Spears M, Anderson R, et al. Classroom based cognitive behavioural therapy in reducing symptoms of depression in high risk adolescents: pragmatic cluster randomised controlled trial. BMJ. 2012;345 doi: 10.1136/bmj.e6058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Wong N, Kady L, Mewton L, Sunderland M, Andrews G. Preventing anxiety and depression in adolescents: A randomised controlled trial of two school based Internet-delivered cognitive behavioural therapy programmes. Internet Interv. 2014;1(2):90–4. [Google Scholar]
- 114.Young JF, Mufson L, Gallop RJ. Preventing depression: A randomized trial of interpersonal psychotherapy-adolescent skills training. Depress Anxiety. 2010 May;27(5):426–33. doi: 10.1002/da.20664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Aune T, Stiles TC. Universal-based prevention of syndromal and subsyndromal social anxiety: A randomized controlled study. J Consult Clin Psychol. 2009 Oct;77(5):867–79. doi: 10.1037/a0015813. [DOI] [PubMed] [Google Scholar]
- 116.Balle M, Tortella-Feliu M. Efficacy of a brief school-based program for selective prevention of childhood anxiety. Anxiety Stress Coping Int J. 2010 Jan;23(1):71–85. doi: 10.1080/10615800802590652. [DOI] [PubMed] [Google Scholar]
- 117.Barrett PM, Turner C. Prevention of anxiety symptoms in primary school children: Preliminary results from a universal school-based trial. Br J Clin Psychol. 2001;40(4):399–410. doi: 10.1348/014466501163887. [DOI] [PubMed] [Google Scholar]
- 118.Barrett PM, Sonderegger R, Xenos S. Using FRIENDS to combat anxiety and adjustment problems among young migrants to Australia: A national trial. Clin Child Psychol Psychiatry. 2003 Apr;8(2):241–60. [Google Scholar]
- 119.Essau CA, Conradt J, Sasagawa S, Ollendick TH. Prevention of anxiety symptoms in children: Results from a universal school-based trial. Behav Ther. 2012 Jun;43(2):450–64. doi: 10.1016/j.beth.2011.08.003. [DOI] [PubMed] [Google Scholar]
- 120.Gallegos J. Preventing childhood anxiety and depression: Testing the effectiveness of a school-based program in Mexico. [Internet] ProQuest Information & Learning (,US) 2009 [cited 2015 Oct 17]. Available from: http://search.proquest.com.proxy.library.vanderbilt.edu/psycinfo/docview/622064740/FAEF3BF7B2541DFPQ/1.
- 121.Hains AA, Ellmann SW. Stress inoculation training as a preventative intervention for high school youths. J Cogn Psychother. 1994 Fal;8(3):219–32. [Google Scholar]
- 122.Hains AA, Szyjakowski M. A cognitive stress-reduction intervention program for adolescents. J Couns Psychol. 1990 Jan;37(1):79–84. [Google Scholar]
- 123.Kehoe CE, Havighurst SS, Harley AE. Tuning in to teens: Improving parent emotion socialization to reduce youth internalizing difficulties. Soc Dev. 2014 May;23(2):413–31. [Google Scholar]
- 124.Lock S, Barrett PM. A Longitudinal Study of Developmental Differences in Universal Preventive Intervention for Child Anxiety. Behav Change. 2003;20(4):183–99. [Google Scholar]
- 125.Lowry-Webster HM, Barrett PM, Dadds MR. A universal prevention trial of anxiety and depressive symptomatology in childhood: Preliminary data from an Australian study. Behav Change. 2001;18(1):36–50. [Google Scholar]
- 126.Weersing R, Jeffreys M, Do M, Schwartz KG, Bolano C. Evidence-based update: Treatment of depression in children and adolescents. J Clin Child Adolesc Psychol. doi: 10.1080/15374416.2016.1220310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Kovacs M. Children’s Depression Inventory. North Tonawanda, NY: Multi-Health Systems, Inc; 1992. [Google Scholar]
- 128.Spence SH. A measure of anxiety symptoms among children. Behav Res Therapy. 1998;36(5):545–566. doi: 10.1016/s0005-7967(98)00034-5. [DOI] [PubMed] [Google Scholar]
- 129.Price M1, Higa-McMillan C, Ebesutani C, Okamura K, Nakamura BJ, Chorpita BF, Weisz J. Symptom differentiation of anxiety and depression across youth development and clinic-referred/nonreferred samples: An examination of competing factor structures of the Child Behavior Checklist DSM-oriented scales. Dev Psychopathol. 2013;4(Pt 1):1005–1015. doi: 10.1017/S0954579413000333. [DOI] [PubMed] [Google Scholar]
- 130.TADS. Fluoxetine, cognitive-behavioral therapy, and their combination for adolescents with depression: Treatment for Adolescents with Depression Study (TADS) randomized controlled trial. JAMA. 2004;292:807–820. doi: 10.1001/jama.292.7.807. [DOI] [PubMed] [Google Scholar]


